Synergic Activity Against MCF-7 Breast Cancer Cell Growth of Nanocurcumin-Encapsulated and Cisplatin-Complexed Nanogels
Abstract
1. Introduction
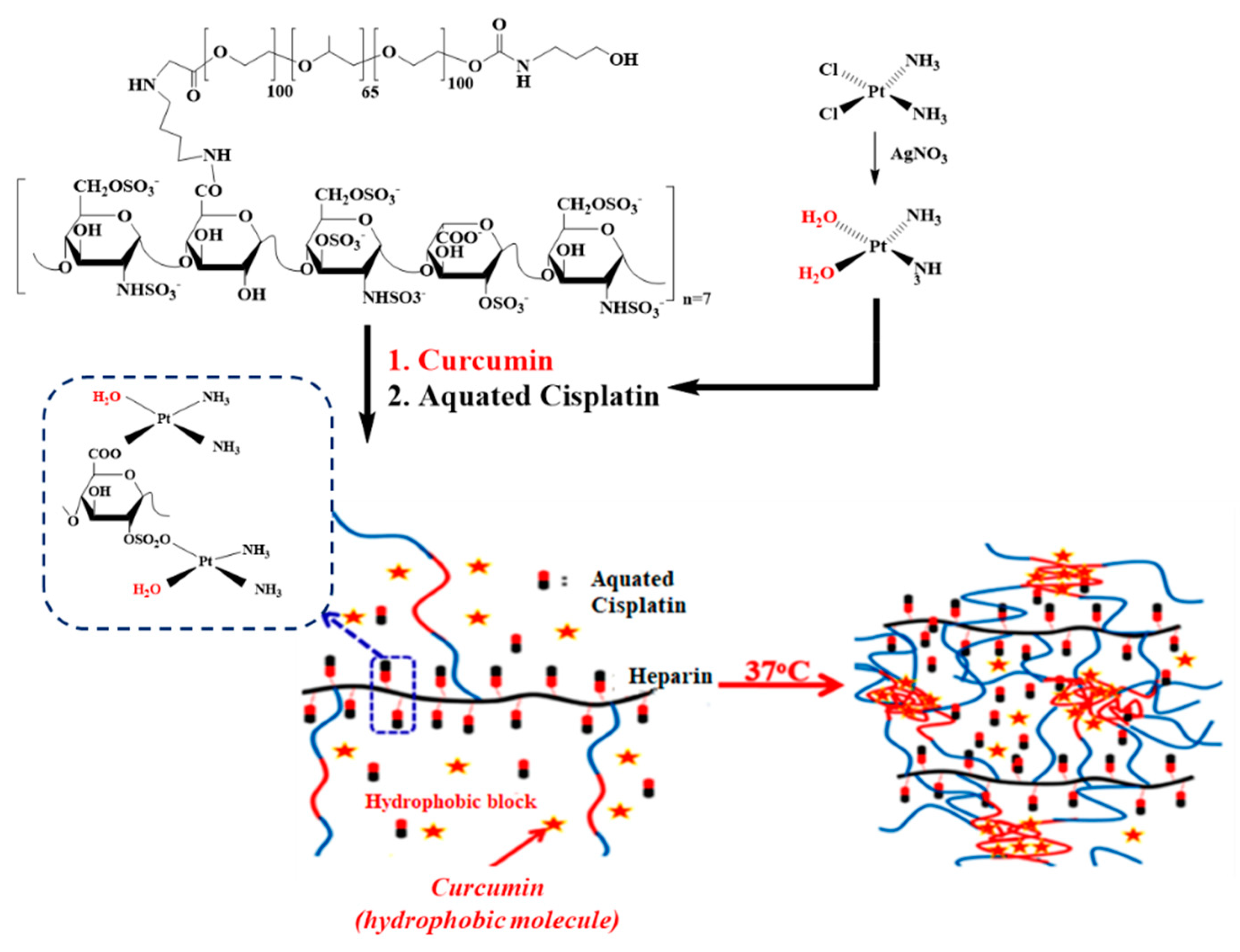
2. Results and Discussion
2.1. Characterizations of the Amphiphilic Hep-F127
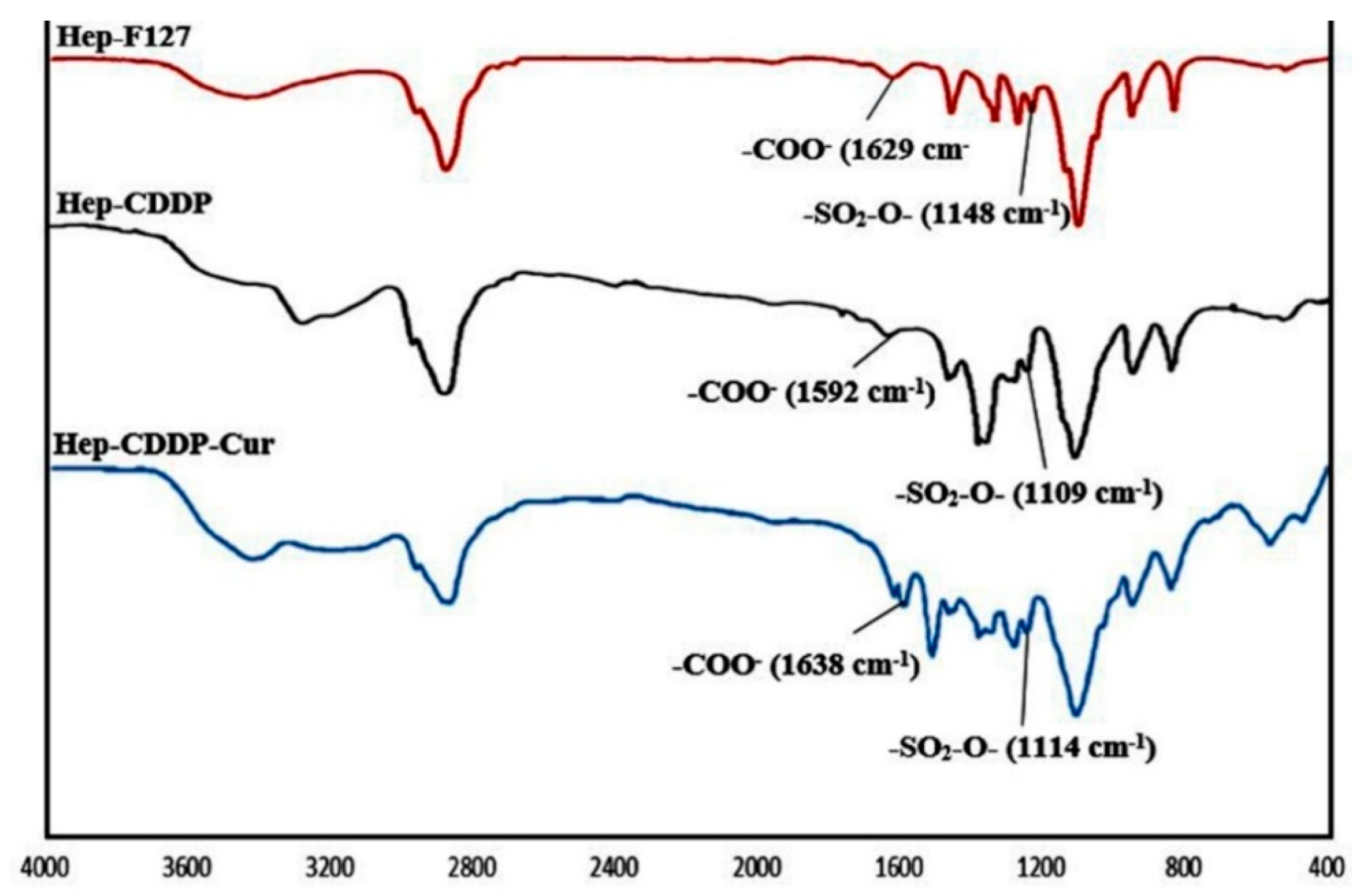
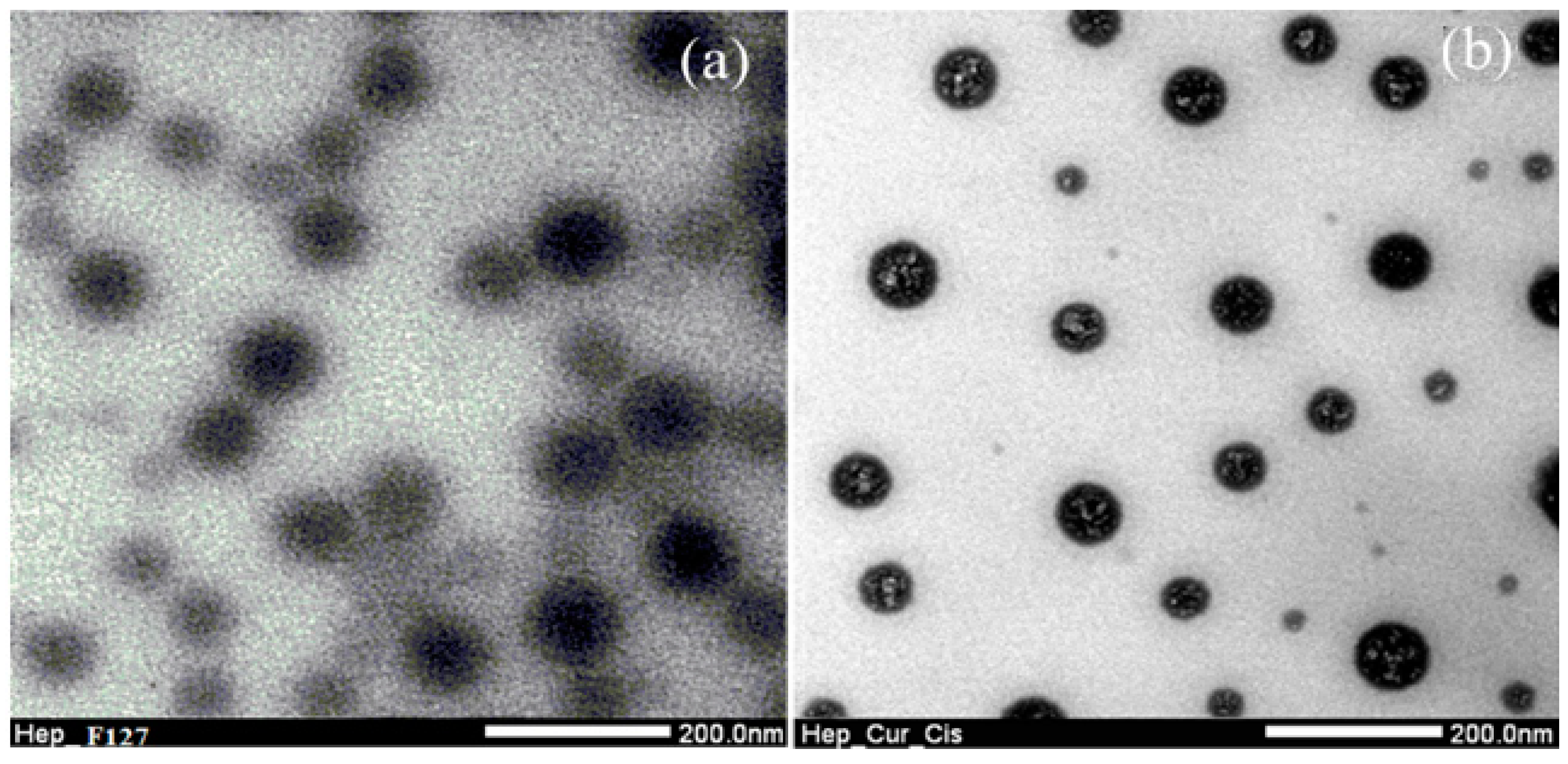
2.2. Characterizations of Nano-Complexes
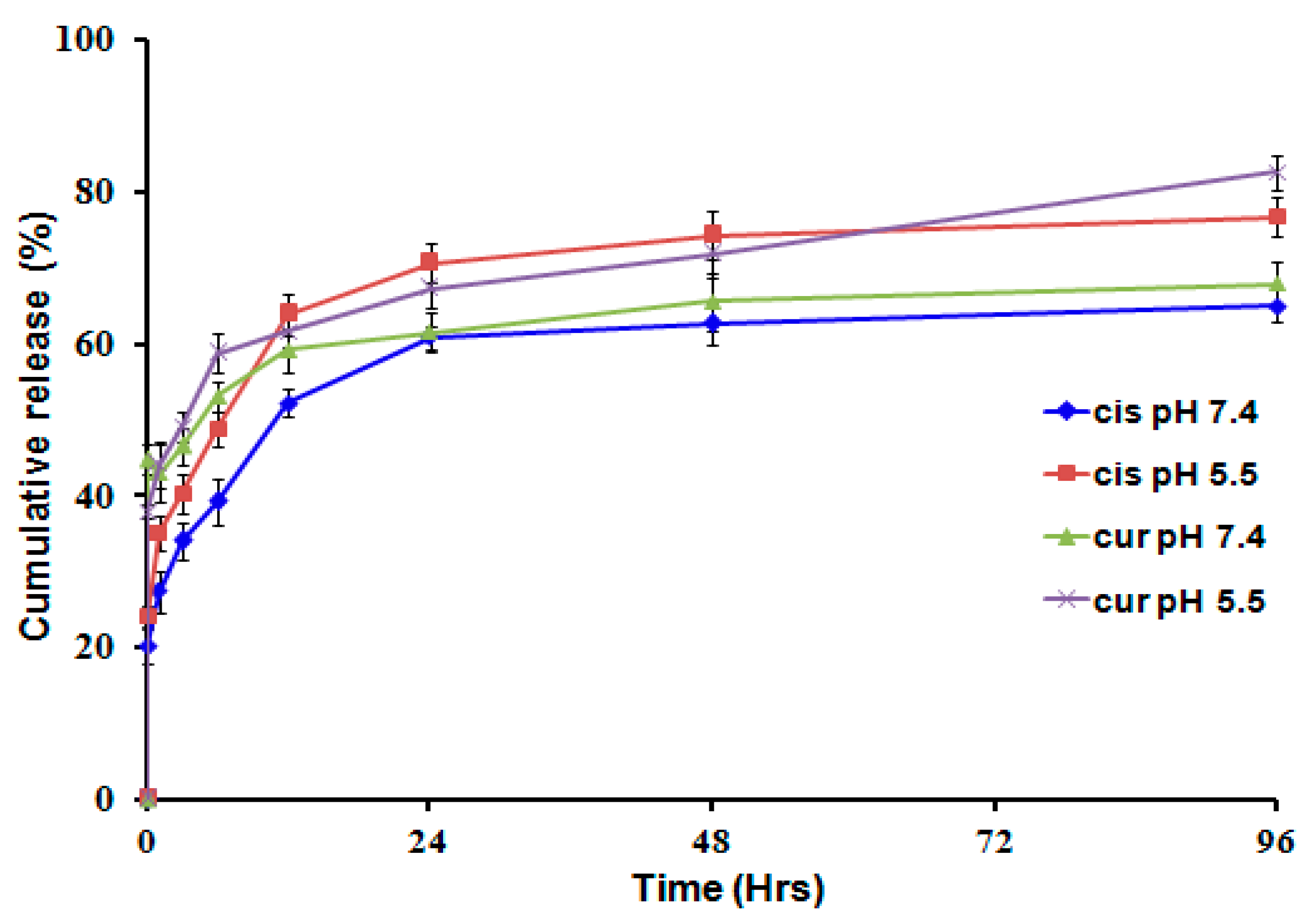
2.3. Dual Drug Releasing Profiles from the Nanocarrier
2.4. Cytotoxicity Assay
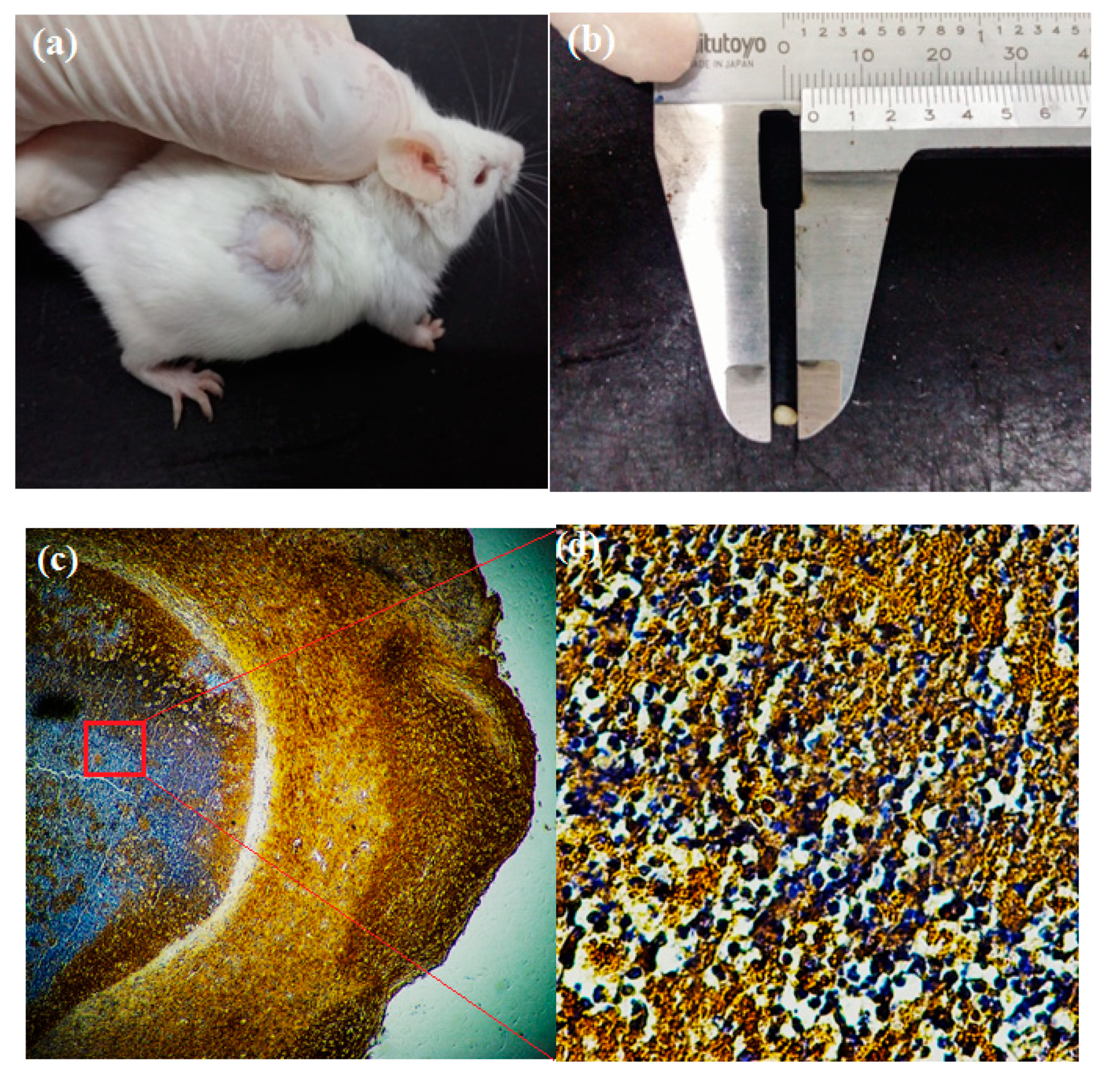
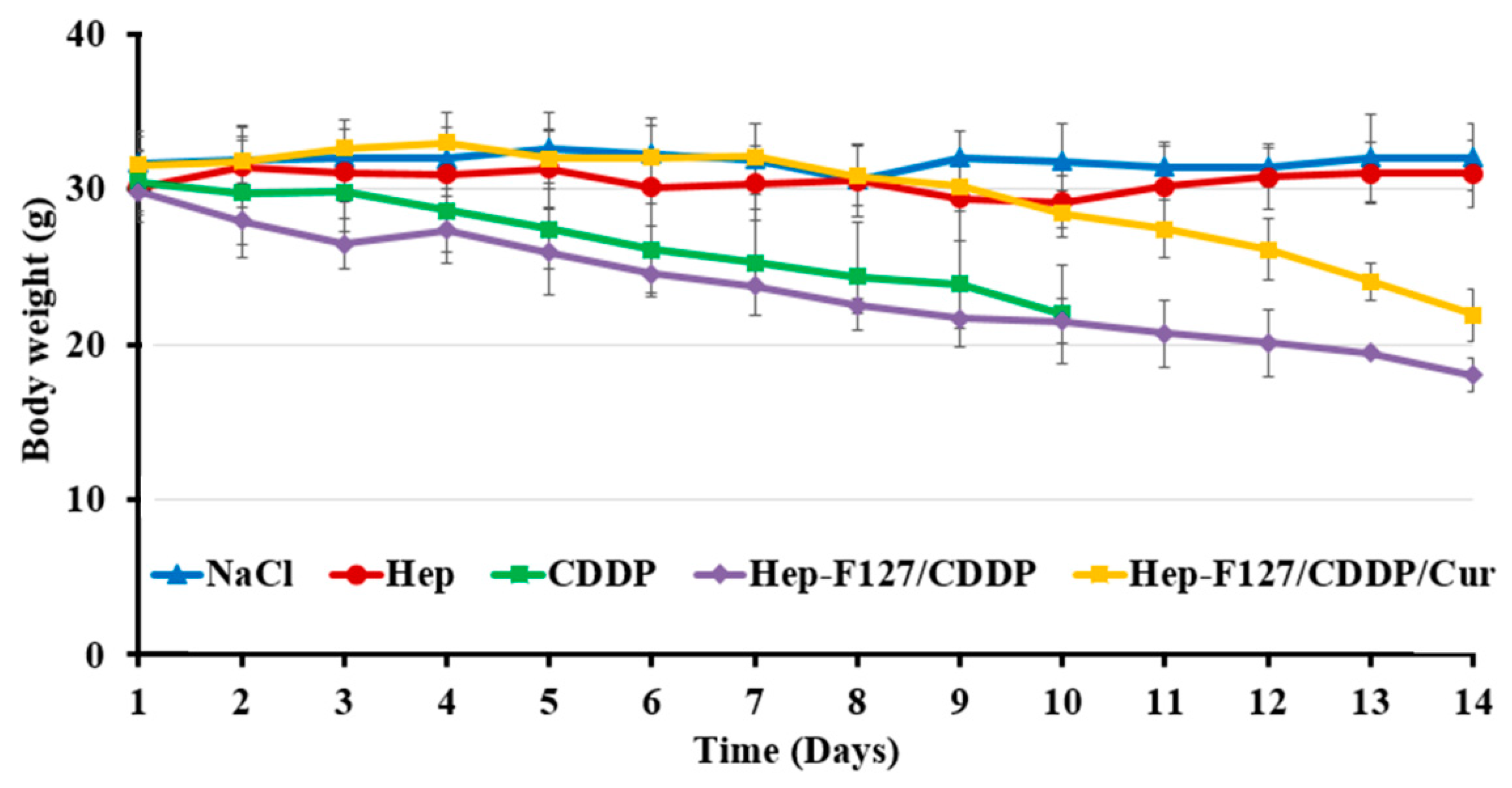
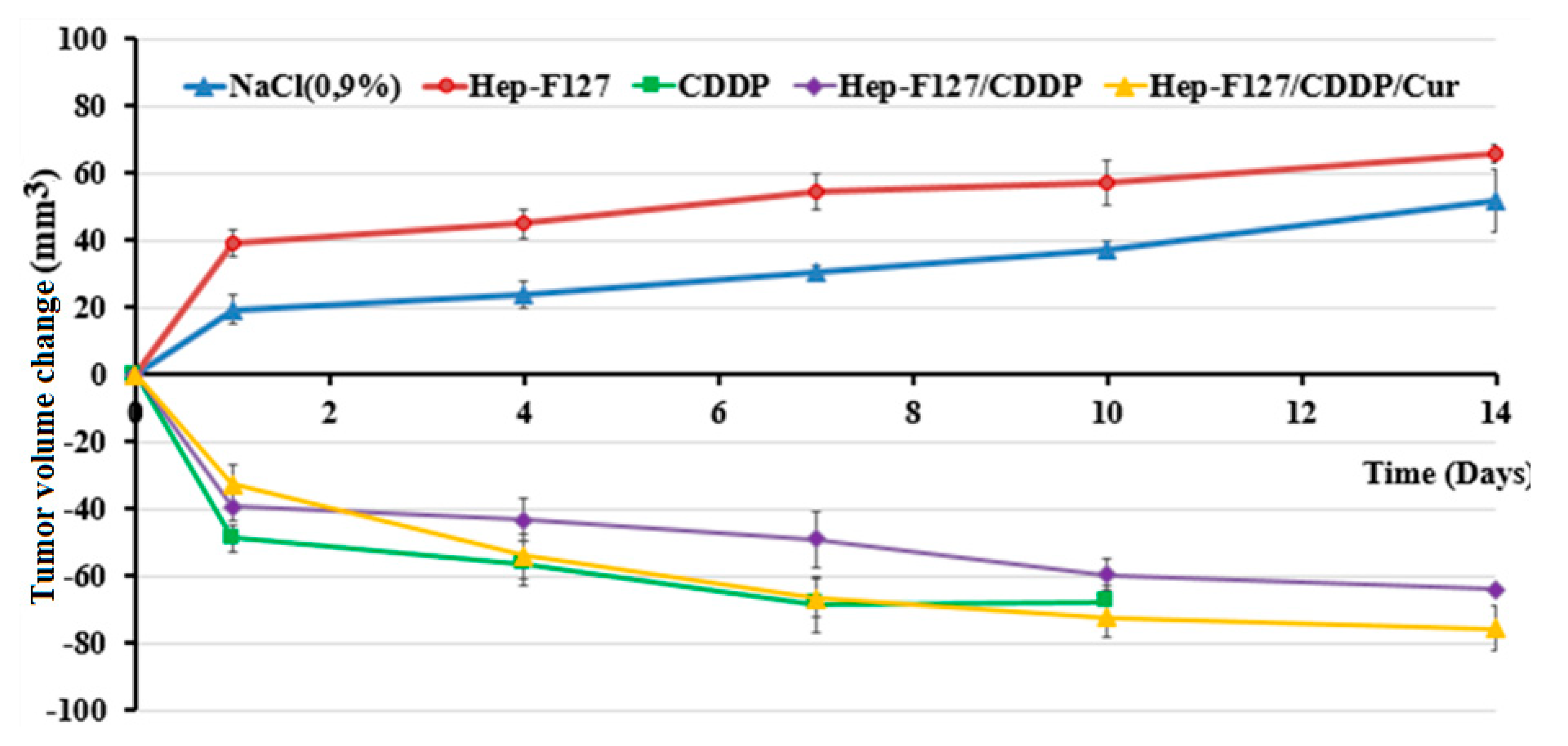
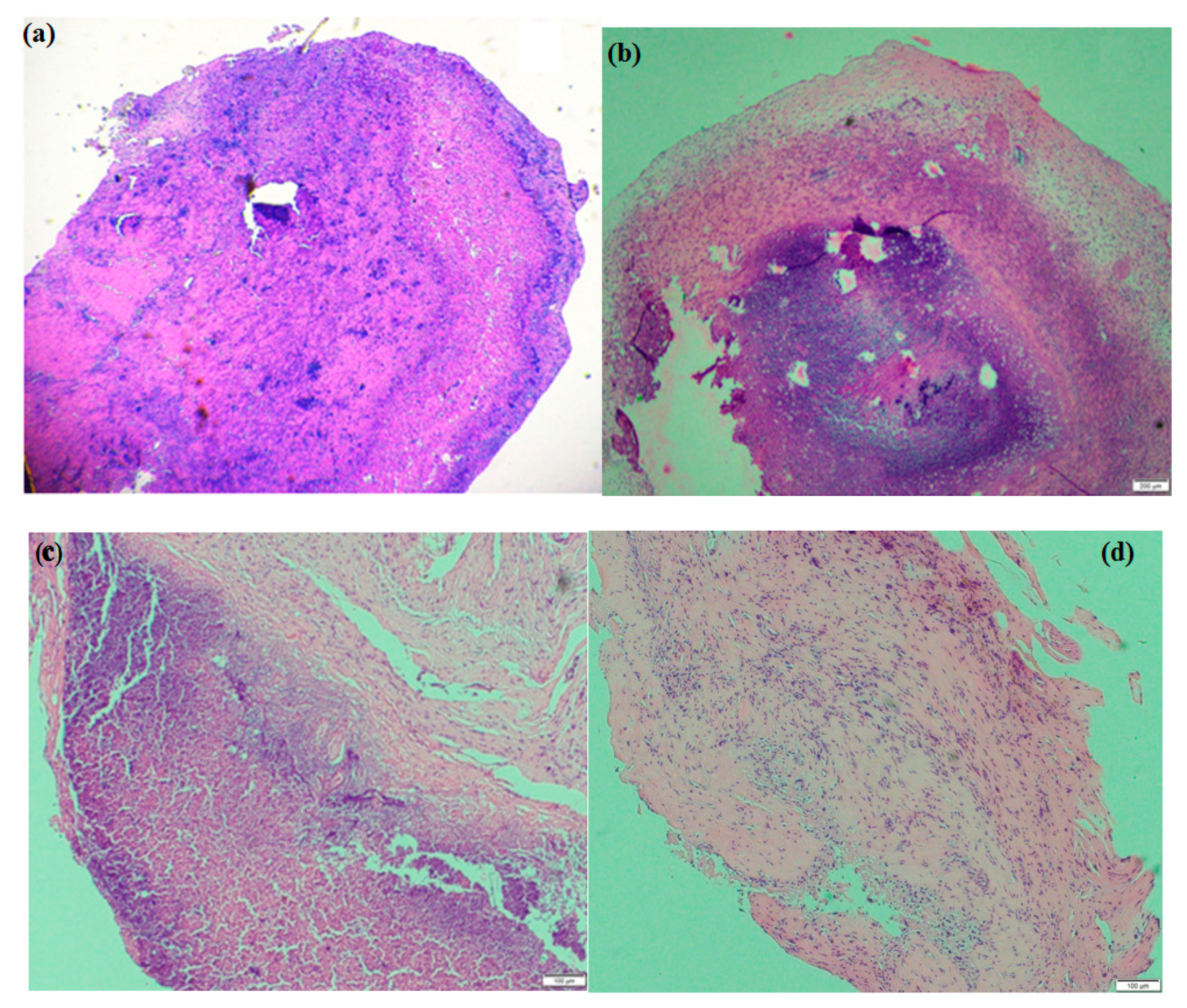
2.5. Tumor Growth Suppression Results in Xenograft Models
3. Materials and Methods
3.1. Materials
3.2. Preparation and Characterizations of Copolymer
3.3. Dual Drug Encapsulation
3.4. In-Vitro Release of Dual Drugs from the Thermo-Responsive Platform
3.5. Evaluation of the Antiproliferative Activity of Dual Drugs Delivery System
3.6. In-Vivo Xenograft Tumor Models for Drug Testing
3.7. Characterizations
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J. Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef] [PubMed]
- Wexselblatt, E.; Gibson, D. Cellular interactions of platinum drugs. Inorganica. Chim. Acta 2012, 393, 75–83. [Google Scholar] [CrossRef]
- Ly, T.U.; Tran, N.Q.; Hoang, T.K.D.; Phan, K.N.; Trương, T.C.N.; Nguyen, C.K. Pegylated dendrimer and its effect in fluorouracil loading and release for enhancing antitumor activity. J. Biomed. Nanotechnol. 2013, 9, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Rexer, B.N.; Arteaga, C.L. Intrinsic and acquired resistance to HER2-targeted therapies in HER2 gene-amplified breast cancer: Mechanisms and clinical implications. Crit. Rev. Oncog. 2012, 17, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.C.; Nguyen, T.H.; Tran, N.Q.; Nguyen, C.K. Highly lipophilic pluronics-conjugated polyamidoamine dendrimer nanocarriers as potential delivery system for hydrophobic drugs. Mater. Sci. Eng. C: Mater. Biol. Appl. 2017, 70, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Moss, D.M.; Siccardi, M. Optimizing nanomedicine pharmacokinetics using physiologically based pharmacokineticmodeling. Br. J. Pharmacol. 2014, 171, 3963–3979. [Google Scholar] [CrossRef] [PubMed]
- Tran, N.Q.; Joung, Y.K.; Lih, E.; Park, K.M.; Park, K.D. RGD-Conjugated in situ forming hydrogels as cell-adhesive injectable scaffolds. Macromol. Res. 2011, 19, 300–306. [Google Scholar] [CrossRef]
- Le, P.N.; Huynh, C.K.; Tran, N.Q. Advances in thermosensitive polymer-grafted platforms for biomedical applications. Mater. Sci. Eng.: C 2018, 92, 1016–1030. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.H.; Tran, N.Q.; Nguyen, C.K. Tetronic-grafted chitosan hydrogel as an injectable and biocompatible scaffold for biomedical applications. Sci. Polym. Ed. 2013, 24, 1636–1648. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Nan, A. Combination drug delivery approaches in metastatic breast cancer. J. Drug Delivery 2012, 2012, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Tong, N.A.N.; Tran, N.Q.; Nguyen, X.D.T.; Cao, V.D.; Nguyen, T.P.; Nguyen, C.K. Thermosensitive heparin-Pluronic® copolymer as effective dual anticancer drugs delivery system for combination cancer therapy. Int. J. Nanotechnol. 2018, 15, 174–187. [Google Scholar] [CrossRef]
- Wu, H.; Jin, H.; Wang, C.; Zhang, Z.; Ruan, H.; Sun, L.; Yang, C.; Li, Y.; Qin, W.; Wang, C. Synergistic cisplatin/doxorubicin combination chemotherapy for multidrug-resistant cancer via polymeric nanogels targeting delivery. ACS Appl. Mater. Interfaces 2017, 9, 9426–9436. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.T.; Tran, T.V.; Tran, N.Q.; Nguyen, C.K.; Nguyen, D.H. Hierarchical self-assembly of heparin-PEG end-capped porous silica as a redox-sensitive nanocarrier for doxorubicin delivery. Mater. Sci. Eng. C: Mater. Biol. Appl. 2017, 70, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Amin, A.; Gali-Muhtasib, H.; Ocker, M.; Schneider-Stock, R. Overview of major classes of plant-derived anticancer drugs. Int. J. Biomed. Sci 2009, 5, 1–11. [Google Scholar] [PubMed]
- Weaver, B.A. How Taxol/paclitaxel kills cancer cells. Mol. Biol. Cell 2014, 25, 2677–2681. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, S.; Somasagara, R.R.; Hegde, M.; Nishana, M.; Tadi, S.K.; Srivastava, M.; Choudhary, B.; Raghavan, S.C. Quercetin,; A natural flavonoid interacts with dna, arrests cell cycle and causes tumor regression by activating mitochondrial pathway of apoptosis. Sci. Rep. 2016, 6, 24049. [Google Scholar] [CrossRef] [PubMed]
- Das, M.; Sahoo, S.K. Folate decorated dual drug loaded nanoparticle: Role of curcumin in enhancing therapeutic potential of nutlin-3a by reversing multidrug resistance. PLoS ONE 2012, 7, e32920. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Jain, R.; Das, M.; Agrawal, A.K.; Thankia, K.; Kushwaha, V. Combinatorial bio-conjugation of gemcitabine and curcumin enables dual drug delivery with synergistic anticancer efficacy and reduced toxicity. RSC Adv. 2014, 4, 29193–29201. [Google Scholar] [CrossRef]
- Baek, J.S.; Cho, C.W. A multifunctional lipid nanoparticle for co-delivery of paclitaxel and curcumin for targeted delivery and enhanced cytotoxicity in multidrug resistant breast cancer cells. Oncotarget 2017, 8, 30369–30382. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.B.T.; Nguyen, T.T.C.; Tran, H.C.; Nguyen, C.K.; Tran, N.Q. 1H NMR spectroscopy as an effective method for predicting molecular weight of polyaminoamine dendrimers and their derivatives. Int. J. Polym. Anal. Charact. 2015, 20, 57–68. [Google Scholar] [CrossRef]
- Jiang, H.; Geng, D.; Liu, H.; Li, Z.; Cao, J. Co-delivery of etoposide and curcumin by lipid nanoparticulate drug delivery system for the treatment of gastric tumors. Drug Deliv. 2016, 23, 3665–3673. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Si, X.; Han, M.K.; Viennois, E.; Zhang, M.; Merlin, D. Co-delivery of camptothecin and curcumin by cationic polymeric nanoparticles for synergistic colon cancer combination chemotherapy. J. Mater. Chem. B, Mater. Biol. Med. 2015, 3, 7724–7733. [Google Scholar] [CrossRef]
- Tong, N.N.A.; Nguyen, T.P.; Nguyen, C.K.; Tran, N.Q. Aquated cisplatin and heparin-pluronicnano-complexes exhibiting sustainable release of active platinum compound and NCI-H460 lung cancer cell antiproliferation. J. Biomater. Sci. Polym. Ed. 2016, 27, 709–720. [Google Scholar] [CrossRef] [PubMed]
- Kozlov, M.Y.; Melik-Nubarov, N.S.; Batrakova, E.V.; Kabanov, A.V. Relationship between pluronic block copolymer structure, critical micellization concentration and partitioning coefficients of low molecular mass solutes. Macromolecules, 2000, 33, 3305–3313. [Google Scholar] [CrossRef]
- Nguyen, T.B.T.; Dang, L.H.; Nguyen, T.T.T.; Tran, D.L.; Nguyen, D.H.; Nguyen, V.T.; Nguyen, C.K.; Nguyen, T.H.; Le, V.T.; Tran, N.Q. Green processing of thermosensitive nanocurcumin-encapsulated chitosan hydrogel towards biomedical application. Green Process and synth. 2016, 5, 511–520. [Google Scholar] [CrossRef]
- Dang, L.H.; Nguyen, T.H.; Tran, L.B.H.; Doan, N.V.; Tran, N.Q. Injectable nanocurcumin–formulated chitosan-g-pluronic hydrogel exhibiting a great potential for burn treatment. J. Health. Eng. 2018. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, G.J.; Plumb, J.A.; Sutcliffe, O.B.; Flint, D.J.; Wheate, N.J. Evaluation of anionic half generation 3.5–6.5poly(amidoamine) dendrimers as delivery vehicles for the active component of the anticancer drug cisplatin. J. Inorg. Biochem. 2011, 105, 1115–1122. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.; Nguyen, C.K.; Nguyen, N.H.; Tran, N.Q. Improved method for cisplatin-loading dendrimer and behavior of the complex nanoparticles in vitro release and cytotoxicity. J. Nanosci. Nanotechnol. 2015, 16, 4106–4110. [Google Scholar] [CrossRef]
- Tomayko, M.M.; Reynolds, C.P. Determination of subcutaneous tumor size in athymic (nude) mice. Cancer Chemother. Pharmacol. 1989, 24, 148–514. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.H.; Jacobson, K.A.; Rose, J.; Zeller, R. Hematoxylin and eosin staining of tissue and cell sections. Cold Spring Harbor Protoc. 2008, 3, 4986. [Google Scholar] [CrossRef] [PubMed]
Sample Availability: Samples of the compounds Hep-F127, Hep-F127/CDDP/Cur are available from the authors N.T.N and N.Q.T. |

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, N.T.; Nguyen, N.N.T.; Tran, N.T.N.; Le, P.N.; Nguyen, T.B.T.; Nguyen, N.H.; Bach, L.G.; Doan, V.N.; Tran, H.L.B.; Le, V.T.; et al. Synergic Activity Against MCF-7 Breast Cancer Cell Growth of Nanocurcumin-Encapsulated and Cisplatin-Complexed Nanogels. Molecules 2018, 23, 3347. https://doi.org/10.3390/molecules23123347
Nguyen NT, Nguyen NNT, Tran NTN, Le PN, Nguyen TBT, Nguyen NH, Bach LG, Doan VN, Tran HLB, Le VT, et al. Synergic Activity Against MCF-7 Breast Cancer Cell Growth of Nanocurcumin-Encapsulated and Cisplatin-Complexed Nanogels. Molecules. 2018; 23(12):3347. https://doi.org/10.3390/molecules23123347
Chicago/Turabian StyleNguyen, Ngoc The, Ngoc Nhat Thanh Nguyen, Ngo The Nhan Tran, Phung Ngan Le, Thi Bich Tram Nguyen, Ngoc Hoa Nguyen, Long Giang Bach, Vu Nguyen Doan, Ha Le Bao Tran, Van Thu Le, and et al. 2018. "Synergic Activity Against MCF-7 Breast Cancer Cell Growth of Nanocurcumin-Encapsulated and Cisplatin-Complexed Nanogels" Molecules 23, no. 12: 3347. https://doi.org/10.3390/molecules23123347
APA StyleNguyen, N. T., Nguyen, N. N. T., Tran, N. T. N., Le, P. N., Nguyen, T. B. T., Nguyen, N. H., Bach, L. G., Doan, V. N., Tran, H. L. B., Le, V. T., & Tran, N. Q. (2018). Synergic Activity Against MCF-7 Breast Cancer Cell Growth of Nanocurcumin-Encapsulated and Cisplatin-Complexed Nanogels. Molecules, 23(12), 3347. https://doi.org/10.3390/molecules23123347




