Cranberry Polyphenols and Prevention against Urinary Tract Infections: Relevant Considerations
Abstract
1. Introduction
2. UTIs Pathogenesis
3. UPEC and Other Uropathogenic Bacteria
4. Cranberry in UTIs Prophylaxis
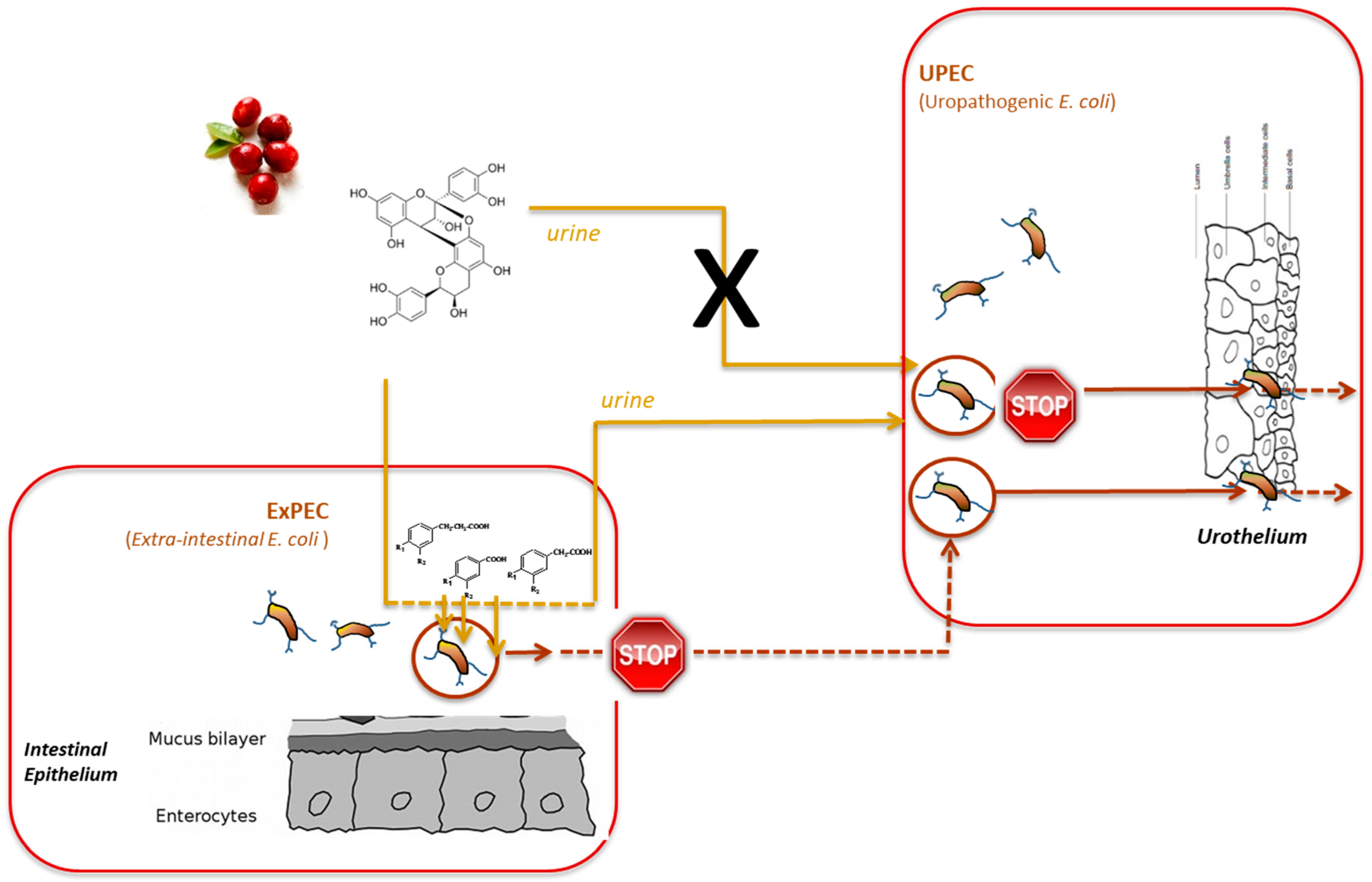
5. Antiadherence Activity Derived from Cranberry Consumption
6. Other Potential Mechanisms Involved in Cranberry Efficiency against UTIs
7. Combined Action of Cranberry and Probiotics against UTIs
8. Conclusions
Funding
Conflicts of Interest
References
- Foxman, B. Urinary tract infection syndromes. Infect. Dis. Clin. N. Am. 2014, 28, 1–13. [Google Scholar] [CrossRef]
- Sivick, K.E.; Mobley, H.L.T. Waging war against uropathogenic escherichia coli: Winning back the urinary tract. Infect. Immun. 2010, 78, 568–585. [Google Scholar] [CrossRef]
- Baron, E.J.; Miller, J.M.; Weinstein, M.P.; Richter, S.S.; Gilligan, P.H.; Thomson, R.B.; Bourbeau, P.; Carroll, K.C.; Kehl, S.C.; Dunne, W.M.; et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2013 recommendations by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM) a. Clin. Infect. Dis. 2013, 57, 22–121. [Google Scholar] [CrossRef]
- Luís, Â.; Domingues, F.; Pereira, L. Can cranberries contribute to reduce the incidence of urinary tract infections? A systematic review with meta-analysis and trial sequential analysis of clinical trials. J. Urol. 2017, 198, 614–621. [Google Scholar] [CrossRef]
- Spaulding, C.; Hultgren, S. Adhesive pili in UTI pathogenesis and drug development. Pathogens 2016, 5, 30. [Google Scholar] [CrossRef]
- Lane, M.C.; Mobley, H.L.T. Role of P-fimbrial-mediated adherence in pyelonephritis and persistence of uropathogenic Escherichia coli (UPEC) in the mammalian kidney. Kidney Int. 2007, 72, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Scholes, D.; Hooton, T.M.; Roberts, P.L.; Gupta, K.; Stapleton, A.E.; Stamm, W.E. Risk factors associated with acute pyelonephritis in healthy women. Ann. Intern. Med. 2005, 142, 20. [Google Scholar] [CrossRef] [PubMed]
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef] [PubMed]
- Tamadonfar, K.O.; Omattage, N.S.; Spaulding, C.N.; Hultgren, S.J. Reaching the end of the line: Urinary tract infections. Microbiol. Spectr. 2019, 7, 1–16. [Google Scholar]
- Nik-Ahd, F.; Lenore Ackerman, A.; Anger, J. Recurrent urinary tract infections in females and the overlap with overactive bladder. Curr. Urol. Rep. 2018, 19, 94. [Google Scholar] [CrossRef]
- Beerepoot, M.; Geerlings, S. Non-antibiotic prophylaxis for urinary tract infections. Pathogens 2016, 5, 36. [Google Scholar] [CrossRef] [PubMed]
- Jepson, R.G.; Williams, G.; Craig, J.C. Cranberries for preventing urinary tract infections. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-H.; Fang, C.-C.; Chen, N.-C.; Liu, S.S.-H.; Yu, P.-H.; Wu, T.-Y.; Chen, W.-T.; Lee, C.-C.; Chen, S.-C. Cranberry-containing products for prevention of urinary tract infections in susceptible populations. Arch. Intern. Med. 2012, 172, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, J.B.; Camesano, T.A.; Cassidy, A.; Kris-etherton, P.; Howell, A.; Manach, C.; Ostertag, L.M.; Sies, H.; Skulas-ray, A.; Vita, J.A. Cranberries and their bioactive constituents in human health. Adv. Nutr. 2013, 4, 618–632. [Google Scholar] [CrossRef] [PubMed]
- Vasileiou, I.; Katsargyris, A.; Theocharis, S.; Giaginis, C. Current clinical status on the preventive effects of cranberry consumption against urinary tract infections. Nutr. Res. 2013, 33, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Occhipinti, A.; Germano, A.; Maffei, M.E. Prevention of urinary tract infection with oximacro, a cranberry extract with a high content of A-type proanthocyanidins: A pre-clinical double-blind controlled study. Urol. J. 2016, 13, 2640–2649. [Google Scholar]
- Maki, K.C.; Kaspar, K.L.; Khoo, C.; Derrig, L.H.; Schild, A.L.; Gupta, K. Consumption of a cranberry juice beverage lowered the number of clinical urinary tract infection episodes in women with a recent history of urinary tract infection. Am. J. Clin. Nutr. 2016, 103, 1434–1442. [Google Scholar] [CrossRef]
- Foxman, B.; Cronenwett, A.E.W.; Spino, C.; Berger, M.B.; Morgan, D.M. Cranberry juice capsules and urinary tract infection after surgery: Results of a randomized trial. Am. J. Obs. Gynecol. 2015, 213, 194.e1–194.e8. [Google Scholar] [CrossRef]
- Stapleton, A.E.; Dziura, J.; Hooton, T.M.; Cox, M.E.; Yarova-Yarovaya, Y.; Chen, S.; Gupta, K. Recurrent urinary tract infection and urinary Escherichia coli in women ingesting cranberry juice daily: A randomized controlled trial. Mayo Clin. Proc. 2012, 87, 143–150. [Google Scholar] [CrossRef]
- Liu, H.; Howell, A.B.; Zhang, D.J.; Khoo, C. A randomized, double-blind, placebo-controlled pilot study to assess bacterial anti-adhesive activity in human urine following consumption of a cranberry supplement. Food Funct. 2019, 10, 7645–7652. [Google Scholar] [CrossRef]
- Pappas, E.; Schaich, K.M. Phytochemicals of cranberries and cranberry products: Characterization, potential health effects, and processing stability. Crit. Rev. Food Sci. Nutr. 2009, 49, 741–781. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Patán, F.; Bartolomé, B.; Martín-Alvarez, P.J.; Anderson, M.; Howell, A.; Monagas, M. Comprehensive assessment of the quality of commercial cranberry products. Phenolic characterization and in vitro bioactivity. J. Agric. Food Chem. 2012, 60, 3396–3408. [Google Scholar] [CrossRef] [PubMed]
- González de Llano, D.; Liu, H.; Khoo, C.; Moreno-Arribas, M.V.; Bartolomé, B. Some new findings regarding the antiadhesive activity of cranberry phenolic compounds and their microbial-derived metabolites against uropathogenic bacteria. J. Agric. Food Chem. 2019, 67, 2166–2174. [Google Scholar] [CrossRef] [PubMed]
- Howell, A.B. Bioactive compounds in cranberries and their role in prevention of urinary tract infections. Mol. Nutr. Food Res. 2007, 51, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Ermel, G.; Georgeault, S.; Inisan, C.; Besnard, M. Inhibition of adhesion of uropathogenic escherichia coli bacteria to uroepithelial cells by extracts from cranberry. J. Med. Food 2012, 15, 126–134. [Google Scholar] [CrossRef]
- De Llano, D.G.; Esteban-Fernández, A.; Sánchez-Patán, F.; Martín-Álvarez, P.J.; Moreno-Arribas, M.V.; Bartolomé, B. Anti-adhesive activity of cranberry phenolic compounds and their microbial-derived metabolites against uropathogenic escherichia coli in bladder epithelial cell cultures. Int. J. Mol. Sci. 2015, 16, 12119–12130. [Google Scholar] [CrossRef]
- de Llano, D.G.; Arroyo, A.; Cárdenas, N.; Rodríguez, J.M.; Moreno-Arribas, M.V.; Bartolomé, B. Strain-specific inhibition of the adherence of uropathogenic bacteria to bladder cells by probiotic Lactobacillus spp. Pathog. Dis. 2017, 75, 1–8. [Google Scholar] [CrossRef]
- Mena, P.; González de Llano, D.; Brindani, N.; Esteban-Fernández, A.; Curti, C.; Moreno-Arribas, M.V.; Del Rio, D.; Bartolomé, B. 5-(3′,4′-Dihydroxyphenyl)-γ-valerolactone and its sulphate conjugates, representative circulating metabolites of flavan-3-ols, exhibit anti-adhesive activity against uropathogenic Escherichia coli in bladder epithelial cells. J. Funct. Foods 2017, 29, 275–280. [Google Scholar] [CrossRef]
- Al-Ghazzewi, F.H.; Tester, R.F. Biotherapeutic agents and vaginal health. J. Appl. Microbiol. 2016, 121, 18–27. [Google Scholar] [CrossRef]
- Reid, G. The development of probiotics for women’s health. Can. J. Microbiol. 2017, 63, 269–277. [Google Scholar] [CrossRef]
- Stapleton, A.E.; Au-Yeung, M.; Hooton, T.M.; Fredricks, D.N.; Roberts, P.L.; Czaja, C.A.; Yarova-Yarovaya, Y.; Fiedler, T.; Cox, M.; Stamm, W.E. Randomized, placebo-controlled phase 2 trial of a lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin. Infect. Dis. 2011, 52, 1212–1217. [Google Scholar] [CrossRef] [PubMed]
- Montorsi, F.; Gandaglia, G.; Salonia, A.; Briganti, A.; Mirone, V. Effectiveness of a combination of cranberries, lactobacillus rhamnosus, and Vitamin C for the management of recurrent urinary tract infections in women: Results of a pilot study. Eur. Urol. 2016, 70, 912–915. [Google Scholar] [CrossRef] [PubMed]
- Barrons, R.; Tassone, D. Use of Lactobacillus probiotics for bacterial genitourinary infections in women: A review. Clin. Ther. 2008, 30, 453–468. [Google Scholar] [CrossRef] [PubMed]
- Scholes, D.; Hawn, T.R.; Roberts, P.L.; Li, S.S.; Stapleton, A.E.; Zhao, L.-P.; Stamm, W.E.; Hooton, T.M. Family history and risk of recurrent cystitis and pyelonephritis in women. J. Urol. 2010, 184, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Beerepoot, M.A.J. Lactobacilli vs. antibiotics to prevent urinary tract infections. Arch. Intern. Med. 2012, 172, 704. [Google Scholar] [CrossRef]
- Mulvey, M.A. Adhesion and entry of uropathogenic Escherichia coli. Cell. Microbiol. 2002, 4, 257–271. [Google Scholar] [CrossRef]
- Jagannathan, V.; Viswanathan, P. Proanthocyanidins—Will they effectively restrain conspicuous bacterial strains devolving on urinary tract infection? J. Basic Microbiol. 2018, 58, 567–578. [Google Scholar] [CrossRef]
- Whiteside, S.A.; Razvi, H.; Dave, S.; Reid, G.; Burton, J.P. The microbiome of the urinary tract—A role beyond infection. Nat. Rev. Urol. 2015, 12, 81–90. [Google Scholar] [CrossRef]
- Kline, K.A.; Lewis, A.L. Gram-positive uropathogens, polymicrobial urinary tract infection, and the emerging microbiota of the urinary tract. Microbiol. Spectr. 2016, 4, 1–54. [Google Scholar] [CrossRef]
- Alam Parvez, S.; Rahman, D. Virulence factors of uropathogenic E. coli. In Microbiology of Urinary Tract Infections-Microbial Agents and Predisposing Factors; IntechOpen: Hamilton, NJ, USA, 2019. [Google Scholar]
- Ismail, M.D.; Ali, I.; Hatt, S.; Salzman, E.A.; Cronenwett, A.W.; Marrs, C.F.; Rickard, A.H.; Foxman, B. Association of Escherichia coli ST131 lineage with risk of urinary tract infection recurrence among young women. J. Glob. Antimicrob. Resist. 2018, 13, 81–84. [Google Scholar] [CrossRef]
- Mantzorou, M.; Giaginis, C. Cranberry consumption against urinary tract infections: Clinical stateof—the-art and future perspectives. Curr. Pharm. Biotechnol. 2019, 19, 1049–1063. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, A.J.; Amundsen, S.K.; Jones, J.M. Effect of carbohydrates on adherence of Escherichia coli to human urinary tract epthelial cells. Infect. Immun. 1980, 30, 531–537. [Google Scholar] [PubMed]
- Rossi, R.; Porta, S.; Canovi, B. Overview on cranberry and urinary tract infections in females. J. Clin. Gastroenterol. 2010, 44, S61–S62. [Google Scholar] [CrossRef] [PubMed]
- Vigil, P.D.; Alteri, C.J.; Mobley, H.L.T. Identification of in vivo -induced antigens including an RTX family exoprotein required for uropathogenic Escherichia coli virulence. Infect. Immun. 2011, 79, 2335–2344. [Google Scholar] [CrossRef]
- Stærk, K.; Khandige, S.; Kolmos, H.J.; Møller-Jensen, J.; Andersen, T.E. Uropathogenic Escherichia coli express Type 1 fimbriae only in surface adherent populations under physiological growth conditions. J. Infect. Dis. 2016, 213, 386–394. [Google Scholar] [CrossRef][Green Version]
- Andreu, A. Patogenia de las infecciones del tracto urinario. Enferm. Infecc. Microbiol. Clin. 2005, 23, 15–21. [Google Scholar] [CrossRef]
- Soltani, S.; Emamie, A.D.; Dastranj, M.; Farahani, A. Role of toxins of uropathogenic Escherichia coli in development of urinary role of toxins of uropathogenic escherichia coli in development of urinary tract infection. J. Pharm. Res. Int. 2018, 1–11. [Google Scholar] [CrossRef]
- Matulay, J.T.; Mlynarczyk, C.M.; Cooper, K.L. Urinary tract infections in women: Pathogenesis, diagnosis, and management. Curr. Bladder Dysfunct. Rep. 2016, 11, 53–60. [Google Scholar] [CrossRef]
- Rodriguez-Mateos, A.; Vauzour, D.; Krueger, C.G.; Shanmuganayagam, D.; Reed, J.; Calani, L.; Mena, P.; Del Rio, D.; Crozier, A. Bioavailability, bioactivity and impact on health of dietary flavonoids and related compounds: An update. Arch. Toxicol. 2014, 88, 1803–1853. [Google Scholar] [CrossRef]
- Kimble, L.L.; Mathison, B.D.; Kaspar, K.L.; Khoo, C.; Chew, B.P. Development of a fluorometric microplate antiadhesion assay using uropathogenic escherichia coli and human uroepithelial cells. J. Nat. Prod. 2014, 77, 1102–1110. [Google Scholar] [CrossRef]
- Juthani-Mehta, M.; Van Ness, P.H.; Bianco, L.; Rink, A.; Rubeck, S.; Ginter, S.; Argraves, S.; Charpentier, P.; Acampora, D.; Trentalange, M.; et al. Effect of cranberry capsules on bacteriuria plus pyuria among older women in nursing homes. JAMA 2016, 316, 1879–1887. [Google Scholar] [CrossRef] [PubMed]
- Chughtai, B.; Howell, A.B.; Thomas, D.; Blumberg, J.B. Efficacy of cranberry in preventing recurrent urinary tract infections: Have we learned anything new? Urology 2017, 103, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Rafsanjany, N.; Lechtenberg, M.; Petereit, F.; Hensel, A. Antiadhesion as a functional concept for protection against uropathogenic Escherichia coli: In vitro studies with traditionally used plants with antiadhesive activity against uropathognic Escherichia coli. J. Ethnopharmacol. 2013, 145, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Monagas, M.; Urpi-Sarda, M.; Sánchez-Patán, F.; Llorach, R.; Garrido, I.; Gómez-Cordovés, C.; Andres-Lacueva, C.; Bartolomé, B. Insights into the metabolism and microbial biotransformation of dietary flavan-3-ols and the bioactivity of their metabolites. Food Funct. 2010, 1, 233–253. [Google Scholar] [CrossRef] [PubMed]
- Feliciano, R.P.; Boeres, A.; Massacessi, L.; Istas, G.; Heiss, C.; Ventura, M.R.; Rodriguez-mateos, A. Identi fi cation and quanti fi cation of novel cranberry-derived plasma and urinary (poly) phenols. Arch. Biochem. Biophys. 2016, 599, 31–41. [Google Scholar] [CrossRef]
- Feliciano, R.P.; Mills, C.E.; Istas, G.; Heiss, C.; Rodriguez-Mateos, A. Absorption, metabolism and excretion of cranberry (poly)phenols in humans: A dose response study and assessment of inter-individual variability. Nutrients 2017, 9, 268. [Google Scholar] [CrossRef]
- Peron, G.; Pellizzaro, A.; Brun, P.; Schievano, E.; Mammi, S.; Sut, S.; Castagliuolo, I.; Dall’Acqua, S. Antiadhesive activity and metabolomics analysis of rat urine after cranberry (vaccinium macrocarpon aiton) administration. J. Agric. Food Chem. 2017, 65, 5657–5667. [Google Scholar] [CrossRef]
- Baron, G.; Altomare, A.; Regazzoni, L.; Fumagalli, L.; Artasensi, A.; Borghi, E.; Ottaviano, E.; Del Bo, C.; Riso, P.; Allegrini, P.; et al. Profiling vaccinium macrocarpon components and metabolites in human urine and the urine ex-vivo effect on Candida albicans adhesion and biofilm-formation. Biochem. Pharm. 2020, 173, 113726. [Google Scholar] [CrossRef]
- Domenici, L.; Monti, M.; Bracchi, C.; Giorgini, M.; Colagiovanni, V.; Muzii, L.; Benedetti Panici, P. D-mannose: A promising support for acute urinary tract infections in women. A pilot study. Eur. Rev. Med. Pharm. Sci. 2016, 20, 2920–2925. [Google Scholar]
- Hong, V.; Wrolstad, R.E. Cranberry juice composition. J. Assoc. Off. Anal. Chem. 1986, 69, 199–207. [Google Scholar] [CrossRef]
- Jensen, H.D.; Struve, C.; Christensen, S.B.; Krogfelt, K.A. Cranberry juice and combinations of its organic acids are effective against experimental urinary tract infection. Front. Microbiol. 2017, 8, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Patan, F.; Barroso, E.; Van De Wiele, T.; Jimenez-Giron, A.; Martin-Alvarez, P.J.; Moreno-Arribas, M.V.; Martinez-Cuesta, C.; Pelaez, C.; Requena, T.B. Comparative in vitro fermentations of cranberry and grape seed polyphenols with colonic microbiota. Food Chem. 2015, 183, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Scharf, B.; Sendker, J.; Dobrindt, U.; Hensel, A. Influence of cranberry extract on tamm-horsfall protein in human urine and its antiadhesive activity against uropathogenic Escherichia coli. Planta Med. 2019, 85, 126–138. [Google Scholar] [CrossRef] [PubMed]
- Scharf, B.; Schmidt, T.J.; Rabbani, S.; Stork, C.; Dobrindt, U.; Sendker, J.; Ernst, B.; Hensel, A. Antiadhesive natural products against uropathogenic E. coli: What can we learn from cranberry extract ? J. Ethnopharmacol. 2020, 257, 112889. [Google Scholar] [CrossRef]
- Sekirov, I.; Russell, S.L.; Antunes, C.M.; Finlay, B.B. Gut microbiota in health and disease. Physiol. Rev. 2010, 90, 859–904. [Google Scholar] [CrossRef]
- Magistro, G.; Stief, C.G. The urinary tract microbiome: The answer to all our open questions? Eur. Urol. Focus 2019, 5, 36–38. [Google Scholar] [CrossRef]
- Aragón, I.M.; Herrera-Imbroda, B.; Queipo-Ortuño, M.I.; Castillo, E.; Del Moral, J.S.-G.; Gómez-Millán, J.; Yucel, G.; Lara, M.F. The urinary tract microbiome in health and disease. Eur. Urol. Focus 2018, 4, 128–138. [Google Scholar] [CrossRef]
- Stapleton, A.E. The vaginal microbiota and urinary tract infection. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef]
- Bekiares, N.; Krueger, C.G.; Meudt, J.J.; Shanmuganayagam, D.; Reed, J.D. Effect of sweetened dried cranberry consumption on urinary proteome and fecal microbiome in healthy human subjects. Omics J. Integr. Biol. 2017, 21, 1–9. [Google Scholar] [CrossRef]
- Rodríguez-morató, J.; Matthan, N.R.; Liu, J.; De, R.; Chen, C.O. ScienceDirect cranberries attenuate animal-based diet-induced changes in microbiota composition and functionality: A randomized crossover controlled feeding trial. J. Nutr. Biochem. 2018, 62, 76–86. [Google Scholar] [CrossRef]
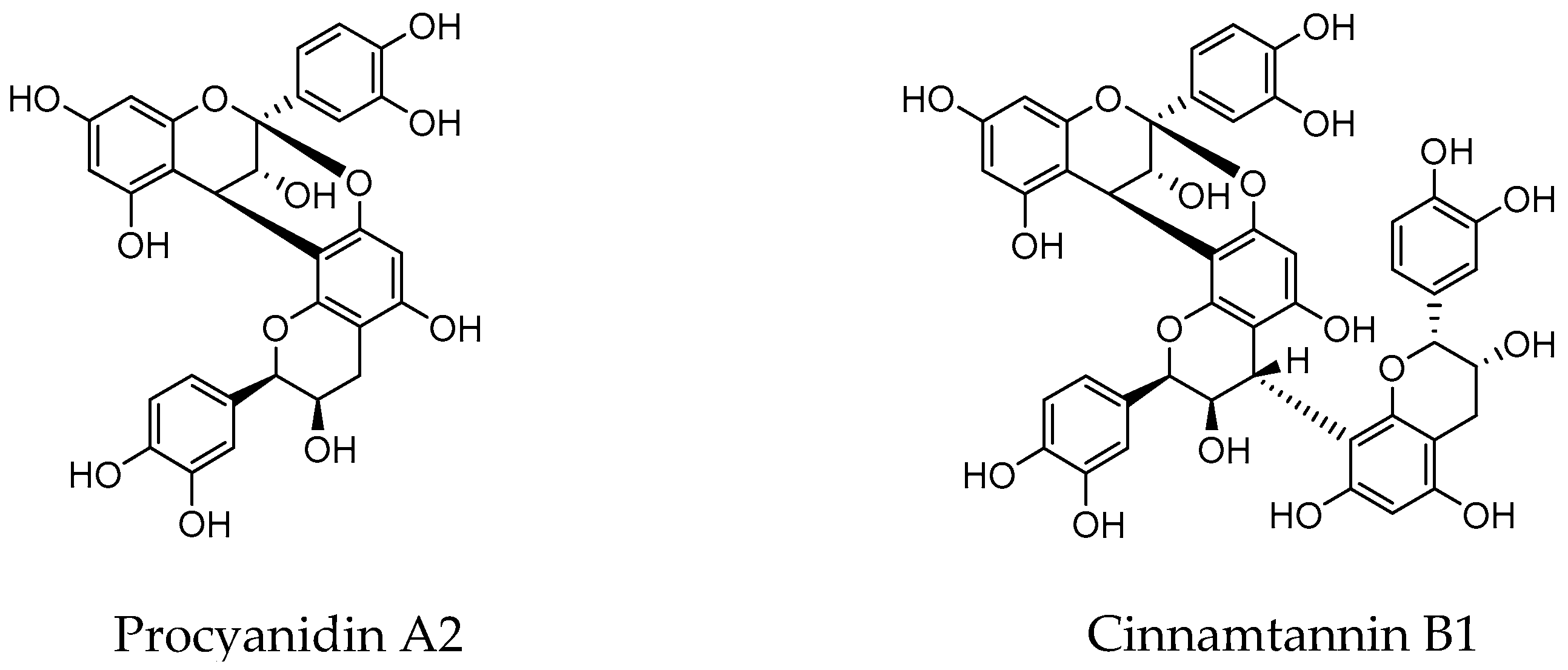
- Feliciano, R.P.; Meudt, J.J.; Shanmuganayagam, D.; Krueger, C.G.; Reed, J.D. Ratio of “a-type” to “b-type” proanthocyanidin interflavan bonds affects extra-intestinal pathogenic escherichia coli invasion of gut epithelial cells. J. Agric. Food Chem. 2014, 62, 3919–3925. [Google Scholar] [CrossRef] [PubMed]
- van Duynhoven, J.; van der Hooft, J.J.J.; van Dorsten, F.A.; Peters, S.; Foltz, M.; Gomez-Roldan, V.; Vervoort, J.; de Vos, R.C.H.; Jacobs, D.M. Rapid and sustained systemic circulation of conjugated gut microbial catabolites after single-dose black tea extract consumption. J. Proteome Res. 2014, 2, 2668–2678. [Google Scholar] [CrossRef] [PubMed]
- Dueñas, M.; Cueva, C.; Muñoz-gonzález, I.; Jiménez-girón, A.; Sánchez-patán, F.; Santos-buelga, C.; Moreno-arribas, M.V.; Bartolomé, B. Studies on modulation of gut microbiota by wine polyphenols: From isolated cultures to omic approaches. Antioxidants 2015, 4, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.R.; Russo, T.A.; Brown, J.J.; Stapleton, A. papG alleles of Escherichia coli strains causing first-episode or recurrent acute cystitis in adult women. J. Infect. Dis. 1998, 177, 97–101. [Google Scholar] [CrossRef][Green Version]
- Álvarez-Calatayud, G.; Suárez, E.; Rodríguez, J.M.; Pérez-Moreno, J. La microbiota en la mujer; aplicaciones clínicas de los probióticos. Nutr. Hosp. 2015, 32, 56–61. [Google Scholar]
- Reid, G.; Beuerman, D.; Heinemann, C.; Bruce, A.W. Probiotic Lactobacillus dose required to restore and maintain a normal vaginal flora. FEMS Immunol. Med. Microbiol. 2001, 32, 37–41. [Google Scholar] [CrossRef]
- Rodríguez, J.M. The origin of human milk bacteria: Is there a bacterial entero-mammary pathway during late pregnancy and lactation? Adv. Nutr. 2014, 5, 779–784. [Google Scholar] [CrossRef]
- Kontiokari, T.; Laitinen, J.; Järvi, L.; Pokka, T.; Sundqvist, K.; Uhari, M. Dietary factors protecting women from urinary tract infection. Am. J. Clin. Nutr. 2003, 77, 600–604. [Google Scholar] [CrossRef]
- Osset, J.; Bartolomé, R.M.; García, E.; Andreu, A. Assessment of the capacity of lactobacillus to inhibit the growth of uropathogens and block their adhesion to vaginal epithelial cells. J. Infect. Dis. 2001, 183, 485–491. [Google Scholar] [CrossRef]
- Castro, J.; Henriques, A.; Machado, A.; Henriques, M.; Jefferson, K.K.; Cerca, N.; Whiteside, S.A.; Razvi, H.; Dave, S.; Reid, G.; et al. Effect of two probiotic strains of Lactobacillus on in vitro adherence of listeria monocytogenes, streptococcus agalactiae, and staphylococcus aureus to vaginal epithelial cells. Arch. Gynecol. Obs. 2014, 12, 479–489. [Google Scholar]
- Delley, M.; Bruttin, A.; Richard, M.; Affolter, M.; Rezzonico, E.; Brück, W.M. In vitro activity of commercial probiotic Lactobacillus strains against uropathogenic Escherichia coli. FEMS Microbiol. Lett. 2015, 362, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bruce, A.W.; Reid, G. Intravaginal instillation of lactobacilli for prevention of recurrent urinary tract infections. Can. J. Microbiol. 1988, 34, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Saxelin, M.; Pessi, T.; Salminen, S. Fecal recovery following oral administration of Lactobacillus strain GG (ATCC 53103) in gelatine capsules to healthy volunteers. Int. J. Food Microbiol. 1995, 25, 199–203. [Google Scholar] [CrossRef]
- Hagan, E.C.; Mobley, H.L.T. Heme acquisition is facilitated by a novel receptor Hma and required by uropathogenic Escherichia coli for kidney infection. Mol. Microbiol. 2009, 71, 79–91. [Google Scholar] [CrossRef]
- Cadieux, P.A.; Burton, J.; Devillard, E.; Reid, G. Lactobacillus by-products inhibit the growth and virulence of uropathogenic Escherichia coli. J. Physiol. Pharm. 2009, 60 (Suppl. 6), 13–18. [Google Scholar]
- Rupasinghe, H.P.V.; Parmar, I.; Neir, S.V. Biotransformation of cranberry proanthocyanidins to probiotic metabolites by lactobacillus rhamnosus enhances their anticancer activity in HepG2 cells in vitro. Oxid. Med. Cell Longev. 2019, 2019, 1–14. [Google Scholar] [CrossRef]
- Peter, M.G.; Paulina, M.K.; Waleed, A.; Alison, E.F.-R. Lactobacillus for preventing recurrent urinary tract infections in women: Meta-analysis. Can. J. Urol. 2013, 20, 6607–6614. [Google Scholar]
- Schwenger, E.M.; Tejani, A.M.; Loewen, P.S. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst. Rev. 2015, 12. [Google Scholar] [CrossRef]
- Ahumada-cota, R.E.; Hernandez-chiñas, U.; Mili, F.; Ch, E.; Navarro-ocaña, A.; Mart, D. Effect and analysis of bacterial lysates for the treatment of recurrent urinary tract infections in adults. Pathogens 2020, 9, 102. [Google Scholar] [CrossRef]
- Polewski, M.A.; Krueger, C.G.; Reed, J.D.; Leyer, G. Ability of cranberry proanthocyanidins in combination with a probiotic formulation to inhibit in vitro invasion of gut epithelial cells by extra-intestinal pathogenic E. coli. J. Funct. Foods 2016, 25, 123–134. [Google Scholar] [CrossRef]
- Yuan, H.; Ma, Q.; Cui, H.; Liu, G.; Zhao, X.; Li, W.; Piao, G. How can synergism of traditional medicines benefit from network pharmacology? Molecules 2017, 22, 1135. [Google Scholar] [CrossRef] [PubMed]
- Coleman, C.M.; Ferreira, D. Oligosaccharides and complex carbohydrates: A new paradigm for cranberry bioactivity. Molecules 2020, 25, 881. [Google Scholar] [CrossRef] [PubMed]
| Concentration (µM) | |||
|---|---|---|---|
| 100 | 250 | 500 | |
| Flavan-3-ols | |||
| Cinnamtannin B1 | 1.05 | 4.11 | 13.95 * |
| Procyanidin A2 | 23.67 | 30.7 | 54.5 ** |
| Procyanidin B2 | 6.79 | 10.0 | −14.7 |
| (™)-Epicatechin | −6.02 | −1.21 | −5.82 |
| Simple phenols | |||
| 1,2-Dihydroxybenzene (catechol/pyrocatechol) | 17.0 * | 26.0 * | 33.2 ** |
| 1,3,5-Trihydroxybenzene (phloroglucinol) | −8.53 | 17.6 | −8.15 |
| Benzoic acids | |||
| Benzoic acid | 16.5 * | 23.3 ** | 32.2 ** |
| 3-Hydroxybenzoic acid | 11.1 | 17.0* | −9.7 |
| 3,4-Dihydroxybenzoic acid (protocatechuic acid) | 25.5 * | 24.0 | 9.44 |
| 4-Hydroxy-3-methoxybenzoic acid (vanillic acid) | 18.3 ** | 24.9 ** | 29.2 ** |
| 3,4,5-Trihydroxybenzoic acid (gallic acid) | −3.72 | 19.7 | 40.6** |
| Phenylacetic acids | |||
| Phenylacetic acid | 33.5 * | 39.0 ** | 40.6 ** |
| 3-Hydroxyphenylacetic acid | 15.0 | 11.9 | 19.4 |
| 3,4-Dihydroxyphenylacetic acid | 18.6 | 32.5 * | 37.0 ** |
| 4-Hydroxy-3-methoxyphenylacetic acid | 7.11 | 11.92 | 12.8 |
| Phenylpropionic acids | |||
| 3-Phenylpropionic acid | −11.8 | 14.7 | 12.2 |
| 3-(3-Hydroxyphenyl)-propionic acid | 10.2 | 18.6 | 30.5 * |
| 3-(3,4-Dihydroxyphenyl)-propionic acid | 6.66 | 1.19 | 13.1 |
| 3-(3,4-Dihydroxyphenyl)-propionic acid 3-O-sulphate sodium salt | 6.52 | 11.22 | 21.0 * |
| Dihydroxyphenyl-γ-valerolactones | |||
| 5-(3′,4′-Dihydroxyphenyl)-γ-valerolactone | 6.79 ± 3.92 | 9.95 ± 8.28 | 19.4 ± 10.3 * |
| 5-Phenyl-γ-valerolactone-3′,4′-di-O-sulphate | −0.22 ± 0.71 | 14.7 ± 1.5 | 30.3 ± 3.6 ** |
| 5-(4′-Hydroxyphenyl)-γ-valerolactone-3′-O-sulphate | 11.9 ± 1.7 | 10.2 ± 3.9 | 22.2 ± 5.9 ** |
| 5-(3′-Hydroxyphenyl)-γ-valerolactone-4′-O-sulphate | 10.1 ± 3.1 | 16.1 ± 6.1* | 24.2 ± 3.1 ** |
| Hippuric acids | |||
| Hippuric acids | 15.6 | 14.9 | 25.5 * |
| α-Hippuric acid | 20.8 | 23.01 | 20.0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
González de Llano, D.; Moreno-Arribas, M.V.; Bartolomé, B. Cranberry Polyphenols and Prevention against Urinary Tract Infections: Relevant Considerations. Molecules 2020, 25, 3523. https://doi.org/10.3390/molecules25153523
González de Llano D, Moreno-Arribas MV, Bartolomé B. Cranberry Polyphenols and Prevention against Urinary Tract Infections: Relevant Considerations. Molecules. 2020; 25(15):3523. https://doi.org/10.3390/molecules25153523
Chicago/Turabian StyleGonzález de Llano, Dolores, M. Victoria Moreno-Arribas, and Begoña Bartolomé. 2020. "Cranberry Polyphenols and Prevention against Urinary Tract Infections: Relevant Considerations" Molecules 25, no. 15: 3523. https://doi.org/10.3390/molecules25153523
APA StyleGonzález de Llano, D., Moreno-Arribas, M. V., & Bartolomé, B. (2020). Cranberry Polyphenols and Prevention against Urinary Tract Infections: Relevant Considerations. Molecules, 25(15), 3523. https://doi.org/10.3390/molecules25153523






