COVID-19 Prophylaxis Efforts Based on Natural Antiviral Plant Extracts and Their Compounds
Abstract
1. Introduction
2. Results and Discussion
2.1. Ethnobotanical Background of Plants with Antiviral Potential
2.2. Plant-Derived Antiviral Compounds Against Coronavirus
2.2.1. Zoonotic Interventions
2.2.2. Antiviral Flavonoids
2.2.3. Antiviral Terpenoids
2.2.4. Antiviral Alkaloids
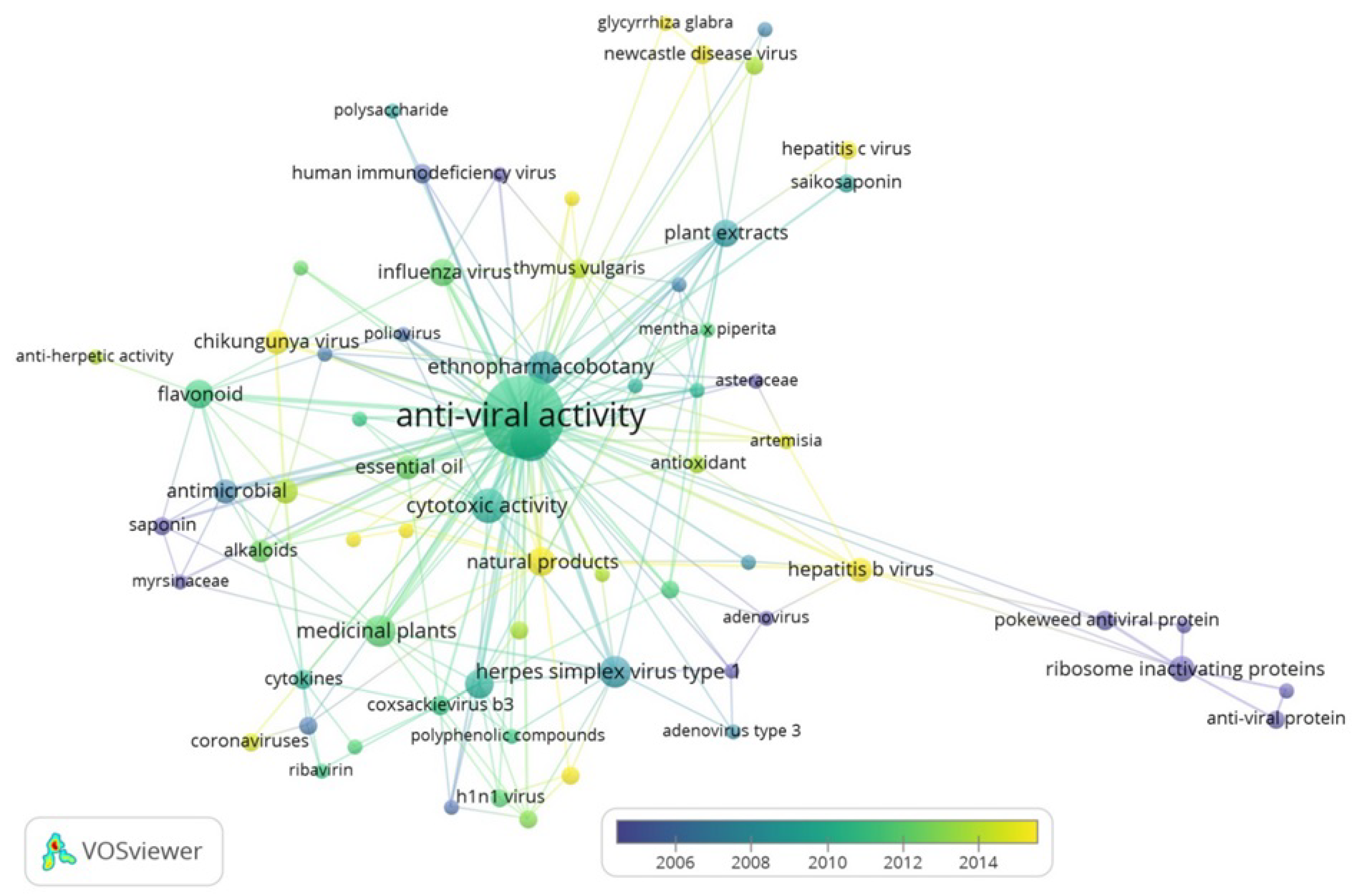
2.3. VOSviewer Visualization of Scientific Data Analysis of Antiviral Potential of Natural Compounds from Various Medicinal Herbs and Crops
3. Methodology
4. Conclusions
Autor Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, Y.-C.; Kuo, R.-L.; Shih, S.-R. COVID-19: The first documented coronavirus pandemic in history. Biomed. J. 2020, 43, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Coronaviridae Study Group of the International Committee on Taxonomy of V. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.F.-W.; Yuan, S.; Kok, K.-H.; To, K.K.-W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.-Y.; Poon, R.W.-S.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef]
- Rehman, I.U.; Khan, H.R.; E Zainab, W.; Ahmed, A.; Ishaq, M.D.; Ullah, I. Barriers in Social Distancing during Covid19 pandemic -Is a message for forced lockdown? J. Med. Res. Innov. 2020, 4, e000222. [Google Scholar] [CrossRef]
- Balachandar, V.; Mahalaxmi, I.; Kaavya, J.; Vivekanandhan, G.; Ajithkumar, S.; Arul, N.; Singaravelu, G.; Kumar, N.S.; Dev, S.M. COVID-19: Emerging protective measures. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 3422–3425. [Google Scholar] [PubMed]
- Dong, Y.; Dai, T.; Wei, Y.; Zhang, L.; Zheng, M.; Zhou, F. A systematic review of SARS-CoV-2 vaccine candidates. Sig. Transduct. Target Ther. 2020, 5, 237. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Vaccines. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 10 January 2020).
- Huang, J.; Tao, G.; Liu, J.; Cai, J.; Huang, Z.; Chen, J.-X. Current Prevention of COVID-19: Natural Products and Herbal Medicine. Front. Pharmacol. 2020, 11, 588508. [Google Scholar] [CrossRef]
- Mahmood, N.; Nasir, S.B.; Hefferon, K. Plant-Based Drugs and Vaccines for COVID-19. Vaccines 2020, 9, 15. [Google Scholar] [CrossRef]
- Liew, P.S.; Hair-Bejo, M. Farming of plant-based veterinary vaccines and their applications for disease prevention in animal. Adv. Virol. 2015, 2015, 936940. [Google Scholar] [CrossRef]
- Naja, F.; Hamadeh, R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. Eur. J. Clin. Nutr. 2020, 74, 1117–1121. [Google Scholar] [CrossRef]
- Galanakis, C.M. The food systems in the era of the coronavirus (COVID-19) pandemic crisis. Foods 2020, 9, 523. [Google Scholar] [CrossRef] [PubMed]
- Panyod, S.; Ho, C.-T.; Sheen, L.-Y. Dietary therapy and herbal medicine for COVID-19 prevention: A review and perspective. J. Tradit. Complement. Med. 2020, 10, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shabat, S.; Yarmolinsky, L.; Porat, D.; Dahan, A. Antiviral effect of phytochemicals from medicinal plants: Applications and drug delivery strategies. Drug Deliv. Transl. Res. 2019, 10, 354–367. [Google Scholar] [CrossRef]
- Joshi, B.; Panda, S.K.; Jouneghani, R.S.; Liu, M.; Parajuli, N.; Leyssen, P.; Neyts, J.; Luyten, W. Antibacterial, antifungal, antiviral, and anthelmintic activities of medicinal plants of Nepal selected sased on ethnobotanical evidence. Evid. Based Complementary Altern. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Zambounis, A.; Sytar, O.; Valasiadis, D.; Hilioti, Z. Effect of photosensitisers on growth and morphology of Phytophthora citrophthora coupled with leaf bioassays in pear seedlings. Plant Protect. Sci. 2020, 56, 74–82. [Google Scholar] [CrossRef]
- Ríos, J.L.; Recio, M.C. Medicinal plants and antimicrobial activity. J. Ethnopharmacol. 2005, 100, 80–84. [Google Scholar] [CrossRef]
- Ghildiyal, R.; Prakash, V.; Chaudhary, V.K.; Gupta, V.; Gabrani, R. Phytochemicals as Antiviral Agents: Recent Updates. In Plant-Derived Bioactives; Swamy, M., Ed.; Springer: Singapore, 2020. [Google Scholar]
- Gautret, P.; Lagier, J.-C.; Honoré, S.; Hoang, V.T.; Raoult, D. Clinical efficacy and safety profile of hydroxychloroquine and azithromycin against COVID-19. Int. J. Antimicrob. Agents 2021, 57, 106242. [Google Scholar] [CrossRef]
- Zhang, D.-H.; Wu, K.-L.; Zhang, X.; Deng, S.-Q.; Peng, B. In silico screening of Chinese herbal medicines with the potential to directly inhibit 2019 novel coronavirus. J. Integr. Med. 2020, 18, 152–158. [Google Scholar] [CrossRef]
- Sampangi-Ramaiah, M.H.; Vishwakarma, R.; Shaanker, R.U. Molecular docking analysis of selected natural products from plants for inhibition of SARS-CoV-2 main protease. Curr. Sci. 2020, 118, 1087–1092. [Google Scholar]
- Lee, H.; Lei, H.; Santarsiero, B.D.; Gatuz, J.L.; Cao, S.; Rice, A.J.; Patel, K.; Szypulinski, M.Z.; Ojeda, I.; Ghosh, A.K.; et al. Inhibitor recognition specificity of MERS-CoV papain-like protease may differ from that of SARS-CoV. ACS Chem. Biol. 2015, 10, 1456–1465. [Google Scholar] [CrossRef]
- Liu, A.; Du, G.-H. Antiviral Properties of Phytochemicals. In Dietary Phytochemicals and Microbes; Patra, A., Ed.; Springer: Dordrecht, The Netherlands, 2012. [Google Scholar]
- Monajjemi, M.; Mollaamin, F.; Shojaei, S. An overview on Coronaviruses family from past to Covid-19: Introduce some inhibitors as antiviruses from Gillan’s plants. Biointerface Res. Appl. Chem. 2020, 10, 5575–5585. [Google Scholar]
- Eng, Y.S.; Lee, C.-H.; Lee, W.C.; Huang, C.C.; Chang, J.S. Unraveling the molecular mechanism of traditional chinese medicine: Formulas against acute airway viral infections as examples. Molecules 2019, 24, 3505. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Islam, S.; Wang, J.; Li, Y.; Chen, X. Traditional Chinese Medicine in the Treatment of Patients Infected with 2019-New Coronavirus (SARS-CoV-2): A Review and Perspective. Int. J. Biol. Sci. 2020, 16, 1708–1717. [Google Scholar] [CrossRef] [PubMed]
- Ameri, A.; Heydarirad, G.; Jafari, J.M.; Ghobadi, A.; Rezaeizadeh, H.; Choopani, R. Medicinal plants contain mucilage used in traditional Persian medicine (TPM). Pharm. Biol. 2015, 53, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Buso, P.; Manfredini, S.; Ashtiani, H.R.A.; Sciabica, S.; Buzzi, R.; Vertuani, S.; Baldisserotto, A. Iranian Medicinal Plants: From Ethnomedicine to Actual Studies. Medicina (Kaunas) 2020, 56, 97. [Google Scholar] [CrossRef]
- Raheel, R.; Ashraf, M.; Ejaz, S.; Javeed, A.; Altaf, I. Assessment of the cytotoxic and antiviral potential of aqueous extracts from different parts of Acacia nilotica (Linn) Delile against Peste des petits ruminants virus. Environ. Toxicol. Pharmacol. 2013, 35, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Ramezany, F.; Kiyani, N.; Khademizadeh, M. Persian manna in the past and the present: An overview. Am. J. Pharmacol. Sci. 2013, 1, 35–37. [Google Scholar] [CrossRef]
- Shojai, T.M.; Langeroudi, A.G.; Karimi, V.; Barin, A.; Sadri, N. The effect of Allium sativum (Garlic) extract on infectious bronchitis virus in specific pathogen free embryonic egg. Avicenna J. Phytomedicine 2016, 6, 458-267. [Google Scholar]
- Pontin, M.; Bottini, R.; Burba, J.L.; Piccoli, P.N. Allium sativum produces terpenes with fungistatic properties in response to infection with Sclerotium cepivorum. Phytochemistry 2015, 115, 152–160. [Google Scholar] [CrossRef]
- Mustafayeva, I.R.; Ibadullayeva, S.J.; Alakbarov, R.A.; Ismayilov, A.H.; Qasimov, H.Z.; Qasimova, S.S. Pharmacognosis with the Basis of Botany. Science-Education: Baku, Azerbaijan, 2015; 615p. [Google Scholar]
- Shah, S.M.A.; Akhtar, N.; Akram, M.; Shah, P.A.; Tariq Saeed, T.; Ahmed, K.; Asif, H.M. Pharmacological activity of Althaea officinalis L. J. Med. Plants Res. 2011, 5, 5662–5666. [Google Scholar]
- Munir, O.; Volkan, A.; Ernaz, A.; Ibadullayeva, S.J.; Aslanipour, B.; Günenç, T.M. Herbals in Iğdır (Turkey), Nakhchivan (Azerbaijan), and Tabriz (Iran)/Herbs and Human Health. In Ethnobotany and Physiology; Springer: Berlin/Heidelberg, Germany, 2018; Volume 1, pp. 197–262. [Google Scholar]
- Peçanha, L.M.T.; Fernandes, P.D.; Simen, T.J.-M.; De Oliveira, D.R.; Finotelli, P.V.; Pereira, M.V.A.; Barboza, F.F.; Almeida, T.D.S.; Carvalhal, S.; Pierucci, A.P.T.R.; et al. Immunobiologic and antiinflammatory properties of a bark extract from Ampelozizyphus amazonicus Ducke. BioMed. Res. Int. 2013, 2013, 451679. [Google Scholar] [CrossRef] [PubMed]
- Hossain, S.; Urbi, Z.; Sule, A.; Rahman, K.M.H. Andrographis paniculata (Burm. f.) Wall. ex Nees: A review of ethnobotany, phytochemistry, and pharmacology. Sci. World J. 2014, 2014, 274905. [Google Scholar] [CrossRef] [PubMed]
- Ulasli, M.; Gurses, S.A.; Bayraktar, R.; Yumrutas, O.; Oztuzcu, S.; Igci, M.; Igci, Y.Z.; Cakmak, E.A.; Arslan, A. The effects of Nigella sativa (Ns), Anthemis hyalina (Ah) and Citrus sinensis (Cs) extracts on the replication of coronavirus and the expression of TRP genes family. Mol. Biol. Rep. 2014, 41, 1703–1711. [Google Scholar] [CrossRef] [PubMed]
- Brandão, G.; Kroon, E.; Dos Santos, J.; Stehmann, J.; Lombardi, J.; De Oliveira, A.B. Antiviral activity of Bignoniaceae species occurring in the State of Minas Gerais (Brazil): Part 1. Lett. Appl. Microbiol. 2010, 51, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.-B.; Choi, M.-S.; Ryu, B.; Lee, N.-R.; Kim, H.-I.; Choi, H.-E.; Chang, J.; Lee, K.-T.; Jang, D.S.; Inn, K.-S. Antiviral activity of carnosic acid against respiratory syncytial virus. Virol. J. 2013, 10, 303. [Google Scholar] [CrossRef] [PubMed]
- Nigam, M.; Atanassova, M.; Mishra, A.P.; Pezzani, R.; Devkota, H.P.; Plygun, S.; Salehi, B.; Setzer, W.N.; Sharifi-Rad, J. Bioactive compounds and health benefits of Artemisia species. Nat. Prod. Commun. 2019, 14, 1–17. [Google Scholar] [CrossRef]
- Kohn, L.; Foglio, M.; Rodrigues, R.; De O Sousa, I.; Martini, M.; Padilla, M.; Neto, D.D.L.; Arns, C. In-Vitro Antiviral Activities of Extracts of Plants of The Brazilian Cerrado against the Avian Metapneumovirus (aMPV). Braz. J. Poult. Sci. 2015, 17, 275–280. [Google Scholar] [CrossRef]
- LaRocca, D.G.; Da Silva, I.V.; Junior, N.G.R.; Saldanha, K.L.A.; Rocha, J.A.; De Andrade Royo, V. Characterizing Casca d´anta: An Apocynaceae used to treat tropical diseases in the Amazonian region. Idesia (Arica) 2019, 37, 65–73. [Google Scholar] [CrossRef]
- Lebedeva, A.A.; Zakharchenko, N.S.; Trubnikova, E.V.; Medvedeva, O.A.; Kuznetsova, T.; Masgutova, G.A.; Zylkova, M.V.; Buryanov, Y.I.; Belous, A.S. Bactericide, immunomodulating, and wound healing properties of transgenic Kalanchoe pinnata Synergize with antimicrobial peptide cecropin P1 in vivo. J. Immunol. Res. 2017, 2017, 4645701. [Google Scholar] [CrossRef]
- Yang, J.L.; Ha, T.K.Q.; Oh, W.K. Discovery of inhibitory materials against PEDV corona virus from medicinal plants. Jpn. J. Vet. Res. 2016, 64, S53–S63. [Google Scholar] [CrossRef]
- Yang, J.-L.; Ha, T.-K.-Q.; Dhodary, B.; Pyo, E.; Nguyen, N.H.; Cho, H.; Kim, E.; Oh, W.K. Oleanane triterpenes from the flowers of Camellia japonica inhibit porcine epidemic diarrhea virus (PEDV) replication. J. Med. Chem. 2015, 58, 1268–1280. [Google Scholar] [CrossRef] [PubMed]
- Ziai, S.A.; Hamkar, R.; Monavari, H.R.; Norooz-Babaei, Z.; Adibi, L. Antiviral effect assay of twenty five species of various medicinal plants families in Iran. J. Med. Plants 2007, 1, 1–9. [Google Scholar]
- Fatima, M.; Zaidi, N.-U.-S.S.; Amraiz, D.; Afzal, F. In vitro antiviral activity of cinnamomum cassia and its nanoparticles against H7N3 Influenza A Virus. J. Microbiol. Biotechnol. 2016, 26, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.F.; Chang, J.S.; Wang, K.C.; Shieh, D.E.; Chiang, L.C. Water extract of Cinnamomum cassia Blume inhibited human respiratory syncytial virus by preventing viral attachment, internalization, and syncytium formation. J. Ethnopharmacol. 2013, 147, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Ooi, L.S.M.; Li, Y.; Kam, S.-L.; Wang, H.; Wong, E.Y.L.; Ooi, V.E.C. Antimicrobial activities of cinnamon oil and cinnamaldehyde from the Chinese medicinal herb Cinnamomum cassia Blume. Am. J. Chin. Med. 2006, 34, 511–522. [Google Scholar] [CrossRef]
- Heo, Y.; Cho, Y.; Ju, K.S.; Cho, H.; Park, K.H.; Choi, H.; Yoon, J.K.; Moon, C.; Kim, Y.B. Antiviral activity of Poncirus trifoliata seed extract against oseltamivir-resistant influenza virus. J. Microbiol. 2018, 56, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Elsebai, M.F.; Mocan, A.; Atanasov, A.G. Cynaropicrin: A comprehensive research review and therapeutic potential as an anti-hepatitis C virus agent. Front. Pharmacol. 2016, 7, 472. [Google Scholar] [CrossRef]
- Lelešius, R.; Karpovaitė, A.; Mickienė, R.; Drevinskas, T.; Tiso, N.; Ragažinskienė, O.; Kubilienė, L.; Maruška, A.; Salomskas, A. In vitro antiviral activity of fifteen plant extracts against avian infectious bronchitis virus. BMC Vet. Res. 2019, 15, 178. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Shawn, A.; Anderson, S.A.; Schoop, R.; Hudson, J.B. Induction of multiple pro-inflammatory cytokines by respiratory viruses and reversal by standardized Echinacea, a potent antiviral herbal extract. Antivir. Res. 2009, 83, 165–170. [Google Scholar] [CrossRef]
- Nasseri, M.A.; Keshtkar, H.; Kazemnejadi, M.; Allahresani, A. Phytochemical properties and antioxidant activity of Echinops persicus plant extract: Green synthesis of carbon quantum dots from the plant extract. SN Appl. Sci. 2020, 2, 1–12. [Google Scholar] [CrossRef]
- Farahani, M. Antiviral effect assay of aqueous extract of Echium amoenum L. against HSV-1. Zahedan J. Res. Med Sci. (Tabib-E-Shargh) 2013, 15, 46–48. [Google Scholar]
- Abolhassani, M. Antiviral activity of borage (Echium amoenum). Arch Med. Sci. 2010, 3, 366–369. [Google Scholar] [CrossRef] [PubMed]
- A Betancur-Galvis, L.; E Morales, G.; E Forero, J.; Roldan, J. Cytotoxic and antiviral activities of colombian medicinal plant extracts of the Euphorbia genus. Mem. Inst. Oswaldo Cruz. 2002, 97, 541–546. [Google Scholar] [CrossRef]
- Gyuris, A.; Szlávik, L.; Minárovits, J.; Vasas, A.; Molnár, J.; Hohmann, J. Antiviral activities of extracts of Euphorbia hirta L. against HIV-1, HIV-2 and SIVmac251. In Vivo 2009, 23, 429–432. [Google Scholar]
- Iranshahy, M.; Iranshahi, M. Traditional uses, phytochemistry and pharmacology of asafoetida (Ferula assa-foetida oleo-gum-resin)-a review. J. Ethnopharmacol. 2011, 134, 1–10. [Google Scholar] [CrossRef]
- Lee, C.-L.; Chiang, L.-C.; Cheng, L.-H.; Liaw, C.-C.; El-Razek, M.H.A.; Chang, F.-R.; Wu, Y.-C. Influenza A (H(1)N(1)) Antiviral and Cytotoxic Agents from Ferula assa-foetida. J. Nat. Prod. 2009, 72, 1568–1572. [Google Scholar] [CrossRef]
- Kakhramanova, M.; Ibadullaeva, S.J. Mysterious World of Plants (Grass Plants). Science-Education: Baku, Azerbaijan, 2017; p. 350. [Google Scholar]
- Kakhramanova, M.; Ibadullaeva, S.J. Immunostimulatory Phytospore with a General Strengthening Effect; Eurasian Patent Office: Moscow, Russia, 2017; pp. 1–4. [Google Scholar]
- Anagha, K.; Manasi, D.; Meera, M. Scope of Glycyrrhiza glabra (Yashtimadhu) as an antiviral agent: A Review. Int. J. Curr. Microbiol. App. Sci. 2014, 3, 657–665. [Google Scholar]
- Khan, F.; Sarker, M.R.; Ming, L.C.; Mohamed, I.N.; Zhao, C.; Sheikh, B.Y.; Tsong, H.F.; Rashid, M.A. Comprehensive review on phytochemicals, pharmacological and clinical potentials of Gymnema sylvestre. Front. Pharmacol. 2019, 10, 1223. [Google Scholar] [CrossRef]
- Mishra, K.P.; Chanda, S.; Karan, D.; Ganju, L.; Sawhney, R.C. Effect of Seabuckthorn (Hippophae rhamnoides) flavone on immune system: An in-vitro approach. Phytother. Res. 2008, 22, 1490–1495. [Google Scholar] [CrossRef]
- Ibadullayeva, S.J.; Mamedova, S.E.; Sultanova, Z.R.; Movsumova, N.V.; Jafarli, I.A. Medicinal plants of Azerbaijan flora used in the treatment of certain diseases. Afr. J. Pharm. Pharmacol. 2010, 4, 545–548. [Google Scholar]
- Enkhtaivan, G.; John, K.M.; Pandurangan, M.; Hur, J.H.; Leutou, A.S.; Kim, D.H. Extreme effects of Seabuckthorn extracts on influenza viruses and human cancer cells and correlation between flavonol glycosides and biological activities of extracts. Saudi J. Biol. Sci. 2017, 24, 1646–1656. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.-M.; Lee, K.-M.; Koon, C.-M.; Cheung, C.S.-F.; Lau, C.-P.; Ho, H.-M.; Lee, M.Y.-H.; Au, S.W.-N.; Cheng, C.H.-K.; Lau, C.B.-S.; et al. Immunomodulatory and anti-SARS activities of Houttuynia cordata. J. Ethnopharmacol. 2008, 118, 79–85. [Google Scholar] [CrossRef] [PubMed]
- E Buckwold, V.; Wilson, R.J.H.; Nalca, A.; Beer, B.B.; Voss, T.G.; A Turpin, J.; Buckheit, R.W.; Wei, J.; Wenzel-Mathers, M.; Walton, E.M. Antiviral activity of hop constituents against a series of DNA and RNA viruses. Antivir. Res. 2004, 61, 57–62. [Google Scholar] [CrossRef]
- Ibadullayeva, S.; Alekperov, R. Medicinal Herbs (Ethnobotany and Phyitotherapy) Baku; ELM: Baku, Azerbaijan, 2013; p. 337. [Google Scholar]
- Di Sotto, A.; Checconi, P.; Celestino, I.; Locatelli, M.; Carissimi, S.; De Angelis, M.; Rossi, V.; Limongi, D.; Toniolo, C.; Martinoli, L.; et al. Antiviral and Antioxidant Activity of a Hydroalcoholic Extract from Humulus lupulus L. Oxidative Med. Cell. Longev. 2018, 2018, 5919237. [Google Scholar] [CrossRef]
- Amber, R.; Adnan, M.; Tariq, A.; Mussarat, S. A review on antiviral activity of the Himalayan medicinal plants traditionally used to treat bronchitis and related symptoms. J. Pharm. Pharmacol. 2017, 69, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Rajbhandari, M.; Mentel, R.; Jha, P.K.; Chaudhary, R.P.; Bhattarai, S.; Gewali, M.B.; Karmacharya, N.; Hipper, M.; Lindequist, U. Antiviral activity of some plants used in Nepalese traditional medicine. Evid. Based Complement. Altern. Med. 2009, 6, 517–522. [Google Scholar] [CrossRef]
- Akram, M.; Tahir, I.M.; Shah, S.M.A.; Mahmood, Z.; Altaf, A.; Ahmad, K.; Munir, N.; Daniyal, M.; Nasir, S.; Mehboob, H. Antiviral potential of medicinal plants against HIV, HSV, influenza, hepatitis, and coxsackievirus: A systematic review. Phytother. Res. 2018, 32, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Li, R.-S.; Chen, C.; Zhang, H.-Q.; Guo, H.-Y.; Wang, H.; Wang, L.; Zhang, X.; Hua, S.-N.; Yu, J.; Xiao, P.-G. Identification of natural compounds with antiviral activities against SARS-associated coronavirus. Antivir. Res. 2005, 67, 18–23. [Google Scholar] [CrossRef]
- Speranza, J.; Miceli, N.; Taviano, M.F.; Ragusa, S.; Kwiecień, I.; Szopa, A.; Ekiert, H.M. Isatis tinctoria L. (Woad): A Review of its botany, ethnobotanical uses, phytochemistry, biological activities, and biotechnological studies. Plants 2020, 9, 298. [Google Scholar] [CrossRef]
- Li, W.; Moore, M.J.; Vasilieva, N.; Sui, J.; Wong, S.K.; Berne, M.A.; Somasundaran, M.; Sullivan, J.L.; Luzuriaga, K.; Greenough, T.C.; et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 2003, 426, 450–454. [Google Scholar] [CrossRef]
- Bais, S.; Gill, N.S.; Rana, N.; Shandil, S. A phytopharmacological review on a medicinal Plant: Juniperus communis. Int. Sch. Res. Not. 2014, 2014, 634723. [Google Scholar] [CrossRef]
- Gong, S.J.; Su, X.J.; Yu, H.P.; Li, J.; Qin, Y.J.; Xu, Q.; Luo, W.-S. A study on anti-SARS-CoV 3CL protein of flavonoids from litchi chinensis sonn core. Chin. Pharmacol. Bull. 2008, 24, 699–700. [Google Scholar]
- Jo, S.; Kim, S.; Shin, D.H.; Kim, M.-S. Inhibition of SARS-CoV 3CL protease by flavonoids. J. Enzym. Inhib. Med. Chem. 2020, 35, 145–151. [Google Scholar] [CrossRef]
- Nimmanpipug, P.; Lee, V.S.; Wolschann, P.; Hannongbua, S. Litchi chinensis-derived terpenoid as anti-HIV-1 protease agent: Structural design from molecular dynamics simulations. Molecular Simulation Mol. Simul. 2009, 35, 673–680. [Google Scholar] [CrossRef]
- Wu, Q.; Yu, C.; Yan, Y.; Chen, J.; Zhang, C.; Wen, X. Antiviral flavonoids from Mosla scabra. Fitoterapia 2010, 81, 429–433. [Google Scholar] [CrossRef]
- Wu, Q.; Wang, W.; Dai, X.-Y.; Wang, Z.-Y.; Shen, Z.-H.; Ying, H.-Z.; Yu, C.-H. Chemical compositions and anti-influenza activities of essential oils from Mosla dianthera. J. Ethnopharmacol. 2012, 139, 668–671. [Google Scholar] [CrossRef]
- Mahboubi, M. Natural therapeutic approach of Nigella sativa (Black seed) fixed oil in management of sinusitis. Integr. Med. Res. 2018, 7, 27–32. [Google Scholar] [CrossRef]
- Mohamed, S.; Hossain, M.S. Protective effect of black seed oil from Nigella sativa against murine cytomegalovirus infection. Int. J. Immunopharmacol. 2000, 22, 729–740. [Google Scholar] [CrossRef]
- Ahmad, A.; Rehman, M.U.; Lkharfy, K.M. An alternative approach to minimize the risk of coronavirus (Covid-19) and similar infections. Eur. Rev. Med Pharmacol. Sci. 2020, 24, 4030–4034. [Google Scholar] [CrossRef]
- Molla, S.; Azad, A.K.; Hasib, A.A.A.; Hossain, M.M.; Ahammed, S.; Rana, S.; Islam, M.T. A review on antiviral effects of Nigella sativa L. Pharmacologyonline 2019, 2, 47–53. [Google Scholar]
- Yoon, T.J.; Hur, J.W.; Cho, E.H.; Lee, B.K.; Lee, U. The enhanced effect of Oplopanax elatus Nakai on the immune system and antitumor activity. Korean J. Food Nutr. 2013, 26, 375–382. [Google Scholar] [CrossRef]
- Shikov, A.N.; Pozharitskaya, O.N.; Makarov, V.G.; Yang, W.; Guo, D.-A. Oplopanax elatus (Nakai) Nakai: Chemistry, traditional use and pharmacology. Chin. J. Nat. Med. 2014, 12, 721–729. [Google Scholar] [CrossRef]
- Agayeva, N.A.; Rafiyeva, S.R.; Shiraliyeva, G.S.; Ibadullayeva, S.J. Antimicrobe characteristics of essential oil of the Origanum vulgare L. Int. J. Curr. Microbiol. Appl. Sci. (IJCMAS) 2017, 6, 019–027. [Google Scholar] [CrossRef]
- Blank, D.E.; Hübner, S.D.O.; Alves, G.H.; Cardoso, C.A.L.; Freitag, R.A.; Cleff, M.B. Chemical composition and antiviral effect of extracts of Origanum vulgare. Adv. Biosci. Biotechnol. 2019, 10, 188–196. [Google Scholar] [CrossRef]
- Santoyo, S.; Jaime, L.; García-Risco, M.R.; Ruiz-Rodríguez, A.; Reglero, G. Antiviral Properties of Supercritical CO2 Extracts from Oregano and Sage. Int. J. Food Prop. 2014, 17, 1150–1161. [Google Scholar] [CrossRef]
- Careddu, D.; Pettenazzo, A. Pelargonium sidoides extract EPs 7630: A review of its clinical efficacy and safety for treating acute respiratory tract infections in children. Int. J. Gen. Med. 2018, 11, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Chiang, L.; Chiang, W.; Chang, M.; Ng, L.; Lin, C.-C. Antiviral activity of Plantago major extracts and related compounds in vitro. Antivir. Res. 2002, 55, 53–62. [Google Scholar] [CrossRef]
- Chiang, L.-C.; Chiang, W.; Chang, M.-Y.; Lin, C.-C. In vitro cytotoxic, antiviral and immunomodulatory effects of Plantago major and Plantago asiatica. Am. J. Chin. Med. 2003, 31, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Moradi, M.-T.; Karimi, A.; Shahrani, M.; Hashemi, L.; Ghaffari-Goosheh, M.-S. Anti-influenza virus activity and phenolic content of pomegranate (Punica granatum L.) peel extract and fractions. Avicenna J. Med Biotechnol. 2019, 11, 285–291. [Google Scholar] [PubMed]
- Shin, H.-Y. Coronavirus Replication Inhibition by Herbal. Ph.D. Thesis, Ajou University, Suwon, Korea, 2007. [Google Scholar]
- Lee, J.-H.; Oh, M.; Seok, J.H.; Kim, S.; Lee, D.B.; Bae, G.; Bae, H.-I.; Bae, S.Y.; Hong, Y.-M.; Kwon, S.-O.; et al. Antiviral effects of black raspberry (Rubus coreanus) seed and its gallic acid against influenza virus infection. Viruses 2016, 8, 157. [Google Scholar] [CrossRef] [PubMed]
- Oh, M.; Bae, S.Y.; Lee, J.-H.; Cho, K.J.; Kim, K.H.; Chung, M.S. Antiviral effects of black raspberry (Rubus coreanus) juice on foodborne viral surrogates. Foodborne Pathog. Dis. 2012, 9, 915–921. [Google Scholar] [CrossRef]
- Parsania, M.; Rezaee, M.B.; Monavari, S.H.; Jaimand, K.; Mousavi Jazayeri, S.M.; Razazian, M.; Nadjarha, M.H. Evaluation of antiviral effects of sumac (Rhus coriaria L.) fruit extract on acyclovir resistant Herpes simplex virus type 1. Med. Sci. 2017, 27, 1–8. [Google Scholar]
- AbouReidah, I.; Jamous, R.; Shtayeh, M. Phytochemistry, pharmacological properties and industrial applications of Rhus coriaria L. Jordan J. Biol. Sci. 2014, 7, 233–244. [Google Scholar]
- Agayeva, E.; Ibadullaeva, S.; Movsumova, N.; Mammadova, R.; Abbasova, V.; Ganbarly, I. Screening of microbicidal activity of some plants of the azerbaijan flora in relation to antibiotic-resistant microorganisms. IOSR J. Pharm. Biol. Sci. 2020, 15, 33–36. [Google Scholar] [CrossRef]
- Mani, J.S.; Johnson, J.B.; Steel, J.C.; Broszczak, D.A.; Neilsen, P.M.; Walsh, K.B.; Naiker, M. Natural product-derived phytochemicals as potential agents against coronaviruses: A review. Virus Res. 2020, 284, 197989. [Google Scholar] [CrossRef]
- Mármol, I.; De Diego, C.S.; Jiménez-Moreno, N.; Azpilicueta, C.A.; Rodríguez-Yoldi, M.J. Therapeutic applications of rose hips from different rosa species. Int. J. Mol. Sci. 2017, 18, 1137. [Google Scholar] [CrossRef]
- Modarressi, M.H.; Namazi, R.; Sadat, S.M.; Zabihollahi, R.; Aghasadeghi, M.R.; Esfahani, A.F. The in vitro antiviral potential of Setarud (IMOD™), a commercial herbal medicine with protective activity against acquired immune deficiency syndrome in clinical trials. Indian J. Pharmacol. 2012, 44, 448–453. [Google Scholar] [CrossRef]
- Loizzo, M.R.; Saab, A.M.; Tundis, R.; Statti, G.A.; Menichini, F.; Lampronti, I.; Gambari, R.; Cinatl, J.; Doerr, H.W. Phytochemical analysis and in vitro antiviral activities of the essential oils of seven Lebanon species. Chem. Biodivers. 2008, 5, 461–470. [Google Scholar] [CrossRef]
- Porter, R.S.; Bode, R.F. A review of the antiviral properties of black elder (Sambucus nigra L.) products. Phytother. Res. 2017, 31, 533–554. [Google Scholar] [CrossRef]
- Khan, T.; Khan, M.A.; Mashwani, Z.; Ullah, N.; Nadhman, A. Therapeutic potential of medicinal plants against COVID-19: The role of antiviral medicinal metabolites. Biocatal. Agric. Biotechnol. 2021, 31, 101890. [Google Scholar] [CrossRef]
- Yu, M.-S.; Lee, J.; Lee, J.M.; Kim, Y.; Chin, Y.-W.; Jee, J.-G.; Keum, Y.-S.; Jeong, Y.-J. Identification of myricetin and scutellarein as novel chemical inhibitors of the SARS coronavirus helicase, nsP13. Bioorganic Med. Chem. Lett. 2012, 22, 4049–4054. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Tang, H.; Xie, L.; Zheng, Y.; Ma, Z.; Sun, Q.; Li, X. Scutellaria baicalensis Georgi. (Lamiaceae): A review of its traditional uses, botany, phytochemistry, pharmacology and toxicology. J. Pharm. Pharmacol. 2019, 71, 1353–1369. [Google Scholar] [CrossRef]
- Galani, V.J.; Patel, B.G.; Rana, D.G. Sphaeranthus indicus Linn.: A phytopharmacological review. Int. J. Ayurveda Res. 2010, 1, 247–253. [Google Scholar] [CrossRef]
- Mohammadi, N.; Shaghaghi, N. Inhibitory Effect of Eight Secondary Metabolites from Conventional Medicinal Plants on COVID_19 Virus Protease by Molecular Docking Analysis. ChemRxiv. Preprint. 2020. [Google Scholar] [CrossRef]
- Liu, T.; Liu, X.; Li, W. Tetrandrine, a Chinese plant-derived alkaloid, is a potential candidate for cancer chemotherapy. Oncotarget 2016, 7, 40800–40815. [Google Scholar] [CrossRef]
- Kim, D.E.; Min, J.S.; Jang, M.S.; Lee, J.Y.; Shin, Y.S.; Park, C.M.; Song, J.H.; Kim, H.R.; Kim, S.; Jin, Y.-H.; et al. Natural bis-benzylisoquinoline alkaloids-tetrandrine, fangchinoline, and cepharanthine, inhibit human coronavirus OC43 infection of MRC-5 Human Lung Cells. Biomolecules 2019, 9, 696. [Google Scholar] [CrossRef]
- Tsai, Y.-C.; Lee, C.-L.; Yen, H.-R.; Chang, Y.-S.; Lin, Y.-P.; Huang, S.-H.; Lin, C.-W. Antiviral action of tryptanthrin isolated from Strobilanthes cusia leaf against human coronavirus NL63. Biomolecules 2020, 10, 366. [Google Scholar] [CrossRef]
- Gu, W.; Wang, W.; Li, X.-N.; Zhang, Y.; Wang, L.-P.; Yuan, C.; Huang, L.; Hao, X.-J. A novel isocoumarin with anti-influenza virus activity from Strobilanthes cusia. Fitoterapia 2015, 107, 60–62. [Google Scholar] [CrossRef]
- Jiménez-González, F.J.; Veloza, L.A.; Sepúlveda-Arias, J.C. Anti-infectious activity in plants of the genus Tabebuia. Univ. Sci. 2013, 18, 257–267. [Google Scholar] [CrossRef]
- Nepomuceno, J.C. Lapachol and its derivatives as potential drugs for cancer treatment. In Plants and Crop the Biology and Biotechnology Research, 1st ed.; Chapter: Lapachol and its derivatives as potential drugs for cancer treatment; iConcept Press Ltd.: Hong Kong, China, 2014. [Google Scholar]
- Naser, B.; Bodinet, C.; Tegtmeier, M.; Lindequist, U. Thuja occidentalis (Arbor vitae): A review of its pharmaceutical, pharmacological and clinical properties. Evid. Based Complementary Altern. Med. 2005, 2, 69–78. [Google Scholar] [CrossRef]
- Kumaki, Y.; Wandersee, M.K.; Smith, A.J.; Zhou, Y.; Simmons, G.; Nelson, N.M.; Bailey, K.W.; Vest, Z.G.; Li, J.K.-K.; Chan, P.K.-S.; et al. Inhibition of severe acute respiratory syndrome coronavirus replication in a lethal SARS-CoV BALB/c mouse model by stinging nettle lectin, Urtica dioica agglutinin. Antivir. Res. 2011, 90, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Altun, M.L.; Çitoğlu, G.S.; Yilmaz, B.S.; Özbek, H. Antinociceptive and anti-inflammatory activities of Viburnum opulus. Pharm. Biol. 2009, 47, 653–658. [Google Scholar] [CrossRef]
- Vimalanathan, S.; Ignacimuthu, S.; Hudson, J.B. Medicinal plants of Tamil Nadu (Southern India) are a rich source of antiviral activities. Pharm. Biol. 2009, 47, 422–429. [Google Scholar] [CrossRef]
- Chang, J.S.; Wang, K.C.; Yeh, C.F.; Shieh, D.E.; Chiang, L.C. Fresh ginger (Zingiber officinale) has antiviral activity against human respiratory syncytial virus in human respiratory tract cell lines. J. Ethnopharmacol. 2013, 145, 146–151. [Google Scholar] [CrossRef]
- Hong, E.-H.; Song, J.H.; Bin Kang, K.; Sung, S.H.; Ko, H.-J.; Yang, H. Anti-influenza activity of betulinic acid from Zizyphus jujuba on Influenza A/PR/8 Virus. Biomol. Ther. 2015, 23, 345–349. [Google Scholar] [CrossRef]
- Kim, E.B.; Kwak, J.H. Antiviral phenolic compounds from the whole plants of Zostera marina against influenza A virus. Planta Medica 2015, 81, 1494. [Google Scholar] [CrossRef]
- Al-Ansary, L.A.; Bawazeer, G.A.; Beller, E.; Clark, J.; Conly, J.; Del Mar, C.; Dooley, E.; Ferroni, E.; Glasziou, P.; Hoffman, T.; et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Part 2—Hand hygiene and other hygiene measures: Systematic review and meta-analysis. MedRxiv 2020. [Google Scholar] [CrossRef]
- Lin, L.-T.; Hsu, W.-C.; Lin, C.-C. Antiviral natural products and herbal medicines. J. Tradit. Complement. Med. 2014, 4, 24–35. [Google Scholar] [CrossRef]
- Huang, J.; Wu, L.; Ren, X.; Wu, X.; Chen, Y.; Ran, G.; Huang, A.; Huang, L.; Zhong, D. Traditional Chinese medicine for corona virus disease 2019: A protocol for systematic review. Medicine 2020, 99, e21774. [Google Scholar] [CrossRef]
- Yang, R.; Liu, H.; Bai, C.; Wang, Y.; Zhang, X.; Guo, R.; Wu, S.; Wang, J.; Leung, E.; Chang, H.; et al. Chemical composition and pharmacological mechanism of Qingfei Paidu Decoction and Ma Xing Shi Gan Decoction against Coronavirus Disease 2019 (COVID-19): In silico and experimental study. Pharmacol. Res. 2020, 157, 104820. [Google Scholar] [CrossRef]
- Khailany, R.A.; Safdar, M.; Ozaslan, M. Genomic characterization of a novel SARS-CoV-2. Gene Rep. 2020, 19, 100682. [Google Scholar] [CrossRef] [PubMed]
- Arunkumar, G.; Mudgal, P.P.; Maity, H.; Dowarha, D.; Devadiga, S.; Nag, S.; Arunkumar, G. Herbal plants and plant preparations as remedial approach for viral diseases. Virus 2015, 26, 225–236. [Google Scholar] [CrossRef]
- Williamson, E.M.; Liu, X.; Izzo, A.A. Trends in use, pharmacology, and clinical applications of emerging herbal nutraceuticals. Br. J. Pharmacol. 2020, 177, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Islam, T.; Sarkar, C.; El-Kersh, D.M.; Jamaddar, S.; Uddin, S.J.; Shilpi, J.A.; Mubarak, M.S. Natural products and their derivatives against coronavirus: A review of the non-clinical and pre-clinical data. Phytother. Res. 2020, 34, 2471–2492. [Google Scholar] [CrossRef] [PubMed]
- Ložienė, K.; Švedienė, J.; Paškevičius, A.; Raudoniene, V.; Sytar, O.; Kosyan, A. Influence of plant origin natural α-pinene with different enantiomeric composition on bacteria, yeasts and fungi. Fitoterapia 2018, 127, 20–24. [Google Scholar] [CrossRef]
- Schwarz, S.; Sauter, D.; Wang, K.; Zhang, R.; Sun, B.; Karioti, A.; Bilia, A.R.; Efferth, T.; Schwarz, W. Kaempferol derivatives as antiviral drugs against the 3a channel protein of coronavirus. Planta Medica 2014, 80, 177–182. [Google Scholar] [CrossRef]
- Roviello, V.; Roviello, G.N. Lower COVID-19 mortality in Italian forested areas suggests immunoprotection by Mediterranean plants. Environ. Chem. Lett. 2020, 1–12. [Google Scholar] [CrossRef]
- Song, J.-W.; Long, J.-Y.; Xie, L.; Zhang, L.-L.; Xie, Q.-X.; Chen, H.-J.; Deng, M.; Li, X. Applications, phytochemistry, pharmacological effects, pharmacokinetics, toxicity of Scutellaria baicalensis Georgi. and its probably potential therapeutic effects on COVID-19: A review. Chin. Med. 2020, 15, 1–26. [Google Scholar] [CrossRef]
- Sytar, O.; Švedienė, J.; Ložienė, K.; Paškevičius, A.; Kosyan, A.; Taran, N. Antifungal properties of hypericin, hypericin tetrasulphonic acid and fagopyrin on pathogenic fungi and spoilage yeasts. Pharm. Biol. 2016, 54, 3121–3125. [Google Scholar] [CrossRef]
- Morán-Santibañez, K.; Peña-Hernández, M.A.; Cruz-Suarez, L.E.; Ricque-Marie, D.; Skouta, R.; Vasquez, A.H.; Rodríguez-Padilla, M.C.; Trejo-Avila, L.M. Virucidal and synergistic activity of polyphenol-rich extracts of seaweeds against measles virus. Viruses 2018, 10, 465. [Google Scholar] [CrossRef]
- Salehi, B.; Iriti, M.; Vitalini, S.; Antolak, H.; Pawlikowska, E.; Kręgiel, D.; Sharifi-Rad, J.; Oyeleye, S.I.; Ademiluyi, A.O.; Czopek, K.; et al. Euphorbia-Derived Natural Products with Potential for Use in Health Maintenance. Biomolecules 2019, 9, 337. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Chen, X.; Li, Y.; Guo, S.; Wang, Z.; Yu, X. Advances in Pharmacological Activities of Terpenoids. Nat. Prod. Commun. 2020, 15. [Google Scholar] [CrossRef]
- Cheng, P.-W.; Ng, L.-T.; Chiang, L.-C.; Lin, C.-C. Antiviral effects of saikosaponins on human coronavirus 229E in vitro. Clin. Exp. Pharmacol. Physiol. 2006, 33, 612–616. [Google Scholar] [CrossRef]
- Azuma, C.M.; Dos Santos, F.C.S.; Lago, J.H. Flavonoids and fatty acids of Camellia japonica leaves extract. Rev. Bras. Farmacogn. 2011, 21, 1159–1162. [Google Scholar] [CrossRef]
- Itokawa, H.; Nakajima, H.; Ikuta, A.; Iitaka, Y. Two triterpenes from the flowers of Camellia japonica. Phytochemistry 1981, 20, 2539–2542. [Google Scholar] [CrossRef]
- Kato, M.; Hiroshi, A. Biosynthesis and catabolism of purine alkaloids in camellia plants. Nat. Prod. Commun. 2008, 3, 1429–1435. [Google Scholar] [CrossRef]
- Pompei, R.; Flore, O.; Marccialis, M.A.; Pani, A.; Loddo, B. Glycyrrhizic acid inhibits virus growth and inactivates virus particles. Nature 1979, 281, 689–690. [Google Scholar] [CrossRef]
- Munir, O.; Ernaz, A.; Ibadullayeva, S.J.; Altay, V.; Aslanipour, B. A comparative analysis of medicinal and aromatic plants in the traditional medicine of İgdir (Turkey), Nakhchivan (Azerbaijan) and Tabriz (İran). Pak. J. Bot. 2018, 50, 337–343. [Google Scholar]
- van de Sand, L.; Bormann, M.; Alt, M.; Schipper, L.; Heilingloh, C.S.; Todt, D.; Dittmer, U.; Elsner, C.; Witzke, O.; Krawczyk, A. Glycyrrhizin effectively neutralizes SARS-CoV-2 in vitro by inhibiting the viral main protease. bioRxiv 2020, 423104. [Google Scholar] [CrossRef]
- Park, J.-Y.; Ko, J.-A.; Kim, D.W.; Kim, Y.M.; Kwon, H.-J.; Jeong, H.J.; Kim, C.Y.; Park, K.; Lee, W.S.; Ryu, Y.B. Chalcones isolated from Angelicakeiskei inhibit cysteine proteases of SARS-CoV. J. Enzym. Inhib. Med. Chem. 2016, 31, 23–30. [Google Scholar] [CrossRef]
- Bailly, C.; Vergoten, G. Glycyrrhizin: An alternative drug for the treatment of COVID-19 infection and the associated respiratory syndrome? Pharmacol. Ther. 2020, 214, 107618. [Google Scholar] [CrossRef] [PubMed]
- da Silva, J.K.R.; Figueiredo, P.L.; Byler, K.G.; Setzer, W.N. Essential oils as antiviral agents, potential of essential oils to treat SARS-CoV-2 infection: An in-silico investigation. Int. J. Mol. Sci. 2020, 21, 3426. [Google Scholar] [CrossRef] [PubMed]
- Andre, C.M.; Hausman, J.-F.; Guerriero, G. Cannabis sativa: The Plant of the Thousand and One Molecules. Front. Plant Sci. 2016, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Campos, A.C.; Moreira, F.A.; Gomes, F.V.; Del Bel, E.A.; Guimarães, F.S. Multiple mechanisms involved in the large-spectrum therapeutic potential of cannabidiol in psychiatric disorders. Philosophical Transactions of the Royal Society of London. Philos. Trans. R. Soc. B Biol. Sci. 2012, 367, 3364–3378. [Google Scholar] [CrossRef] [PubMed]
- Mabou Tagne, A.; Pacchetti, B.; Sodergren, M.; Cosentino, M.; Marino, F. Cannabidiol for Viral Diseases: Hype or Hope? Cannabis Cannabinoid Res. 2020, 5, 121–131. [Google Scholar] [CrossRef]
- de ASilva, J.R.; Geone, M.C.; Carvalho, R.; Renyer, A.C.; Pinheiro, M.L.B.; Araujo Lídia, M.; Amaral Ana Claudia, F. Analyses of Ampelozizyphus amazonicus, a plant used in folk medicine of the Amazon Region. Pharmacogn. Mag. 2009, 5, 75–80. [Google Scholar]
- Kapepula, P.M.; Kabengele, J.K.; Kingombe, M.; Van Bambeke, F.; Tulkens, P.M.; Sadiki Kishabongo, A.; Decloedt, E.; Zumla, A.; Tiberi, S.; Suleman, F.; et al. Artemisia spp. Derivatives for COVID-19 Treatment: Anecdotal Use, Political Hype, Treatment Potential, Challenges, and Road Map to Randomized Clinical Trials. Am. J. Trop. Med. Hyg. 2020, 103, 960–964. [Google Scholar] [CrossRef]
- Layne, T.H.; Roach, J.S.; Tinto, W.F. Review of β-carboline alkaloids from the genus Aspidosperma. Nat. Prod. Commun. 2015, 10, 183–186. [Google Scholar] [CrossRef]
- Hudson, J.; Lee, M.; Rasoanaivo, P. Antiviral activities in plants endemic to madagascar. Pharm. Biol. 2000, 38, 36–39. [Google Scholar] [CrossRef]
- Qing, Z.-X.; Yang, P.; Tang, Q.; Cheng, P.; Liu, X.-B.; Zheng, Y.-J.; Liu, Y.-S.; Zeng, J. Isoquinoline alkaloids and their antiviral, antibacterial, and antifungal activities and structure-activity relationship. Curr. Org. Chem. 2017, 21, 1920–1934. [Google Scholar] [CrossRef]
- Jahan, I.; Onay, A. Potentials of plant-based substance to inhabit and probable cure for the COVID-19. Turk. J. Biol. 2020, 44, 228–241. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Prasad, S.K.; Hemalatha, S. A current update on the phytopharmacological aspects of Houttuynia cordata Thunb. Pharmacogn. Rev. 2014, 8, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Kovalchuk, A.; Li, D.; Ilnytskyy, Y.; Kovalchuk, I.; Kovalchuk, O. In Search of Preventative Strategies: Novel Anti-Inflammatory High-CBD Cannabis Sativa Extracts Modulate ACE2 Expression in COVID-19 Gateway Tissues. Preprints 2020. [Google Scholar] [CrossRef]
- Weng, J.K. Plant solutions for the COVID-19 pandemic and beyond: Historical reflections and future perspectives. Mol. Plant 2020, 13, 803–807. [Google Scholar] [CrossRef] [PubMed]
- Bieski, I.G.C.; Leonti, M.; Arnason, J.T.; Ferrier, J.; Rapinski, M.; Violante, I.M.P.; Balogun, S.O.; Pereira, J.F.C.A.; Figueiredo, R.D.C.F.; Lopes, C.R.A.S.; et al. Ethnobotanical study of medicinal plants by population of Valley of Juruena Region, Legal Amazon, Mato Grosso, Brazil. J. Ethnopharmacol. 2015, 173, 383–423. [Google Scholar] [CrossRef]
- van Eck, N.J.; Ludo, W. Citation-based clustering of publications using CitNetExplorer and VOSviewer. Scientometrics 2017, 111, 1053–1070. [Google Scholar] [CrossRef]
- Sweileh, W.M.; Al-Jabi, S.W.; Zyoud, S.H.; Sawalha, A.F.; Abu-Taha, A.S. Global research output in antimicrobial resistance among uropathogens: A bibliometric analysis (2002–2016). J. Glob. Antimicrob. Resist. 2018, 13, 104–114. [Google Scholar] [CrossRef]
- Soosaraei, M.; Khasseh, A.A.; Fakhar, M.; Hezarjaribi, H.Z. A decade bibliometric analysis of global research on leishmaniasis in Web of Science database. Ann. Med. Surg. 2018, 26, 30–37. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Mocan, A.; Atanasov, A.G. Let food be thy medicine and medicine be thy food: A bibliometric analysis of the most cited papers focusing on nutraceuticals and functional foods. Food Chem. 2018, 269, 455–465. [Google Scholar] [CrossRef]
- World Health Organization. Chikungunya Fact Sheet. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/chikungunya (accessed on 9 January 2020).
- Sharma, V.; Kaushik, S.; Pandit, P.; Dhull, D.; Yadav, J.P.; Kaushik, S. Green synthesis of silver nanoparticles from medicinal plants and evaluation of their antiviral potential against chikungunya virus. Appl. Microbiol. Biotechnol. 2019, 103, 881–891. [Google Scholar] [CrossRef]
- Gurib-Fakim, A. Medicinal plants: Traditions of yesterday and drugs of tomorrow. Mol. Asp. Med. 2006, 27, 1–93. [Google Scholar] [CrossRef] [PubMed]
- Lopez, V. Are traditional medicinal plants and ethnobotany still valuable approaches in pharmaceutical research. Boletín Latinoam. y Del Caribe de Plantas Med. y Aromáticas 2011, 10, 3–10. [Google Scholar]
| Plant Species | Family | Plant Part | Origin Native Area | Mode of Action Pharmaceutical Activity | Reference |
|---|---|---|---|---|---|
| Acacia nilotica | Fabaceae | Whole plant | Africa and Middle East, Indian subcontinent | Inhibits human immunodeficiency virus (HIV) protease; antiviral and cytotoxic | [6,29] |
| Alhagi maurorum | Fabaceae | Gum tragacanth | South-east Europe, south-west Asia | Inhibits influenza and cold viruses; relieves cough, pectoral aches, fever, vomiting and thirst | [30] |
| Allium sativum | Alliaceae | Bulb | Central Asia, Iran | Inhibits avian coronavirus; antiviral, fungistatic | [31,32] |
| Althaea officinalis | Malvaceae | Whole plant | Western palearctic, boreal area, Europe, Asia and Africa | Anti-inflammatory in diseases of the upper respiratory tract; antitussive, chest emollient, immuno-modulator, antiviral | [33,34,35] |
| Ampelozizyphus amazonicus | Rhamnaceae | Whole plant | South America | Immunomodulation, anti-inflammatory | [36] |
| Andrographis paniculata | Acanthaceae | Leaves | India, Sri Lanka | Antiviral | [6,37] |
| Anthemis hyalina | Asteraceae | Whole plant | Mediterranean region, south-west Asia to Iran | Inhibits coronavirus replication and expression of transient receptor potential gene family | [38] |
| Arrabidaea samydoides | Bignoniaceae | Whole plant | South America | Antiviral activity against human herpes simplex virus-1 (HSV-1), vaccinia virus and murine encephalomyocarditis virus | [39] |
| Artemisia sp. (Artemisia absinthium) | Asteraceae | Whole plant | Eurasia, north Africa, North America | Reduces coronavirus replication; antibacterial, anti-inflammatory | [40,41] |
| Aspidosperma sp. | Apocynaceae | Whole plant | South America | Antiviral activity against avian metapneumovirus and other groups | [42,43] |
| Bryophyllum pinnatum | Crassulaceae | Whole plant | Madagascar | Anti-inflammatory immunomodulator; induces production of host antiviral agents; prescribed for polio and enteroviruses | [33,44] |
| Camellia japonica | Theaceae | Whole plant, Flowers | East Asia | High antiviral activity on porcine epidemic diarrhea virus (PEDV) of coronavirus family; inhibitory effects on key gene and protein syntheses during PEDV replication | [45,46] |
| Cichorium intybus | Asteraceae | Whole plant, Roots | Eurasia, Mediterranean region | Immunomodulation; antiviral activity against HSV-1 and adenovirus type 5 | [37,47] |
| Cinnamomum cassia | Lauraceae | Bark | Vietnam and eastern Himalayas, China | Antiviral, anti-inflammatory; inhibits attachment of human respiratory syncytial virus | [48,49,50] |
| Citrus trifoliata | Rutaceae | Seeds | Northern China and Korea | Antiviral against oseltamivir-resistant influenza virus | [51] |
| Clitoria ternatea | Fabaceae | Whole plant | Indian sub-continent, Southeast Asia | Antiviral | [6] |
| Cynara scolymus | Asteraceae | Flower heads | Mediterranean region | ACE inhibitor, antiviral | [6,52] |
| Desmodium canadense | Fabaceae | Whole plant | North America | High antiviral activity towards coronaviruses | [53] |
| Echinacea angustifolia | Asteraceae | Flowers | North America | Antiviral activity against cold and flu viruses; inhibits viral growth and secretion of pro-inflammatory cytokines. | [54] |
| Echinops sp. | Asteraceae | Trehala manna | Iran | Antiviral, cough suppressant | [55] |
| Echium amoenum | Boraginaceae | Flowers | Iran, Caucasus, Russia | Antiviral | [56,57] |
| Euphorbia sp. | Euphorbiaceae | Roots | Southern Africa and Madagascar, North and South America, Mediterranean region | Antiviral activity against HIV-1, HIV-2, HSV-2 and SIVmac251 | [35,58,59] |
| Ferula assa-foetida | Apiaceae | Oleo-Gum-resin | Iran, Afghanistan | Antiviral activity; great potency against H1N1; anti-inflammatory | [60,61] |
| Firmiana simplex | Malvaceae | Leaves | South Japan, China and Indonesia | Immunomodulation; general tonic and adaptogenic drug | [33] |
| Glycyrrhiza glabra | Fabaceae | Roots | Mediterranean area, Iran-Turan, Azerbaijan | Immunomodulation; antiviral activity against HSV-1, Epstein–Barr virus, human cytomegalo-virus, and RNA viruses such as influenza A, H5N1, and H1N1 | [35,62,63,64] |
| Gymnema sylvestre | Apocynaceae | Leaves, Whole plant | Asia, Africa, Australia | Inhibition of viral DNA synthesis; immunomodulation | [6,65] |
| Hippophae rhamnoides | Elaeagnaceae | Fruits | Cold-temperate regions of Europe and Asia | Anti-influenza activities against influenza A/Victoria virus and B | Immunomodulation | [66,67,68] |
| Houttuynia cordata | Saururaceae | Whole plant | Southern Asia | Inhibits viral SARS-3CLpro and tRNA polymerase activity (RdRp); stimulates secretion of IL-2 and IL-10 | [69] |
| Humulus lupulus | Cannabaceae | Inflorescences | Europe, western Asia, North America | Immunomodulation; antiviral activity against influenza and cold viruses, hepatitis C, and herpesvirus; inhibits viral replication | [70,71,72] |
| Hyoscyamus niger | Solanaceae | Whole plant | Continental Europe, Asia, Middle East | Viral inhibition; bronchodilator; antiviral effect against human influenza virus A/WSN/33 | [6,73,74] |
| Hypericum connatum | Hypericaceae | Whole plant | North America, eastern Asia | High antiviral activity | [75] |
| Inula helenium | Asteraceae | Rhizomes, Roots | Eastern Europe, Caucasus, western Siberia, Far East and Central Asia | Anti-inflammatory | [71] |
| Isatis tinctoria | Brassicaceae | Roots extracts | Caucasus, Central Asia, eastern Siberia, western Asia | Inhibits cleavage activity of SARS-3CLpro enzyme; high antioxidant potential and anti-inflammatory effects | [76,77] |
| Juniperus communis | Cupressaceae | Fruits | North America, Europe, Asia | Inhibits replication, 3CLpro; anti-inflammatory, antiseptic | [78,79] |
| Litchi chinensis | Sapindaceae | Seeds | Southeastern China | Inhibit SARS-3CLpro; terpenoids inhibit HIV-1 protease | [17,53,80,81,82] |
| Mentha piperita | Lamiaceae | Whole plant | Europe, Middle East | High antiviral activity against coronavirus group | [17] |
| Mosla sp. | Lamiaceae | Whole plant | Eastern and south-eastern Asia, Himalayas | Anti-influenza activity | [83,84] |
| Nigella sativa | Ranunculaceae | Whole plant | Eastern Mediterranean, northern Africa, Indian Subcontinent, western Asia | Immunomodulator, anti-inflammatory agent, and broncho-dilator; antiviral activity against avian influenza virus (H9N2) | [85,86,87,88] |
| Ocimum kilimandscharicum | Lamiaceae | Whole plant | Central Africa, Southeast Asia | Antiviral activity against HIV-1, SARS-CoV-2 | [6,21] |
| Oplopanax elatus | Araliaceae | Whole plant | North America, north-eastern Asia | Immunomodulation and anti-inflammatory activities | [33,89,90] |
| Origanum vulgare | Lamiaceae | Leaves, Stems | Western and south-western Eurasia, Mediterranean region | Respiratory and antiviral activity | [91,92,93] |
| Pelargonium sidoides | Geraniaceae | Leaves, Whole plant | South Africa | Decreases rhinovirus infection via modulation of viral binding proteins on human bronchial epithelial cells | [87,94] |
| Plantago major | Plantaginaceae | Leaves, Whole plant | Europe, Northern and central Asia | Anti-inflammatory; antiviral activity against herpesviruses and adenoviruses | [35,95,96] |
| Punica granatum | Lythraceae | Fruits, Peel, Seeds | Iran to northern India, Mediterranean region | Inhibits viral glycoproteins; antiviral activity against HSV-1 and influenza virus | [6,97] |
| Rhaponticum carthamoides | Asteraceae | Roots | Southern Siberia, Kazakhstan, Altay region | Immunomodulation | [33] |
| Rosmarinus officinalis | Lamiaceae | Whole plant | Mediterranean region | Antiviral activity against human respiratory syncytial virus; immunomodu-lator; anti-inflammatory | [33,98] |
| Rubus sp. | Rosaceae | Fruits, Flowers | Forest-steppe zones of Eurasia | Antiviral effect against human influenza virus | [33,71,99,100] |
| Rhus coriaria | Anacardiaceae | Fruit | Mild Mediterranean climates of southern Europe and western Asia | Antiviral potential | [101,102] |
| Rosa sp. | Rosaceae | Completely matured fruits | Europe, North America, Northwestern Africa | Immunomodulatory effects; antiviral activity against HIV and HSV | [103,104,105,106] |
| Salvia officinalis | Lamiaceae | Whole plant | Mediterranean basin | High binding to COVID-19 proteases; Inhibits SARS-CoV and HSV-1 replication | [21,107] |
| Sambucus nigra | Adoxaceae | Whole plant | Europe and North America | Antiviral activity against HIV, HSV, influenza, hepatitis, and coxsackievirus | [75,108] |
| Saposhnikovia divaricata | Apiaceae | Whole plant | China | High antiviral activity against PEDV corona-virus | [45,109] |
| Scutellaria baicalensis | Lamiaceae | Roots | China, Korea, Mongolia, Russian far east, Siberia | Inhibit nsP13 by affecting the ATPase activity | [110,111] |
| Sphaeranthus indicus | Asteraceae | Whole plant | Northern Australia, Indomalayan realm | Antiviral activity against mouse coronavirus; bronchodilation and anti-inflammatory activities | [6,112] |
| Stachys schtschegleevii | Lamiaceae | Leaves | Iran | Antiviral activity against SARS-CoV-2; anti-inflammatory potential | [113] |
| Stephania tetrandra | Menispermaceae | Roots | China, Taiwan | Inhibits expression of HCoV-OC43 spike and nucleocapsid proteins; immunomodulation and anticancer potential | [114,115] |
| Strobilanthes cusia | Acanthaceae | Leaves, Whole plant | Tropical Asia, Madagascar | Inhibits HCoV-NL63 via tryptanthrin; anti-influenza virus activity; anti-inflammatory potential | [6,116,117] |
| Tabebuia sp. | Bignoniaceae | Whole plant | South America | Antiviral potential | [118,119] |
| Thymus vulgaris | Lamiaceae | Whole plant | Southern Europe | High antiviral activity towards coronaviruses; antioxidant effects | [21,53] |
| Thuja occidentalis | Cupressaceae | Leaves Whole plant | Eastern Canada, north, central and upper north-eastern United States | Immunostimulation; antiviral activity against acute common cold | [120] |
| Urtica dioica | Urticaceae | Leaves | Europe, temperate Asia, and western North Africa | Inhibition of SARS coronavirus replication | [121] |
| Viburnum opulus | Adoxaceae | Fruits | Eastern Europe, Caucasus, western and eastern Siberia and Central Asia | Immunomodulation; anti-inflammatory effects | [33,122] |
| Vitex trifolia | Verbenaceae | Whole plant | Tropical East Africa, French Polynesia | Anti-inflammatory effects on lungs; immunomodulation; strong antiviral activity against HSV and mouse coronavirus (surrogate for human SARS virus) | [6,123] |
| Zingiber officinale | Zingiberaceae | Rhizome | Maritime Southeast Asia | Antiviral activity against human respiratory syncytial virus | [124] |
| Ziziphus jujuba | Rhamnaceae | Fruit | Southeastern Europe to China | Antiviral activity; potential therapeutic agent for treating influenza | [125] |
| Zostera marina | Zosteraceae | Whole plant | North America, Europe, Asia | Antiviral activity against influenza A virus | [126] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sytar, O.; Brestic, M.; Hajihashemi, S.; Skalicky, M.; Kubeš, J.; Lamilla-Tamayo, L.; Ibrahimova, U.; Ibadullayeva, S.; Landi, M. COVID-19 Prophylaxis Efforts Based on Natural Antiviral Plant Extracts and Their Compounds. Molecules 2021, 26, 727. https://doi.org/10.3390/molecules26030727
Sytar O, Brestic M, Hajihashemi S, Skalicky M, Kubeš J, Lamilla-Tamayo L, Ibrahimova U, Ibadullayeva S, Landi M. COVID-19 Prophylaxis Efforts Based on Natural Antiviral Plant Extracts and Their Compounds. Molecules. 2021; 26(3):727. https://doi.org/10.3390/molecules26030727
Chicago/Turabian StyleSytar, Oksana, Marian Brestic, Shokoofeh Hajihashemi, Milan Skalicky, Jan Kubeš, Laura Lamilla-Tamayo, Ulkar Ibrahimova, Sayyara Ibadullayeva, and Marco Landi. 2021. "COVID-19 Prophylaxis Efforts Based on Natural Antiviral Plant Extracts and Their Compounds" Molecules 26, no. 3: 727. https://doi.org/10.3390/molecules26030727
APA StyleSytar, O., Brestic, M., Hajihashemi, S., Skalicky, M., Kubeš, J., Lamilla-Tamayo, L., Ibrahimova, U., Ibadullayeva, S., & Landi, M. (2021). COVID-19 Prophylaxis Efforts Based on Natural Antiviral Plant Extracts and Their Compounds. Molecules, 26(3), 727. https://doi.org/10.3390/molecules26030727












