The Multiple Faces of C-Reactive Protein—Physiological and Pathophysiological Implications in Cardiovascular Disease
Abstract
1. Introduction
2. Structure of Native C-Reactive Protein
3. Pentameric C-Reactive Protein
3.1. Glycosylated C-Reactive Protein
3.2. High-Order Assembly of Pentameric C-Reactive Protein
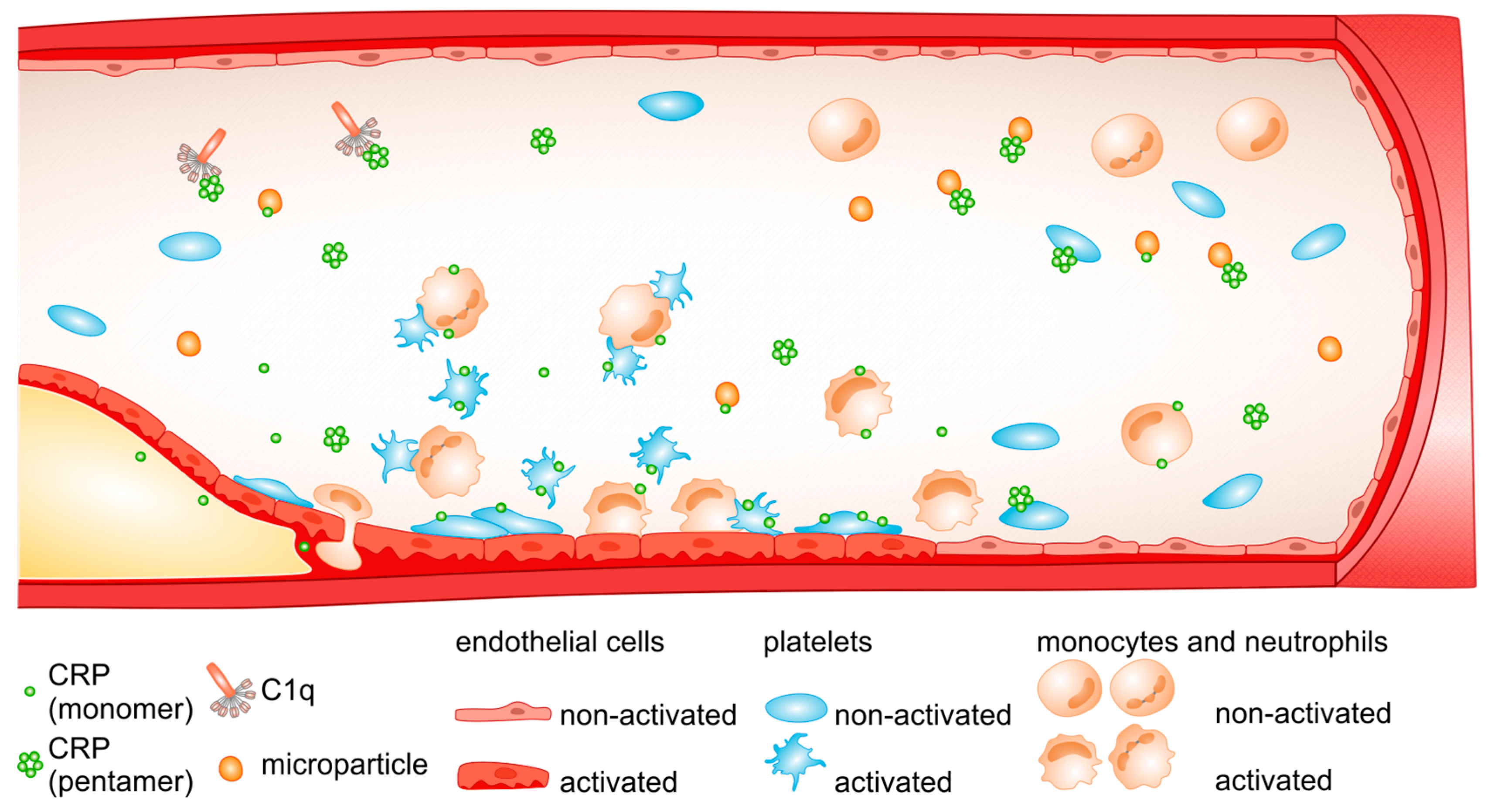
4. Monomeric C-Reactive Protein
5. Conclusions
Funding
Conflicts of Interest
References
- Wu, Y.; Potempa, L.A.; El Kebir, D.; Filep, J.G. C-reactive protein and inflammation: Conformational changes affect function. Biol. Chem. 2015, 396, 1181–1197. [Google Scholar] [CrossRef]
- Pepys, M.B. C-reactive protein fifty years on. Lancet 1981, 1, 653–657. [Google Scholar] [CrossRef]
- Gewurtz, H.; Mold, C.; Siegel, J.; Fiedel, B. C-reactive protein and the acute phase response. Adv. Intern. Med. 1982, 27, 345–372. [Google Scholar] [CrossRef]
- Du Clos, T.W. C-Reactive Protein as a Regulator of Autoimmunity and Inflammation. Arthritis Rheum 2003, 48, 1475–1477. [Google Scholar] [CrossRef]
- Ridker, P.M. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003, 107, 363–369. [Google Scholar] [CrossRef]
- Lippi, G.; Favaloro, E.J.; Montagnana, M.; Franchini, M. C-reactive protein and venous thromboembolism: Causal or casual association? Clin. Chem. Lab. Med. 2010, 48, 1693–1701. [Google Scholar] [CrossRef]
- Simpson, R.M.; Prancan, A.; Izzi, J.M.; Fiedel, B.A. Generation of thromboxane A2 and aorta-contracting activity from platelets stimulated with modified C-reactive protein. Immunology 1982, 47, 193–202. [Google Scholar] [PubMed]
- Nillson, J. CRP-marker or maker of cardiovascular disease? Arterioscler Thromb. Vasc. Biol. 2005, 25, 1527–1528. [Google Scholar] [CrossRef]
- Emsley, J.; White, H.E.; O’Hara, B.P.; Oliva, G.; Srinivasan, N.; Tickle, I.J.; Blundell, T.L.; Pepys, M.B.; Wood, S.P. Structure of pentameric human serum amyloid P component. Nature 1994, 367, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.; Pepys, M.B.; Wood, S.P. The physiological structure of human C-reactive protein and its complex with phosphocholine. Structure 1999, 7, 169–177. [Google Scholar] [CrossRef]
- Shrive, A.K.; Cheetham, G.M.; Holden, D.; Myles, D.A.; Turnell, W.G.; Volanakis, J.E.; Pepys, M.B.; Bloomer, A.C.; Greenhough, T.J. Three dimensional structure of human C-reactive protein. Nat. Struct. Biol. 1996, 3, 346–354. [Google Scholar] [CrossRef]
- Goda, T.; Miyahara, Y. Specific binding of human C-reactive protein towards supported monolayers of binary and engineered phospholipids. Colloids Surf. B Biointerfaces 2018, 161, 662–669. [Google Scholar] [CrossRef]
- Goda, T.; Miyahara, Y. Engineered zwitterionic phosphorylcholine monolayers for elucidating multivalent binding kinetics of C-reactive protein. Acta Biomater. 2016, 40, 46–53. [Google Scholar] [CrossRef]
- Agrawal, A.; Shrive, A.K.; Greenhough, T.J.; Volanakis, J.E. Topology and structure of the C1q-binding site on C-reactive protein. J. Immunol. 2001, 166, 3998–4004. [Google Scholar] [CrossRef]
- Braig, D.; Nero, T.L.; Koch, H.G.; Kaiser, B.; Wang, X.; Thiele, J.R.; Morton, C.J.; Zeller, J.; Kiefer, J.; Potempa, L.A.; et al. Transitional changes in the CRP structure lead to the exposure of proinflammatory binding sites. Nat. Commun. 2017, 8, 14188. [Google Scholar] [CrossRef]
- McGrath, F.D.G.; Brouwer, M.C.; Arlaud, G.J.; Daha, M.R.; Hack, C.E.; Roos, A. Evidence That Complement Protein C1q Interacts with C-Reactive Protein through Its Globular Head Region. J. Immunol. 2006, 176, 2950–2957. [Google Scholar] [CrossRef]
- Biro, A.; Rovo, Z.; Papp, D.; Cervenak, L.; Varga, L.; Füst, G.; Thielens, N.M.; Arlaud, G.J.; Prohászka, Z. Studies on the interactions between C-reactive protein and complement proteins. Immunology 2007, 121, 40–50. [Google Scholar] [CrossRef]
- Osmand, A.P.; Gerwurz, H.; Friedenson, B. Partial amino-acid sequences of human and rabbit C-reactive proteins: Homology with immunoglobulins and histocompatibility antigens. Proc. Natl. Acad. Sci. USA 1977, 74, 1214–1218. [Google Scholar] [CrossRef]
- Pepys, M.B. The pentraxins 1975–2018: Serendipity, diagnostics and drugs. Front Immunol 2018, 9, 2382. [Google Scholar] [CrossRef]
- Gotschlich, E.C.; Edelman, G.M. C-reactive protein: A molecule composed of subunits. Proc. Natl. Acad. Sci. USA 1965, 54, 558–566. [Google Scholar] [CrossRef]
- Szalai, A.J.; Agrawal, A.; Greenhough, T.J.; Volanakis, J.E. C-reactive protein: Structural biology and host defense function. Clin. Chem. Lab. Med. 1999, 37, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Bang, R.; Marnell, L.; Mold, C.; Stein, M.P.; Clos, K.T.; Chivington-Buck, C.; Clos, T.W. Analysis of binding sites in human C-reactive protein for FcγRI, FcγRIIA, and C1q by site-directed mutagenesis. J. Biol. Chem. 2005, 280, 25095–25102. [Google Scholar] [CrossRef]
- Bally, I.; Ancelet, S.; Moriscot, C.; Gonnet, F.; Mantovani, A.; Daniel, R.; Schoehn, G.; Arlaud, G.J.; Thielens, N.M. Expression of recombinant human complement C1q allows identification of the C1r/C1s-binding sites. Proc. Natl. Acad. Sci. USA 2013, 110, 8650–8655. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.I. The occurrence during acute infections of a protein not normally present in the blood. J. Exp. Med. 1947, 85, 491–498. [Google Scholar] [CrossRef]
- DeLucas, L.J.; Greenhough, T.J.; Rule, S.A.; Myles, D.A.; Babu, Y.S.; Volanakis, J.E.; Bugg, C.E. Preliminary X-ray study of crystals of human C-reactive protein. J. Mol. Biol. 1987, 196, 741–742. [Google Scholar] [CrossRef]
- Ramadan, M.A.; Shrive, A.K.; Holden, D.; Myles, D.A.; Volanakis, J.E.; DeLucas, L.J.; Greenhough, T.J. The three-dimensional structure of calcium-depleted human C-reactive protein from perfectly twinned crystals. Acta Crystallogr. D Biol. Crystallogr. 2002, 58, 992–1001. [Google Scholar] [CrossRef]
- Potempa, L.A.; Maldonado, B.A.; Laurent, P.; Zemel, E.S.; Gewurz, H. Antigenic, electrophoretic and binding alterations of human C-reactive protein modified selectively in the absence of calcium. Mol. Immunol. 1983, 20, 1165–1175. [Google Scholar] [CrossRef]
- Wang, M.Y.; Ji, S.R.; Bai, C.J.; El Kebir, D.; Li, H.Y.; Shi, J.M.; Zhu, W.; Costantino, S.; Zhou, H.H.; Potempa, L.A.; et al. A redox switch in C-reactive protein modulates activation of endothelial cells. FASEB J. 2011, 25, 3186–3196. [Google Scholar] [CrossRef] [PubMed]
- Du Clos, T.W. Pentraxins: Structure, function, and role in inflammation. ISRN Inflamm 2013, 2013, 379040. [Google Scholar] [CrossRef]
- Black, S.; Kushner, I.; Samols, D. C-reactive Protein. J. Biol. Chem. 2004, 279, 48487–48490. [Google Scholar] [CrossRef]
- Agassandian, M.; Shurin, G.V.; Ma, Y.; Shurin, M.R. C-reactive protein and lung diseases. Int. J. Biochem. Cell Biol. 2014, 53, 77–88. [Google Scholar] [CrossRef]
- Pepys, M.B.; Hirschfield, G.M. C-reactive protein: A critical update. J. Clin. Invest. 2003, 111, 1805–1812. [Google Scholar] [CrossRef]
- Karasahin, O.; Tasar, P.T.; Timur, O.; Yildirim, F.; Binici, D.N.; Sahin, S. The value of C-reactive protein in infection diagnosis and prognosis in elderly patients. Aging Clin. Exp. Res. 2018, 30, 555–562. [Google Scholar] [CrossRef]
- Ryu, J.A.; Yang, J.H.; Lee, D.; Park, C.M.; Suh, G.Y.; Jeon, K.; Cho, J.; Baek, S.Y.; Carriere, K.C.; Chung, C.R. Clinical Usefulness of Procalcitonin and C-Reactive Protein as Outcome Predictors in Critically Ill Patients with Severe Sepsis and Septic Shock. PLoS ONE 2015, 10. [Google Scholar] [CrossRef]
- Bray, C.; Bell, L.N.; Liang, H.; Haykal, R.; Kaiksow, F.; Mazza, J.J.; Yale, S.H. Erythrocyte Sedimentation Rate and C-reactive Protein Measurements and Their Relevance in Clinical Medicine. Wis. Med. J. 2016, 115, 317–321. [Google Scholar]
- Ticinesi, A.; Lauretani, F.; Nouvenne, A.; Porro, E.; Fanelli, G.; Maggio, M.; Meschi, T. C-reactive protein (CRP) measurement in geriatric patients hospitalized for acute infection. Eur. J. Intern. Med. 2017, 37, 7–12. [Google Scholar] [CrossRef]
- Vermeire, S.; Van Assche, G.; Rutgeerts, P. The role of C-reactive protein as an inflammatory marker in gastrointestinal diseases. Nat. Clin. Pract. Gastr. 2005, 2, 580–586. [Google Scholar] [CrossRef]
- Sproston, N.R.; Ashworth, J.J. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef]
- Chandrashekara, S. C-reactive protein: An inflammatory marker with specific role in physiology, pathology, and diagnosis. J. Rheumatol. Clin. Immunol. 2014, 2, S1. [Google Scholar]
- Simental-Mendia, L.E.; Sahebkar, A.; Rodriguez-Moran, M.; Zambrano-Galvan, G.; Guerrero-Romero, F. Effect of Magnesium Supplementation on Plasma C-reactive Protein Concentrations: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Curr. Pharm. Des. 2017, 23, 4678–4686. [Google Scholar] [CrossRef]
- Tang, Y.; Fung, E.; Xu, A.; Lan, H.Y. C-reactive protein and ageing. Clin. Exp. Pharmacol. Physiol. 2017, 44, 9–14. [Google Scholar] [CrossRef]
- Lu, J.; Mold, C.; Du Clos, T.W.; Sun, P.D. Pentraxins and Fc Receptor-Mediated Immune Responses. Front. Immunol. 2018, 9, 2607. [Google Scholar] [CrossRef]
- Pepys, M.B. CRP or not CRP? That Is the Question. Arterioscler Thromb. Vasc. Biol. 2005, 25, 1091–1094. [Google Scholar] [CrossRef]
- Agrawal, A.; Gang, T.B.; Rusinol, A.E. Recognition functions of pentameric C-reactive protein in cardiovascular disease. Mediators Inflamm. 2014, 2014, 319215. [Google Scholar] [CrossRef]
- Ji, S.R.; Wu, Y.; Potempa, L.A.; Qiu, Q.; Zhao, J. Interactions of C-reactive protein with low-density lipoproteins: Implications for an active role of modified C-reactive protein in atherosclerosis. Int. J. Biochem. Cell Biol. 2006, 38, 648–661. [Google Scholar] [CrossRef]
- Khreiss, T.; Jozsef, L.; Potempa, L.A.; Filep, J.G. Conformational rearrangement in C-reactive protein is required for proinflammatory actions on human endothelial cells. Circulation 2004, 109, 2016–2022. [Google Scholar] [CrossRef]
- Pepys, M.B.; Hawkins, P.N.; Kahan, M.C.; Tennent, G.A.; Gallimore, J.R.; Graham, D.; Sabin, C.A.; Zychlinsky, A.; De Diego, J. Pro-inflammatory Effects of Bacterial Recombinant Human C-Reactive Protein are Caused by Contamination with Bacterial Products not by C-Reactive Protein Itself. Circ. Res. 2005, 97, 97–103. [Google Scholar] [CrossRef]
- Molins, B.; Pena, E.; de la Torre, R.; Badimon, L. Monomeric C-reactive protein is prothrombotic and dissociates from circulating pentameric C-reactive protein on adhered activated platelets under flow. Cardiovasc. Res. 2011, 92, 328–337. [Google Scholar] [CrossRef]
- Heuertz, R.M.; Schneider, G.P.; Potempa, L.A.; Webster, R.O. Native and modified C-reactive protein bind different receptors on human neutrophils. Int. J. Biochem. Cell Biol. 2005, 37, 320–335. [Google Scholar] [CrossRef]
- Crossman, D.C.; Morton, A.C.; Gunn, J.P.; Greenwood, J.P.; Hall, A.S.; Fox, K.A.; Lucking, A.J.; Flather, M.D.; Lees, B.; Foley, C.E. Investigation of the effect of Interleukin-1 receptor antagonist (IL-1ra) on markers of inflammation in non-ST elevation acute coronary syndromes (The MRC-ILA-HEART Study). Trials 2008, 9, 8. [Google Scholar] [CrossRef]
- Galea, J.; Ogungbenro, K.; Hulme, S.; Patel, H.; Scarth, S.; Hoadley, M.; Illingworth, K.; McMahon, C.J.; Tzerakis, N.; King, A.T.; et al. Reduction of inflammation after administration of interleukin-1 receptor antagonist following aneurysmal subarachnoid hemorrhage: Results of the Subcutaneous Interleukin-1Ra in SAH (SCIL-SAH) study. J. Neurosurg. 2018, 128, 515–523. [Google Scholar] [CrossRef]
- Tilg, H.; Vannier, E.; Vachino, G.; Dinarello, C.A.; Mier, J.W. Antiinflammatory Properties of Hepatic Acute Phase Proteins: Preferential Induction of Interleukin 1 (IL-1) Receptor Antagonist over ID113 Synthesis by Human Peripheral Blood Mononuclear Cells. J. Exp. Med. 1993, 178, 1629–1636. [Google Scholar] [CrossRef]
- Mold, C.; Rodriguez, W.; Rodic-Polic, B.; Du Clos, T.W. C-Reactive Protein Mediates Protection from Lipopolysaccharide Through Interactions With FcγR. J. Immunol. 2002, 169, 7019–7025. [Google Scholar] [CrossRef]
- Filep, J.; Foldes-Filep, E. Effects of C-reactive protein on human neutrophil granulocytes challenged with N-formyl-methionyl-leucyl-phenylalanine and platelet-activating factor. Life Sci. 1989, 44, 517–524. [Google Scholar] [CrossRef]
- Heuertz, R.M.; Ahmed, N.; Webster, R.O. Peptides derived from C-reactive protein inhibit neutrophil alveolitis. J. Immunol. 1996, 156, 3412–3417. [Google Scholar]
- Heuertz, R.M.; Tricomi, S.M.; Ezekiel, U.R.; Webster, R.O. C-reactive protein inhibits chemotactic peptide-induced p38 mitogen-activated protein kinase activity and human neutrophil movement. J. Biol. Chem. 1999, 274, 17968–17974. [Google Scholar] [CrossRef]
- Kew, R.R.; Hyers, T.M.; Webster, R.O. Human C-reactive protein inhibits neutrophil chemotaxis in vitro: Possible implications for the adult respiratory distress syndrome. J. Lab. Clin. Med. 1990, 115, 339–345. [Google Scholar]
- Ling, M.R.; Chapple, I.L.; Creese, A.J.; Matthews, J.B. Effects of C-reactive protein on the neutrophil respiratory burst in vitro. Innate Immun. 2014, 20, 339–349. [Google Scholar] [CrossRef]
- Devaraj, S.; Dasu, M.R.; Singh, U.; Rao, L.V.; Jialal, I. C-reactive protein stimulates superoxide anion release and tissue factor activity in vivo. Atherosclerosis 2009, 203, 67–74. [Google Scholar] [CrossRef]
- Noren Hooten, N.; Ejiogu, N.; Zonderman, A.B.; Evans, M.K. Association of oxidative DNA damage and C-reactive protein in women at risk for cardiovascular disease. Arterioscler Thromb. Vasc. Biol. 2012, 32, 2776–2784. [Google Scholar] [CrossRef]
- Mortensen, R.F.; Zhong, W. Regulation of phagocytic leukocyte activities by C-reactive protein. J. Leukoc. Biol. 2000, 67, 495–500. [Google Scholar] [CrossRef]
- Cheryk, L.A.; Hayes, M.A.; Gentry, P.A. Modulation of bovine platelet function by C-reactive protein. Vet. Immunol. Immunopathol. 1996, 52, 27–36. [Google Scholar] [CrossRef]
- Fiedel, B.A.; Gewurz, H. Effects of C-reactive protein on platelet function. I. Inhibition of platelet aggregation and release reactions. J. Immunol. 1976, 116, 1289–1294. [Google Scholar]
- Fiedel, B.A.; Gewurz, H. Effects of C-reactive protein on platelet function. II. Inhibition by CRP of platelet reactivities stimulated by poly-L-lysine, ADP, epinephrine, and collagen. J. Immunol. 1976, 117, 1073–1078. [Google Scholar]
- Filep, J.G.; Herman, F.; Kelemen, E.; Foldes-Filep, E. C-reactive protein inhibits binding of platelet-activating factor to human platelets. Thromb. Res. 1991, 61, 411–421. [Google Scholar] [CrossRef]
- Kilpatrick, J.M.; Virella, G. Inhibition of platelet-activating factor by rabbit C-reactive protein. Clin. Immunol. Immunopathol. 1985, 37, 276–281. [Google Scholar] [CrossRef]
- Sestito, A.; Sgueglia, G.A.; Spinelli, A.; Navarese, E.P.; Infusino, F.; Crea, F.; Lanza, G.A. Increased platelet reactivity in unstable angina patients is not related to C-reactive protein levels. Platelets 2006, 17, 336–339. [Google Scholar] [CrossRef]
- Boncler, M.; Luzak, B.; Rozalski, M.; Golanski, J.; Rychlik, B.; Watala, C. Acetylsalicylic acid is compounding to antiplatelet effect of C-reactive protein. Thromb. Res. 2007, 119, 209–216. [Google Scholar] [CrossRef]
- Spieker, L.E.; Flammer, A.J.; Amacker, N.; Sudano, I.; Badimon, J.J.; Ruschitzka, F.; Luscher, T.F.; Noll, G.; Corti, R. C-reactive protein influences shear stress-dependent platelet adhesion in patients with familiar hypercholesterolemia and coronary artery disease undergoing LDL apheresis. Thromb. Haemost. 2006, 96, 540–542. [Google Scholar] [CrossRef]
- Molins, B.; Pena, E.; Vilahur, G.; Mendieta, C.; Slevin, M.; Badimon, L. C-reactive protein isoforms differ in their effects on thrombus growth. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 2239–2246. [Google Scholar] [CrossRef]
- Grad, E.; Pachino, R.M.; Danenberg, H.D. Endothelial C-reactive protein increases platelet adhesion under flow conditions. Am. J. Physiol. Heart Circ. Physiol. 2011, 301, H730–H736. [Google Scholar] [CrossRef][Green Version]
- Yaron, G.; Brill, A.; Dashevsky, O.; Yosef-Levi, I.M.; Grad, E.; Danenberg, H.D.; Varon, D. C-reactive protein promotes platelet adhesion to endothelial cells: A potential pathway in atherothrombosis. Br. J. Haematol. 2006, 134, 426–431. [Google Scholar] [CrossRef]
- Boncler, M.; Rywaniak, J.; Sicinska, P.; Watala, C. Effectiveness of modified C-reactive protein in the modulation of platelet function under different experimental conditions. Blood Coagul Fibrinolysis 2011, 22, 301–309. [Google Scholar] [CrossRef]
- Boncler, M.; Rywaniak, J.; Szymanski, J.; Potempa, L.A.; Rychlik, B.; Watala, C. Modified C-reactive protein interacts with platelet glycoprotein Ib alpha. Pharmacol. Rep. 2011, 63, 464–475. [Google Scholar] [CrossRef]
- Skoglund, C.; Wettero, J.; Skogh, T.; Sjowall, C.; Tengvall, P.; Bengtsson, T. C-reactive protein and C1q regulate platelet adhesion and activation on adsorbed immunoglobulin G and albumin. Immunol. Cell Biol. 2008, 86, 466–474. [Google Scholar] [CrossRef]
- Pasceri, V.; Willerson, J.T.; Yeh, E.T. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation 2000, 102, 2165–2168. [Google Scholar] [CrossRef]
- Pasceri, V.; Cheng, J.S.; Willerson, J.T.; Yeh, E.T. Modulation of C-reactive protein-mediated monocyte chemoattractant protein-1 induction in human endothelial cells by anti-atherosclerosis drugs. Circulation 2001, 103, 2531–2534. [Google Scholar] [CrossRef]
- Venugopal, S.K.; Devaraj, S.; Yuhanna, I.; Shaul, P.; Jialal, I. Demonstration that C-reactive protein decreases eNOS expression and bioactivity in human aortic endothelial cells. Circulation 2002, 106, 1439–1441. [Google Scholar] [CrossRef]
- Verma, S.; Wang, C.H.; Li, S.H.; Dumont, A.S.; Fedak, P.W.; Badiwala, M.V.; Dhillon, B.; Weisel, R.D.; Li, R.K.; Mickle, D.A.; et al. A self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesis. Circulation 2002, 106, 913–919. [Google Scholar] [CrossRef]
- Grad, E.; Danenberg, H.D. C-reactive protein and atherothrombosis: Cause or effect? Blood Rev. 2013, 27, 23–29. [Google Scholar] [CrossRef]
- Tvarijonaviciute, A.; Aznar-Cayuela, C.; Rubio, C.P.; Ceron, J.J.; López-Jornet, P. Evaluation of salivary oxidate stress biomarkers, nitric oxide and C-reactive protein in patients with oral lichen planus and burning mouth syndrome. J. Oral. Pathol. Med. 2016, 46, 387–392. [Google Scholar] [CrossRef]
- Fichtlscherer, S.; Rosenberger, G.; Walter, D.H.; Breuer, S.; Dimmeler, S.; Zeiher, A.M. Elevated C-reactive protein levels and impaired endothelial vasoreactivity in patients with coronary artery disease. Circulation 2000, 102, 1000–1006. [Google Scholar] [CrossRef]
- Nabata, A.; Kuroki, M.; Ueba, H.; Hashimoto, S.; Umemoto, T.; Wada, H.; Yasu, T.; Saito, M.; Momomura, S.; Kawakami, M. C-reactive protein induces endothelial cell apoptosis and matrix metalloproteinase-9 production in human mononuclear cells: Implications for the destabilization of atherosclerotic plaque. Atherosclerosis 2008, 196, 129–135. [Google Scholar] [CrossRef]
- Venugopal, S.K.; Devaraj, S.; Jialal, I. C-reactive protein decreases prostacyclin release from human aortic endothelial cells. Circulation 2003, 108, 1676–1678. [Google Scholar] [CrossRef]
- Hein, T.W.; Qamirani, E.; Ren, Y.; Kuo, L. C-reactive protein impairs coronary arteriolar dilation to prostacyclin synthase activation: Role of peroxynitrite. J. Mol. Cell Cardiol. 2009, 47, 196–202. [Google Scholar] [CrossRef]
- Devaraj, S.; Xu, D.Y.; Jialal, I. C-reactive protein increases plasminogen activator inhibitor-1 expression and activity in human aortic endothelial cells: Implications for the metabolic syndrome and atherothrombosis. Circulation 2003, 107, 398–404. [Google Scholar] [CrossRef]
- Ji, Y.; Fish, P.M.; Strawn, T.L.; Lohman, A.W.; Wu, J.; Szalai, A.J.; Fay, W.P. C-reactive protein induces expression of tissue factor and plasminogen activator inhibitor-1 and promotes fibrin accumulation in vein grafts. J. Thromb. Haemost. 2014, 12, 1667–1677. [Google Scholar] [CrossRef]
- Singh, U.; Devaraj, S.; Jialal, I. C-Reactive Protein Decreases Tissue Plasminogen Activator Activity in Human Aortic Endothelial Cells Evidence that C-Reactive Protein Is a Procoagulant. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 2216–2221. [Google Scholar] [CrossRef]
- Cermak, J.; Key, N.S.; Bach, R.R.; Balla, J.; Jacob, H.S.; Vercellotti, G.M. C-Reactive Protein Induces Human Peripheral Blood Monocytes to Synthesize Tissue Factor. Blood 1993, 82, 513–520. [Google Scholar]
- Cirillo, P.; Golino, P.; Calabro, P.; Calì, G.; Ragni, M.; De Rosa, S.; Cimmino, G.; Pacileo, M.; De Palma, R.; Forte, L.; et al. C-reactive protein induces tissue factor expression and promotes smooth muscle and endothelial cell proliferation. Cardiovasc. Res. 2005, 68, 47–55. [Google Scholar] [CrossRef]
- Paffen, E.; Vos, H.L.; Bertina, R.M. C-Reactive Protein Does Not Directly Induce Tissue Factor in Human Monocytes. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 975–981. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mousa, S.A. Inhibitory effect of C-reactive protein on the release of tissue factor pathway inhibitor from human endothelial cells: Reversal by low molecular weight heparin. Int. Angiol. 2006, 25, 10–13. [Google Scholar] [CrossRef]
- Li, L.; Roumeliotis, N.; Sawamura, T.; Renier, G. C-reactive protein enhances LOX-1 expression in human aortic endothelial cells: Relevance of LOX-1 to C-reactive protein-induced endothelial dysfunction. Circ. Res. 2004, 95, 877–883. [Google Scholar] [CrossRef]
- Wang, C.H.; Li, S.H.; Weisel, R.D.; Fedak, P.W.; Dumont, A.S.; Szmitko, P.; Li, R.K.; Mickle, D.A.; Verma, S. C-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscle. Circulation 2003, 107, 1783–1790. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, S.; Yun, J.M.; Adamson, G.; Galvez, J.; Jialal, I. C-reactive protein impairs the endothelial glycocalyx resulting in endothelial dysfunction. Cardiovasc. Res. 2009, 84, 479–484. [Google Scholar] [CrossRef]
- Bisoendial, R.J.; Kastelein, J.J.; Levels, J.H.; Zwaginga, J.J.; van den Bogaard, B.; Reitsma, P.H.; Meijers, J.C.; Hartman, D.; Levi, M.; Stroes, E.S. Activation of Inflammation and Coagulation After Infusion of C-Reactive Protein in Humans. Circ. Res. 2005, 96, 714–716. [Google Scholar] [CrossRef] [PubMed]
- Bisoendial, R.J.; Kastelein, J.J.; Peters, S.L.; Levels, J.H.; Birjmohun, R.; Rotmans, J.I.; Hartman, D.; Meijers, J.C.; Levi, M.; Stroes, E.S. Effects of CRP infusion on endothelial function and coagulation in normocholesterolemic and hypercholesterolemic subjects. J. Lipid Res. 2007, 48, 952–960. [Google Scholar] [CrossRef]
- Xu, P.C.; Lin, S.; Yang, X.W.; Gu, D.M.; Yan, T.K.; Wei, L.; Wang, B.L. C-reactive protein enhances activation of coagulation system and inflammatory response through dissociating into monomeric form in antineutrophil cytoplasmic antibody-associated vasculitis. BMC Immunol. 2015, 16, 10. [Google Scholar] [CrossRef]
- Biggs, T.C.; Bird, J.H.; Frampton, S.J.; Harries, P.G.; Salib, R.J. C-reactive protein and coagulation studies in secondary post-tonsillectomy haemorrhage—Need for routine testing? Our experience in ninety-three patients. Clin. Otolaryngol. 2014, 39, 238–240. [Google Scholar] [CrossRef]
- Pepys, M.B.; Hirschfield, G.M.; Tennent, G.A.; Gallimore, J.R.; Kahan, M.C.; Bellotti, V.; Hawkins, P.N.; Myers, R.M.; Smith, M.D.; Polara, A.; et al. Targeting C-reactive protein for the treatment of cardiovascular disease. Nature 2006, 440, 1217–1221. [Google Scholar] [CrossRef]
- Thiele, J.R.; Habersberger, J.; Braig, D.; Schmidt, Y.; Goerendt, K.; Maurer, V.; Bannasch, H.; Scheichl, A.; Woollard, K.J.; von Dobschutz, E.; et al. Dissociation of pentameric to monomeric C-reactive protein localizes and aggravates inflammation: In vivo proof of a powerful proinflammatory mechanism and a new anti-inflammatory strategy. Circulation 2014, 130, 35–50. [Google Scholar] [CrossRef]
- Slevin, M.; Iemma, R.S.; Zeinolabediny, Y.; Liu, D.; Ferris, G.R.; Caprio, V.; Phillips, N.; Di Napoli, M.; Guo, B.; Zeng, X.; et al. Acetylcholine Inhibits Monomeric C-Reactive Protein Induced Inflammation, Endothelial Cell Adhesion, and Platelet Aggregation; A Potential Therapeutic? Front. Immunol. 2018, 9, 2124. [Google Scholar] [CrossRef] [PubMed]
- Hounsell, E.F.; Davies, M.J.; Renouf, D.V. O-linked protein glycosylation structure and function. Glycoconj. J. 1996, 13, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Spiro, R.G. Protein glycosylation: Nature, distribution, enzymatic formation, and disease implications of glycopeptide bonds. Glycobiology 2002, 12, 43R–56R. [Google Scholar] [CrossRef]
- Sola, R.J.; Griebenow, K. Glycosylation of therapeutic proteins: An effective strategy to optimize efficacy. BioDrugs 2010, 24, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Goettig, P. Effects of Glycosylation on the Enzymatic Activity and Mechanisms of Proteases. Int. J. Mol. Sci. 2016, 17, 1969. [Google Scholar] [CrossRef] [PubMed]
- Ohtsubo, K.; Marth, J.D. Glycosylation in cellular mechanisms of health and disease. Cell 2006, 126, 855–867. [Google Scholar] [CrossRef] [PubMed]
- Gornik, O.; Lauc, G. Glycosylation of serum proteins in inflammatory diseases. Dis. Markers 2008, 25, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Das, T.; Sen, A.K.; Kempf, T.; Pramanik, S.R.; Mandal, C.; Mandal, C. Induction of glycosylation in human C-reactive protein under different pathological conditions. Biochem. J. 2003, 373, 345–355. [Google Scholar] [CrossRef]
- Vigushin, D.M.; Pepys, M.B.; Hawkins, P.N. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J. Clin. Invest. 1993, 91, 1351–1357. [Google Scholar] [CrossRef]
- Das, T.; Mandal, C.; Mandal, C. Variations in binding characteristics of glycosylated human C-reactive proteins in different pathological conditions. Glycoconj. J. 2004, 20, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Ansar, W.; Mukhopadhyay, S.; Habib, S.K.; Basu, S.; Saha, B.; Sen, A.K.; Mandal, C.N.; Mandal, C. Disease-associated glycosylated molecular variants of human C-reactive protein activate complement-mediated hemolysis of erythrocytes in tuberculosis and Indian visceral leishmaniasis. Glycoconj. J. 2009, 26, 1151–1169. [Google Scholar] [CrossRef]
- Wang, H.W.; Wu, Y.; Chen, Y.; Sui, S.F. Polymorphism of structural forms of C-reactive protein. Int. J. Mol. Med. 2002, 9, 665–671. [Google Scholar] [CrossRef] [PubMed]
- Blizniukov, O.P.; Kozmin, L.D.; Falikova, V.V.; Martynov, A.I.; Tischenko, V.M. Effect of Calcium Ions on Hydrodynamic Properties of Pentameric and Decameric C-Reactive Protein in Solution. Mol. Biol. (Mosk) 2003, 37, 912–919. [Google Scholar] [CrossRef]
- Okemefuna, A.I.; Stach, L.; Rana, S.; Buetas, A.J.; Gor, J.; Perkins, S.J. C-reactive protein exists in an NaCl concentration-dependent pentamer-decamer equilibrium in physiological buffer. J. Biol. Chem. 2010, 285, 1041–1052. [Google Scholar] [CrossRef]
- Li, Q.; Xu, W.; Xue, X.; Wang, Q.; Han, L.; Li, W.; Lv, S.; Liu, D.; Richards, J.; Shen, Z.; et al. Presence of multimeric isoforms of human C-reactive protein in tissues and blood. Mol. Med. Rep. 2016, 14, 5461–5466. [Google Scholar] [CrossRef][Green Version]
- Wu, Y.; Ji, S.R.; Wang, H.W.; Sui, S.F. Study of the spontaneous dissociation of rabbit C-reactive protein. Biochemistry (Mosc) 2002, 67, 1377–1382. [Google Scholar] [CrossRef] [PubMed]
- Potempa, L.A.; Siegel, J.N.; Fiedel, B.A.; Potempa, R.T.; Gewurz, H. Expression, detection and assay of a neoantigen (Neo-CRP) associated with a free, human C-reactive protein subunit. Mol. Immunol. 1987, 24, 531–541. [Google Scholar] [CrossRef]
- Sui, S.F.; Liu, Z.; Li, W.; Xiao, C.; Wang, S.; Gao, Q.; Zhou, Q. Two-dimensional crystallization of rabbit C-reactive protein on lipid monolayers. FEBS Lett. 1996, 388, 103–111. [Google Scholar] [CrossRef]
- Wang, H.W.; Sui, S.F. Dissociation and subunit rearrangement of membrane-bound human C-reactive proteins. Biochem. Biophys. Res. Commun. 2001, 288, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, H.W.; Ji, S.R.; Sui, S.F. Two-dimensional crystallization of rabbit C-reactive protein monomeric subunits. Acta Crystallogr. D Biol. Crystallogr. 2003, 59, 922–926. [Google Scholar] [CrossRef]
- Ji, S.R.; Wu, Y.; Zhu, L.; Potempa, L.A.; Sheng, F.L.; Lu, W.; Zhao, J. Cell membranes and liposomes dissociate C-reactive protein (CRP) to form a new, biologically active structural intermediate: mCRP(m). FASEB J. 2007, 21, 284–294. [Google Scholar] [CrossRef] [PubMed]
- de la Torre, R.; Pena, E.; Vilahur, G.; Slevin, M.; Badimon, L. Monomerization of C-reactive protein requires glycoprotein IIb-IIIa activation: Pentraxins and platelet deposition. J. Thromb. Haemost. 2013, 11, 2048–2058. [Google Scholar] [CrossRef] [PubMed]
- Eisenhardt, S.U.; Habersberger, J.; Murphy, A.; Chen, Y.C.; Woollard, K.J.; Bassler, N.; Qian, H.; von Zur Muhlen, C.; Hagemeyer, C.E.; Ahrens, I.; et al. Dissociation of pentameric to monomeric C-reactive protein on activated platelets localizes inflammation to atherosclerotic plaques. Circ. Res. 2009, 105, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Braig, D.; Kaiser, B.; Thiele, J.R.; Bannasch, H.; Peter, K.; Stark, G.B.; Koch, H.G.; Eisenhardt, S.U. A conformational change of C-reactive protein in burn wounds unmasks its proinflammatory properties. Int. Immunol. 2014, 26, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Lauer, N.; Mihlan, M.; Hartmann, A.; Schlotzer-Schrehardt, U.; Keilhauer, C.; Scholl, H.P.; Charbel Issa, P.; Holz, F.; Weber, B.H.; Skerka, C.; et al. Complement regulation at necrotic cell lesions is impaired by the age-related macular degeneration-associated factor-H His402 risk variant. J. Immunol. 2011, 187, 4374–4383. [Google Scholar] [CrossRef]
- Mihlan, M.; Blom, A.M.; Kupreishvili, K.; Lauer, N.; Stelzner, K.; Bergstrom, F.; Niessen, H.W.; Zipfel, P.F. Monomeric C-reactive protein modulates classic complement activation on necrotic cells. FASEB J. 2011, 25, 4198–4210. [Google Scholar] [CrossRef]
- Hammond, D.J. Jr.; Singh, S.K.; Thompson, J.A.; Beeler, B.W.; Rusinol, A.E.; Pangburn, M.K.; Potempa, L.A.; Agrawal, A. Identification of acidic pH-dependent ligands of pentameric C-reactive protein. J. Biol. Chem. 2010, 285, 36235–36244. [Google Scholar] [CrossRef]
- Boncler, M.; Kehrel, B.; Szewczyk, R.; Stec-Martyna, E.; Bednarek, R.; Brodde, M.; Watala, C. Oxidation of C-reactive protein by hypochlorous acid leads to the formation of potent platelet activator. Int. J. Biol. Macromol. 2018, 107, 2701–2714. [Google Scholar] [CrossRef]
- Singh, S.K.; Thirumalai, A.; Pathak, A.; Ngwa, D.N.; Agrawal, A. Functional Transformation of C-reactive Protein by Hydrogen Peroxide. J. Biol. Chem. 2017, 292, 3129–3136. [Google Scholar] [CrossRef]
- Habersberger, J.; Strang, F.; Scheichl, A.; Htun, N.; Bassler, N.; Merivirta, R.M.; Diehl, P.; Krippner, G.; Meikle, P.; Eisenhardt, S.U.; et al. Circulating microparticles generate and transport monomeric C-reactive protein in patients with myocardial infarction. Cardiovasc. Res. 2012, 96, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Strang, F.; Scheichl, A.; Chen, Y.C.; Wang, X.; Htun, N.M.; Bassler, N.; Eisenhardt, S.U.; Habersberger, J.; Peter, K. Amyloid plaques dissociate pentameric to monomeric C-reactive protein: A novel pathomechanism driving cortical inflammation in Alzheimer’s disease? Brain Pathol. 2012, 22, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Ji, S.R.; Wu, Y.; Potempa, L.A.; Liang, Y.H.; Zhao, J. Effect of modified C-reactive protein on complement activation: A possible complement regulatory role of modified or monomeric C-reactive protein in atherosclerotic lesions. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Mihlan, M.; Stippa, S.; Jozsi, M.; Zipfel, P.F. Monomeric CRP contributes to complement control in fluid phase and on cellular surfaces and increases phagocytosis by recruiting factor H. Cell Death Differ. 2009, 16, 1630–1640. [Google Scholar] [CrossRef] [PubMed]
- Ji, S.R.; Ma, L.; Bai, C.J.; Shi, J.M.; Li, H.Y.; Potempa, L.A.; Filep, J.G.; Zhao, J.; Wu, Y. Monomeric C-reactive protein activates endothelial cells via interaction with lipid raft microdomains. FASEB J. 2009, 23, 1806–1816. [Google Scholar] [CrossRef] [PubMed]
- Khreiss, T.; Jozsef, L.; Hossain, S.; Chan, J.S.; Potempa, L.A.; Filep, J.G. Loss of pentameric symmetry of C-reactive protein is associated with delayed apoptosis of human neutrophils. J. Biol. Chem. 2002, 277, 40775–40781. [Google Scholar] [CrossRef] [PubMed]
- Khreiss, T.; Jozsef, L.; Potempa, L.A.; Filep, J.G. Opposing effects of C-reactive protein isoforms on shear-induced neutrophil-platelet adhesion and neutrophil aggregation in whole blood. Circulation 2004, 110, 2713–2720. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Khreiss, T.; Jozsef, L.; Potempa, L.A.; Filep, J.G. Loss of pentameric symmetry in C-reactive protein induces interleukin-8 secretion through peroxynitrite signaling in human neutrophils. Circ. Res. 2005, 97, 690–697. [Google Scholar] [CrossRef]
- Zouki, C.; Haas, B.; Chan, J.S.; Potempa, L.A.; Filep, J.G. Loss of pentameric symmetry of C-reactive protein is associated with promotion of neutrophil-endothelial cell adhesion. J. Immunol. 2001, 167, 5355–5361. [Google Scholar] [CrossRef]
- Li, H.Y.; Wang, J.; Meng, F.; Jia, Z.K.; Su, Y.; Bai, Q.F.; Lv, L.L.; Ma, F.R.; Potempa, L.A.; Yan, Y.B.; et al. An Intrinsically Disordered Motif Mediates Diverse Actions of Monomeric C-reactive Protein. J. Biol. Chem. 2016, 291, 8795–8804. [Google Scholar] [CrossRef]
- Schwedler, S.B.; Guderian, F.; Dammrich, J.; Potempa, L.A.; Wanner, C. Tubular staining of modified C-reactive protein in diabetic chronic kidney disease. Nephrol. Dial. Transplant. 2003, 18, 2300–2307. [Google Scholar] [CrossRef][Green Version]
- Crawford, J.R.; Trial, J.; Nambi, V.; Hoogeveen, R.C.; Taffet, G.E.; Entman, M.L. Plasma Levels of Endothelial Microparticles Bearing Monomeric C-reactive Protein are Increased in Peripheral Artery Disease. J. Cardiovasc. Transl. Res. 2016, 9, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.P.; Hsu, H.Y.; Chiou, A.; Tseng, K.Y.; Lin, H.Y.; Chang, G.L.; Chen, S.J. Immunodetection of pentamer and modified C-reactive protein using surface plasmon resonance biosensing. Biosens. Bioelectron. 2006, 21, 1631–1637. [Google Scholar] [CrossRef] [PubMed]
- Ying, S.C.; Gewurz, H.; Kinoshita, C.M.; Potempa, L.A.; Siegel, J.N. Identification and partial characterization of multiple native and neoantigenic epitopes of human C-reactive protein by using monoclonal antibodies. J. Immunol. 1989, 143, 221–228. [Google Scholar] [PubMed]
- Ying, S.C.; Shephard, E.; de Beer, F.C.; Siegel, J.N.; Harris, D.; Gewurz, B.E.; Fridkin, M.; Gewurz, H. Localization of sequence-determined neoepitopes and neutrophil digestion fragments of C-reactive protein utilizing monoclonal antibodies and synthetic peptides. Mol. Immunol. 1992, 29, 677–687. [Google Scholar] [CrossRef]
- Bell, S.A.; Faust, H.; Schmid, A.; Meurer, M. Autoantibodies to C-reactive protein (CRP) and other acute-phase proteins in systemic autoimmune diseases. Clin. Exp. Immunol. 1998, 113, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Sjowall, C.; Eriksson, P.; Almer, S.; Skogh, T. Autoantibodies to C-reactive protein is a common finding in SLE, but not in primary Sjögren’s syndrome, rheumatoid arthritis or inflammatory bowel disease. J. Autoimmun. 2002, 19, 155–160. [Google Scholar] [CrossRef]
- Tan, Y.; Yu, F.; Yang, H.; Chen, M.; Fang, Q.; Zhao, M.H. Autoantibodies against monomeric C-reactive protein in sera from patients with lupus nephritis are associated with disease activity and renal tubulointerstitial lesions. Hum. Immunol. 2008, 69, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.Y.; Li, H.Y.; Fu, G.; Yu, F.; Wu, Y.; Zhao, M.H. Autoantibodies against C-Reactive Protein Influence Complement Activation and Clinical Course in Lupus Nephritis. J. Am. Soc. Nephrol. 2017, 28, 3044–3054. [Google Scholar] [CrossRef] [PubMed]
- Hirschfield, G.M.; Gallimore, J.R.; Kahan, M.C.; Hutchinson, W.L.; Sabin, C.A.; Benson, G.M.; Dhillon, A.P.; Tennent, G.A.; Pepys, M.B. Transgenic human C-reactive protein is not proatherogenic in apolipoprotein E-deficient mice. Proc. Natl. Acad. Sci. USA 2005, 102, 8309–8314. [Google Scholar] [CrossRef]
- Koike, T.; Kitajima, S.; Yu, Y.; Nishijima, K.; Zhang, J.; Ozaki, Y.; Morimoto, M.; Watanabe, T.; Bhakdi, S.; Asada, Y.; et al. Human C-reactive protein does not promote atherosclerosis in transgenic rabbits. Circulation 2009, 120, 2088–2094. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kovacs, A.; Tornvall, P.; Nilsson, R.; Tegner, J.; Hamsten, A.; Bjorkegren, J. Human C-reactive protein slows atherosclerosis development in a mouse model with human-like hypercholesterolemia. Proc. Natl. Acad. Sci. USA 2007, 104, 13768–13773. [Google Scholar] [CrossRef]
- Paul, A.; Ko, K.W.; Li, L.; Yechoor, V.; McCrory, M.A.; Szalai, A.J.; Chan, L. C-reactive protein accelerates the progression of atherosclerosis in apolipoprotein E-deficient mice. Circulation 2004, 109, 647–655. [Google Scholar] [CrossRef]
- Reifenberg, K.; Lehr, H.A.; Baskal, D.; Wiese, E.; Schaefer, S.C.; Black, S.; Samols, D.; Torzewski, M.; Lackner, K.J.; Husmann, M.; et al. Role of C-reactive protein in atherogenesis: Can the apolipoprotein E knockout mouse provide the answer? Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1641–1646. [Google Scholar] [CrossRef]
- Teupser, D.; Weber, O.; Rao, T.N.; Sass, K.; Thiery, J.; Fehling, H.J. No reduction of atherosclerosis in C-reactive protein (CRP)-deficient mice. J. Biol. Chem. 2011, 286, 6272–6279. [Google Scholar] [CrossRef] [PubMed]
- Trion, A.; de Maat, M.P.; Jukema, J.W.; van der Laarse, A.; Maas, M.C.; Offerman, E.H.; Havekes, L.M.; Szalai, A.J.; Princen, H.M.; Emeis, J.J. No effect of C-reactive protein on early atherosclerosis development in apolipoprotein E*3-leiden/human C-reactive protein transgenic mice. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1635–1640. [Google Scholar] [CrossRef]
- Elliott, P.; Chambers, J.C.; Zhang, W.; Clarke, R.; Hopewell, J.C.; Peden, J.F.; Erdmann, J.; Braund, P.; Engert, J.C.; Bennett, D.; et al. Genetic Loci associated with C-reactive protein levels and risk of coronary heart disease. JAMA 2009, 302, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M. From C-Reactive Protein to Interleukin-6 to Interleukin-1: Moving Upstream To Identify Novel Targets for Atheroprotection. Circ. Res. 2016, 118, 145–156. [Google Scholar] [CrossRef]
- Zacho, J.; Tybjaerg-Hansen, A.; Jensen, J.S.; Grande, P.; Sillesen, H.; Nordestgaard, B.G. Genetically elevated C-reactive protein and ischemic vascular disease. N Engl. J. Med. 2008, 359, 1897–1908. [Google Scholar] [CrossRef]
- Jia, Z.K.; Li, H.Y.; Liang, Y.L.; Potempa, L.A.; Ji, S.R.; Wu, Y. Monomeric C-Reactive Protein Binds and Neutralizes Receptor Activator of NF-κB Ligand-Induced Osteoclast Differentiation. Front. Immunol. 2018, 9, 234. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tang, B.; Liu, X.; Wu, X.; Wang, H.; Xu, D.; Guo, Y. Increased monomeric CRP levels in acute myocardial infarction: A possible new and specific biomarker for diagnosis and severity assessment of disease. Atherosclerosis 2015, 239, 343–349. [Google Scholar] [CrossRef]
- Zhang, L.; Li, H.Y.; Li, W.; Shen, Z.Y.; Wang, Y.D.; Ji, S.R.; Wu, Y. An ELISA Assay for Quantifying Monomeric C-Reactive Protein in Plasma. Front. Immunol. 2018, 9, 511. [Google Scholar] [CrossRef]
- Lee, J.W. Method validation and application of protein biomarkers: Basic similarities and differences from biotherapeutics. Bioanalysis 2009, 1, 1461–1474. [Google Scholar] [CrossRef] [PubMed]
- Dasu, M.R.; Devaraj, S.; Du Clos, T.W.; Jialal, I. The biological effects of CRP are not attributable to endotoxin contamination: Evidence from TLR4 knockdown human aortic endothelial cells. J. Lipid Res. 2007, 48, 509–512. [Google Scholar] [CrossRef]
- Potempa, L.A.; Yao, Z.Y.; Ji, S.R.; Filep, J.G.; Wu, Y. Solubilization and purification of recombinant modified C-reactive protein from inclusion bodies using reversible anhydride modification. Biophys. Rep. 2015, 1, 18–33. [Google Scholar] [CrossRef] [PubMed]
- Taylor, K.E.; Giddings, J.C.; Van Den Berg, C.W. C-Reactive Protein–Induced In Vitro Endothelial Cell Activation Is an Artefact Caused by Azide and Lipopolysaccharide. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 1225–1230. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thiele, J.R.; Zeller, J.; Bannasch, H.; Stark, G.B.; Peter, K.; Eisenhardt, S.U. Targeting C-Reactive Protein in Inflammatory Disease by Preventing Conformational Changes. Mediators Inflamm. 2015, 2015, 372432. [Google Scholar] [CrossRef]
- Boguslawski, G.; McGlynn, P.W.; Potempa, L.A.; Filep, J.G.; Labarrere, C.A. Conduct unbecoming: C-reactive protein interactions with a broad range of protein molecules. J. Heart Lung Transplant. 2007, 26, 705–713. [Google Scholar] [CrossRef] [PubMed]
- Boncler, M.; Dudzinska, D.; Nowak, J.; Watala, C. Modified C-reactive protein selectively binds to immunoglobulins. Scand. J. Immunol 2012, 76, 1–10. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boncler, M.; Wu, Y.; Watala, C. The Multiple Faces of C-Reactive Protein—Physiological and Pathophysiological Implications in Cardiovascular Disease. Molecules 2019, 24, 2062. https://doi.org/10.3390/molecules24112062
Boncler M, Wu Y, Watala C. The Multiple Faces of C-Reactive Protein—Physiological and Pathophysiological Implications in Cardiovascular Disease. Molecules. 2019; 24(11):2062. https://doi.org/10.3390/molecules24112062
Chicago/Turabian StyleBoncler, Magdalena, Yi Wu, and Cezary Watala. 2019. "The Multiple Faces of C-Reactive Protein—Physiological and Pathophysiological Implications in Cardiovascular Disease" Molecules 24, no. 11: 2062. https://doi.org/10.3390/molecules24112062
APA StyleBoncler, M., Wu, Y., & Watala, C. (2019). The Multiple Faces of C-Reactive Protein—Physiological and Pathophysiological Implications in Cardiovascular Disease. Molecules, 24(11), 2062. https://doi.org/10.3390/molecules24112062





