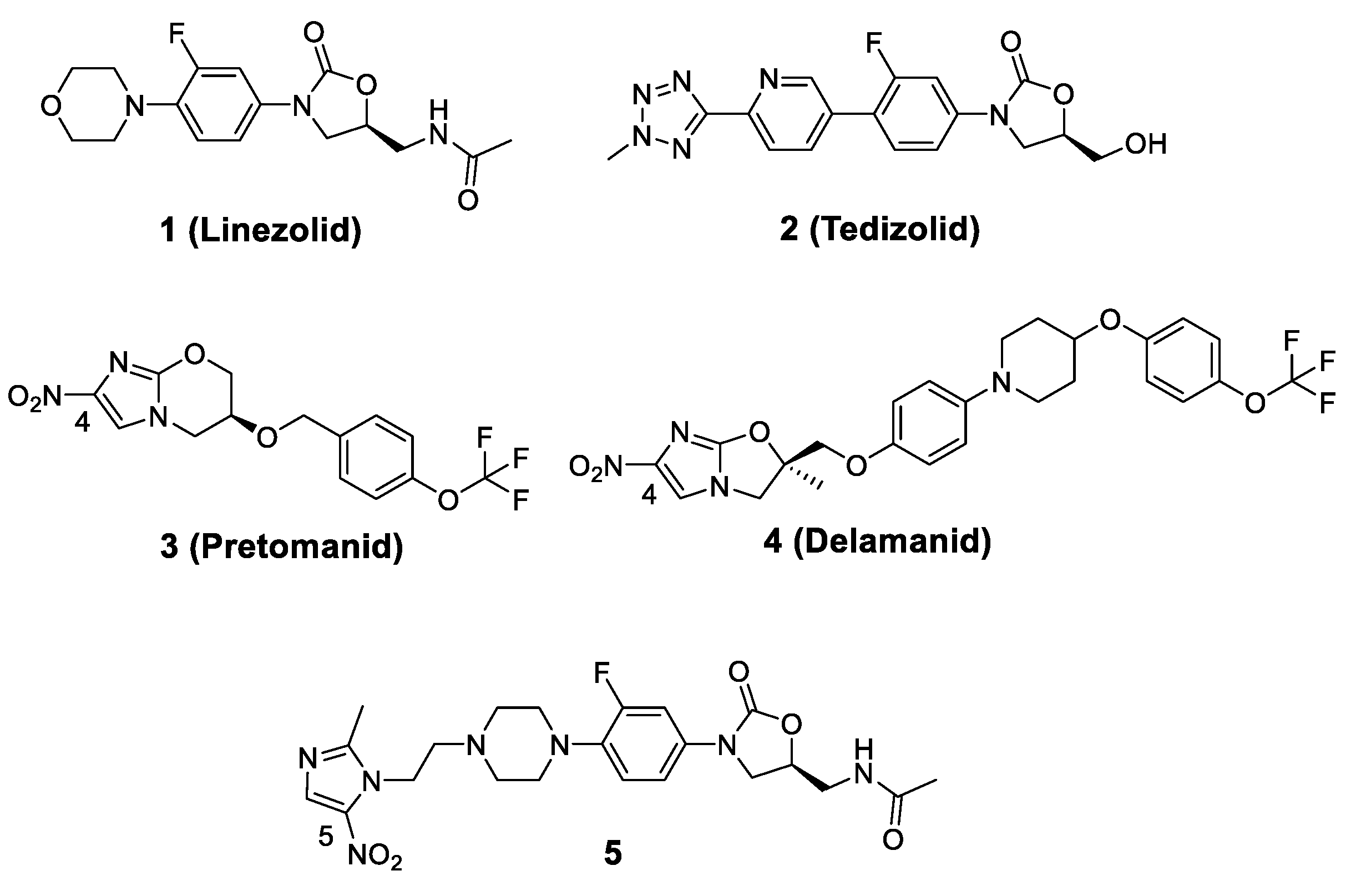
Synergistic Activity of Nitroimidazole-Oxazolidinone Conjugates against Anaerobic Bacteria
Abstract
1. Introduction
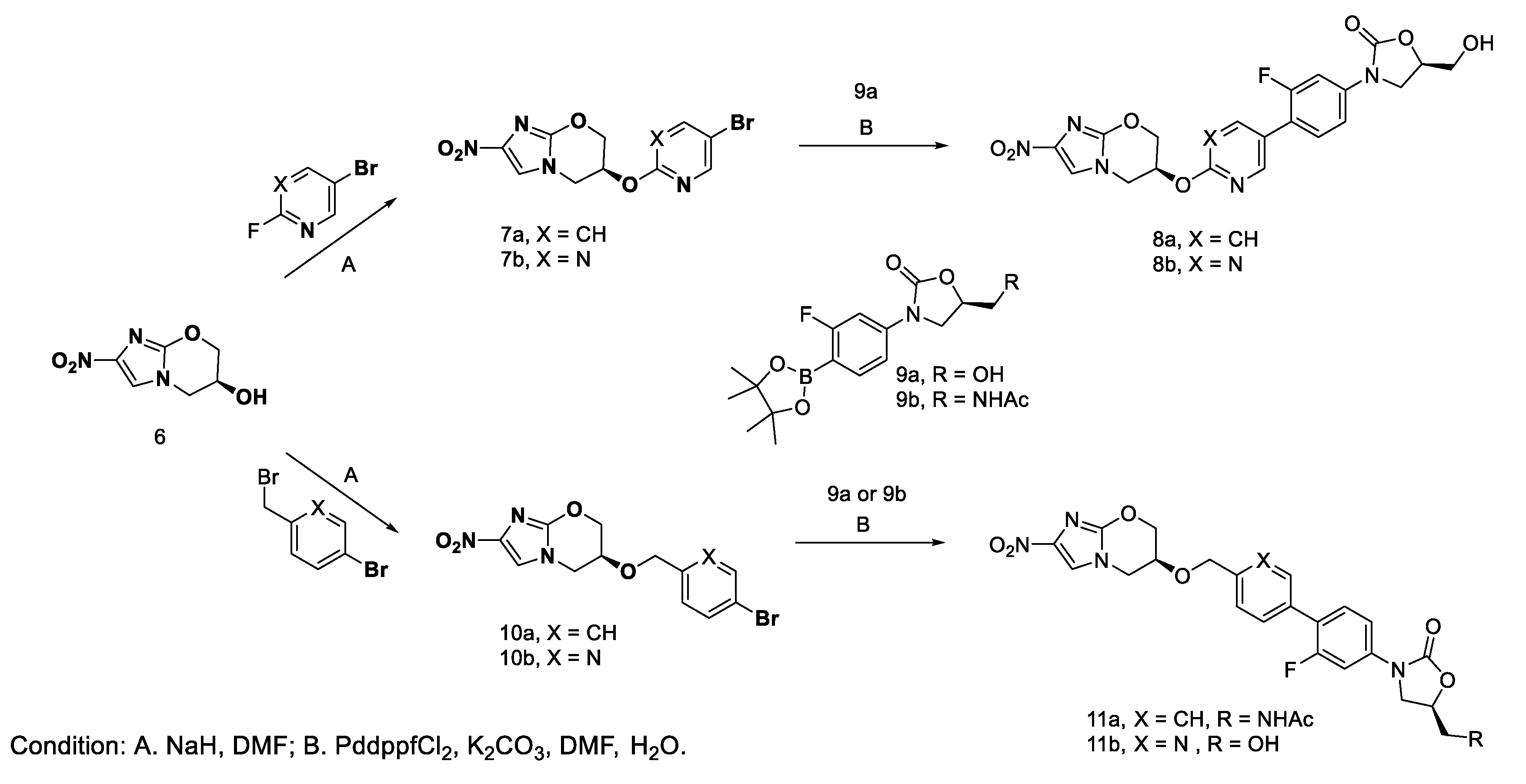
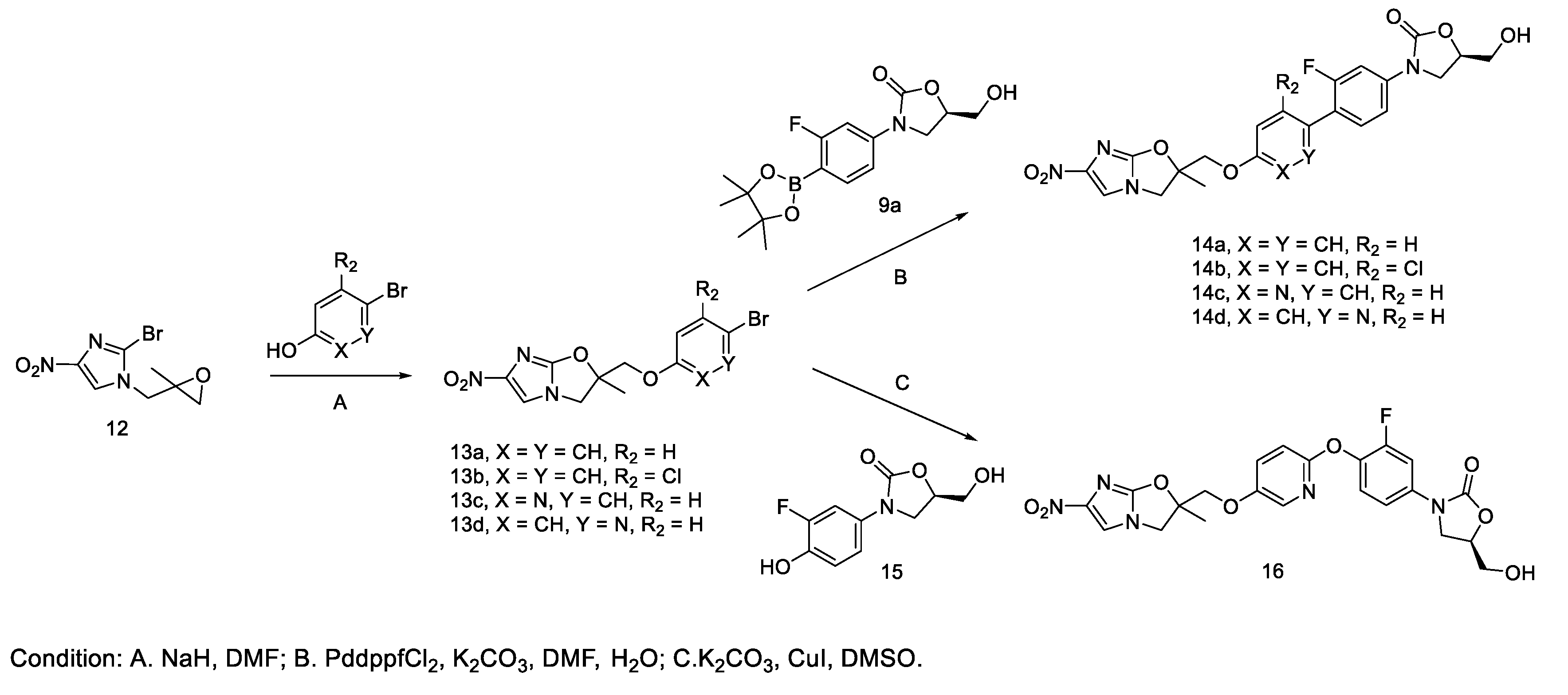
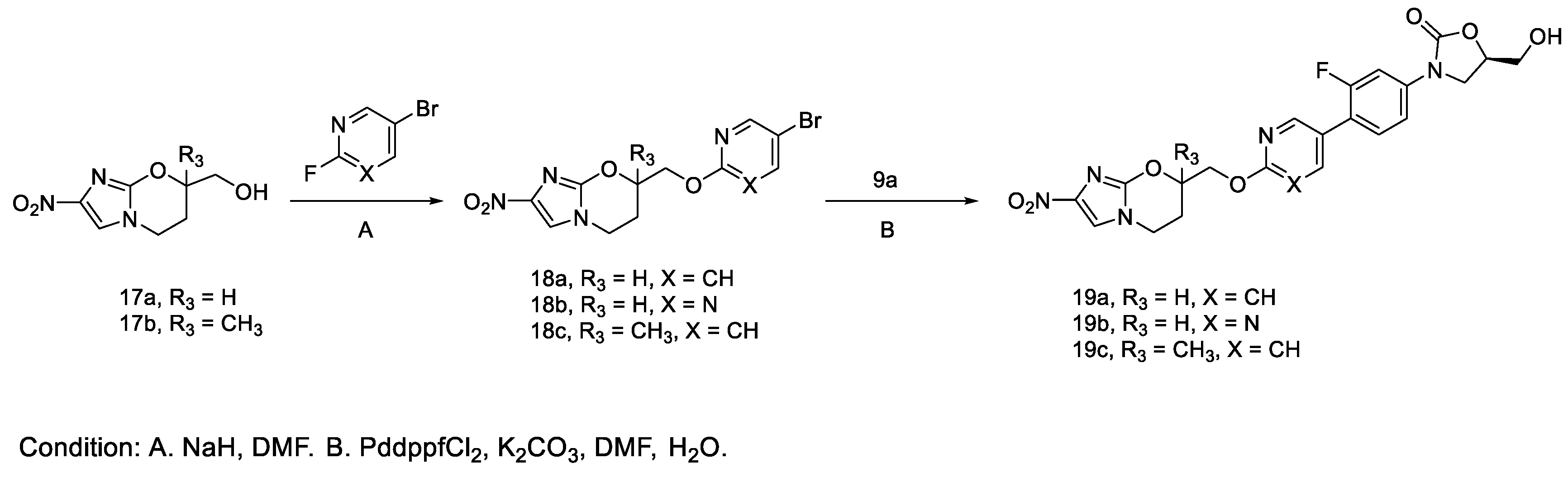
2. Results and Discussion
2.1. Chemistry
2.2. Mechanism of Action
2.3. Spectrum of Activity
2.4. Anaerobic Activity
3. Materials and Methods
3.1. Chemistry
3.2. Biology
3.2.1. Bacterial Strains
3.2.2. Generation of Isogenic Mutant Panel
3.2.3. Media
3.2.4. Minimum Inhibitory Concentration Testing
3.2.5. Cytotoxicity Assay
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hashemian, S.M.R.; Farhadi, T.; Ganjparvar, M. Linezolid: A review of its properties, function, and use in critical care. Drug Des. Dev. Ther. 2018, 12, 1759–1767. [Google Scholar] [CrossRef] [PubMed]
- Cellitti, S.E.; Shaffer, J.; Jones, D.H.; Mukherjee, T.; Gurumurthy, M.; Bursulaya, B.; Boshoff, H.I.; Choi, I.; Nayyar, A.; Lee, Y.S.; et al. Structure of Ddn, the deazaflavin-dependent nitroreductase from Mycobacterium tuberculosis involved in bioreductive activation of PA-824. Structure 2012, 20, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Manjunatha, U.; Boshoff, H.I.M.; Ha, Y.H.; Niyomrattanakit, P.; Ledwidge, R.; Dowd, C.S.; Lee, I.Y.; Kim, P.; Zhang, L.; et al. PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release. Science 2008, 322, 1392–1395. [Google Scholar] [CrossRef] [PubMed]
- Conradie, F.; Diacon, A.H.; Ngubane, N.; Howell, P.; Everitt, D.; Crook, A.M.; Mendel, C.M.; Egizi, E.; Moreira, J.; Timm, J.; et al. Treatment of highly drug-resistant pulmonary tuberculosis. N. Engl. J. Med. 2020, 382, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Lynch, A.S. Development of a dual-acting antibacterial agent (TNP-2092) for the treatment of persistent bacterial infections. J. Med. Chem. 2016, 59, 6645–6657. [Google Scholar] [CrossRef] [PubMed]
- Ippolito, J.A.; Kanyo, Z.F.; Wang, D.; Franceschi, F.J.; Moore, P.B.; Steitz, T.A.; Duffy, E.M. Crystal structure of the oxazolidinone antibiotic linezolid bound to the 50S ribosomal subunit. J. Med. Chem. 2008, 51, 3353–3356. [Google Scholar] [CrossRef] [PubMed]
- Varshney, V.; Mishra, N.N.; Shukla, P.K.; Sahu, D.P. Synthesis of nitroimidazole derived oxazolidinones as antibacterial agents. Eur. J. Med. Chem. 2010, 45, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Markad, S.D.; Kaur, P.; Kishore, R.B.K.; Chinnapattu, M.; Raichurkar, A.; Nandishaiah, R.; Panda, M.; Iyer, P.S. Novel lead generation of an anti-tuberculosis agent active against non-replicating mycobacteria: Exploring hybridization of pyrazinamide with multiple fragments. Med. Chem. Res. 2015, 24, 2986–2992. [Google Scholar] [CrossRef]
- Goto, F.; Takemura, N.; Otani, T.; Hasegawa, T.; Tsubouchi, H.; Utsumi, N.; Fujita, S.; Kuroda, H.; Shitsuta, T.; Sasaki, H. 1-Substituted-4-Nitroimidazole Compound and Process for Producing the Same. U.S. Patent US7368579B2, 6 May 2008. [Google Scholar]
- Thompson, A.M.; Denny, W.A.; Blaser, A.; Ma, Z. Nitroimidazooxazine and Nitroimidazooxazole Analogues and Their Uses. U.S. Patent US8293734B2, 23 October 2012. [Google Scholar]
- Ding, C.Z.; Lu, G.; Combrink, K.; Chen, D.D.; Song, M.; Wang, J.; Ma, Z.; Palmer, B.D.; Blaser, A.; Thompson, A.M. Bicyclic Nitroimidazole-Substituted Phenyl Oxazolidinones. U.S. Patent US7666864B2, 23 February 2010. [Google Scholar]
- Hu, M.H.; Wang, B.; Fu, L.; Xu, J.; Lu, Y. Induction and stability of Mycobacterium tuberculosis resistance to PA-824 in vitro. J. Chin. Ant. 2011, 42, 144–148. [Google Scholar]
- Hu, M.H.; Wang, B.; Fu, L.; Xu, J.; Lu, Y. Induction in vitro and stability of Mycobacterium tuberculosis resistance to Linezolid. Chin. J. Antibio. 2017, 39, 400–405. [Google Scholar]
- Lu, Y.; Zheng, M.; Wang, B.; Fu, L.; Zhao, W.; Li, P.; Xu, J.; Zhu, H.; Jin, H.; Yin, D.; et al. Clofazimine analogs with efficacy against experimental tuberculosis and reduced potential for accumulation. Antimicrob. Agents Chemother. 2011, 55, 5185–5193. [Google Scholar] [CrossRef] [PubMed]
- Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria; Approved Guideline Second Edition; CLSI Document M45-A2; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2010.
- Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria; Approved Standard-Eighth Edition; CLSI Document M11-A8; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012.
- Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Seventh Informational Supplement; CLSI Document M100-S27; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2017.
Sample Availability: All samples of the compounds are available from the authors. |
| Compounds | M. tuberculosis Isogenic Mutant Panel MIC (μg/mL) | ||||
|---|---|---|---|---|---|
| H37Rv | L1 | L3 | P1 | P3 | |
| Linezolid | 0.15 | 4.80 | 8.18 | 0.29 | 0.31 |
| Pretomanid | 0.07 | 0.15 | 0.24 | >20 | >20 |
| 8a | 0.06 | 1.95 | 1.78 | 6.48 | 5.96 |
| 8b | 0.20 | 0.91 | 1.87 | 1.04 | 3.30 |
| 14c | 0.08 | 1.84 | 0.81 | 1.77 | 1.80 |
| 14d | 0.33 | 1.88 | 1.46 | 1.93 | 2.94 |
| Compounds | Representative of Major Pathogens MIC (μg/mL) | Vero IC50 μg/mL | ||||||
|---|---|---|---|---|---|---|---|---|
| Ef ATCC 708221 | Sa ATCC 29213 | Kp ATCC 43816 | Ab ATCC 19606 | Pa ATCC 27853 | Ec ATCC 25922 | Cd ATCC 43255 | ||
| Linezolid | 4 | 8 | >64 | >64 | >64 | >64 | 4 | >64 |
| Levofloxacin | >16 | 0.25 | 0.063 | 0.5 | 1 | <0.016 | 4 | - |
| Metronidazole | >64 | 64 | >64 | >64 | >64 | >64 | 0.25 | - |
| 8a | 0.5 | 1 | >64 | >64 | >64 | >64 | 0.125 | >64 |
| 8b | 2 | 2 | >64 | >64 | >64 | >64 | 0.25 | >64 |
| 11a | 1 | 2 | >64 | >64 | >64 | >64 | 0.25 | - |
| 11b | 4 | 8 | >64 | >64 | >64 | >64 | 0.125 | >64 |
| 14a | 4 | 4 | >64 | >64 | >64 | >64 | 0.25 | >64 |
| 14b | 8 | 16 | >64 | >64 | >64 | >64 | 0.5 | >64 |
| 14c | 1 | 2 | >64 | >64 | >64 | >64 | 0.125 | >64 |
| 14d | 4 | 4 | >64 | >64 | >64 | >64 | 0.5 | >64 |
| Compounds | Anaerobic and Microaerophilic Bacterial Panel, MIC (ug/mL) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gram-Positive | Gram-Negative | Micro- Aerophilic | ||||||||||||
| Cd ATCC 700057 | La ATCC 4356 | El ATCC 43055 | Gv ATCC 14018 | Pm ATCC 23195 | Pas ATCC 3553 | Pac ATCC 11829 | Bf ATCC 25285 | Bl ATCC 15707 | Fn ATCC 10953 | Mm ATCC 35243 | Pv ATCC 29303 | Vp ATCC 17745 | Hp ATCC 43504 | |
| Metronidazole | ≤0.25 | >256 | 0.5 | 2 | >256 | 0.5 | >256 | ≤0.25 | 4 | ≤0.25 | 8 | 2 | >256 | 64 |
| Pretomanid (P) | 2 | >32 | 8 | >32 | >32 | 2 | >32 | 16 | >32 | 4 | >32 | 32 | >32 | 16 |
| Linezolid (L) | 0.5 | 2 | 1 | 0.25 | 1 | 0.5 | 0.06 | 2 | 0.5 | 0.25 | 0.12 | 2 | 0.5 | 8 |
| L + P (1:1) | 1 | 4 | 2 | 0.5 | 2 | 1 | 0.25 | 4 | 2 | 1 | 0.25 | 4 | 1 | 16 |
| 5 | 0.06 | NA | 0.06 | 0.12 | 0.25 | 0.06 | 1 | 0.25 | 0.5 | 0.06 | 0.25 | 0.5 | 1 | - |
| 8a | ≤0.03 | 0.5 | ≤0.03 | 0.06 | 0.12 | 0.06 | ≤0.03 | 1 | 0.25 | ≤0.03 | ≤0.03 | 4 | 0.25 | 0.5 |
| 8b | ≤0.03 | 0.5 | ≤0.03 | 0.06 | 0.25 | ≤0.03 | 0.06 | 4 | 0.12 | ≤0.03 | 0.06 | 8 | 0.25 | 1 |
| 11a | 0.12 | 0.5 | 0.06 | 0.06 | 0.5 | 0.06 | 0.06 | 2 | 0.25 | 0.06 | 0.06 | 4 | 0.25 | 2 |
| 11b | 0.06 | 2 | 0.06 | 0.12 | 1 | ≤0.03 | 0.12 | 4 | 0.25 | ≤0.03 | 0.25 | 8 | 1 | 2 |
| 14a | 0.25 | 1 | 0.12 | 0.12 | 0.5 | 0.12 | 0.12 | 1 | 0.25 | 0.12 | 0.25 | 16 | 0.5 | 2 |
| 14b | 0.5 | 2 | 0.12 | 0.25 | 1 | 0.25 | 0.25 | 4 | 0.5 | 1 | 0.5 | >32 | 1 | 8 |
| 14c | 0.06 | 0.5 | ≤0.03 | 0.12 | 0.5 | ≤0.03 | 0.06 | 0.5 | 0.25 | ≤0.03 | 0.12 | 8 | 0.25 | 1 |
| 14d | 0.25 | 2 | 0.12 | 0.12 | 1 | 0.12 | 0.25 | 8 | 0.5 | 0.12 | 0.25 | 16 | 0.5 | 1 |
| 16 | 4 | >32 | 16 | >32 | >32 | 8 | >32 | >32 | >32 | >32 | >32 | >32 | >32 | 16 |
| 19a | ≤0.03 | 0.25 | ≤0.06 | 0.06 | 0.12 | ≤0.03 | ≤0.03 | 0.12 | 0.06 | ≤0.03 | 0.06 | 2 | 0.25 | 0.25 |
| 19b | ≤0.03 | 0.5 | 0.06 | 0.06 | 0.12 | ≤0.03 | 0.06 | 1 | 0.06 | ≤0.03 | 0.06 | 4 | 0.25 | 0.25 |
| 19c | ≤0.03 | 0.25 | ≤0.03 | ≤0.03 | 0.06 | ≤0.03 | ≤0.03 | 0.5 | 0.12 | ≤0.03 | 0.06 | 2 | 0.25 | 0.5 |
| Panel | Organism | ATCC No. | Testing Facility |
|---|---|---|---|
| Spectrum Panel | Enterococcus faecalis (Ef) | 700221 | HD Biosciences |
| Staphylococcus aureus (Sa) | 292213 | ||
| Klebciella pneumonia (Kp) | 43816 | ||
| Acinetobacter baumannii (Ab) | 19606 | ||
| Pseudomonas aeruginosa (Pa) | 27853 | ||
| Escherichia coli (Ec) | 25922 | ||
| Clostrium difficile (Cd) | 43255 | ||
| M. tuberculosis Isogenic Resistant Mutant Panel | M. tuberculosis H37Rv (Wild-Type) | 27294 | BTTTRI |
| M. tuberculosis P1 (Pretomanid-R) | Isogenic | ||
| M. tuberculosis P3 (Pretomanis-R) | Isogenic | ||
| M. tuberculosis L1 (Linezolid-R) | Isogenic | ||
| M. tuberculosis L3 (Linezolid-R) | Isogenic | ||
| Anaerobic Bacterial Panel | Clostridium difficile (Cd) | 700057 | Micromyx |
| Lactobacillus acidophilus (Lc) | 4356 | ||
| Eggerthella lenta (El) | 43055 | ||
| Gardnerella vaginalis (Gv) | 14018 | ||
| Peptostreptococcus micros (Pm) | 23195 | ||
| Porphyromonas asaccharolytica (Pas) | M3553 | ||
| Propionibacterium acnes (Pac) | 11892 | ||
| Bacteroides fragilis (Bf) | 25285 | ||
| Bifidobacterium longum (Bl) | 15707 | ||
| Fusobacterium nucleatum (Fn) | 10953 | ||
| Mobiluncus mulieris (Mm) | 35243 | ||
| Prevotella bivia (Pb) | 29303 | ||
| Veillonella parvula (Vp) | 17745 | ||
| Helicobacter pylori (Hp) | 43504 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhuang, Z.; Wan, D.; Ding, J.; He, S.; Zhang, Q.; Wang, X.; Yuan, Y.; Lu, Y.; Z. Ding, C.; Lynch, A.S.; et al. Synergistic Activity of Nitroimidazole-Oxazolidinone Conjugates against Anaerobic Bacteria. Molecules 2020, 25, 2431. https://doi.org/10.3390/molecules25102431
Zhuang Z, Wan D, Ding J, He S, Zhang Q, Wang X, Yuan Y, Lu Y, Z. Ding C, Lynch AS, et al. Synergistic Activity of Nitroimidazole-Oxazolidinone Conjugates against Anaerobic Bacteria. Molecules. 2020; 25(10):2431. https://doi.org/10.3390/molecules25102431
Chicago/Turabian StyleZhuang, Zhijun, Dawei Wan, Jun Ding, Shijie He, Qian Zhang, Xiaomei Wang, Ying Yuan, Yu Lu, Charles Z. Ding, Anthony Simon Lynch, and et al. 2020. "Synergistic Activity of Nitroimidazole-Oxazolidinone Conjugates against Anaerobic Bacteria" Molecules 25, no. 10: 2431. https://doi.org/10.3390/molecules25102431
APA StyleZhuang, Z., Wan, D., Ding, J., He, S., Zhang, Q., Wang, X., Yuan, Y., Lu, Y., Z. Ding, C., Lynch, A. S., M. Upton, A., B. Cooper, C., A. Denny, W., & Ma, Z. (2020). Synergistic Activity of Nitroimidazole-Oxazolidinone Conjugates against Anaerobic Bacteria. Molecules, 25(10), 2431. https://doi.org/10.3390/molecules25102431






