Cytotoxic, Antitumor and Toxicological Profile of Passiflora alata Leaf Extract
Abstract
1. Introduction
2. Results and Discussion
3. Materials and Methods
3.1. Source of Leaf Extract from Passiflora alata Curtis
3.2. Saponin Identification
3.3. Tumor Cells
3.4. Cytotoxicity in Tumor Cell Lines
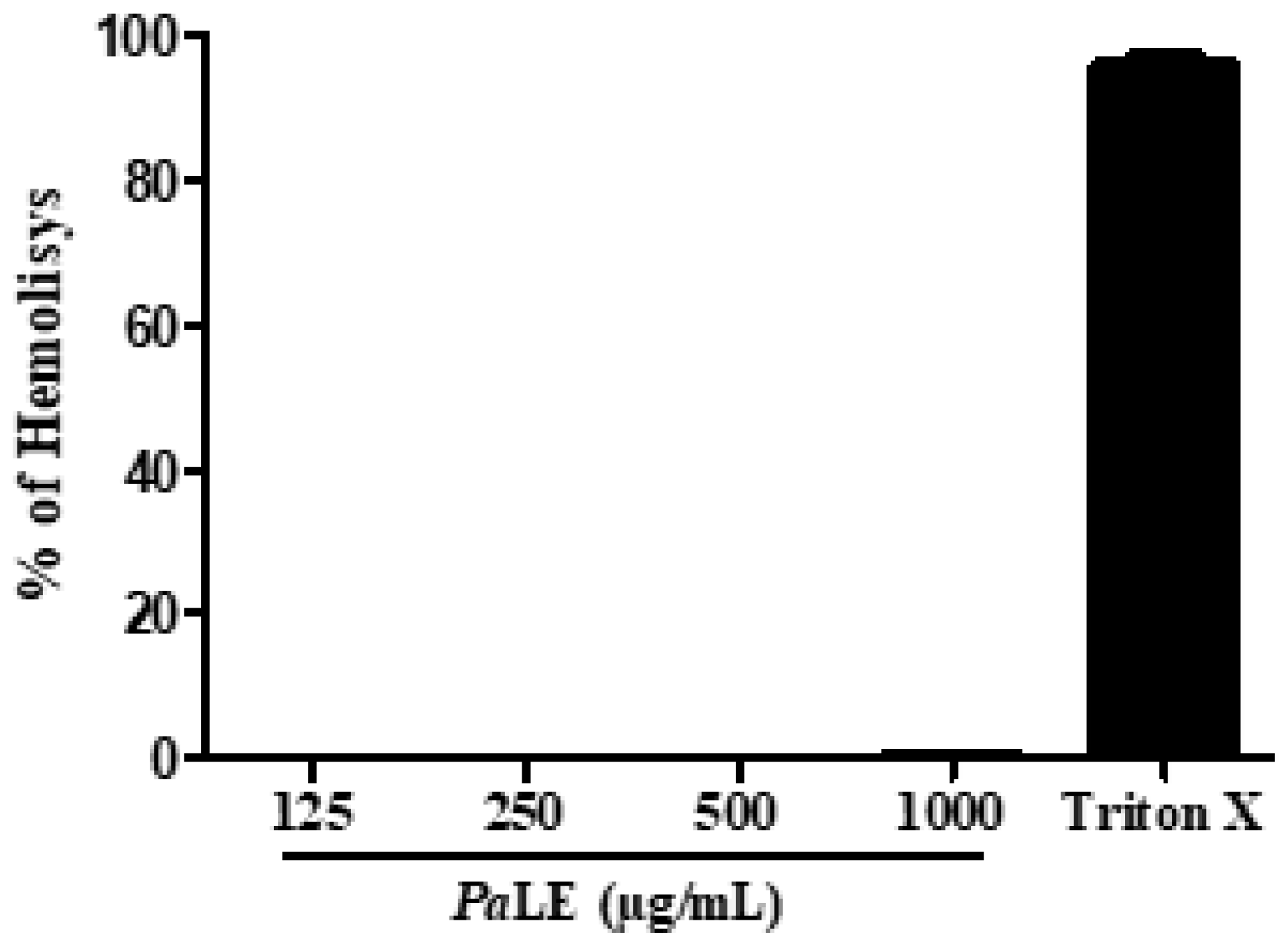
3.5. Hemolytic Activity
3.6. Antitumoral Activity In Vivo
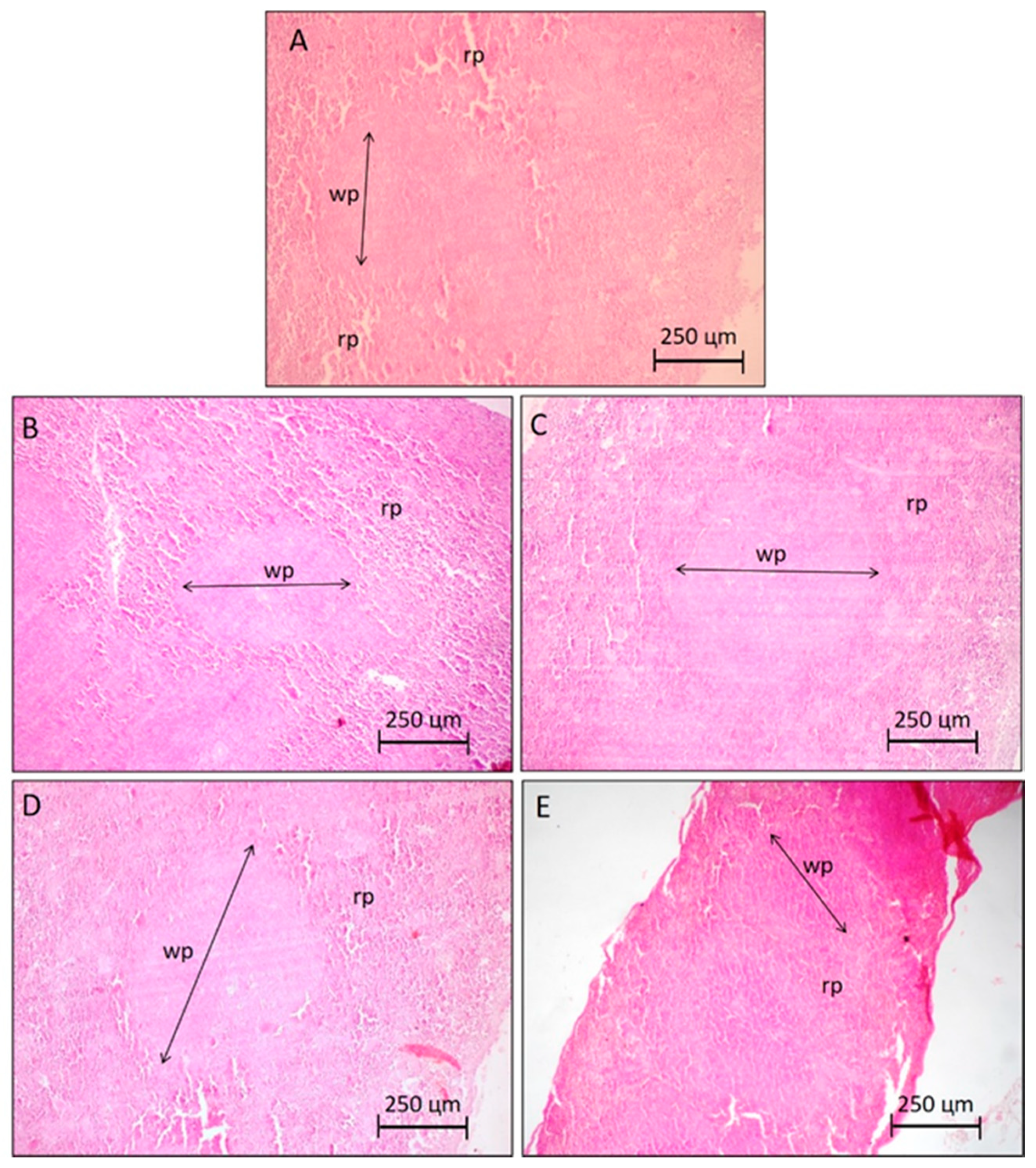
3.7. In Vivo Antitumoral Activity in Sarcoma Tumor 180-Bearing Mice
3.8. Evaluation of the Toxicological Effects
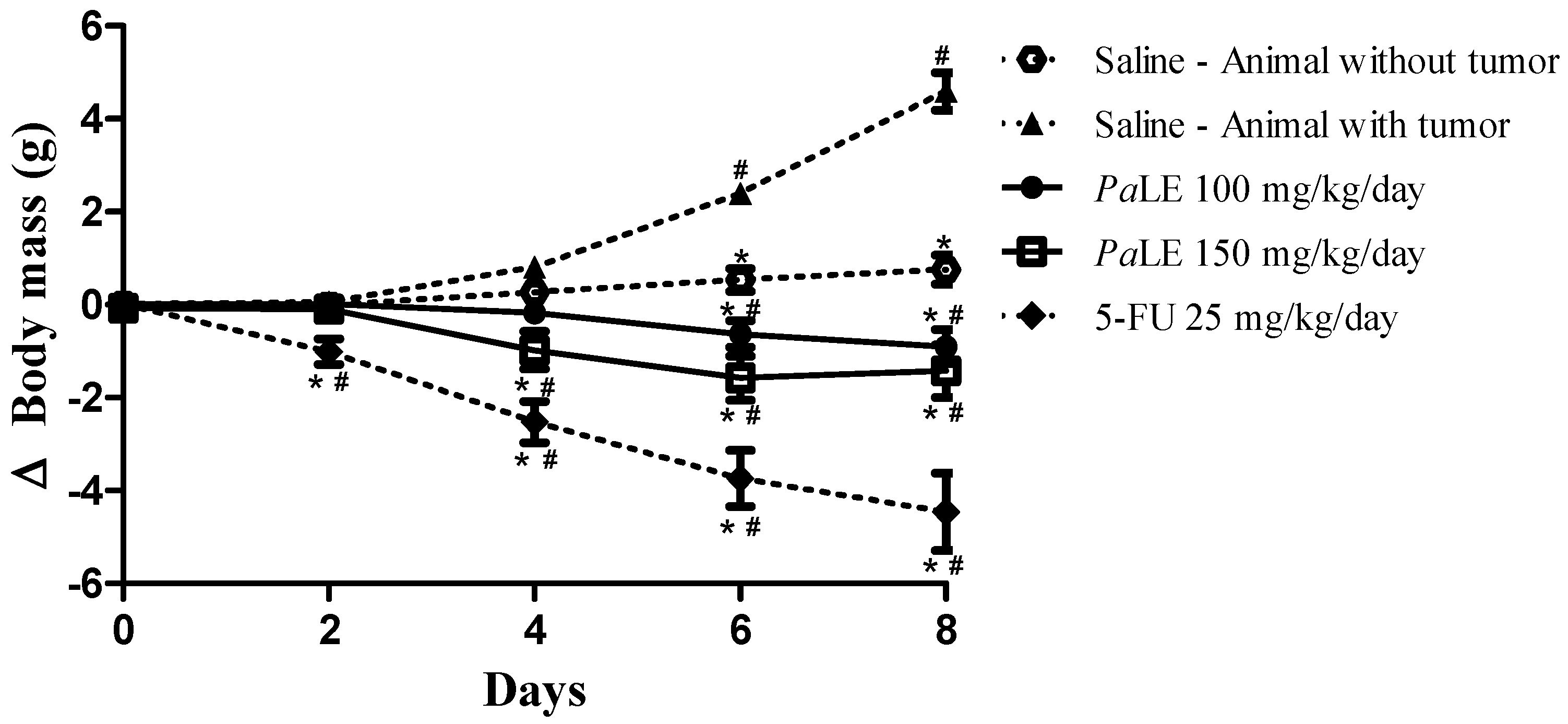
3.8.1. Determination of Body Mass
3.8.2. Determination of Water and Feed Ingestion
3.8.3. Determination of the Mass of Organs
3.9. Evaluation of Biochemical Parameters
3.10. Evaluation of Hematological Parameters
3.11. Histopathological Evaluation of Organs
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Vinod, S.K.; Hau, E. Radiotherapy treatment for lung cancer: Current status and future directions. Respirology 2020. [Google Scholar] [CrossRef] [PubMed]
- Aslakson, R.A.; Chandrashekaran, S.V.; Rickerson, E.; Fahy, B.N.; Johnston, F.M.; Miller, J.A.; Conca-Cheng, A.; Wang, S.; Morris, A.M.; Lorenz, K.; et al. A multicenter, randomized controlled trial of perioperative palliative care surrounding cancer surgery for patients and their family members (PERIOP-PC). J. Palliat. Med. 2019, 22, 44–57. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, M.d.C.; Sanchez-Lopez, E.; Espina, M.; Garcia, M.L.; Durazzo, A.; Lucarini, M.; Novellino, E.; Souto, S.B.; Santini, A.; Souto, E.B. Sirtuins and SIRT6 in carcinogenesis and in diet. Int. J. Mol. Sci. 2019, 20, 4945. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.R.; Santos, A.C.; Sanchez-Lopez, E.; Kovacevic, A.B.; Espina, M.; Calpena, A.C.; Veiga, F.J.; Garcia, M.L.; Souto, E.B. Neoplastic multifocal skin lesions: Biology, etiology, and targeted therapies for nonmelanoma skin cancers. Skin Pharm. Physiol. 2018, 31, 59–73. [Google Scholar] [CrossRef] [PubMed]
- Britto, A.C.; de Oliveira, A.C.; Henriques, R.M.; Cardoso, G.M.; Bomfim, D.S.; Carvalho, A.A.; Moraes, M.O.; Pessoa, C.; Pinheiro, M.L.; Costa, E.V. In vitro and in vivo antitumor effects of the essential oil from the leaves of Guatteria friesiana. Planta Med. 2012, 78, 409–414. [Google Scholar] [CrossRef]
- Antoni, S.; Soerjomataram, I.; Møller, B.; Bray, F.; Ferlay, J. An assessment of GLOBOCAN methods for deriving national estimates of cancer incidence. Bull. World Health Organ. 2016, 94, 174. [Google Scholar] [CrossRef]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in globocan 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef]
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef]
- Dias, D.A.; Urban, S.; Roessner, U. A historical overview of natural products in drug discovery. Metabolites 2012, 2, 303–336. [Google Scholar] [CrossRef]
- Newman, D.J.; Cragg, G.M. Natural products as sources of new drugs from 1981 to 2014. J. Nat. Prod. 2016, 79, 629–661. [Google Scholar] [CrossRef]
- Harvey, A.L.; Edrada-Ebel, R.; Quinn, R.J. The re-emergence of natural products for drug discovery in the genomics era. Nature Rev. Drug Discov. 2015, 14, 111–129. [Google Scholar] [CrossRef] [PubMed]
- Rayan, A.; Raiyn, J.; Falah, M. Nature is the best source of anticancer drugs: Indexing natural products for their anticancer bioactivity. PLoS ONE 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Kuete, V.; Dzotam, J.K.; Voukeng, I.K.; Fankam, A.G.; Efferth, T. Cytotoxicity of methanol extracts of annona muricata, passiflora edulis and nine other cameroonian medicinal plants towards multi-factorial drug-resistant cancer cell lines. Springerplus 2016, 5, 1666. [Google Scholar] [CrossRef] [PubMed]
- Carraz, M.; Lavergne, C.; Jullian, V.; Wright, M.; Gairin, J.E.; de la Cruz, M.G.; Bourdy, G. Antiproliferative activity and phenotypic modification induced by selected Peruvian medicinal plants on human hepatocellular carcinoma Hep3B cells. J. Ethnopharmacol. 2015, 166, 185–199. [Google Scholar] [CrossRef]
- Kapadia, G.J.; Azuine, M.A.; Tokuda, H.; Hang, E.; Mukainaka, T.; Nishino, H.; Sridhar, R. Inhibitory effect of herbal remedies on 12-O-tetradecanoylphorbol-13-acetate-promoted Epstein-Barr virus early antigen activation. Pharmacol. Res. 2002, 45, 213–220. [Google Scholar] [CrossRef]
- Ma, W.-D.; Zou, Y.-P.; Wang, P.; Yao, X.-H.; Sun, Y.; Duan, M.-H.; Fu, Y.-J.; Yu, B. Chimaphilin induces apoptosis in human breast cancer MCF-7 cells through a ROS-mediated mitochondrial pathway. Food Chem. Toxicol. 2014, 70, 1–8. [Google Scholar] [CrossRef]
- Sujana, N.; Ramanathan, S.; Vimala, V.; Sundaram, M.; Pemaiah, B. Antitumour potential of Passiflora incarnata L. against Ehrlich ascites carcinoma. Int. J. Pharm. Pharm. Sci. 2012, 4, 10–13. [Google Scholar]
- Chaparro, D.C.; Maldonado Celis, M.E.; Urango, L.A.; RojanoI, B.A. Propiedades quimiopreventivas de Passiflora mollissima (Kunth) LH Bailey (curuba larga) contra cáncer colorrectal. Rev. Cuba. Plan. Med. 2015, 20, 62–74. [Google Scholar]
- Perry, N.; Albertson, G.; Blunt, J.; Cole, A.; Munro, M.; Walker, J. 4-Hydroxy-2-cyclopentenone: An anti-pseudomonas and cytotoxic component from passiflora tetrandra1. Planta Méd. 1991, 57, 129–131. [Google Scholar] [CrossRef]
- Amaral, R.G.; Gomes, S.V.F.; Luciano, M.C.D.S.; Pessoa, C.D.Ó.; Andrade, L.N.; Severino, P.; Brandão, G.C.; Bomfim, L.M.; Soares, M.B.P.; Bezerra, D.P.; et al. Cytotoxic potential of 14 Passiflora species against cancer cells. J. Med. Plants Res. 2019, 13, 157–166. [Google Scholar]
- Colomeu, T.; Figueiredo, D.; Cazarin, C.; Schumacher, N.; Maróstica Jr, M.; Meletti, L.; Zollner, R. Antioxidant and anti-diabetic potential of Passiflora alata Curtis aqueous leaves extract in type 1 diabetes mellitus (NOD-mice). Int. Immunopharmacol. 2014, 18, 106–115. [Google Scholar] [CrossRef]
- Boeira, J.M.; Fenner, R.; Betti, A.H.; Provensi, G.; Lacerda, L.d.A.; Barbosa, P.R.; González, F.H.; Corrêa, A.M.; Driemeier, D.; Dall’Alba, M.P. Toxicity and genotoxicity evaluation of Passiflora alata Curtis (Passifloraceae). J. Ethnopharmacol. 2010, 128, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Miroddi, M.; Calapai, G.; Navarra, M.; Minciullo, P.; Gangemi, S. Passiflora incarnata L.: Ethnopharmacology, clinical application, safety and evaluation of clinical trials. J. Ethnopharmacol. 2013, 150, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Montero, D.A.; Marques, M.O.M.; Meletti, L.M.; KAMPEN, M.H.; Polozzi, S.C. Floral scent of brazilian Passiflora: Five species analised by dynamic headspace. An. Acad. Bras. Ciênc. 2016, 88, 1191–1200. [Google Scholar] [CrossRef] [PubMed]
- Man, S.; Gao, W.; Zhang, Y.; Huang, L.; Liu, C. Chemical study and medical application of saponins as anti-cancer agents. Fitoterapia 2010, 81, 703–714. [Google Scholar] [CrossRef]
- Xu, X.-H.; Li, T.; Fong, C.M.V.; Chen, X.; Chen, X.-J.; Wang, Y.-T.; Huang, M.-Q.; Lu, J.-J. Saponins from Chinese medicines as anticancer agents. Molecules 2016, 21, 1326. [Google Scholar] [CrossRef]
- Andrade, L.N.; Lima, T.C.; Amaral, R.G.; Pessoa, C.d.O.; Soares, B.M.; Nascimento, L.G.d.; Carvalho, A.A.; de Sousa, D.P. Evaluation of the cytotoxicity of structurally correlated p-menthane derivatives. Molecules 2015, 20, 13264–13280. [Google Scholar] [CrossRef]
- da Silva, T.B.; Costa, C.O.S.; Galvão, A.F.; Bomfim, L.M.; Rodrigues, A.C.B.d.C.; Mota, M.C.; Dantas, A.A.; dos Santos, T.R.; Soares, M.B.; Bezerra, D.P. Cytotoxic potential of selected medicinal plants in northeast Brazil. BMC Complement. Altern. Med. 2016, 16, 199. [Google Scholar] [CrossRef]
- Mahmoud, T.S.; Marques, M.R.; Pessoa, C.d.Ó.; Lotufo, L.V.; Magalhães, H.I.; Moraes, M.O.d.; Lima, D.P.d.; Tininis, A.G.; Oliveira, J.E.d. In vitro cytotoxic activity of Brazilian Middle West plant extracts. Revista Bras. Farmacogn. 2011, 21, 456–464. [Google Scholar] [CrossRef]
- Silveira, F.; Rossi, S.; Fernández, C.; Gosmann, G.; Schenkel, E.; Ferreira, F. Alum-type Adjuvant Effect of Non-haemolytic Saponins Purified from Ilex and Passiflora spp. Phytother. Res. 2011, 25, 1783–1788. [Google Scholar] [CrossRef]
- Dai, F.; Miao, Q.; Zhou, B.; Yang, L.; Liu, Z.-L. Protective effects of flavonols and their glycosides against free radical-induced oxidative hemolysis of red blood cells. Life Sci. 2006, 78, 2488–2493. [Google Scholar] [CrossRef] [PubMed]
- Amaral, R.G.; Fonseca, C.S.; Silva, T.K.M.; Andrade, L.N.; França, M.E.; Barbosa-Filho, J.M.; de Sousa, D.P.; Moraes, M.O.; Pessoa, C.Ó.; Carvalho, A.A. Evaluation of the cytotoxic and antitumour effects of the essential oil from M entha x villosa and its main compound, rotundifolone. J. Pharm. Pharmacol. 2015, 67, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.-X.; Peng, X.-Y. Protective effect of triterpenoid fractions from the rhizomes of Astilbe chinensis on cyclophosphamide-induced toxicity in tumor-bearing mice. J. Ethnopharmacol. 2008, 119, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.; Stein, A.C.; Stolz, E.D.; Dallegrave, E.; Buffon, A.; do Rego, J.-C.; Gosmann, G.; Viana, A.F.; Rates, S.M.K. Repeated administration of an aqueous spray-dried extract of the leaves of Passiflora alata Curtis (Passifloraceae) inhibits body weight gain without altering mice behavior. J. Ethnopharmacol. 2013, 145, 59–66. [Google Scholar] [CrossRef]
- Andrade, L.N.; Amaral, R.G.; Dória, G.A.A.; Fonseca, C.S.; Da Silva, T.K.M.; Albuquerque Júnior, R.L.C.; Thomazzi, S.M.; Do Nascimento, L.G.; Carvalho, A.A.; De Sousa, D.P. In vivo anti-tumor activity and toxicological evaluations of Perillaldehyde 8, 9-Epoxide, a derivative of Perillyl alcohol. Int. J. Mol. Sci. 2016, 17, 32. [Google Scholar] [CrossRef]
- Dória, G.A.A.; Menezes, P.P.; Lima, B.S.; Vasconcelos, B.S.; Silva, F.A.; Henriques, R.M.; Melo, M.G.; Alves, Â.V.; Moraes, M.O.; Pessoa, C.Ó. In vivo antitumor effect, induction of apoptosis and safety of Remirea maritima Aubl.(Cyperaceae) extracts. Phytomedicine 2016, 23, 914–922. [Google Scholar] [CrossRef]
- Mousinho, K.C.; Oliveira, C.d.C.; Ferreira, J.R.d.O.; Carvalho, A.A.; Magalhães, H.I.F.; Bezerra, D.P.; Alves, A.P.N.; Costa-Lotufo, L.V.; Pessoa, C.; de Matos, M.P.V. Antitumor effect of laticifer proteins of Himatanthus drasticus (Mart.) Plumel–Apocynaceae. J. Ethnopharmacol. 2011, 137, 421–426. [Google Scholar] [CrossRef]
- Amaral, R.G.; Andrade, L.N.; Dória, G.A.A.; Barbosa-Filho, J.M.; de Sousa, D.P.; Carvalho, A.A.; Thomazzi, S.M. Antitumour effects of the essential oil from Mentha x villosa combined with 5-fluorouracil in mice. Flavour Fragr. J. 2016, 31, 250–254. [Google Scholar] [CrossRef]
- Bronte, V.; Pittet, M.J. The spleen in local and systemic regulation of immunity. Immunity 2013, 39, 806–818. [Google Scholar] [CrossRef]
- Grigorian, A.; O’Brien, C.B. Hepatotoxicity secondary to chemotherapy. J. Clin. Transl. Hepatol. 2014, 2, 95. [Google Scholar]
- Rudnicki, M.; Silveira, M.; Pereira, T.; Oliveira, M.; Reginatto, F.; Dal-Pizzol, F.; Moreira, J. Protective effects of Passiflora alata extract pretreatment on carbon tetrachloride induced oxidative damage in rats. Food Chem. Toxicol. 2007, 45, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.; Gadewar, M.; Tahilyani, V.; Patel, D.K. A review on pharmacological and analytical aspects of diosmetin: A concise report. Chin. J. Integr. Med. 2013, 19, 792–800. [Google Scholar] [CrossRef]
- Berridge, M.V.; Herst, P.M.; Tan, A.S. Tetrazolium dyes as tools in cell biology: New insights into their cellular reduction. Biotechnol. Ann. Rev. 2005, 11, 127–152. [Google Scholar]
- Bezerra, D.P.; Pessoa, C.; Moraes, M.O.d.; Alencar, N.M.d.; Mesquita, R.O.; Lima, M.W.; Alves, A.P.N.; Pessoa, O.D.L.; Chaves, J.H.; Silveira, E.R. In vivo growth inhibition of sarcoma 180 by piperlonguminine, an alkaloid amide from the Piper species. J. Appl. Toxicol. 2008, 28, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, L.; Cheung, P.C.K. Immunopotentiation and anti-tumor activity of carboxymethylated-sulfated β-(1→3)-D-glucan from Poria cocos. Int. Immunopharmacol. 2010, 10, 398–405. [Google Scholar] [CrossRef]
- Zheng, Y.; Zhou, F.; Wu, X.; Wen, X.; Li, Y.; Yan, B.; Zhang, J.; Hao, G.; Ye, W.; Wang, G. 23-Hydroxybetulinic acid from Pulsatilla chinensis (Bunge) Regel synergizes the antitumor activities of doxorubicin in vitro and in vivo. J. Ethnopharmacol. 2010, 128, 615–622. [Google Scholar] [CrossRef]
Sample Availability: Samples of Passiflora alata leaves are available from the authors. |




| Compounds | RT (min) | [M + H]+ (m/z) | [M − H]− (m/z) | [M + CHCOOH]− (m/z) | Sugar Residues | Characteristic m/z of Ions in Negative Ion Mode |
|---|---|---|---|---|---|---|
| C42H68O13 | 6.15 | 781 | 779.6 | 825 | Glc; Glc | 779.2; 617.5; 455.1 |
| C42H68O13 | 6.23 | 781 | 779.8 | 825 | Glc; Glc | 779.4; 617.4; 455.2 |
| C42H70O13 | 6.86 | 783 | 781.5 | 827 | Glc, Glu | 781.5; 619.7; 443.3; 178.8; 161.1 |
| C42H70O13 | 6.07 | 783 | 781.8 | 827 | Glc; Rham | 781.4; 619.6; 160.8; 146.8 |
| C42H70O13 | 6.48 | 783 | 781.5 | 827 | Glc; Pent | 781.5; 619.0; 161.3; 130.9 |
| C42H70O14 | 4.81 | 799 | 797.4 | 843 | Glc | 797.5; 635.2; 179.0 |
| C42H70O14 | 5.22 | 799 | 797.6 | 843 | Glc; Glu | 797.6; 635.2; 460.1; 159.3 |
| C42H70O14 | 5.47 | 799 | 797.4 | 843 | Glc | 797.4; 635.3; 455.5; 159.6 |
| C42H70O14 | 6.02 | 799 | 797.4 | 843 | Glc | 797.3; 635.3; 422.4; 161.2 |
| C42H70O15 | 5.37 | 815 | 813.7 | 859 | Glc; Glc | 813.4; 651.2; 489.6; 161.0 |
| C48H80O18 | 4.96 | 945 | 943.5 | 989 | Glc; Glc | 943.7; 780.4; 653.2; 621.8 |
| C48 H80 O18 | 5.01 | 945 | 943.6 | 989 | Glc; Glu | 943.5; 781.3; 588.8 |
| C48H80O19 | 4.44 | 961 | 959.8 | 1005 | Glc; Glc; Glu | 959.2; 797.5; 459.0; 161.2 |
| C54H90O23 | 4.66 | 1107 | 1105.3 | 1151 | Rham; Glu; Glc; Pent | 1105.2; 959.8; 782.2; 489.0; 179.0 |
| C54H90O23 | 4.86 | 1107 | 1105.1 | 1151 | Glc; Pent | 1105.3; 943.3; 471.4; 131.0 |
| C54H90O24 | 4.46 | 1123 | 1121.4 | 1167 | Glc | 11,121.4; 959.1 |
| C54H90O24 | 4.26 | 1123 | 1121.6 | 1167 | Glc | 11,121.6; 959.4; 691.4 |
| Cell Lines | PaLE | Doxorrubicin | ||
|---|---|---|---|---|
| % CPI ± SD | IC50 | % CPI ± SD | IC50 | |
| PC-3 | 83.26 ± 2.29 | 20.24 (16.58–24.70) | 98.21 ± 0.54 | 0.55 (0.39–0.83) |
| K-562 | 76.24 ± 3.71 | 37.92 (29.56–48.63) | 99.15 ± 0.15 | 0.70 (0.53–0.94) |
| HepG2 | 75.56 ± 4.08 | >50.00 | 85.70 ± 0.88 | 0.35 (0.28–0.44) |
| S180 | 79.11 ± 2.97 | 19.13 (15.43–24.96) | 81.73 ± 1.18 | 4.5 (3.33–5.13) |
| Parameters | Healthy | Animal with Tumor | |||
|---|---|---|---|---|---|
| Saline | Saline | PaLE 100 mg/kg/day | PaLE 150 mg/kg/day | 5-FU 25 mg/kg/day | |
| Water consumption (mL) | 46.2 ± 1.33 | 41.3 ± 3.70 | 41.60 ± 0.93 | 40.90 ± 1.10 | 15.60 ± 0.40 * # |
| Feed Consumption (g) | 37.05 ± 0.38 | 35.60 ± 0.63 | 28.35 ± 0.42 * # | 27.95 ± 0.95 * # | 17.95 ± 0.78 * # |
| Spleen (g/100 g m.c.) | 0.39 ± 0.01 * | 0.52 ± 0.03 | 0.64 ± 0.02 * # | 0.62 ± 0.04 * # | 0.29 ± 0.03 * # |
| Liver (g/100 g m.c.) | 5.33 ± 0.12 | 5.41 ± 0.08 | 5.64 ± 0.20 | 5.88 ± 0.15 | 5.33 ± 0.09 |
| Kidneys (g/100 g m.c.) | 1.35 ± 0.03 | 1.44 ± 0.06 | 1.33 ± 0.04 | 1.38 ± 0.04 | 1.40 ± 0.05 |
| Parameters | Healthy | Animal with Tumor | |||
|---|---|---|---|---|---|
| Saline | Saline | PaLE 100 mg/kg/day | PaLE 150 mg/kg/day | 5-FU 25 mg/kg/day | |
| ALT (U/L) | 53.60 ± 1.97 | 51.60 ± 5.08 | 48.40 ± 4.21 | 49.67 ± 6.01 | 41.60 ± 6.00 |
| AST (U/L) | 85.75 ± 1.05 * | 196.2 ± 9.43 # | 147.5 ± 10.26 * # | 156.5 ± 11.15 * # | 93.33 ± 8.7 * |
| FA (mg/dL) | 70.35 ± 1.97 | 64.32 ± 4.36 | 72.55 ± 1.37 | 69.74 ± 2.79 | 76.55 ± 3.53 |
| Uric acid (mg/dL) | 2.81 ± 0.49 | 2.67 ± 0.57 | 2.51 ± 0.35 | 2.59 ± 0.43 | 2.78 ± 0.55 |
| Creatinine (mg/dL) | 0.32 ± 0.06 | 0.29 ± 0.01 | 0.31 ± 0.01 | 0.28 ± 0.01 | 0.37 ± 0.02 |
| Urea (mg/dL) | 46.60 ± 1.54 | 42.00 ± 4.35 | 36.60 ± 3.97 | 39.00 ± 0.58 | 49.00 ± 5.86 |
| Parameters | Healthy | Animal with Tumor | |||
|---|---|---|---|---|---|
| Saline | Saline | PaLE 100 mg/kg/day | PaLE 150 mg/kg/day | 5-FU 25 mg/kg/day | |
| Total leukocytes (103 cels/µL) | 7.29 ± 0.76 * | 9.49 ± 0.37 # | 12.48 ± 0.55 * # | 13.84 ± 0.95 * # | 2.40 ± 0.37 * # |
| Lymphocytes % | 69.63 ± 1.19 * | 48.13 ± 2.36 # | 55.23 ± 4.76 * # | 54.40 ± 2.62 * # | 82.40 ± 1.29 * # |
| Monocytes % | 1.75 ± 0.53 | 1.63 ± 0.32 | 1.17 ± 0.31 | 1.60 ± 0.24 | 1.20 ± 0.20 |
| Neutrophils % | 28.62 ± 1.13 * | 50.25 ± 2.46 # | 43.60 ± 3.84 * # | 44.00 ± 1.70 * # | 16.40 ± 1.21 * # |
| Red cells (106/mL) | 7.83 ± 0.60 | 7.67 ± 0.61 | 8.00 ± 0.37 | 8.17 ± 0.79 | 7.50 ± 0.56 |
| Hemoglobin (g/dL) | 14.17 ± 0.54 | 13.17 ± 0.79 | 13.33 ± 0.92 | 13.50 ± 1.02 | 12.83 ± 1.14 |
| Hematocrit (%) | 43.17 ± 1.72 | 42.83 ± 1.70 | 43.67 ± 1.23 | 44.33 ± 2.17 | 42.67 ± 1.56 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amaral, R.G.; Gomes, S.V.F.; Andrade, L.N.; dos Santos, S.A.; Severino, P.; de Albuquerque Júnior, R.L.C.; Souto, E.B.; Brandão, G.C.; Santos, S.L.; David, J.M.; et al. Cytotoxic, Antitumor and Toxicological Profile of Passiflora alata Leaf Extract. Molecules 2020, 25, 4814. https://doi.org/10.3390/molecules25204814
Amaral RG, Gomes SVF, Andrade LN, dos Santos SA, Severino P, de Albuquerque Júnior RLC, Souto EB, Brandão GC, Santos SL, David JM, et al. Cytotoxic, Antitumor and Toxicological Profile of Passiflora alata Leaf Extract. Molecules. 2020; 25(20):4814. https://doi.org/10.3390/molecules25204814
Chicago/Turabian StyleAmaral, Ricardo G., Silvana V. F. Gomes, Luciana N. Andrade, Sara A. dos Santos, Patrícia Severino, Ricardo L. C. de Albuquerque Júnior, Eliana B. Souto, Geraldo C. Brandão, Sandra L. Santos, Jorge M. David, and et al. 2020. "Cytotoxic, Antitumor and Toxicological Profile of Passiflora alata Leaf Extract" Molecules 25, no. 20: 4814. https://doi.org/10.3390/molecules25204814
APA StyleAmaral, R. G., Gomes, S. V. F., Andrade, L. N., dos Santos, S. A., Severino, P., de Albuquerque Júnior, R. L. C., Souto, E. B., Brandão, G. C., Santos, S. L., David, J. M., & Carvalho, A. A. (2020). Cytotoxic, Antitumor and Toxicological Profile of Passiflora alata Leaf Extract. Molecules, 25(20), 4814. https://doi.org/10.3390/molecules25204814







