Carbonic Anhydrase Inhibitors and Epilepsy: State of the Art and Future Perspectives
Abstract
:1. Introduction
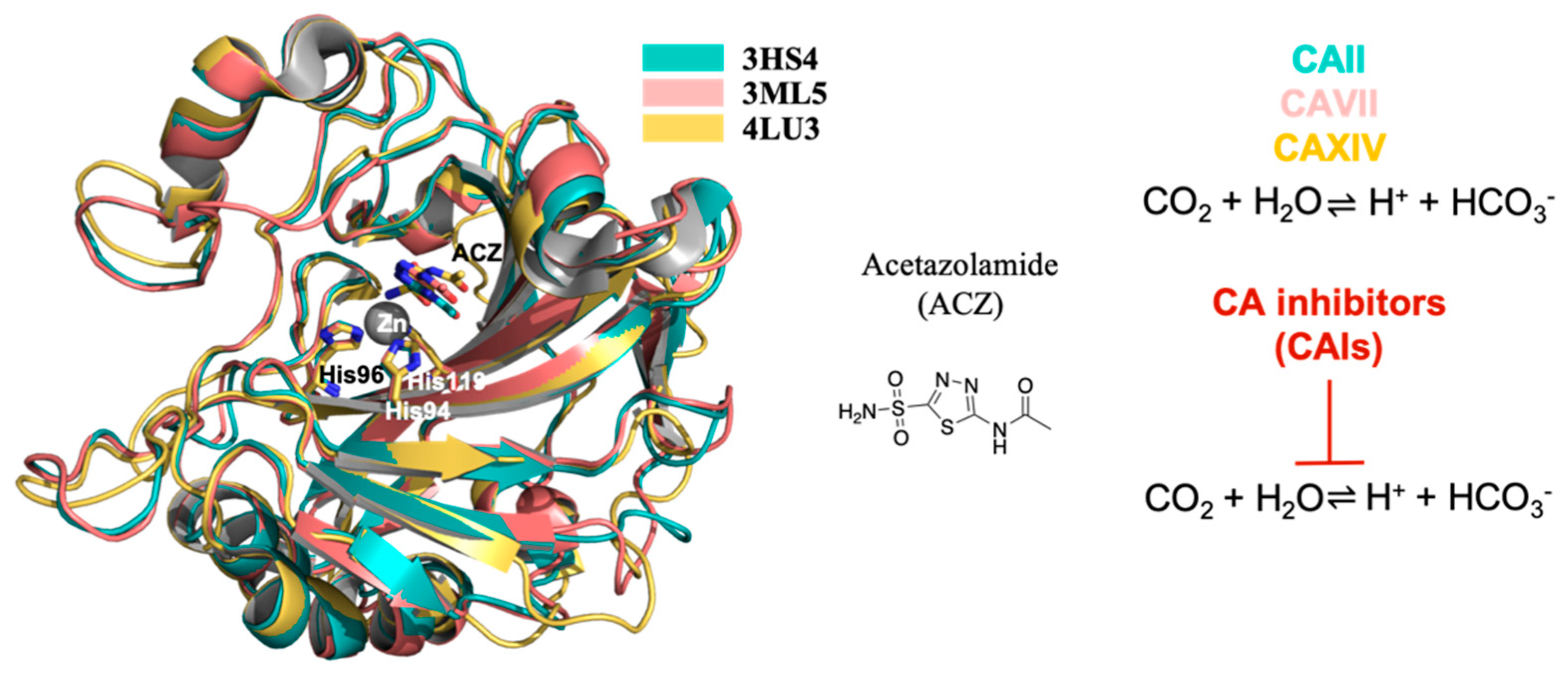
2. Structure of Carbonic Anhydrase (CA): CAII, CAVII and XIV
3. CAs and Their Role in Epilepsy
- (1)
- Seizures are accompanied by pronounced changes in ionic composition in brain compartments and by pH shift that, directly or indirectly, influence the concentration of the chemical species of the reaction catalyzed by CAs.
- (2)
- CAs regulate CO2 tissue concentration, and it has been demonstrated that CO2 has a role in epilepsy. In particular, clinical evidence suggest that the enhancement of CO2 concentration results in better seizure control [50], while low CO2 levels are linked to higher seizure propensity [51]. The inhibition of CAs resulted in increased CO2 concentration and a positive outcome in epilepsy management [9].
- (3)
- It has been clearly shown that alkalosis generally potentiates seizures by increasing neuronal excitability, while acidosis has an opposite effect [52]. Since their role is in the regulation of the CO2/ HCO3− buffer system, CAs are crucially involved in the control of neural excitability [17]. For instance, it has been demonstrated that CA IV and CA XIV play a role in extracellular buffering in response to neural activity [53].
- (4)
- Mitochondrial dysfunction has been identified as one potential cause of epileptic seizures [54]. There is a vicious cycle between mitochondrial dysfunction and epileptic seizures because seizures themselves can induce mitochondrial damage that consequently triggers seizures [54]. It is known that CAs are involved in mitochondria biogenesis and physiology, and in glucose and lipid metabolism in human Sertori cells [55]. In particular, CA V A and CA V B are specifically localized in mitochondria. They hydrate carbon dioxide to yield bicarbonate ions and a proton that contribute to normal mitochondria metabolism. In the nervous system, CA V is expressed in astrocytes as well as in neurons. It has been proposed that CA V in neurons could be involved in the regulation of the intra-mitochondrial Ca2+ levels, thus contributing to the stability of the intracellular calcium concentration preventing neuronal degeneration and cell death [43]. Another possible function of CA V is to participate in the regulation of neuronal HCO3− homeostasis taking part in physiological neuronal function. Moreover, it has been reported that the intracellular regeneration of HCO3− and its elimination from the extracellular environment results in a repolarization in GABA responses, suggesting that CA V might also be involved in neuronal transmission [43,56].
- (5)
- Regulating the kinetics of pH transients [17,57,58]. CAs can influence the function of a broad array of proton-sensitive transmembrane proteins implicated in neuronal signaling such as GABAARs [57,58], N-methyl-D-aspartate (NMDA) receptors [59,60], H+-gated channels [61] and cation channels [62,63]. For example, the activity of excitatory receptors for glutamate, NMDA receptors, is inhibited by extracellular protons [64]. The initial seizure-associated extracellular alkaline shift, apparently influenced by CA activity [53], likely sustains NMDA receptors’ activation during seizures. Moreover, it has been shown that CA XIV, located in close vicinity to the NMDA receptor at the synapses, regulates pH transients in the perisynaptic microenvironment and their impact on NMDA receptors’ activity [60].
- (6)
- It has been shown that glycolysis increases during seizures and that the glycolytic metabolite lactic acid can be used as an energy source [65]. A specific isoform of CAs facilitate lactate transport in astrocytes as well as in neurons [66]. In addition, CAs can intervene in lactic acid-induced acidosis, that seems to be implicated in seizure termination [65,67]. Moreover, CAs provide substrates required for the function of metabolic enzymes involved in epilepsy. For instance, a failure in pyruvate carboxylase (PC) function may lead to seizures, as demonstrated by the fact that PC deficiency is related to recurrent seizures in patients. CA V, providing HCO3− to pyruvate carboxylase, is involved in controlling the proper functioning of this enzyme [40] and, then, its action might have implications for epilepsy.
- (7)
- Numerous experimental and clinical studies support the notion that oxidative stress substantially contributes to the pathogenesis of epilepsy [68]. Studies showed that patients affected by epilepsy report a remarkable increase in levels of oxidative markers, such as malondialdehyde (MDA), protein carbonylation (PC) and nitric oxide (NO), when compared to a control group. An excessive production of free radicals could be implicated in neuronal hyperexcitability that triggers epileptogenesis. Moreover, it has been reported that overproduction of reactive oxygen species (ROS) provokes the progressive disruption of Ca2+ homeostasis essential for neuronal survival. In this context, it has been proposed that CAs, in particular CA VII might also have a role in the cell defence against oxidative damage thanks to its cysteine residues [69].
- (8)
- GABAergic inhibition has been traditionally considered as the principal mechanism counterbalancing glutamatergic excitation and preventing epileptiform activity. Indeed, many of the currently used antiepileptic drugs act through enhancement of GABAergic signaling. However, much evidence has shown that epileptiform events can also be characterized by synchronous firing driven by excitatory GABA [70]. As during the first phases of development [19], excitatory action of GABA in epilepsy is due to (a) elevated intracellular chloride concentration as a result of chloride accumulation during hyperactivity [71]. High levels of intra-neuronal Cl− leads to Cl− efflux and then to depolarization in response to GABA binding to its type A receptor; (b) HCO3− permeability of GABA-A channels [72,73] that causes HCO3− efflux and then depolarization; (c) elevation of extracellular potassium caused by KCC2-mediated extrusion of chloride and potassium that results in membrane depolarization [74]. CAs are implicated in this abnormal epilepsy-associated GABA-A excitation. Specifically, it has been shown that they have a role in favouring the efflux of HCO3− ions through GABA-A receptors [75,76]. CA VII, which plays an important role in the development of febrile seizures [21], has been identified as a key molecule in GABAergic excitation and it has been suggested that CA VII developmental expression governs the electrophysiological behaviour related to neural circuit plasticity and to susceptibility to epileptogenesis [77].
4. CA Inhibitors Clinically Employed in Epilepsy Therapy
5. Anticonvulsant CAIs Design Strategy
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Definition of Epilepsy 2014. International League Against Epilepsy. Available online: https://www.ilae.org/guidelines/definition-and-classification/definition-of-epilepsy-2014 (accessed on 30 June 2021).
- Shakirullah, A.N.; Khan, A.; Nabi, M. The Prevalence, Incidence and Etiology of Epilepsy. Int. J. Clin. Exp. Neurol. 2014, 2, 29–39. [Google Scholar] [CrossRef]
- Sarmast, S.T.; Abdullahi, A.M.; Jahan, N. Current Classification of Seizures and Epilepsies: Scope, Limitations and Recommendations for Future Action. Cureus 2020, 12, e10549. [Google Scholar] [CrossRef]
- Epilepsy. Available online: https://www.who.int/news-room/fact-sheets/detail/epilepsy (accessed on 19 July 2021).
- Löscher, W.; Potschka, H.; Sisodiya, S.M.; Vezzani, A. Drug Resistance in Epilepsy: Clinical Impact, Potential Mechanisms, and New Innovative Treatment Options. Pharmacol. Rev. 2020, 72, 606–638. [Google Scholar] [CrossRef]
- Cerri, C.; Genovesi, S.; Allegra, M.; Pistillo, F.; Püntener, U.; Guglielmotti, A.; Perry, V.H.; Bozzi, Y.; Caleo, M. The Chemokine CCL2 Mediates the Seizure-enhancing Effects of Systemic Inflammation. J. Neurosci. 2016, 36, 3777–3788. [Google Scholar] [CrossRef]
- Cerri, C.; Caleo, M.; Bozzi, Y. Chemokines as New Inflammatory Players in the Pathogenesis of Epilepsy. Epilepsy Res. 2017, 136, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Mishra, C.B.; Tiwari, M.; Supuran, C.T. Progress in the Development of Human Carbonic Anhydrase Inhibitors and their Pharmacological Applications: Where are We Today? Med. Res. Rev. 2020, 40, 2485–2565. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, M.; Kondeti, B.; McKenna, R. Anticonvulsant/Antiepileptic Carbonic Anhydrase Inhibitors: A Patent Review. Expert Opin. Ther. Patents 2013, 23, 717–724. [Google Scholar] [CrossRef]
- Ozsoy, H.Z. Anticonvulsant Effects of Carbonic Anhydrase Inhibitors: The Enigmatic Link Between Carbonic Anhydrases and Electrical Activity of the Brain. Neurochem. Res. 2021, 46, 2783–2799. [Google Scholar] [CrossRef]
- Supuran, C.T. Carbonic Anhydrase Inhibitors. Bioorg. Med. Chem. Lett. 2010, 20, 3467–3474. [Google Scholar] [CrossRef] [PubMed]
- Lill, M.A.; Danielson, M.L. Computer-Aided Drug Design Platform Using PyMOL. J. Comput. Mol. Des. 2010, 25, 13–19. [Google Scholar] [CrossRef]
- Ciccone, L.; Policar, C.; Stura, E.A.; Shepard, W. Human TTR Conformation Altered by Rhenium Tris-Carbonyl Derivatives. J. Struct. Biol. 2016, 195, 353–364. [Google Scholar] [CrossRef]
- Polsinelli, I.; Nencetti, S.; Shepard, W.; Ciccone, L.; Orlandini, E.; Stura, E.A. A New Crystal Form of Human Transthyretin Obtained with a Curcumin Derived Ligand. J. Struct. Biol. 2016, 194, 8–17. [Google Scholar] [CrossRef]
- Solomon, R.W. Free and Open Source Software for the Manipulation of Digital Images. Am. J. Roentgenol. 2009, 192, W330–W334. [Google Scholar] [CrossRef]
- Tong, C.-K.; Cammer, W.; Chesler, M. Activity-Dependent ph Shifts in Hippocampal Slices from Normal and Carbonic Anhydrase II-Deficient Mice. Glia 2000, 31, 125–130. [Google Scholar] [CrossRef]
- Ruusuvuori, E.; Kaila, K. Carbonic Anhydrases and Brain pH in the Control of Neuronal Excitability. In Carbonic Anhydrase: Mechanism, Regulation, Links to Disease, and Industrial Applications; Frost, S.C., McKenna, R., Eds.; Subcellular Biochemistry; Springer: Dordrecht, The Netherlands, 2014; pp. 271–290. ISBN 978-94-007-7359-2. [Google Scholar]
- Leniger, T.; Thöne, J.; Wiemann, M. Topiramate Modulates pH of Hippocampal CA3 Neurons by Combined Effects on Carbonic Anhydrase and Cl−/HCO3−Exchange. Br. J. Pharmacol. 2004, 142, 831–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ben-Ari, Y.; Gaiarsa, J.-L.; Tyzio, R.; Khazipov, R. GABA: A Pioneer Transmitter That Excites Immature Neurons and Generates Primitive Oscillations. Physiol. Rev. 2007, 87, 1215–1284. [Google Scholar] [CrossRef]
- Blaesse, P.; Airaksinen, M.S.; Rivera, C.; Kaila, K. Cation-Chloride Cotransporters and Neuronal Function. Neuron 2009, 61, 820–838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruusuvuori, E.; Huebner, A.K.; Kirilkin, I.; Yukin, A.Y.; Blaesse, P.; Helmy, M.; Kang, H.J.; El Muayed, M.; Hennings, J.C.; Voipio, J.; et al. Neuronal Carbonic Anhydrase VII Provides Gabaergic Excitatory Drive to Exacerbate Febrile Seizures. EMBO J. 2013, 32, 2275–2286. [Google Scholar] [CrossRef] [Green Version]
- Nocentini, A.; Angeli, A.; Carta, F.; Winum, J.-Y.; Zalubovskis, R.; Carradori, S.; Capasso, C.; Donald, W.A.; Supuran, C.T. Reconsidering Anion Inhibitors in the General Context of Drug Design Studies of Modulators of Activity of the Classical Enzyme Carbonic Anhydrase. J. Enzym. Inhib. Med. Chem. 2021, 36, 561–580. [Google Scholar] [CrossRef] [PubMed]
- Supuran, C.T.; Scozzafava, A.; Casini, A. Carbonic Anhydrase Inhibitors. Med. Res. Rev. 2003, 23, 146–189. [Google Scholar] [CrossRef] [PubMed]
- Supuran, C.T. Carbonic Anhydrases: Novel Therapeutic Applications for Inhibitors and Activators. Nat. Rev. Drug Discov. 2008, 7, 168–181. [Google Scholar] [CrossRef]
- Supuran, C.T. How Many Carbonic Anhydrase Inhibition Mechanisms Exist? J. Enzym. Inhib. Med. Chem. 2016, 31, 345–360. [Google Scholar] [CrossRef]
- Alterio, V.; Hilvo, M.; Di Fiore, A.; Supuran, C.T.; Pan, P.; Parkkila, S.; Scaloni, A.; Pastorek, J.; Pastorekova, S.; Pedone, C.; et al. Crystal Structure of the Catalytic Domain of the Tumor-Associated Human Carbonic Anhydrase IX. Proc. Natl. Acad. Sci. USA 2009, 106, 16233–16238. [Google Scholar] [CrossRef] [Green Version]
- Sjoblom, B.; Polentarutti, M.; Djinovic-Carugo, K. Structural Study of X-Ray Induced Activation of Carbonic Anhydrase. Proc. Natl. Acad. Sci. USA 2009, 106, 10609–10613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan, I.; Shajee, B.; Waheed, A.; Ahmad, F.; Sly, W.S. Structure, Function and Applications of Carbonic Anhydrase Isozymes. Bioorg. Med. Chem. 2013, 21, 1570–1582. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, A.E.; Jones, T.A.; Liljas, A. Refined Structure of Human Carbonic Anhydrase II at 2.0 Å Resolution. Proteins Struct. Funct. Bioinform. 1988, 4, 274–282. [Google Scholar] [CrossRef]
- Håkansson, K.; Carlsson, M.; Svensson, L.; Liljas, A. Structure of Native and Apo Carbonic Anhydrase II and Structure of Some of its Anion-Ligand Complexes. J. Mol. Biol. 1992, 227, 1192–1204. [Google Scholar] [CrossRef]
- Supuran, C.T. Structure-Based Drug Discovery of Carbonic Anhydrase Inhibitors. J. Enzym. Inhib. Med. Chem. 2012, 27, 759–772. [Google Scholar] [CrossRef]
- Liljas, A.; Kannan, K.K.; Bergstén, P.-C.; Waara, I.; Fridborg, K.; Strandberg, B.; Carlbom, U.; Järup, L.; Lövgren, S.; Petef, M. Crystal Structure of Human Carbonic Anhydrase, C. Nat. New Biol. 1972, 235, 131–137. [Google Scholar] [CrossRef]
- Sippel, K.H.; Robbins, A.H.; Domsic, J.; Genis, C.; Agbandje-McKenna, M.; McKenna, R. High-Resolution Structure of Human Carbonic Anhydrase II Complexed with Acetazolamide Reveals Insights into Inhibitor Drug Design. Acta Crystallogr. Sect. F Struct. Biol. Cryst. Commun. 2009, 65, 992–995. [Google Scholar] [CrossRef] [Green Version]
- Di Fiore, A.; Truppo, E.; Supuran, C.T.; Alterio, V.; Dathan, N.; Bootorabi, F.; Parkkila, S.; Monti, S.M.; De Simone, G. Crystal Structure of the C183S/C217S Mutant of Human CA VII in Complex with Acetazolamide. Bioorg. Med. Chem. Lett. 2010, 20, 5023–5026. [Google Scholar] [CrossRef] [PubMed]
- Villalba, M.L.; Palestro, P.; Ceruso, M.; Funes, J.L.G.; Talevi, A.; Blanch, L.B.; Supuran, C.T.; Gavernet, L. Sulfamide Derivatives with Selective Carbonic Anhydrase VII Inhibitory Action. Bioorg. Med. Chem. 2016, 24, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Gavernet, L.; Funes, J.L.G.; Palestro, P.H.; Blanch, L.E.B.; Estiu, G.L.; Maresca, A.; Barrios, I.; Supuran, C.T. Inhibition Pattern of Sulfamide-Related Compounds in Binding to Carbonic Anhydrase Isoforms I, II, VII, XII and XIV. Bioorg. Med. Chem. 2013, 21, 1410–1418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whittingtons, D.A.; Grubb, J.H.; Waheed, A.; Shah, G.N.; Sly, W.S.; Christianson, D.W. Expression, Assay, and Structure of the Extracellular Domain of Murine Carbonic Anhydrase XIV. J. Biol. Chem. 2004, 279, 7223–7228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alterio, V.; Pan, P.; Parkkila, S.; Buonanno, M.; Supuran, C.T.; Monti, S.M.; De Simone, G. The Structural Comparison Between Membrane-Associated Human Carbonic Anhydrases Provides Insights into Drug Design of Selective Inhibitors. Biopolymers 2014, 101, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Pastorekova, S.; Parkkila, S.; Pastorek, J.; Supuran, C.T. Review Article. J. Enzym. Inhib. Med. Chem. 2004, 19, 199–229. [Google Scholar] [CrossRef] [PubMed]
- Anne, T.; Jean-Michel, D.; Claudiu, T.S.; Bernard, M. Carbonic Anhydrase Inhibitors as Anticonvulsant Agents. Curr. Top. Med. Chem. 2007, 7, 855–864. [Google Scholar]
- Kida, E.; Palminiello, S.; Golabek, A.A.; Walus, M.; Wierzba-Bobrowicz, T.; Rabe, A.; Albertini, G.; Wisniewski, K.E. Carbonic Anhydrase II in the Developing and Adult Human Brain. J. Neuropathol. Exp. Neurol. 2006, 65, 664–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mishra, C.B.; Kumari, S.; Angeli, A.; Bua, S.; Tiwari, M.; Supuran, C.T. Discovery of Benzenesulfonamide Derivatives as Carbonic Anhydrase Inhibitors with Effective Anticonvulsant Action: Design, Synthesis, and Pharmacological Evaluation. J. Med. Chem. 2018, 61, 3151–3165. [Google Scholar] [CrossRef] [PubMed]
- Ghandour, M.S.; Parkkila, A.-K.; Parkkila, S.; Waheed, A.; Sly, W.S. Mitochondrial Carbonic Anhydrase in the Nervous System. J. Neurochem. 2000, 75, 2212–2220. [Google Scholar] [CrossRef] [PubMed]
- Taniuchi, K.; Nishimori, I.; Takeuchi, T.; Fujikawa-Adachi, K.; Ohtsuki, Y.; Onishi, S. Developmental Expression of Carbonic Anhydrase-Related Proteins VIII, X, And XI in the Human Brain. Neuroscience 2002, 112, 93–99. [Google Scholar] [CrossRef]
- Harju, A.-K.; Bootorabi, F.; Kuuslahti, M.; Supuran, C.T.; Parkkila, S. Carbonic anhydrase III: A Neglected Isozyme is Stepping into the Limelight. J. Enzym. Inhib. Med. Chem. 2013, 28, 231–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aspatwar, A.; Tolvanen, M.E.E.; Ortutay, C.; Parkkila, S. Carbonic Anhydrase Related Proteins: Molecular Biology and Evolution. Carbon. Anhydrase 2014, 75, 135–156. [Google Scholar] [CrossRef]
- Hilvo, M.; Tolvanen, M.; Clark, A.; Shen, B.; Shah, G.N.; Waheed, A.; Halmi, P.; Hänninen, M.; Hämäläinen, J.M.; Vihinen, M.; et al. Characterization of CA XV, a new GPI-anchored form of Carbonic Anhydrase. Biochem. J. 2005, 392, 83–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parkkila, S.; Parkkila, A.-K.; Rajaniemi, H.; Shah, G.N.; Grubb, J.H.; Waheed, A.; Sly, W.S. Expression of Membrane-Associated Carbonic Anhydrase XIV on Neurons and Axons in Mouse and Human Brain. Proc. Natl. Acad. Sci. USA 2001, 98, 1918–1923. [Google Scholar] [CrossRef] [Green Version]
- Halmi, P.; Parkkila, S.; Honkaniemi, J. Expression of Carbonic Anhydrases II, IV, VII, VIII and XII in Rat Brain After Kainic Acid Induced Status Epilepticus. Neurochem. Int. 2006, 48, 24–30. [Google Scholar] [CrossRef]
- Miller, J.W. Stopping Seizures with Carbon Dioxide. Epilepsy Curr. 2011, 11, 114–115. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.; Vignal, J.-P.; Baumann, C.; Anxionnat, J.-F.; Muresan, M.; Vespignani, H.; Maillard, L. Effect of Hyperventilation on Seizure Activation: Potentiation by Antiepileptic Drug Tapering. J. Neurol. Neurosurg. Psychiatry 2011, 82, 928–930. [Google Scholar] [CrossRef]
- Raimondo, J.; Burman, R.J.; Katz, A.A.; Akerman, C.J. Ion Dynamics During Seizures. Front. Cell. Neurosci. 2015, 9, 419. [Google Scholar] [CrossRef] [Green Version]
- Shah, G.N.; Ulmasov, B.; Waheed, A.; Becker, T.; Makani, S.; Svichar, N.; Chesler, M.; Sly, W.S. Carbonic Anhydrase IV and XIV Knockout Mice: Roles of the Respective Carbonic Anhydrases in Buffering the Extracellular Space in Brain. Proc. Natl. Acad. Sci. USA 2005, 102, 16771–16776. [Google Scholar] [CrossRef] [Green Version]
- Folbergrová, J.; Kunz, W.S. Mitochondrial dysfunction in epilepsy. Mitochondrion 2012, 12, 35–40. [Google Scholar] [CrossRef]
- Bernardino, R.; Dias, T.R.; Moreira, B.; Cunha, M.; Barros, A.; Oliveira, E.; Sousa, M.; Alves, M.G.; Oliveira, P.F. Carbonic Anhydrases are Involved in Mitochondrial Biogenesis and Control the Production of Lactate by Human Sertoli Cells. FEBS J. 2019, 286, 1393–1406. [Google Scholar] [CrossRef] [PubMed]
- Lambert, N.; Grover, L. The Mechanism of Biphasic GABA Responses. Science 1995, 269, 928–929. [Google Scholar] [CrossRef]
- Chesler, M. Regulation and Modulation of pH in the Brain. Physiol. Rev. 2003, 83, 1183–1221. [Google Scholar] [CrossRef]
- Casey, J.R.; Grinstein, S.; Orlowski, J. Sensors and Regulators of Intracellular pH. Nat. Rev. Mol. Cell Biol. 2010, 11, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Pasternack, M.; Smirnov, S.; Kaila, K. Proton Modulation of Functionally Distinct GABAA Receptors in Acutely Isolated Pyramidal Neurons of Rat Hippocampus. Neuropharmacology 1996, 35, 1279–1288. [Google Scholar] [CrossRef]
- Wilkins, M.E.; Hosie, A.M.; Smart, T.G. Proton Modulation of Recombinant GABAAreceptors: Influence of GABA Concentration and the β Subunit TM2-TM3 Domain. J. Physiol. 2005, 567, 365–377. [Google Scholar] [CrossRef]
- Traynelis, S.F.; Wollmuth, L.P.; McBain, C.J.; Menniti, F.; Vance, K.M.; Ogden, K.; Hansen, K.; Yuan, H.; Myers, S.J.; Dingledine, R. Glutamate Receptor Ion Channels: Structure, Regulation, and Function. Pharmacol. Rev. 2010, 62, 405–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makani, S.; Chen, H.-Y.; Esquenazi, S.; Shah, G.N.; Waheed, A.; Sly, W.S.; Chesler, M. NMDA Receptor-Dependent Afterdepolarizations Are Curtailed by Carbonic Anhydrase 14: Regulation of a Short-Term Postsynaptic Potentiation. J. Neurosci. 2012, 32, 16754–16762. [Google Scholar] [CrossRef] [Green Version]
- Waldmann, R.; Champigny, G.; Bassilana, F.; Heurteaux, C.; Lazdunski, M. A Proton-Gated Cation Channel Involved in Acid-Sensing. Nature 1997, 386, 173–177. [Google Scholar] [CrossRef]
- Munsch, T.; Pape, H. Modulation of the Hyperpolarization-Activated Cation Current of Rat Thalamic Relay Neurones by Intracellular pH. J. Physiol. 1999, 519, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Enyedi, P.; Czirják, G. Molecular Background of Leak K+ Currents: Two-Pore Domain Potassium Channels. Physiol. Rev. 2010, 90, 559–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, C.M.; Dichter, M.; Morad, M. Modulation of the N-methyl-D-aspartate Channel by Extracellular H+. Proc. Natl. Acad. Sci. USA 1990, 87, 6445–6449. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Wu, J.; Guo, R.; Peng, Y.; Zheng, W.; Liu, D.; Song, Z. Glycolysis in Energy Metabolism During Seizures. Neural Regen. Res. 2013, 8, 1316–1326. [Google Scholar] [CrossRef] [PubMed]
- Svichar, N.; Chesler, M. Surface Carbonic Anhydrase Activity on Astrocytes and Neurons Facilitates Lactate Transport. Glia 2003, 41, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Deitmer, J.W.; Theparambil, S.M.; Ruminot, I.; Noor, S.I.; Becker, H.M. Energy Dynamics in the Brain: Contributions of Astrocytes to Metabolism and pH Homeostasis. Front. Neurosci. 2019, 13, 1301. [Google Scholar] [CrossRef]
- Geronzi, U.; Lotti, F.; Grosso, S. Oxidative Stress in Epilepsy. Expert Rev. Neurother. 2018, 18, 427–434. [Google Scholar] [CrossRef]
- Monti, S.M.; Supuran, C.T.; De Simone, G.; Di Fiore, A. Chapter 9—Carbonic Anhydrase VII. In Carbonic Anhydrases as Biocatalysts; Supuran, C.T., De Simone, G., Eds.; Elsevier: Amsterdam, The Netherlands, 2015; pp. 151–168. ISBN 978-0-444-63258-6. [Google Scholar]
- Khazipov, R. GABAergic Synchronization in Epilepsy. Cold Spring Harb. Perspect. Med. 2016, 6, a022764. [Google Scholar] [CrossRef] [Green Version]
- Fujiwara-Tsukamoto, Y.; Isomura, Y.; Nambu, A.; Takada, M. Excitatory Gaba Input Directly Drives Seizure-Like Rhythmic Synhronization in Mature Hippocampal CA1 Pyramidal Cells. Neuroscience 2003, 119, 265–275. [Google Scholar] [CrossRef]
- Kaila, K.; Lamsa, K.; Smirnov, S.; Taira, T.; Voipio, J. Long-Lasting GABA-Mediated Depolarization Evoked by High-Frequency Stimulation in Pyramidal Neurons of Rat Hippocampal Slice is Attributable to a Network-Driven, Bicarbonate-Dependent K+Transient. J. Neurosci. 1997, 17, 7662–7672. [Google Scholar] [CrossRef] [Green Version]
- Staley, K.J.; Soldo, B.L.; Proctor, W.R. Ionic Mechanisms of Neuronal Excitation by Inhibitory GABA A Receptors. Science 1995, 269, 977–981. [Google Scholar] [CrossRef] [PubMed]
- Viitanen, T.; Ruusuvuori, E.; Kaila, K.; Voipio, J. The K+-Cl−cotransporter KCC2 Promotes GABAergic Excitation in the Mature Rat Hippocampus. J. Physiol. 2010, 588, 1527–1540. [Google Scholar] [CrossRef] [PubMed]
- Velazquez, J.L.P. Bicarbonate-Dependent Depolarizing Potentials in Pyramidal Cells and Interneurons during Epileptiform Activity. Eur. J. Neurosci. 2003, 18, 1337–1342. [Google Scholar] [CrossRef] [PubMed]
- Rivera, C.; Voipio, J.; Kaila, K. Two Developmental Switches in GABAergic Signalling: The K+-Cl-cotransporter KCC2 and Carbonic Anhydrase CAVII. J. Physiol. 2005, 562, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Ruusuvuori, E.; Li, H.; Huttu, K.; Palva, J.M.; Smirnov, S.; Rivera, C.; Kaila, K.; Voipio, J. Carbonic Anhydrase Isoform VII Acts as a Molecular Switch in the Development of Synchronous Gamma-Frequency Firing of Hippocampal CA1 Pyramidal Cells. J. Neurosci. 2004, 24, 2699–2707. [Google Scholar] [CrossRef] [PubMed]
- Lim, L.-L.; Foldvary, N.; Mascha, E.; Lee, J. Acetazolamide in Women with Catamenial Epilepsy. Epilepsia 2001, 42, 746–749. [Google Scholar] [CrossRef] [PubMed]
- Reiss, W.G.; Oles, K.S. Acetazolamide in the Treatment of Seizures. Ann. Pharmacother. 1996, 30, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, S.; Avoli, M. Carbonic Anhydrase Inhibition by Acetazolamide Reduces In Vitro Epileptiform Synchronization. Neuropharmacology 2015, 95, 377–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lillis, K.P.; Kramer, M.A.; Mertz, J.; Staley, K.J.; White, J.A. Pyramidal Cells Accumulate Chloride at Seizure Onset. Neurobiol. Dis. 2012, 47, 358–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woodbury, D.M.; Rollins, L.T.; Gardner, M.D.; Hirschi, W.L.; Hogan, J.R.; Rallison, M.L.; Tanner, G.S.; Brodie, D.A. Effects of Carbon Dioxide on Brain Excitability and Electrolytes. Am. J. Physiol. Content 1957, 192, 79–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maren, T.H. Carbonic Anhydrase: Chemistry, Physiology, and Inhibition. Physiol. Rev. 1967, 47, 595–781. [Google Scholar] [CrossRef]
- Masuda, Y.; Utsui, Y.; Shiraishi, Y.; Karasawa, T.; Yoshida, K.; Shimizu, M. Relationships between Plasma Concentrations of Diphenylhydantoin, Phenobarbital, Carbamazepine, and 3-Sulfamoylmethyl-1,2-Benzisoxazole (AD-810), a New Anticonvulsant Agent, and Their Anticonvulsant or Neurotoxic Effects in Experimental Animals. Epilepsia 1979, 20, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Seizure and Epilepsy Medicines. Available online: https://www.epilepsy.com/learn/treating-seizures-and-epilepsy/seizure-and-epilepsy-medicines (accessed on 3 September 2021).
- Schauf, C. Zonisamide Enhances Slow Sodium Inactivation inMyxicola. Brain Res. 1987, 413, 185–188. [Google Scholar] [CrossRef]
- Rock, D.M.; Macdonald, R.L.; Taylor, C.P. Blockade of Sustained Repetitive Action Potentials in Cultured Spinal Cord Neurons by Zonisamide (AD 810, CI 912), a Novel Anticonvulsant. Epilepsy Res. 1989, 3, 138–143. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, S.; Kawakami, K.; Nishimura, S.; Watanabe, Y.; Yagi, K.; Scino, M.; Miyamoto, K. Zonisamide blocks T-type Calcium Channel in Cultured Neurons of Rat Cerebral Cortex. Epilepsy Res. 1992, 12, 21–27. [Google Scholar] [CrossRef]
- Ueda, Y.; Doi, T.; Tokumaru, J.; Willmore, L. Effect of zonisamide on molecular regulation of glutamate and GABA transporter proteins during epileptogenesis in rats with hippocampal seizures. Mol. Brain Res. 2003, 116, 1–6. [Google Scholar] [CrossRef]
- Yamamura, S.; Saito, H.; Suzuki, N.; Kashimoto, S.; Hamaguchi, T.; Ohoyama, K.; Suzuki, D.; Kanehara, S.; Nakagawa, M.; Shiroyama, T.; et al. Effects of zonisamide on Neurotransmitter Release Associated with Inositol Triphosphate Receptors. Neurosci. Lett. 2009, 454, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Wilfong, A.A.; Willmore, L.J. Zonisamide? A Review of Experience and Use in Partial Seizures. Neuropsychiatr. Dis. Treat. 2006, 2, 269–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mori, A.; Noda, Y.; Packer, L. The Anticonvulsant Zonisamide Scavenges Free Radicals. Epilepsy Res. 1998, 30, 153–158. [Google Scholar] [CrossRef]
- Shank, R.P.; Gardocki, J.F.; Vaught, J.L.; Davis, C.B.; Schupsky, J.J.; Raffa, R.B.; Dodgson, S.J.; Nortey, S.O.; Maryanoff, B.E. Topiramate: Preclinical Evaluation of a Structurally Novel Anticonvulsant. Epilepsia 1994, 35, 450–460. [Google Scholar] [CrossRef]
- Wauquier, A.; Zhou, S. Topiramate: A Potent Anticonvulsant in the Amygdala-Kindled Rat. Epilepsy Res. 1996, 24, 73–77. [Google Scholar] [CrossRef]
- Rigoulot, M.-A.; Boehrer, A.; Nehlig, A. Effects of Topiramate in Two Models of Genetically Determined Generalized Epilepsy, the GAERS and the Audiogenic Wistar AS. Epilepsia 2003, 44, 14–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Lang, S.; Xu, G.; Liu, X.; Zuo, P. Effects of Topiramate on Seizure Susceptibility in Kainate-Kindled Rats: Involvement of Peripheral-Type Benzodiazepine Receptors. Seizure 2008, 17, 358–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffin, A.; Hamling, K.; Hong, S.; Anvar, M.; Lee, L.P.; Baraban, S.C. Preclinical Animal Models for Dravet Syndrome: Seizure Phenotypes, Comorbidities and Drug Screening. Front. Pharmacol. 2018, 9, 573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiron, C. Current Therapeutic Procedures in Dravet Syndrome. Dev. Med. Child Neurol. 2011, 53, 16–18. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, D.W. Usefulness of Extended-Release Topiramate in Patients with Epilepsy: A Two-Year Retention Study. J. Clin. Pharm. Ther. 2021, 46, 1412–1417. [Google Scholar] [CrossRef]
- Herrero, A.I.; Del Olmo, N.; González-Escalada, J.R.; Solís, J.M. Two New Actions of Topiramate: Inhibition of Depolarizing GABAA-Mediated Responses and Activation of a Potassium Conductance. Neuropharmacology 2002, 42, 210–220. [Google Scholar] [CrossRef]
- Aribi, A.M.; Stringer, J.L. Effects of Antiepileptic Drugs on Extracellular pH Regulation in the Hippocampal CA1 Region In Vivo. Epilepsy Res. 2002, 49, 143–151. [Google Scholar] [CrossRef]
- White, H.S.; Brown, S.D.; Woodhead, J.H.; Skeen, G.A.; Wolf, H.H. Topiramate Modulates GABA-evoked Currents in Murine Cortical Neurons By A Nonbenzodiazepine Mechanism. Epilepsia 2000, 41, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Petroff, O.A.C.; Hyder, F.; Rothman, D.L.; Mattson, R.H. Topiramate Rapidly Raises Brain GABA in Epilepsy Patients. Epilepsia 2001, 42, 543–548. [Google Scholar] [CrossRef]
- Gryder, D.S.; Rogawski, M.A. Selective Antagonism of GluR5 Kainate-Receptor-Mediated Synaptic Currents by Topiramate in Rat Basolateral Amygdala Neurons. J. Neurosci. 2003, 23, 7069–7074. [Google Scholar] [CrossRef]
- DeLorenzo, R.J.; Sombati, S.; Coulter, U.A. Effects of Topiramate on Sustained Repetitive Firing and Spontaneous Recurrent Seizure Discharges in Cultured Hippocampal Neurons. Epilepsia 2000, 41, 40–44. [Google Scholar] [CrossRef]
- McLean, M.J.; Bukhari, A.A.; Wamil, A.W. Effects of Topiramate on Sodium-Dependent Action-Potential Firing by Mouse Spinal Cord Neurons in Cell Culture. Epilepsia 2000, 41, 21–24. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.-L.; Velumian, A.A.; Jones, O.T.; Carlen, P.L. Modulation of High-Voltage-Activated Calcium Channels in Dentate Granule Cells by Topiramate. Epilepsia 2000, 41, 52–60. [Google Scholar] [CrossRef]
- Carta, F.; Supuran, C.T.; Scozzafava, A. Sulfonamides and Their Isosters as Carbonic Anhydrase Inhibitors. Future Med. Chem. 2014, 6, 1149–1165. [Google Scholar] [CrossRef] [PubMed]
- Mishra, C.B.; Kumari, S.; Angeli, A.; Bua, S.; Mongre, R.K.; Tiwari, M.; Supuran, C.T. Discovery of Potent Carbonic Anhydrase Inhibitors as Effective Anticonvulsant Agents: Drug Design, Synthesis, and In Vitro and In Vivo Investigations. J. Med. Chem. 2021, 64, 3100–3114. [Google Scholar] [CrossRef] [PubMed]
- Mishra, C.B.; Kumari, S.; Angeli, A.; Monti, S.M.; Buonanno, M.; Tiwari, M.; Supuran, C.T. Discovery of Benzenesulfonamides with Potent Human Carbonic Anhydrase Inhibitory and Effective Anticonvulsant Action: Design, Synthesis, and Pharmacological Assessment. J. Med. Chem. 2017, 60, 2456–2469. [Google Scholar] [CrossRef] [PubMed]









Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciccone, L.; Cerri, C.; Nencetti, S.; Orlandini, E. Carbonic Anhydrase Inhibitors and Epilepsy: State of the Art and Future Perspectives. Molecules 2021, 26, 6380. https://doi.org/10.3390/molecules26216380
Ciccone L, Cerri C, Nencetti S, Orlandini E. Carbonic Anhydrase Inhibitors and Epilepsy: State of the Art and Future Perspectives. Molecules. 2021; 26(21):6380. https://doi.org/10.3390/molecules26216380
Chicago/Turabian StyleCiccone, Lidia, Chiara Cerri, Susanna Nencetti, and Elisabetta Orlandini. 2021. "Carbonic Anhydrase Inhibitors and Epilepsy: State of the Art and Future Perspectives" Molecules 26, no. 21: 6380. https://doi.org/10.3390/molecules26216380
APA StyleCiccone, L., Cerri, C., Nencetti, S., & Orlandini, E. (2021). Carbonic Anhydrase Inhibitors and Epilepsy: State of the Art and Future Perspectives. Molecules, 26(21), 6380. https://doi.org/10.3390/molecules26216380








