Simultaneous Quantification and Pharmacokinetic Study of Five Homologs of Dalbavancin in Rat Plasma Using UHPLC-MS/MS
Abstract
1. Introduction
2. Results and Discussion
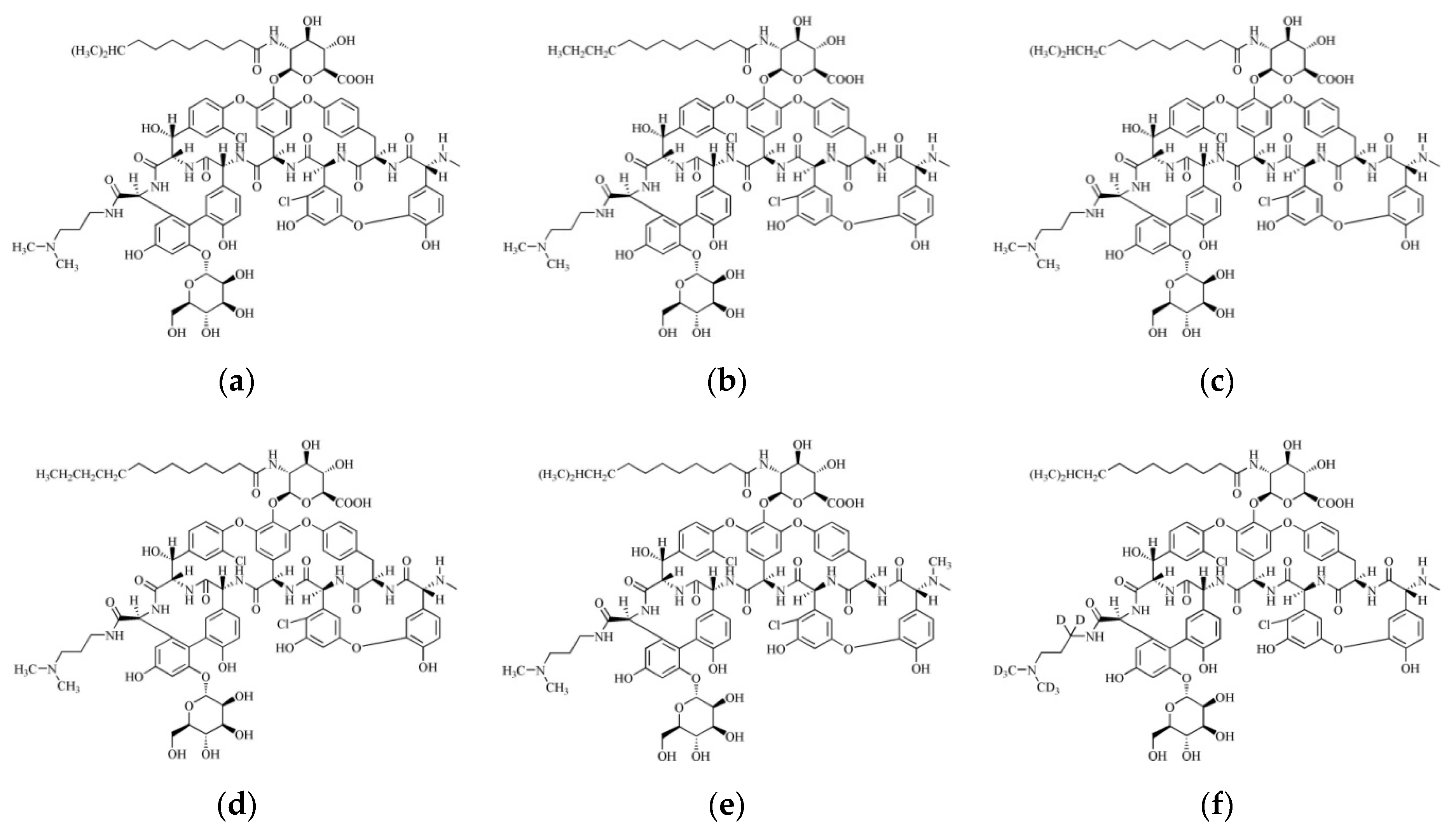
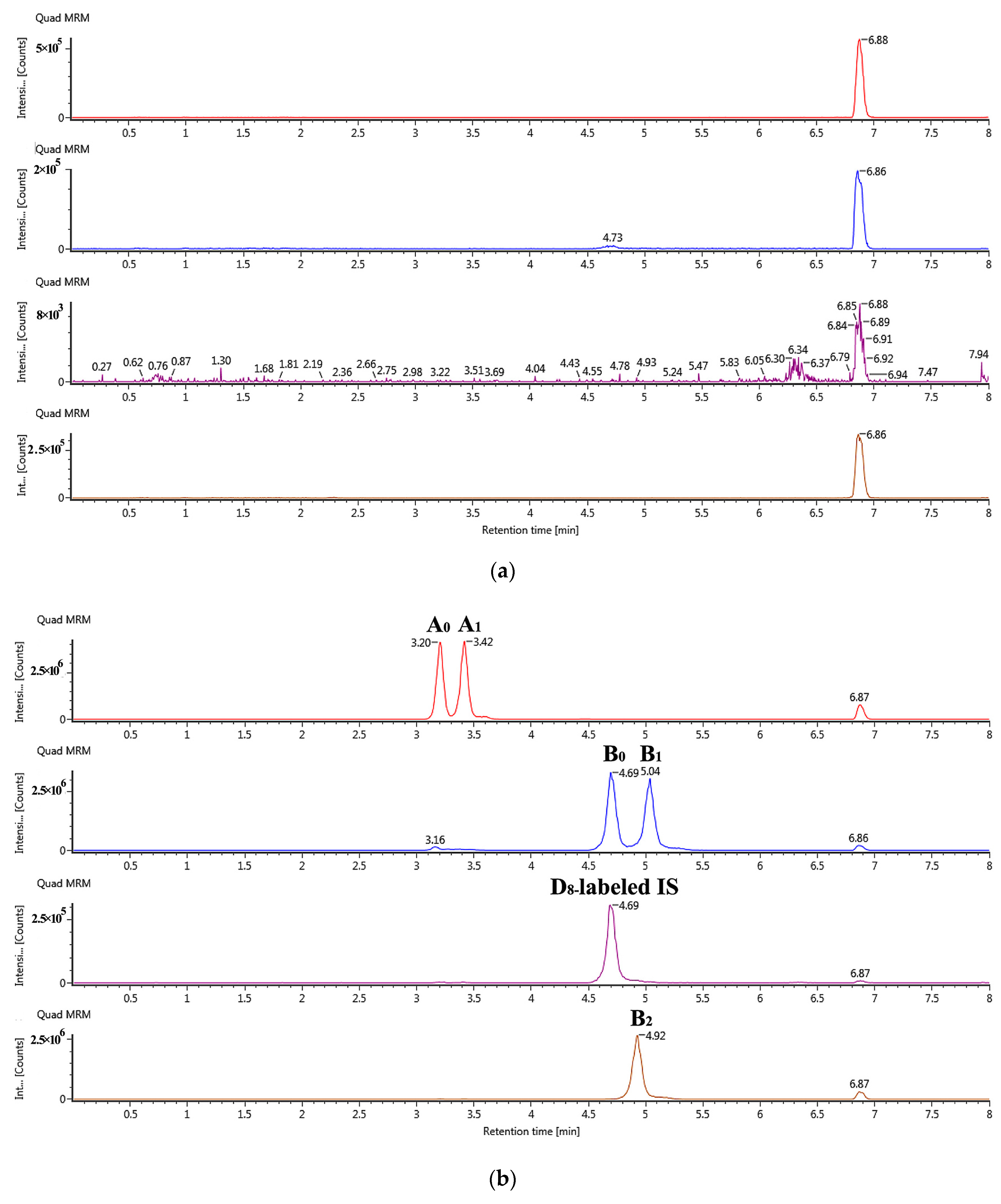
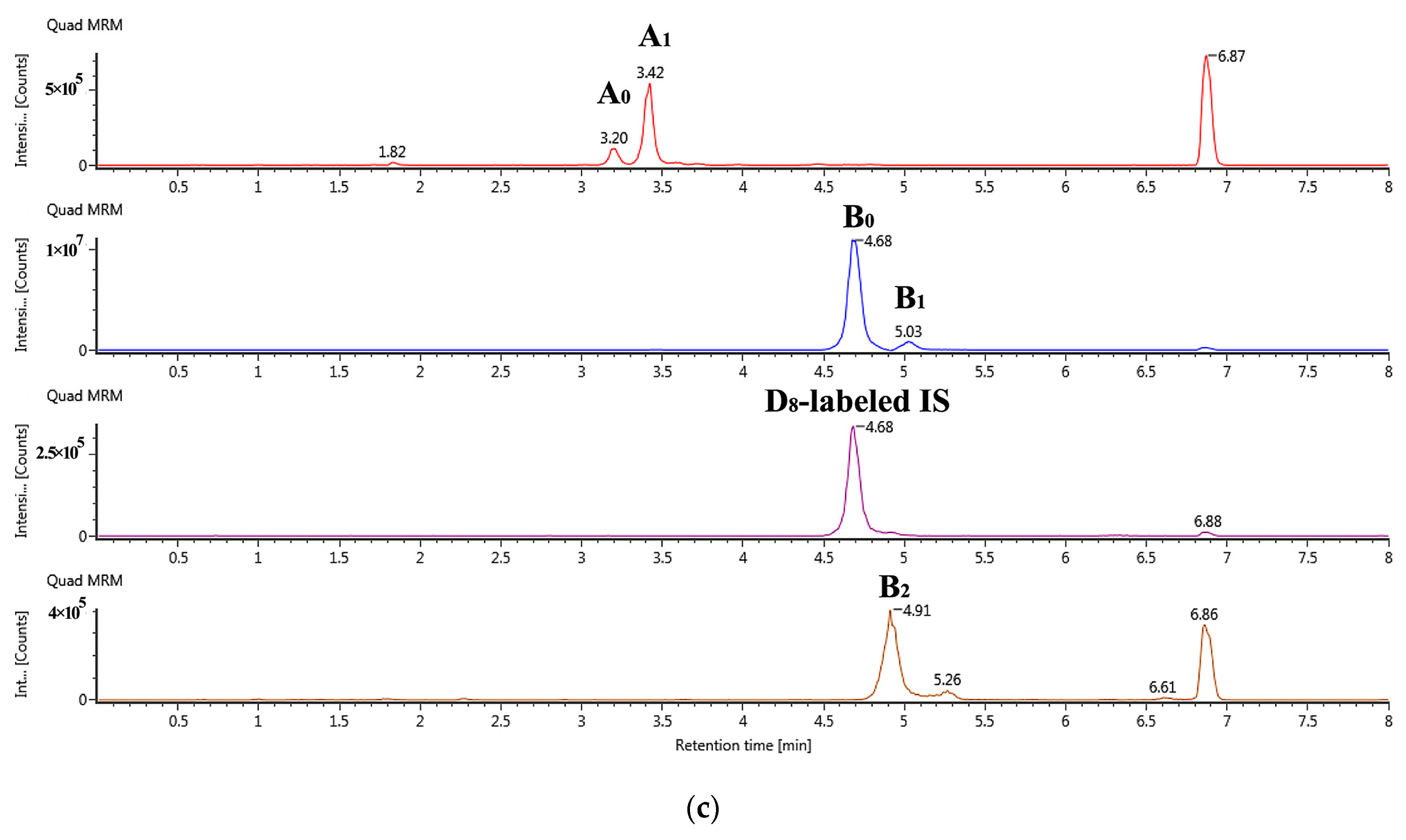
2.1. Optimization of the UHPLC-MS/MS
2.2. Optimization of Sample Preparation
2.3. Method Validation
2.3.1. Specificity, Linearity, Limit of Detection (LOD), and LLOQ
2.3.2. Recovery, Matrix Effect, Intra-Day Precision, and Inter-Day Precision
2.3.3. Stability, Dilution Reliability, and Residue Verification
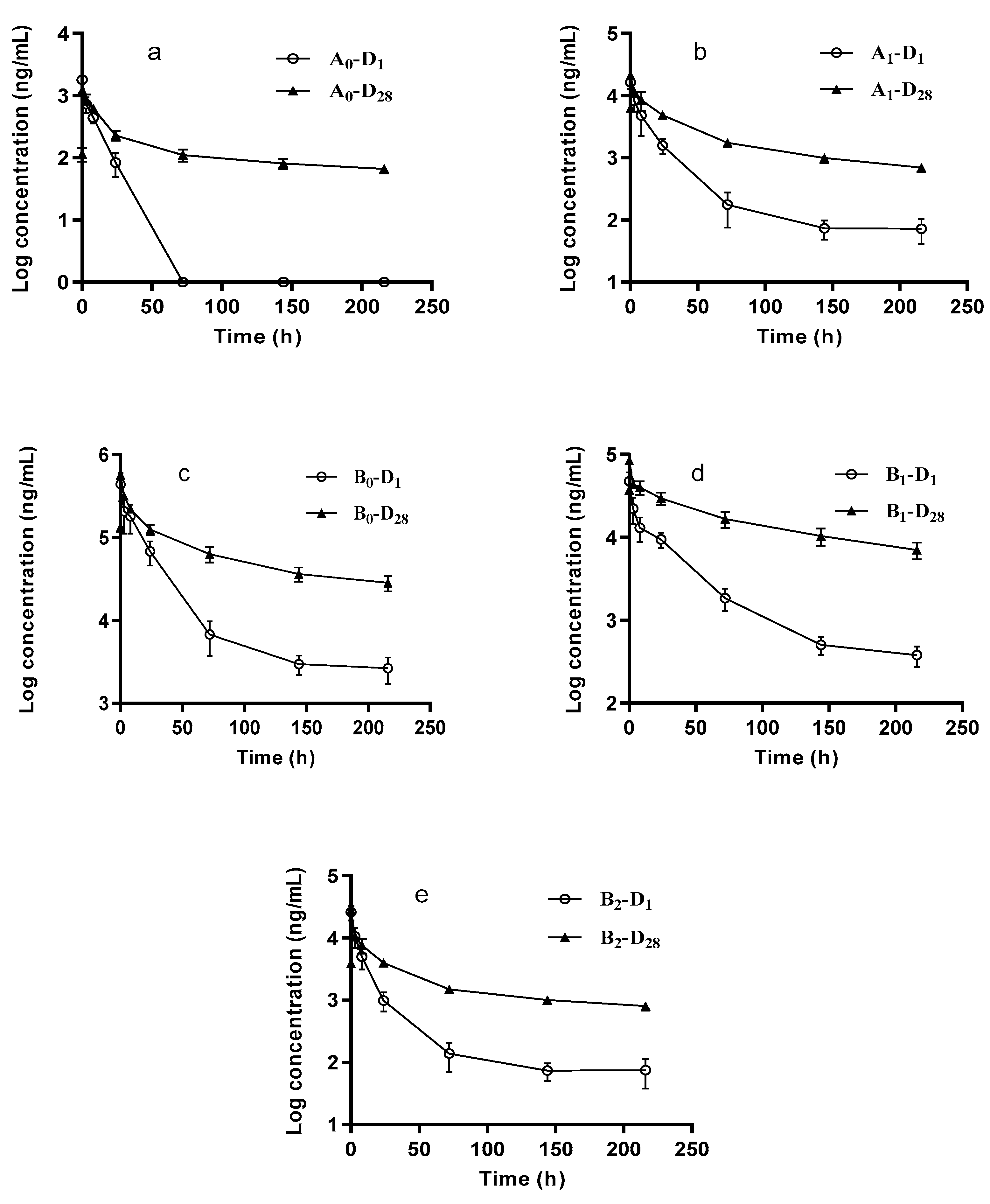
2.4. Application to Pharmacokinetic Study in Rats
3. Materials and Methods
3.1. Reagents and Materials
3.2. Standard Solutions
3.3. Animal Experiments
3.4. Sample Preparation
3.5. Liquid Chromatography-Tandem Mass Spectrometry
3.6. Method Validation
3.6.1. Specificity, Linearity, LOD, and LOQ
3.6.2. Recovery and ME
3.6.3. Intra- and Inter-Day Precision and Accuracy
3.6.4. Stability, Dilution Reliability and Residue Verification
3.7. Pharmacokinetic Study
3.8. Data Analysis
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lee, A.S.; de Lencastre, H.; Garau, J.; Kluytmans, J.; Malhotra-Kumar, S.; Peschel, A.; Harbarth, S. Methicillin-Resistant Staphylococcus aureus. Nat. Rev. Dis. Primers 2018, 4, 18033. [Google Scholar] [CrossRef] [PubMed]
- Holmes, N.E.; Tong, S.Y.C.; Davis, J.S.; van Hal, S.J. Treatment of methicillin-resistant Staphylococcus aureus: Vancomycin and beyond. Semin. Respir. Crit. Care Med. 2015, 36, 17–30. [Google Scholar] [CrossRef]
- Shariati, A.; Dadashi, M.; Chegini, Z.; van Belkum, A.; Mirzaii, M.; Khoramrooz, S.S.; Darban-Sarokhalil, D. The global prevalence of daptomycin, tigecycline, quinupristin/dalfopristin, and linezolid-resistant staphylococcus aureus and coagulase-negative staphylococci strains: A systematic review and meta-analysis. Antimicrob. Resist. Infect. Control. 2020, 9, 56. [Google Scholar] [CrossRef]
- Kim, A.; Kuti, J.L.; Nicolau, D.P. Review of dalbavancin, a novel semisynthetic lipoglycopeptide. Expert. Opin. Investig. Drugs 2007, 16, 717–733. [Google Scholar] [CrossRef]
- Soriano, A.; Rossolini, G.M.; Pea, F. The role of dalbavancin in the treatment of acute bacterial skin and skin structure infections (ABSSSIs). Expert. Rev. Anti. Infect. Ther. 2020, 18, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Mendes, R.E.; Duncan, L.R.; Flamm, R.K.; Sader, H.S. Activity of dalbavancin and comparator agents against Gram-positive cocci from clinical infections in the USA and Europe 2015–16. J. Antimicrob. Chemother. 2018, 73, 2748–2756. [Google Scholar] [CrossRef]
- Goldstein, B.P.; Selva, E.; Gastaldo, L.; Berti, M.; Pallanza, R.; Ripamonti, F.; Ferrari, P.; Denaro, M.; Arioli, V.; Cassani, G. A40926, a new glycopeptide antibiotic with anti-Neisseria activity. Antimicrob. Agents Chemother. 1987, 31, 1961–1966. [Google Scholar] [CrossRef] [PubMed]
- Candiani, G.; Abbondi, M.; Borgonovi, M.; Romanò, G.; Parenti, F. In-Vitro and in-vivo antibacterial activity of BI 397, a new semi-synthetic glycopeptide antibiotic. J. Antimicrob. Chemother. 1999, 44, 179–192. [Google Scholar] [CrossRef][Green Version]
- Dash, R.P.; Babu, R.J.; Srinivas, N.R. Review of the pharmacokinetics of dalbavancin, a recently approved lipoglycopeptide antibiotic. Infect. Dis. 2017, 49, 483–492. [Google Scholar] [CrossRef]
- Gustinetti, G.; Cangemi, G.; Bandettini, R.; Castagnola, E. Pharmacokinetic/Pharmacodynamic parameters for treatment optimization of infection due to antibiotic resistant bacteria: A summary for practical purposes in children and adults. J. Chemother. 2018, 30, 65–81. [Google Scholar] [CrossRef]
- Galluzzo, M.; D’Adamio, S.; Bianchi, L.; Talamonti, M. Pharmacokinetic drug evaluation of dalbavancin for the treatment of skin infections. Expert. Opin. Drug Metab. Toxicol. 2018, 14, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Dunne, M.W.; Talbot, G.H.; Boucher, H.W.; Wilcox, M.; Puttagunta, S. Safety of dalbavancin in the treatment of skin and skin structure infections: A pooled analysis of randomized, comparative studies. Int. J. Antimicrob. Agents Drug Saf. 2016, 39, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Rimkus, G.G.; Huth, T.; Harms, D. Screening of stereoisomeric chloramphenicol residues in honey by ELISA and CHARM®II test—The potential risk of systematically false-compliant (false negative) results. Food Addit. Contam. Part A Chem. Anal. Control Expo. Risk Assess. 2020, 37, 94–103. [Google Scholar] [CrossRef]
- Aga, D.S.; O’Connor, S.; Ensley, S.; Payero, J.O.; Snow, D.; Tarkalson, D. Determination of the persistence of tetracycline antibiotics and their degradates in manure-amended soil using enzyme-linked immunosorbent assay and liquid chromatography-mass spectrometry. J. Agric. Food Chem. 2005, 53, 7165–7171. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Yin, F.; Pan, Y.; Chen, D.; Li, J.; Wan, D.; Liu, Z.; Yuan, Z. Metabolism, distribution, and elimination of mequindox in pigs, chickens, and rats. J. Agric. Food Chem. 2015, 63, 9839–9849. [Google Scholar] [CrossRef] [PubMed]
- Hakk, H.; Shappell, N.W.; Lupton, S.J.; Shelver, W.L.; Fanaselle, W.; Oryang, D.; Yeung, C.Y.; Hoelzer, K.; Ma, Y.; Gaalswyk, D.; et al. Distribution of animal drugs between skim milk and milk fat fractions in spiked whole milk: Understanding the potential impact on commercial milk products. J. Agric. Food Chem. 2016, 64, 326–335. [Google Scholar] [CrossRef]
- Harvanová, M.; Gondová, T. New enantioselective LC method development and validation for the assay of modafinil. J. Chromatogr. Sci. 2019, 57, 204–212. [Google Scholar] [CrossRef]
- D’Orazio, G.; Fanali, C.; Gentili, A.; Tagliaro, F.; Fanali, S. Nano-Liquid chromatography for enantiomers separation of baclofen by using vancomycin silica stationary phase. J. Chromatogr. A 2019, 1605, 360358. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, D.; Tang, L.; Wang, J. Separation and characterization of unknown impurities and isomers in cefminox sodium and study of the forming mechanisms of impurities by liquid chromatography coupled with ion trap/time-of-flight mass spectrometry. J. Chromatogr. Sci. 2019, 57, 204–212. [Google Scholar] [CrossRef]
- Rashid, A.; Mazhar, S.H.; Zeng, Q.; Kiki, C.; Yu, C.P.; Sun, Q. Simultaneous analysis of multiclass antibiotic residues in complex environmental matrices by liquid chromatography with tandem quadrupole mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2020, 1145, 122103. [Google Scholar] [CrossRef]
- Xiao, X.; Wu, J.; Li, Z.; Jia, L. Enantioseparation and sensitive analysis of ofloxacin by poly(3,4-dihydroxyphenylalanine) functionalized magnetic nanoparticles-based solid phase extraction in combination with on-line concentration capillary electrophoresis. J. Chromatogr. A 2019, 1587, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Greño, M.; Castro-Puyana, M.; García, M.Á.; Marina, M.L. Analysis of antibiotics by CE and CEC and their use as chiral selectors: An update. Electrophoresis 2018, 39, 235–259. [Google Scholar] [CrossRef] [PubMed]
- Cavaleri, M.; Riva, S.; Valagussa, A.; Guanci, M.; Colombo, L.; Dowell, J.; Stogniew, M. Pharmacokinetics and excretion of dalbavancin in the rat. J. Antimicrob. Chemother. 2005, 55 (Suppl. 2), ii31–ii35. [Google Scholar] [CrossRef] [PubMed]
- Nicolau, D.P.; Sun, H.K.; Seltzer, E.; Buckwalter, M.; Dowell, J.A. Pharmacokinetics of dalbavancin in plasma and skin blister fluid. J. Antimicrob. Chemother. 2007, 60, 681–684. [Google Scholar] [CrossRef] [PubMed]
- Buckwalter, M. Population pharmacokinetic analysis of dalbavancin, a novel lipoglycopeptide. J. Clin. Pharmacol. 2005, 45, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Bradley, J.S.; Puttagunta, S.; Rubino, C.M.; Blumer, J.L.; Dunne, M.; Sullivan, J.E. Pharmacokinetics, safety and tolerability of single dose dalbavancin in children 12–17 years of age. Pediatr. Infect. Dis. J. 2015, 34, 748–752. [Google Scholar] [CrossRef]
- Alebic-Kolbah, T.; Demers, R.; Cojocaru, L. Dalbavancin: Quantification in human plasma and urine by a new improved high performance liquid chromatography-tandem mass spectrometry method. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2011, 879, 2632–2641. [Google Scholar] [CrossRef]
- Carrothers, T.J.; Chittenden, J.T.; Critchley, I. Dalbavancin population pharmacokinetic modeling and target attainment analysis. Clin. Pharm. Drug Dev. 2020, 9, 21–31. [Google Scholar] [CrossRef]
- Gonzalez, D.; Bradley, J.S.; Blumer, J.; Yogev, R.; Watt, K.M.; James, L.P.; Palazzi, D.L.; Bhatt-Mehta, V.; Sullivan, J.E.; Zhang, L.; et al. Dalbavancin pharmacokinetics and safety in children 3 months to 11 years of age. Pediatr. Infect. Dis. J. 2017, 36, 645–653. [Google Scholar] [CrossRef]
- Van Matre, E.T.; Teitelbaum, I.; Kiser, T.H. Intravenous and intraperitoneal pharmacokinetics of dalbavancin in peritoneal dialysis patients. Antimicrob. Agents Chemother. 2020, 64, e02089-19. [Google Scholar] [CrossRef]
- Corona, A.; Agarossi, A.; Veronese, A.; Cattaneo, D.; D’Avolio, A. Therapeutic drug monitoring of dalbavancin treatment in severe necrotizing fasciitis in 3 critically ill patients a grand round. Ther. Drug Monit. 2020, 42, 165–168. [Google Scholar] [CrossRef]
- Rappo, U.; Dunne, M.W.; Puttagunta, S.; Baldassarre, J.S.; Su, S.F.; Desai-Krieger, D.; Inoue, M. Epithelial lining fluid and plasma concentrations of dalbavancin in healthy adults after a single 1500-milligram infusione. Antimicrob. Agents Chemother. 2019, 63, e01024-19. [Google Scholar] [CrossRef]
- Deng, F.F.; Yu, H.; Pan, X.H.; Hu, G.Y.; Wang, Q.Q.; Peng, R.F.; Tan, L.; Yang, Z.C. Ultra-High performance liquid chromatography tandem mass spectrometry for the determination of five glycopeptide antibiotics in food and biological samples using solid-phase extraction. J. Chromatogr. A 2018, 1538, 54–59. [Google Scholar] [CrossRef]
- Desmons, A.; Thioulouse, E.; Hautem, J.Y.; Saintier, A.; Baudin, B.; Lamazière, A.; Netter, C.; Moussa, F. Direct liquid chromatography tandem mass spectrometry analysis of amino acids in human plasma. J. Chromatogr. A 2020, 17, 461135. [Google Scholar] [CrossRef]
- Lu, X.; Zhang, L.; Sun, Q.; Song, G.; Huang, J. Extraction, identification and structure-activity relationship of antioxidant peptides from sesame (Sesamum indicum L.) protein hydrolysate. Food Res. Int. 2019, 116, 707–716. [Google Scholar] [CrossRef]
- Li, Y.; Sun, M.; Mao, X.; Li, J.; Sumarah, M.W.; You, Y.; Wang, Y. Tracing major metabolites of quinoxaline-1,4-dioxides in abalone with high-performance liquid chromatography tandem positive-mode electrospray ionization mass spectrometry. J. Sci. Food Agric. 2019, 99, 5550–5557. [Google Scholar] [CrossRef]
- Cheng, C.; Liu, S.; Xiao, D.; Hollembaek, J.; Yao, L.; Lin, J.; Hansel, S. LC-MS/MS method development and validation for the determination of polymyxins and vancomycin in rat plasma. J. Chromatogr. B 2010, 878, 2831–2838. [Google Scholar] [CrossRef]
- Bioanalytical Method Validation Guidance for Industry, U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Veterinary Medicine (CVM), May 2018, Food and Drug Administration Guidance for Industry: Bioanalytical Method Validation. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioanalytical-method-validation-guidance-industry (accessed on 4 August 2020).
- European Commission. [EC] (2006b), Commission regulation (EC) no 401/2006 of 23 February 2006 laying down the methods of sampling and analysis for the official control of the levels of mycotoxins in foodstuffs. Off. J. Eur. Union 2006, L70, 12–34. [Google Scholar]
- European Commission. 2002/657/EC, Commission Decision of 12 August 2002 implementing Council directive 96/23/EC concerning the performance of analytical methods and the interpretation of results. Off. J. Eur. Commun. 2002, L221, 8–36. [Google Scholar]
Sample Availability: Samples of the compounds are not available from the authors. |
| Methods | Analytes 1 | Matrix | LOQs (μg/mL) | Reference |
|---|---|---|---|---|
| HPLC-MS/MS | B0/B1 | Rat plasma | 0.5–50 | [23] |
| HPLC-MS/MS | B0/B1 | Human plasma | 1.0–128 | [24] |
| HPLC-MS/MS | B0/B1 | Human plasma | 0.5–50/1.0–128 | [25] |
| HPLC-MS/MS | B0/B1 | Human plasma | 0.5–400 | [26] |
| HPLC-MS/MS | B0/B1 | Human Plasma | 0.5–500 | [27,28,29,30] |
| HPLC-MS | B0/B1 | Human Plasma | 0.7–500 | [31] |
| LC-MS/MS | B0/B1 | Human Plasma | 0.5–500 | [32] |
| UHPLC-MS/MS | B0/B1 | Rat serum | 0.002–0.02 | [33] |
| UHPLC-MS/MS | A0, A1, B0, B1, B2 | Rat plasma | 0.05–2.5 | Present study |
| Analytes | MS Conditions | Retention Time (min) | |||
|---|---|---|---|---|---|
| Precursor Ion (m/z) 1 | Product Ion (m/z) 2 | Cone Voltage (V) | Collision Energy (eV) | ||
| A0 | 902.19 | 84.15 | 54 | 52 | 3.20 |
| A1 | 902.25 | 84.16 | 54 | 52 | 3.42 |
| B0 | 909.21 | 83.91 | 64 | 50 | 4.69 |
| B1 | 909.29 | 84.15 | 64 | 50 | 5.03 |
| B2 | 916.25 | 84.17 | 15 | 58 | 4.92 |
| IS | 913.13 | 158.21 | 64 | 48 | 4.69 |
| Analytes | Linear Range (ng/mL) | LODs (ng/mL) | LLOQs (ng/mL) | Regression Equation | R² |
|---|---|---|---|---|---|
| A0 | 50–2500 | 10 | 50 | y = 0.0033x + 0.0110 | 0.9997 |
| A1 | 50–2500 | 5 | 50 | y = 0.0031x + 0.0183 | 0.9999 |
| B0 | 50–2500 | 5 | 50 | y = 0.0038x + 0.0246 | 0.9998 |
| B1 | 50–2500 | 10 | 50 | y = 0.0038x + 0.0168 | 0.9999 |
| B2 | 50–2500 | 10 | 50 | y = 0.0037x − 0.0228 | 0.9990 |
| Compound | Concentration (ng/mL) | Precision (RSD, %) | Accuracy (RE, %) | ||
|---|---|---|---|---|---|
| Inter-Assay | Intra-Assay | Inter-Assay | Intra-Assay | ||
| A0 | 50 | 2.38–5.96 | 5.49 | 98.8–107.6 | 103.8 |
| 150 | 2.04–4.42 | 4.97 | 96.8−105.9 | 102.1 | |
| 500 | 1.86–2.74 | 2.62 | 98.9−102.1 | 100.9 | |
| 2000 | 1.48–5.99 | 4.13 | 102.6–105.1 | 103.9 | |
| A1 | 50 | 5.78–7.72 | 6.36 | 96.5–106.8 | 100.9 |
| 150 | 1.42–2.53 | 6.10 | 92.4–105.9 | 99.8 | |
| 500 | 0.97–2.88 | 4.77 | 92.2–101.4 | 98.1 | |
| 2000 | 1.27–4.74 | 4.86 | 95.1–103.3 | 99.8 | |
| B0 | 50 | 5.41–7.51 | 6.51 | 97.4–106.1 | 102.8 |
| 150 | 0.98–4.00 | 4.08 | 99.0–107.3 | 103.2 | |
| 500 | 1.45–4.98 | 3.08 | 102.4–102.8 | 102.6 | |
| 2000 | 0.72–3.57 | 3.12 | 103.3–108.0 | 104.9 | |
| B1 | 50 | 3.04–7.32 | 5.91 | 98.5–107.5 | 103.5 |
| 150 | 3.54–5.49 | 6.78 | 97.8–109.9 | 104.4 | |
| 500 | 1.43–9.84 | 6.60 | 105.0–109.1 | 106.7 | |
| 2000 | 1.79−5.87 | 3.68 | 104.4–106.9 | 105.3 | |
| B2 | 50 | 5.47–6.66 | 6.15 | 98.1–105.0 | 102.2 |
| 150 | 1.34–3.60 | 4.40 | 98.8–108.0 | 103.1 | |
| 500 | 1.53–3.72 | 2.90 | 99.3–102.8 | 100.8 | |
| 2000 | 0.47–5.52 | 3.37 | 100.5–103.6 | 101.8 | |
| Stage | Parameters | Components | ||||
|---|---|---|---|---|---|---|
| A0 | A1 | B0 | B1 | B2 | ||
| D1 | AUC(0–t) (μg/mL·h) | 10.5 ± 2.6 | 155.4 ± 79.9 | 5776.5 ± 2593.2 | 688.2 ± 272.2 | 163.7 ± 79.5 |
| AUC(0–∞) (μg/mL·h) | 11.8 ± 2.6 | 173.1 ± 65.6 | 6566.7 ± 1820.3 | 756.2 ± 191.4 | 187.2 ± 61.2 | |
| T1/2 (h) | 6.5 ± 0.6 | 27.5 ± 11.4 | 74.6 ± 45.9 | 29.1 ± 1.1 | 87.3 ± 68.9 | |
| Cmax (μg/mL) | 1.8 ± 0.2 | 14.8 ± 6.1 | 437.3 ± 160.3 | 42.9 ± 18.9 | 23.4 ± 10.4 | |
| MRT(0–t) (h) | 5.6 ± 0.3 | 17.0 ± 3.8 | 23.0 ± 0.9 | 32.3 ± 1.5 | 16.2 ± 2.4 | |
| Vz (L/kg) | 32.9 ± 5.7 | 9.4 ± 3.3 | 0.7 ± 0.5 | 2.3 ± 0.4 | 28.0 ± 23.0 | |
| D28 | AUC(0–t) (μg/mL·h) | 34.0 ± 4.5 *** | 524.7 ± 32.8 *** | 15,781.3 ± 1980.4 *** | 3593.7 ± 6,02.1 *** | 482.4 ± 35.2 *** |
| AUC(0–∞) (μg/mL·h) | 49.5 ± 8.6 *** | 631.0 ± 41.8 *** | 18,543.8 ± 2839.6 *** | 4333.9 ± 848.9 *** | 646.0 ± 53.3 *** | |
| T1/2 (h) | 1,67.1 ± 32.0 *** | 109.5 ± 10.6 *** | 88.8 ± 34.5 | 87.0 ± 27.5 *** | 152.8 ± 43.0 * | |
| C0 (μg/mL) | 0.1 ± 0.0 | 6.3 ± 0.7 | 132.6 ± 15.7 | 37.1 ± 4.1 | 3.9 ± 0.5 | |
| Cmax (μg/mL) | 1.2 ± 0.2 *** | 21.1 ± 1.6 *** | 571.5 ± 67.4 * | 84.3 ± 7.4 *** | 28.0 ± 2.6 | |
| MRT(0–t) (h) | 60.7 ± 2.7 *** | 53.0 ± 5.2 *** | 62.0 ± 3.7 *** | 68.6 ± 8.2 *** | 55.7 ± 4.7 *** | |
| Vz (L/kg) | 196.0 ± 27.3 *** | 10.1 ± 1.3 | 0.3 ± 0.1 * | 1.2 ± 0.4 *** | 13.5 ± 3.4 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, D.; Ping, L.; Hong, Y.; Shen, J.; Weng, Q.; He, Q. Simultaneous Quantification and Pharmacokinetic Study of Five Homologs of Dalbavancin in Rat Plasma Using UHPLC-MS/MS. Molecules 2020, 25, 4100. https://doi.org/10.3390/molecules25184100
Zhu D, Ping L, Hong Y, Shen J, Weng Q, He Q. Simultaneous Quantification and Pharmacokinetic Study of Five Homologs of Dalbavancin in Rat Plasma Using UHPLC-MS/MS. Molecules. 2020; 25(18):4100. https://doi.org/10.3390/molecules25184100
Chicago/Turabian StyleZhu, Difeng, Li Ping, Yawen Hong, Jiale Shen, Qinjie Weng, and Qiaojun He. 2020. "Simultaneous Quantification and Pharmacokinetic Study of Five Homologs of Dalbavancin in Rat Plasma Using UHPLC-MS/MS" Molecules 25, no. 18: 4100. https://doi.org/10.3390/molecules25184100
APA StyleZhu, D., Ping, L., Hong, Y., Shen, J., Weng, Q., & He, Q. (2020). Simultaneous Quantification and Pharmacokinetic Study of Five Homologs of Dalbavancin in Rat Plasma Using UHPLC-MS/MS. Molecules, 25(18), 4100. https://doi.org/10.3390/molecules25184100






