Praziquantel-Solid Lipid Nanoparticles Produced by Supercritical Carbon Dioxide Extraction: Physicochemical Characterization, Release Profile, and Cytotoxicity
Abstract
:1. Introduction
2. Results and Discussion
3. Materials and Methods
3.1. Materials
3.2. Production of SLN
3.3. Mean Particle Size, Polydispersity Index, and Zeta Potential
3.4. Encapsulation Efficiency (EE) and Loading Capacity (LC)
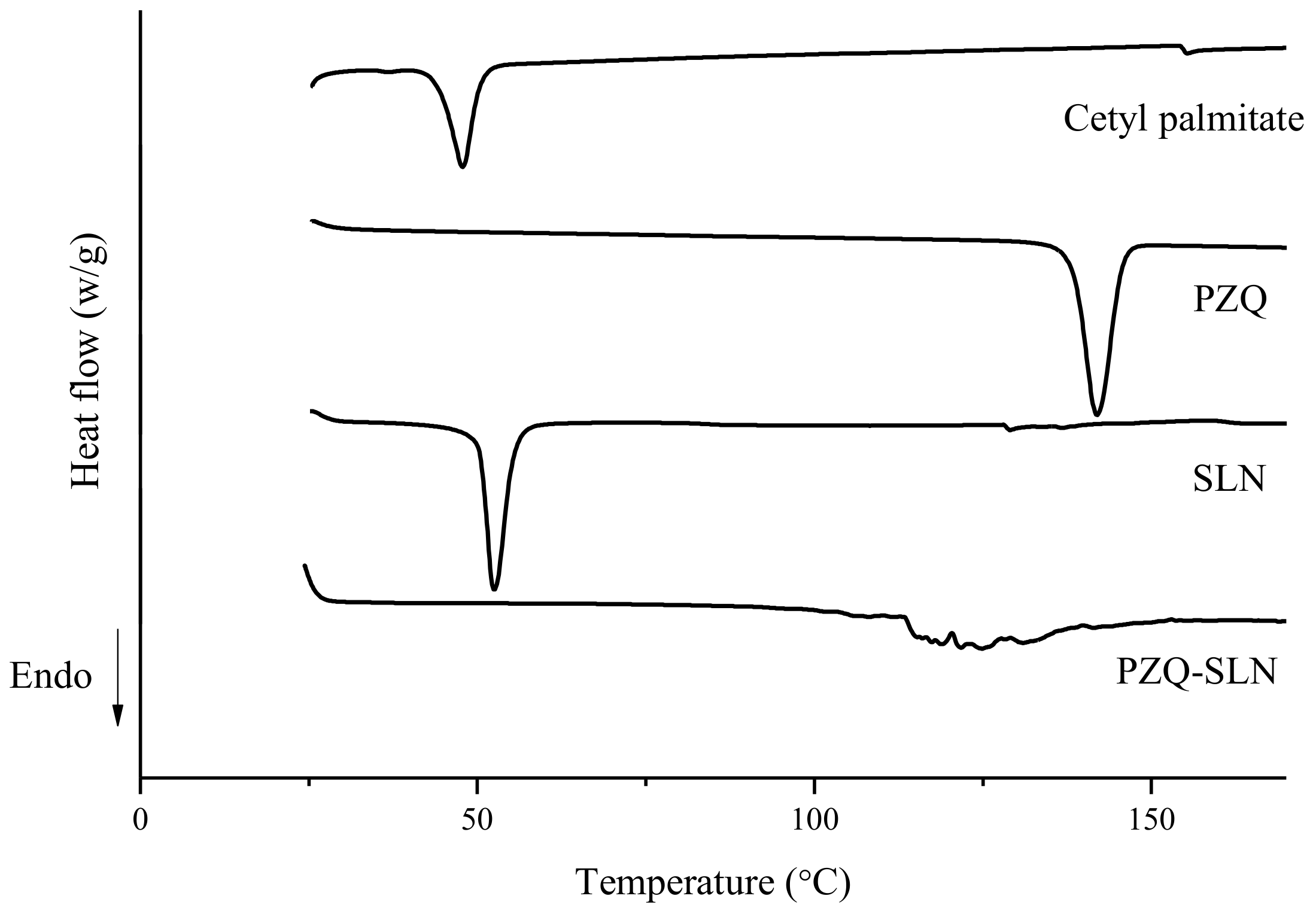
3.5. Differential Scanning Calorimetry (DSC)
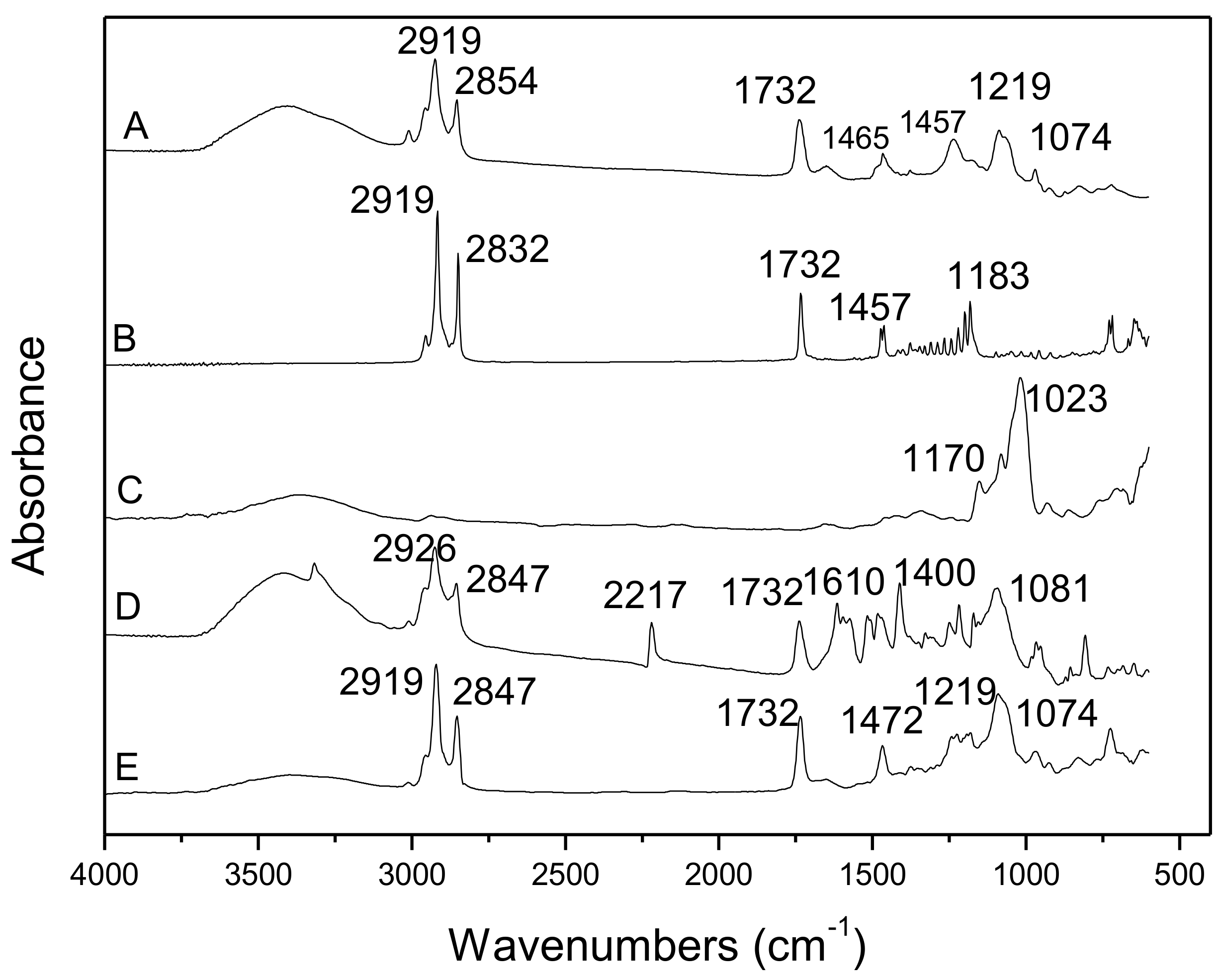
3.6. Fourier-Transform Infrared Spectroscopy (FTIR)
3.7. In Vitro Drug Release Studies
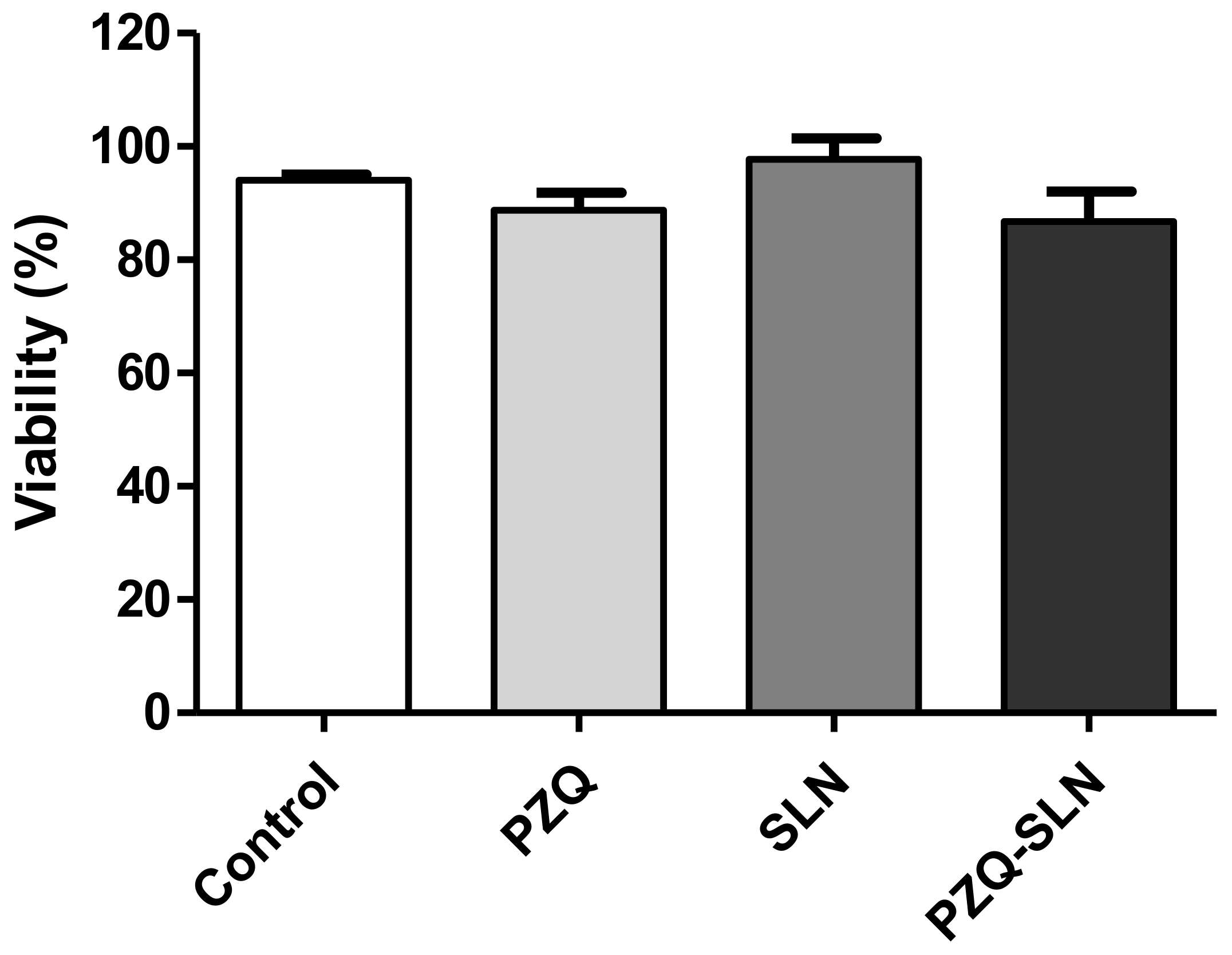
3.8. Cell Viability Assay in L929 Cells
3.9. Statistical Analyses
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Teixeira, M.C.; Carbone, C.; Souto, E.B. Beyond liposomes: Recent advances on lipid based nanostructures for poorly soluble/poorly permeable drug delivery. Prog Lipid Res. 2017, 68, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Souto, E.B.; Muller, R.H. Lipid nanoparticles: Effect on bioavailability and pharmacokinetic changes. Handb. Exp. Pharm. 2010, 115–141. [Google Scholar] [CrossRef]
- Almeida, A.J.; Souto, E. Solid lipid nanoparticles as a drug delivery system for peptides and proteins. Adv. Drug Deliv. Rev. 2007, 59, 478–490. [Google Scholar] [CrossRef] [PubMed]
- Doktorovova, S.; Souto, E.B.; Silva, A.M. Hansen solubility parameters (HSP) for prescreening formulation of solid lipid nanoparticles (SLN): In vitro testing of curcumin-loaded SLN in MCF-7 and BT-474 cell lines. Pharm. Dev. Technol. 2018, 23, 96–105. [Google Scholar] [CrossRef]
- Aji Alex, M.R.; Chacko, A.J.; Jose, S.; Souto, E.B. Lopinavir loaded solid lipid nanoparticles (SLN) for intestinal lymphatic targeting. Eur. J. Pharm. Sci. 2011, 42, 11–18. [Google Scholar] [CrossRef]
- Muller, R.H.; Runge, S.; Ravelli, V.; Mehnert, W.; Thunemann, A.F.; Souto, E.B. Oral bioavailability of cyclosporine: Solid lipid nanoparticles (SLN) versus drug nanocrystals. Int. J. Pharm. 2006, 317, 82–89. [Google Scholar] [CrossRef]
- Campos, J.R.; Fernandes, A.R.; Sousa, R.; Fangueiro, J.F.; Boonme, P.; Garcia, M.L.; Silva, A.M.; Naveros, B.C.; Souto, E.B. Optimization of nimesulide-loaded solid lipid nanoparticles (SLN) by factorial design, release profile and cytotoxicity in human Colon adenocarcinoma cell line. Pharm. Dev. Technol. 2019, 24, 616–622. [Google Scholar] [CrossRef]
- Severino, P.; Santana, M.H.; Souto, E.B. Optimizing SLN and NLC by 2(2) full factorial design: Effect of homogenization technique. Mater. Sci. Eng. C Mater. Biol. Appl. 2012, 32, 1375–1379. [Google Scholar] [CrossRef]
- Salehi, B.; Venditti, A.; Sharifi-Rad, M.; Kregiel, D.; Sharifi-Rad, J.; Durazzo, A.; Lucarini, M.; Santini, A.; Souto, E.B.; Novellino, E.; et al. The therapeutic potential of apigenin. Int. J. Mol. Sci. 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, P.; Shekunov, B.Y.; Yim, D.; Cipolla, D.; Boyd, B.; Farr, S. Production of solid lipid nanoparticle suspensions using supercritical fluid extraction of emulsions (SFEE) for pulmonary delivery using the AERx system. Adv. Drug Deliv. Rev. 2007, 59, 444–453. [Google Scholar] [CrossRef]
- Acevedo-Morantes, C.Y.; Acevedo-Morantes, M.T.; Suleiman-Rosado, D.; Ramirez-Vick, J.E. Evaluation of the cytotoxic effect of camptothecin solid lipid nanoparticles on MCF7 cells. Drug Deliv. 2013, 20, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Corrias, F.; Lai, F. New methods for lipid nanoparticles preparation. Recent Pat. Drug Deliv. 2011, 5, 201–213. [Google Scholar] [CrossRef]
- Trucillo, P.; Campardelli, R. Production of solid lipid nanoparticles with a supercritical fluid assisted process. J. Supercrit. Fluids 2019, 143, 16–23. [Google Scholar] [CrossRef]
- De Souza, A.L.; Andreani, T.; de Oliveira, R.N.; Kiill, C.P.; dos Santos, F.K.; Allegretti, S.M.; Chaud, M.V.; Souto, E.B.; Silva, A.M.; Gremiao, M.P. In vitro evaluation of permeation, toxicity and effect of praziquantel-loaded solid lipid nanoparticles against Schistosoma mansoni as a strategy to improve efficacy of the schistosomiasis treatment. Int. J. Pharm. 2014, 463, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Ferreira Marques, C.S.; Rezende, P.; Andrade, L.N.; Mendes, T.M.F.; Allegretti, S.M.; Bani, C.; Chaud, M.V.; Batista de Almeida, M.; Souto, E.B.; Pereira da Costa, L.; et al. Solid dispersion of praziquantel enhanced solubility and improve the efficacy of the schistosomiasis treatment. J. Drug Deliv. Sci. Technol. 2018, 45, 124–134. [Google Scholar] [CrossRef]
- Santo, I.E.; Pedro, A.S.; Fialho, R.; Cabral-Albuquerque, E. Characteristics of lipid micro- and nanoparticles based on supercritical formation for potential pharmaceutical application. Nanoscale Res. Lett. 2013, 8, 386. [Google Scholar] [CrossRef] [PubMed]
- Danaei, M.; Dehghankhold, M.; Ataei, S.; Hasanzadeh Davarani, F.; Javanmard, R.; Dokhani, A.; Khorasani, S.; Mozafari, M.R. Impact of Particle Size and Polydispersity Index on the Clinical Applications of Lipidic Nanocarrier Systems. Pharmaceutics 2018, 10, 57. [Google Scholar] [CrossRef]
- Jelowdar, A.; Rafiei, A.; Abbaspour, M.R.; Rashidi, I.; Rahdar, M. Efficacy of combined albendazol and praziquntel and their loaded solid lipid nanoparticles components in chemoprophylaxis of experimental hydatidosis. Asian Pac. J. Trop. Biomed. 2017, 7, 549–554. [Google Scholar] [CrossRef]
- Garcia, H.H.; Gonzales, I.; Lescano, A.G.; Bustos, J.A.; Zimic, M.; Escalante, D.; Saavedra, H.; Gavidia, M.; Rodriguez, L.; Najar, E.; et al. Efficacy of combined antiparasitic therapy with praziquantel and albendazole for neurocysticercosis: A double-blind, randomised controlled trial. Lancet Infect. Dis. 2014, 14, 687–695. [Google Scholar] [CrossRef]
- Chaud, M.V.; Tamascia, P.; Lima, A.C.d.; Paganelli, M.O.; Gremião, M.P.D.; Freitas, O.d. Solid dispersions with hydrogenated castor oil increase solubility, dissolution rate and intestinal absorption of praziquantel. Braz. J. Pharm. Sci. 2010, 46, 473–481. [Google Scholar] [CrossRef]
- Chaud, M.V.; Lima, A.C.; Vila, M.M.; Paganelli, M.O.; Paula, F.C.; Pedreiro, L.N.; Gremião, M.P. Development and evaluation of praziquantel solid dispersions in sodium starch glycolate. Trop. J. Pharm. Res. 2013, 163–168. [Google Scholar] [CrossRef]
- Passerini, N.; Albertini, B.; Perissutti, B.; Rodriguez, L. Evaluation of melt granulation and ultrasonic spray congealing as techniques to enhance the dissolution of praziquantel. Int. J. Pharm. 2006, 318, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, X.; Wang, J.K.; Ching, C.B. Structural characterization and enantioseparation of the chiral compound praziquantel. J. Pharm. Sci. 2004, 93, 3039–3046. [Google Scholar] [CrossRef] [PubMed]
- Schepers, H.; Brasseur, R.; Goormaghtigh, E.; Duquenoy, P.; Ruysschaert, J.-M. Mode of insertion of praziquantel and derivatives into lipid membranes. Biochem. Pharm. 1988, 37, 1615–1623. [Google Scholar] [CrossRef]
- Silva, A.M.; Martins-Gomes, C.; Fangueiro, J.F.; Andreani, T.; Souto, E.B. Comparison of antiproliferative effect of epigallocatechin gallate when loaded into cationic solid lipid nanoparticles against different cell lines. Pharm. Dev. Technol. 2019, 1–7. [Google Scholar] [CrossRef]
- 10993-5, I. Biological Evaluation of Medical Devices—Part 5: Tests for In Vitro Cytotoxicity. Available online: https://www.iso.org/standard/36406.html (accessed on 30 August 2019).
- Rigon, R.B.; Goncalez, M.L.; Severino, P.; Alves, D.A.; Santana, M.H.A.; Souto, E.B.; Chorilli, M. Solid lipid nanoparticles optimized by 2(2) factorial design for skin administration: Cytotoxicity in NIH3T3 fibroblasts. Colloids Surf. B Biointerfaces 2018, 171, 501–505. [Google Scholar] [CrossRef]
Sample Availability: Samples of the compounds are available from the authors. |
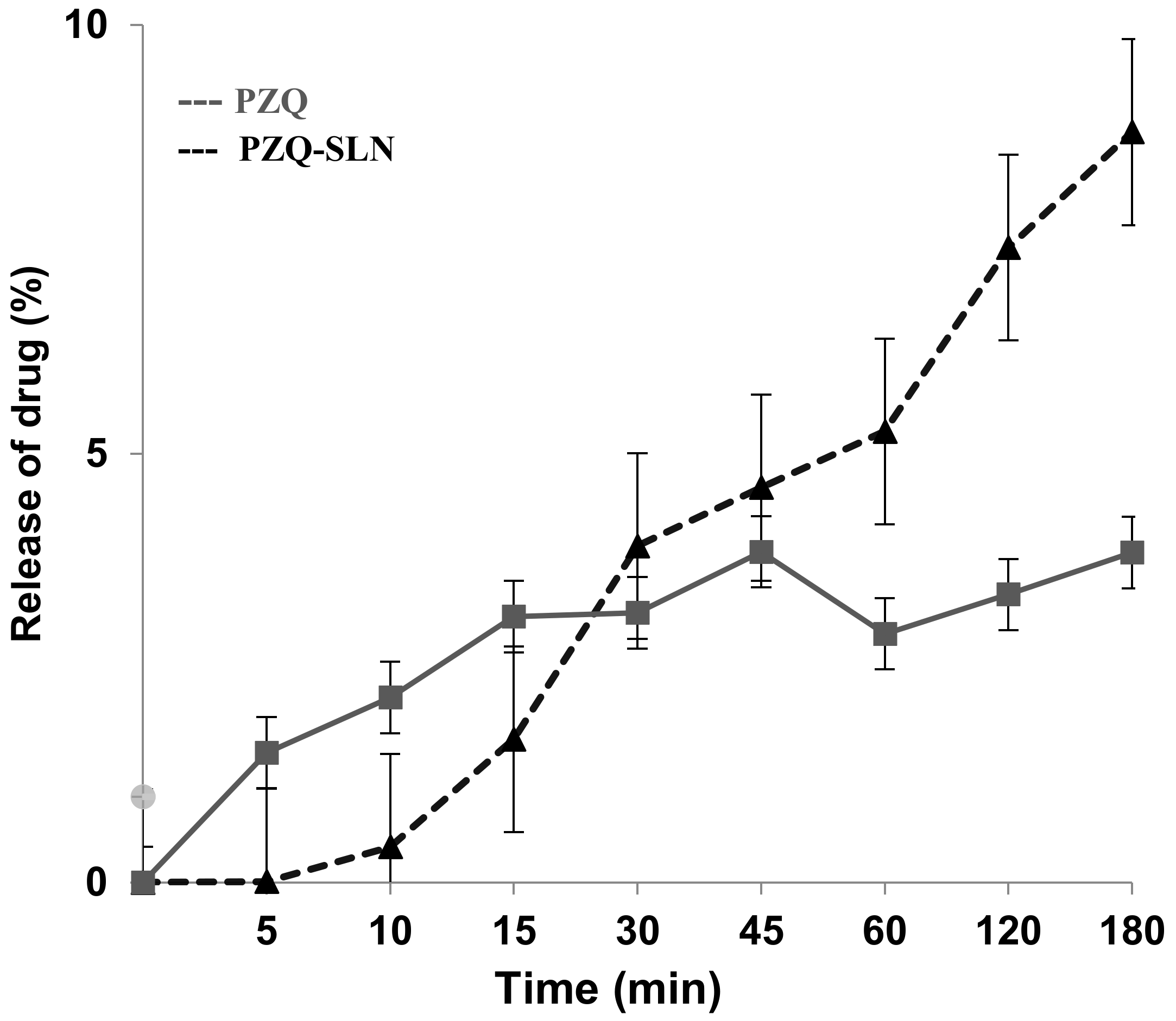
| Square r Value (r2) | ||
|---|---|---|
| PZQ-SLN | PZQ | |
| Mathematical Models | ||
| Baker and Lonsdale | 0.8851 | −0.4559 |
| Korsmeyer-Peppas | 1.0 | 0.8215 |
| Hixon and Crowell | 0.9999 | −2.2413 |
| Higuchi, Square Root | 0.8881 | −0.4665 |
| First Order | 0.9999 | −2.2292 |
| Weibull | 1.0 | 1.0 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andrade, L.N.; Oliveira, D.M.L.; Chaud, M.V.; Alves, T.F.R.; Nery, M.; da Silva, C.F.; Gonsalves, J.K.C.; Nunes, R.S.; Corrêa, C.B.; Amaral, R.G.; et al. Praziquantel-Solid Lipid Nanoparticles Produced by Supercritical Carbon Dioxide Extraction: Physicochemical Characterization, Release Profile, and Cytotoxicity. Molecules 2019, 24, 3881. https://doi.org/10.3390/molecules24213881
Andrade LN, Oliveira DML, Chaud MV, Alves TFR, Nery M, da Silva CF, Gonsalves JKC, Nunes RS, Corrêa CB, Amaral RG, et al. Praziquantel-Solid Lipid Nanoparticles Produced by Supercritical Carbon Dioxide Extraction: Physicochemical Characterization, Release Profile, and Cytotoxicity. Molecules. 2019; 24(21):3881. https://doi.org/10.3390/molecules24213881
Chicago/Turabian StyleAndrade, Luciana N., Daniele M.L. Oliveira, Marco V. Chaud, Thais F.R. Alves, Marcelo Nery, Classius F. da Silva, Joyce K.C. Gonsalves, Rogéria S. Nunes, Cristiane B. Corrêa, Ricardo G. Amaral, and et al. 2019. "Praziquantel-Solid Lipid Nanoparticles Produced by Supercritical Carbon Dioxide Extraction: Physicochemical Characterization, Release Profile, and Cytotoxicity" Molecules 24, no. 21: 3881. https://doi.org/10.3390/molecules24213881
APA StyleAndrade, L. N., Oliveira, D. M. L., Chaud, M. V., Alves, T. F. R., Nery, M., da Silva, C. F., Gonsalves, J. K. C., Nunes, R. S., Corrêa, C. B., Amaral, R. G., Sanchez-Lopez, E., Souto, E. B., & Severino, P. (2019). Praziquantel-Solid Lipid Nanoparticles Produced by Supercritical Carbon Dioxide Extraction: Physicochemical Characterization, Release Profile, and Cytotoxicity. Molecules, 24(21), 3881. https://doi.org/10.3390/molecules24213881











