Podophyllotoxin-Loaded Nanostructured Lipid Carriers for Skin Targeting: In Vitro and In Vivo Studies
Abstract
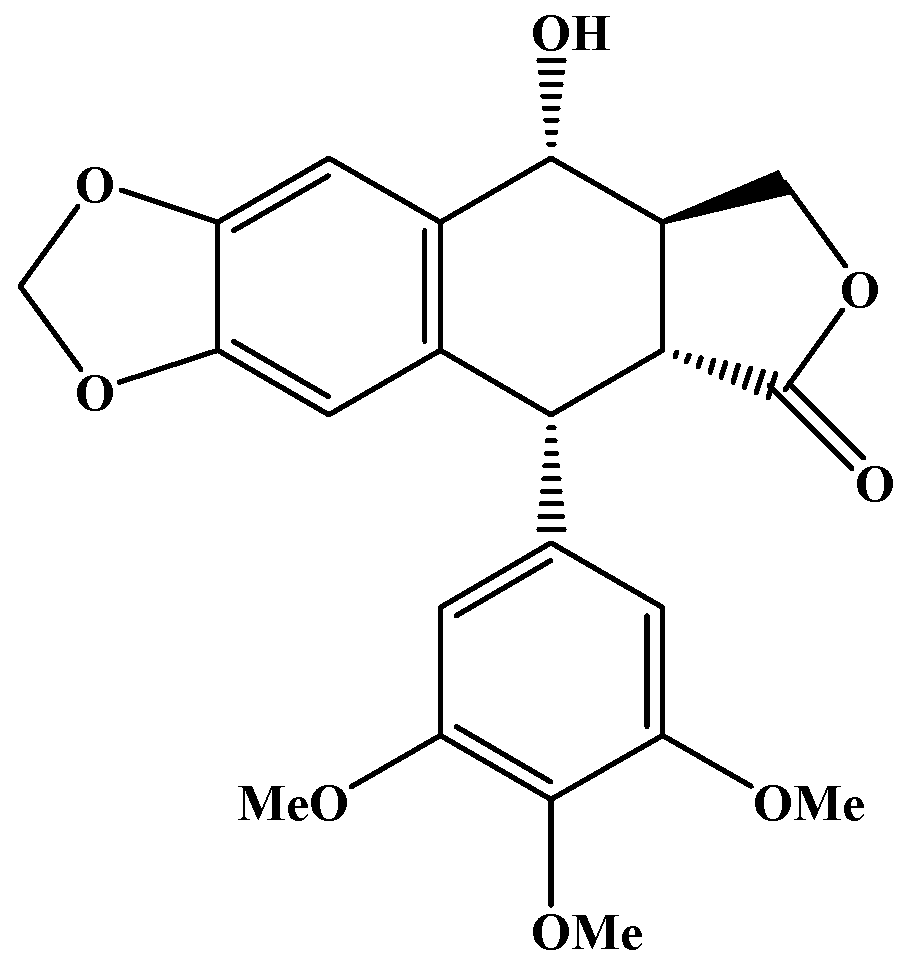
:1. Introduction
2. Results and Discussion
2.1. Mean Particle Size, Polydispersity Index, and Zeta Potential
2.2. POD Loading and Entrapment Efficiency
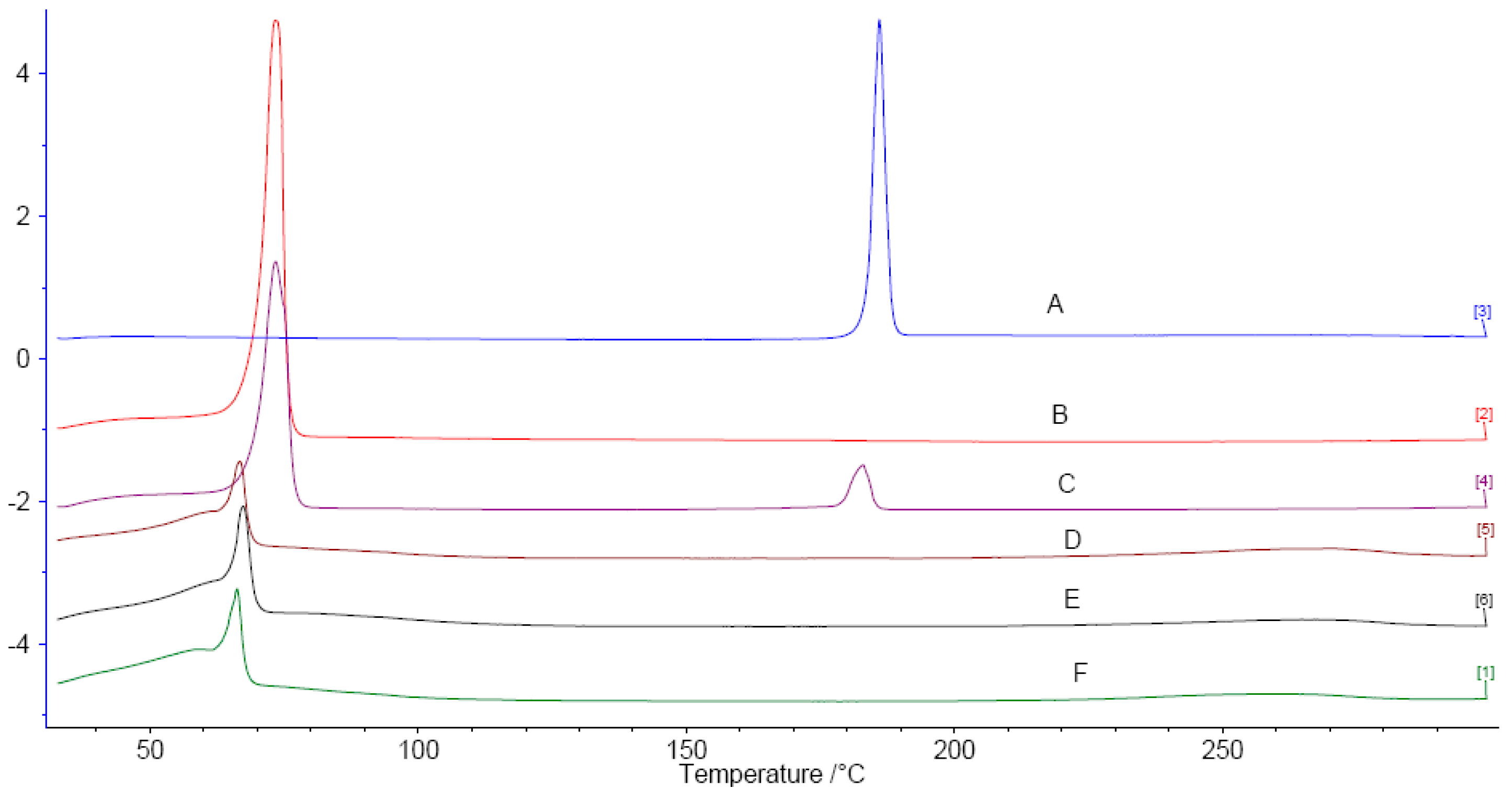
2.3. Differential Scanning Calorimetry (DSC)
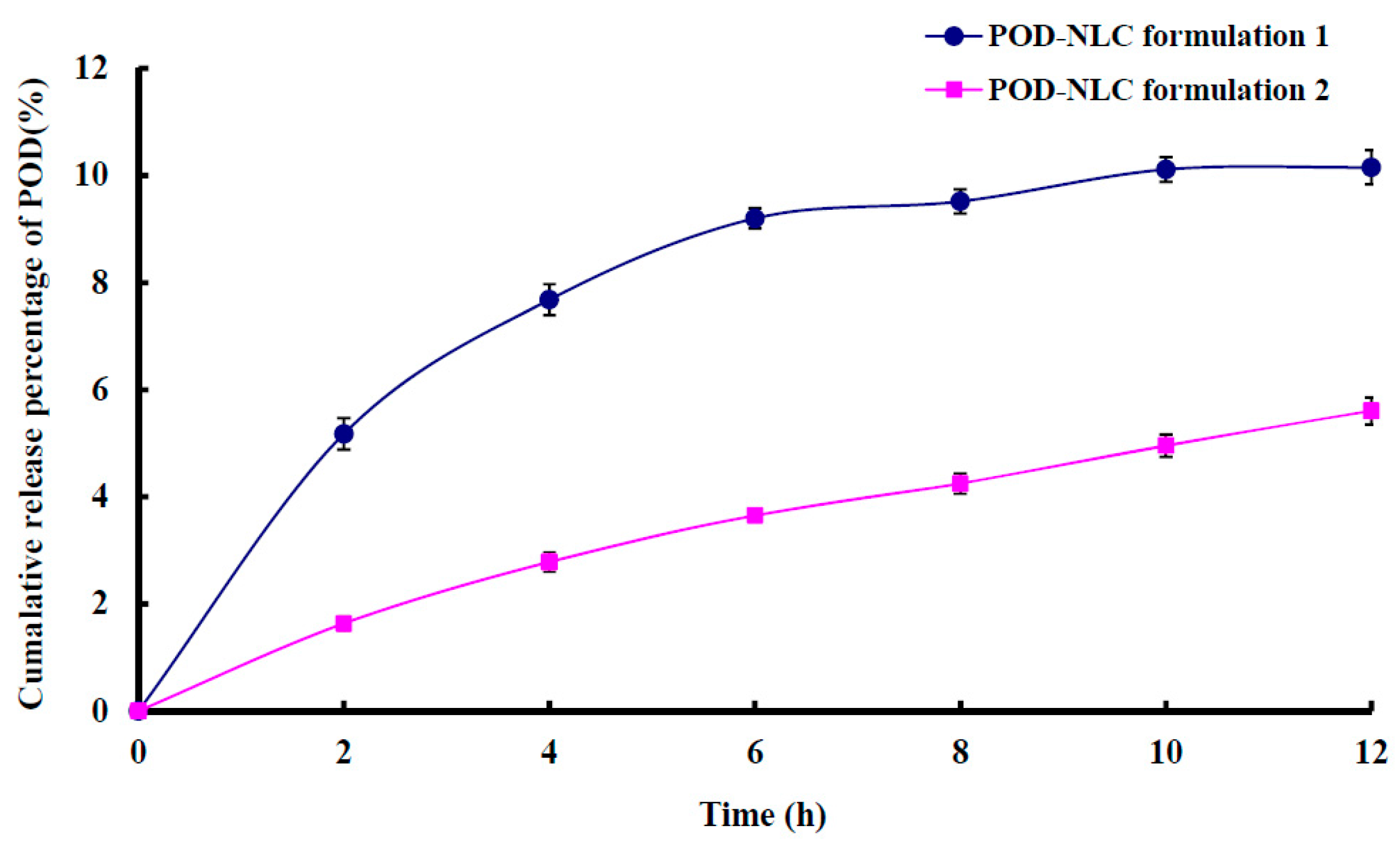
2.4. In Vitro Release
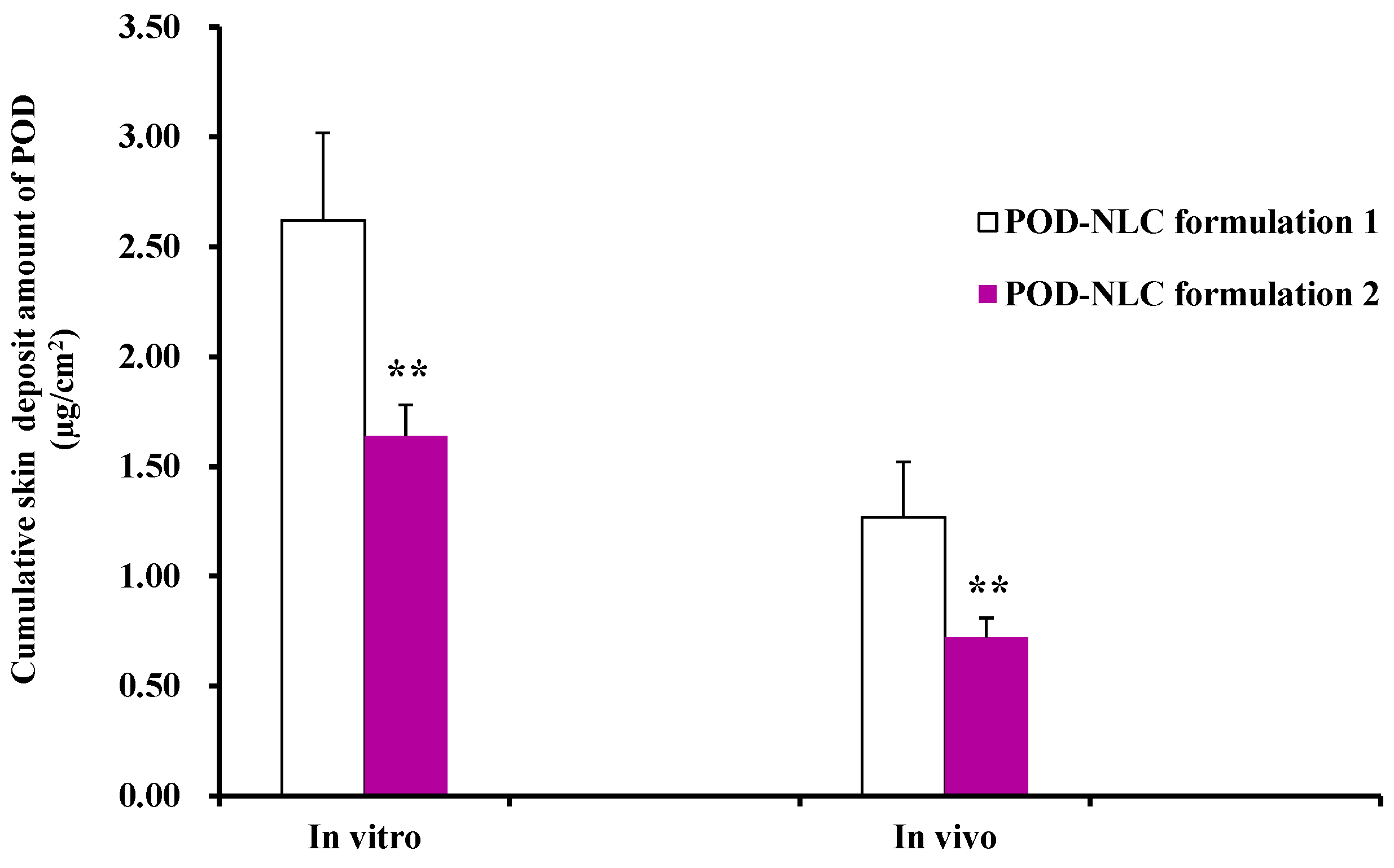
2.5. In Vitro and In Vivo Skin Retention
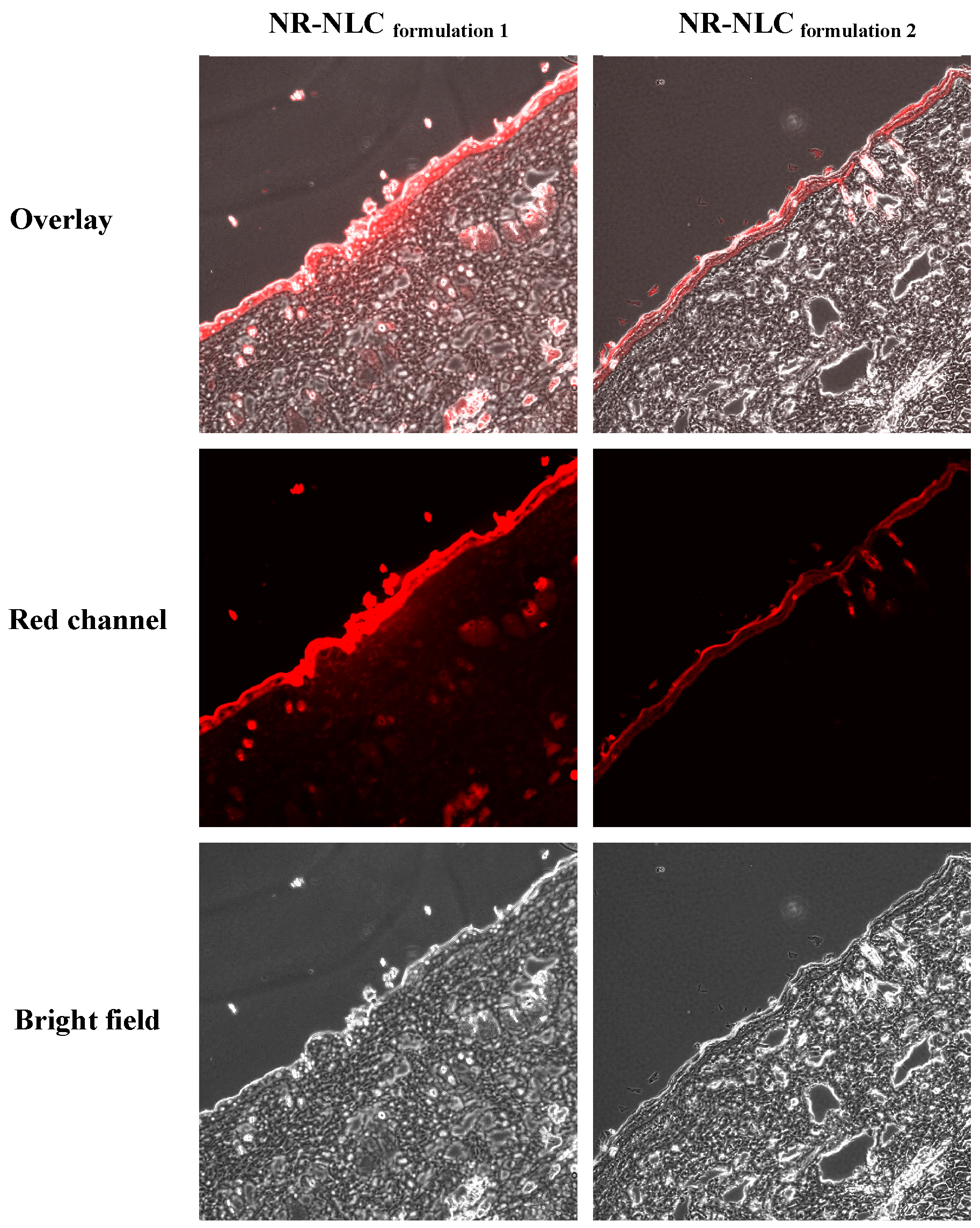
2.6. Confocal Laser Scanning Microscopy (CLSM)
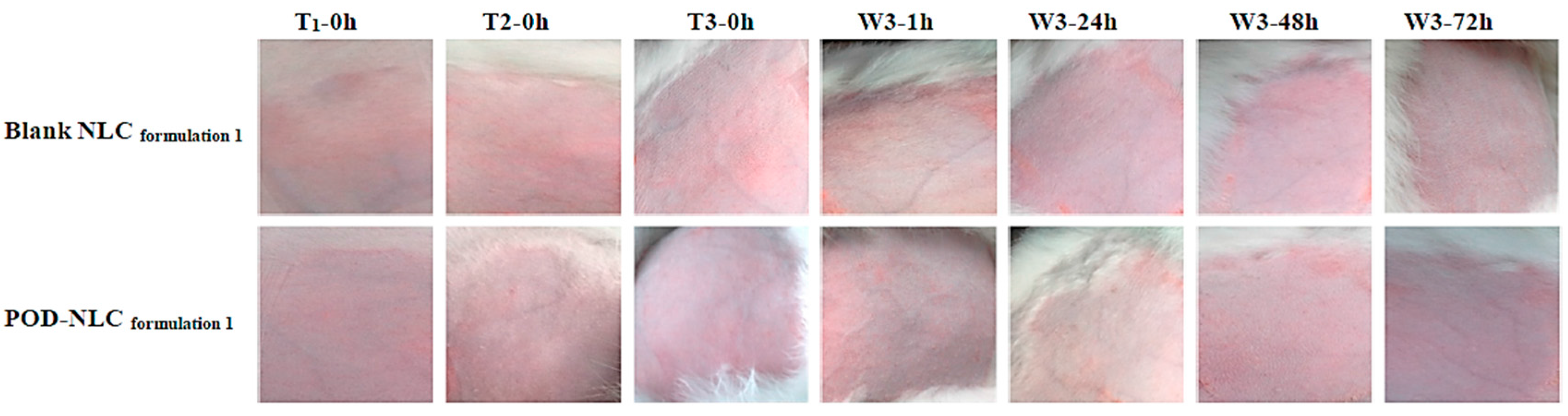
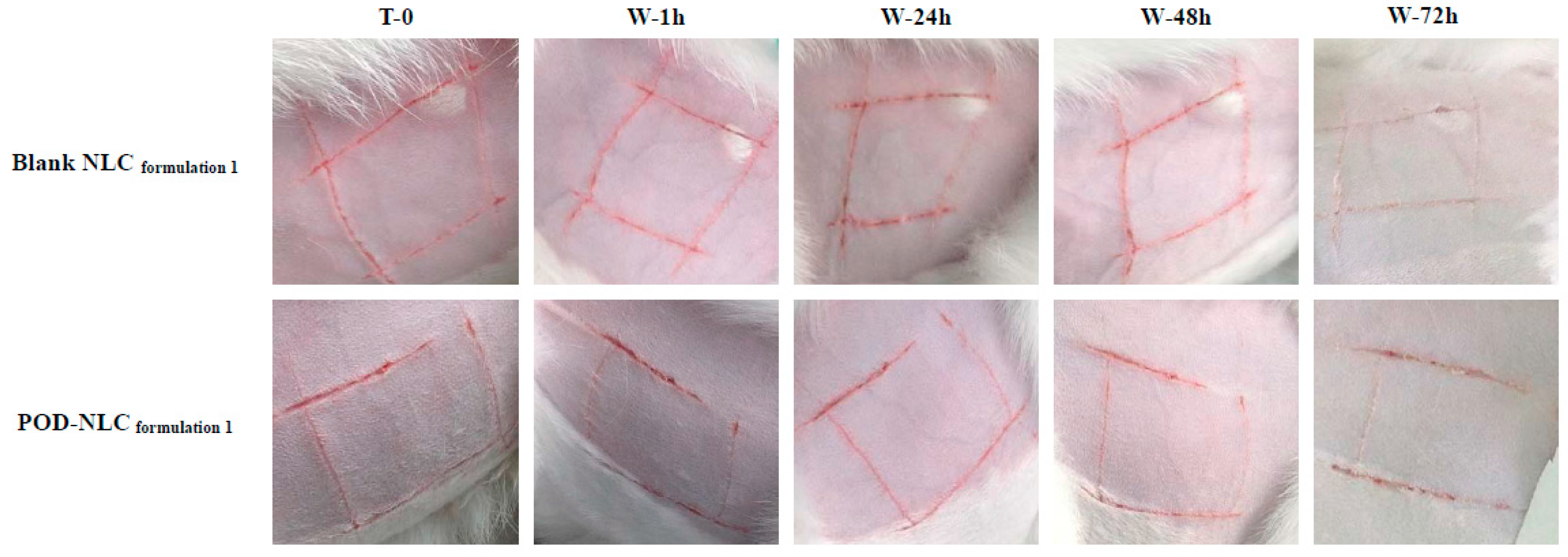
2.7. Skin Irritation Evaluation
3. Materials and Methods
3.1. Reagents
3.2. Preparation of Podophyllotoxin-Loaded Nanostructured Lipid Carriers
3.3. Mean Particle Size, Polydispersity Index, and Zeta Potential
3.4. POD Loading and Entrapment Efficiency
3.5. Differential Scanning Calorimetry (DSC)
3.6. In Vitro Release
3.7. In Vitro Skin Retention
3.8. In Vivo Skin Retention
3.9. Confocal Laser Scanning Microscopy (CLSM)
3.10. Skin Irritation Evaluation
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Mezei, M.; Gulasekharam, V. Liposomes—A selective drug delivery system for the topical route of administration. Lotion dosage form. Life Sci. 1980, 26, 1473–1477. [Google Scholar] [CrossRef]
- Vermorken, A.J.; Hukkelhoven, M.W.; Vermeesch-Markslag, A.M.; Goos, C.M.; Wirtz, P.; Ziegenmeyer, J. The use of liposomes in the topical application of steroids. J. Pharm. Pharmacol. 1984, 36, 334–336. [Google Scholar] [CrossRef] [PubMed]
- Mills, O.H., Jr.; Kligman, A.M. Treatment of acne vulgaris with topically applied erythromycin and tretinoin. Acta. Derm. Venereol. 1978, 58, 555–557. [Google Scholar] [PubMed]
- Bangham, A.D.; Standish, M.M.; Watkins, J.C. Diffusion of univalent ions across the lamellae of swollen phospholipids. J. Mol. Biol. 1965, 13, 238–252. [Google Scholar] [CrossRef]
- Schäfer-Korting, M.; Mehnert, W.; Korting, H.C. Lipid nanoparticles for improved topical application of drugs for skin diseases. Adv. Drug Deliv. Rev. 2007, 59, 427–443. [Google Scholar] [CrossRef] [PubMed]
- Pierre, M.B.; Dos Santos Miranda Costa, I. Liposomal systems as drug delivery vehicles for dermal and transdermal applications. Arch. Dermatol. Res. 2011, 303, 607–621. [Google Scholar] [CrossRef] [PubMed]
- Moghimi, S.M.; Korting, H.C. Therapeutic progress with topical liposome for skin disease. Adv. Drug Deliv. Rev. 1996, 18, 335–342. [Google Scholar]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv. Drug Deliv. Rev. 2002, 54 (Suppl. 1), S131–S155. [Google Scholar] [CrossRef]
- Mehnert, W.; Mäder, K. Solid lipid nanoparticles: Production, characterization and applications. Adv. Drug Deliv. Rev. 2001, 47, 165–196. [Google Scholar] [CrossRef]
- Liu, J.; Hu, W.; Chen, H.; Ni, Q.; Xu, H.; Yang, X. Isotretinoin-loaded solid lipid nanoparticles with skin targeting for topical delivery. Int. J. Pharm. 2007, 328, 191–195. [Google Scholar]
- Jeon, H.S.; Seo, J.E.; Kim, M.S.; Kang, M.H.; Oh, D.H.; Jeon, S.O.; Jeong, S.H.; Choi, Y.W.; Lee, S. A retinyl palmitate-loaded solid lipid nanoparticle system: Effect of surface modification with dicetyl phosphate on skin permeation in vitro and anti-wrinkle effect in vivo. Int. J. Pharm. 2013, 452, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Santos Maia, C.; Mehnert, W.; Schaller, M.; Korting, H.C.; Gysler, A.; Haberland, A.; Schäfer-Korting, M. Drug targeting by solid lipid nanoparticles for dermal use. J. Drug Target. 2002, 10, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Pople, P.V.; Singh, K.K. Targeting tacrolimus to deeper layers of skin with improved safety for treatment of atopic dermatitis—Part II: In vivo assessment of dermatopharmacokinetics, biodistribution and efficacy. Int. J. Pharm. 2012, 434, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Lv, Q.; Yu, A.; Xi, Y.; Li, H.; Song, Z.; Cui, J.; Cao, F.; Zhai, G. Development and evaluation of penciclovir-loaded solid lipid nanoparticles for topical delivery. Int. J. Pharm. 2009, 372, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Souto, E.B.; Wissing, S.A.; Barbosa, C.M.; Müller, R.H. Development of a controlled release formulation based on SLN and NLC for topical clotrimazole delivery. Int. J. Pharm. 2004, 278, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Mitri, K.; Shegokar, R.; Gohla, S.; Anselmi, C.; Müller, R.H. Lipid nanocarriers for dermal delivery of lutein: Preparation, characterization, stability and performance. Int. J. Pharm. 2011, 414, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Tiyaboonchai, W.; Tungpradit, W.; Plianbangchang, P. Formulation and characterization of curcuminoids loaded solid lipid nanoparticles. Int. J. Pharm. 2007, 337, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Bose, S.; Du, Y.; Takhistov, P.; Michniak-Kohn, B. Formulation optimization and topical delivery of quercetin from solid lipid based nanosystems. Int. J. Pharm. 2013, 441, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, L.; Sinico, C.; Castangia, I.; Carbone, C.; Puglisi, G. Idebenone-loaded solid lipid nanoparticles for drug delivery to the skin: In vitro evaluation. Int. J. Pharm. 2012, 434, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Dupin, N. Genital warts. Clin. Dermatol. 2004, 22, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-B.; Liu, Y.-H.; Li, S.-T. A clinical study on 0.5% podophyllotoxin tincture in treatment of condylomata acuminate. Chin. J. New Drugs 1996, 5, 125–127. [Google Scholar]
- Cassidy, D.E.; Drewry, J.; Fanning, J.P. Podophyllum toxicity: A report of a fatal case and a review of the literature. J. Toxicol. Clin. Toxicol. 1982, 19, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Von Krogh, G. Podophyllotoxin in serum: Absorption subsequent to three-day repeated applications of a 0.5% ethanolic preparation on condylomata acuminata. Sex. Transm. Dis. 1982, 9, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Chang, X.; Du, D.; Liu, W.; Liu, J.; Weng, T.; Yang, Y.; Xu, H.; Yang, X. Podophyllotoxin-loaded solid lipid nanoparticles for epidermal targeting. J. Control. Release 2006, 110, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, W.; Mäder, K. Solid lipid nanoparticles: Production, characterization and applications. Adv. Drug Deliv. Rev. 2012, 64, S83–S101. [Google Scholar] [CrossRef]
- Müller, R.H.; Petersen, R.D.; Hommoss, A.; Pardeike, J. Nanostructured lipid carriers (NLC) in cosmetic dermal products. Adv. Drug Deliv. Rev. 2007, 59, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, Y.; Petkar, K.C.; Sawant, K.K. Development, evaluation and clinical studies of Acitretin loaded nanostructured lipid carriers for topical treatment of psoriasis. Int. J. Pharm. 2010, 401, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Puglia, C.; Blasi, P.; Rizza, L.; Schoubben, A.; Bonina, F.; Rossi, C.; Ricci, M. Lipid nanoparticles for prolonged topical delivery: An in vitro and in vivo investigation. Int. J. Pharm. 2008, 357, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Ricci, M.; Puglia, C.; Bonina, F.; di Giovanni, C.; Giovagnoli, S.; Rossi, C. Evaluation of indomethacin percutaneous absorption from nanostructured lipid carriers (NLC): In vitro and in vivo studies. J. Pharm. Sci. 2005, 94, 1149–1159. [Google Scholar] [CrossRef] [PubMed]
- Han, F.; Yin, R.; Che, X.; Yuan, J.; Cui, Y.; Yin, H.; Li, S. Nanostructured lipid carriers (NLC) based topical gel of flurbiprofen: Design, characterization and in vivo evaluation. Int. J. Pharm. 2012, 439, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Brugè, F.; Damiani, E.; Puglia, C.; Offerta, A.; Armeni, T.; Littarru, G.P.; Tiano, L. Nanostructured lipid carriers loaded with CoQ10: Effect on human dermal fibroblasts under normal and UVA-mediated oxidative conditions. Int. J. Pharm. 2013, 55, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Joshi, M.; Patravale, V. Nanostructured lipid carrier (NLC) based gel of celecoxib. Int. J. Pharm. 2008, 346, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Ng, W.K.; Tan, R.B. Are nanostructured lipid carriers (NLCs) better than solid lipid nanoparticles (SLNs): Development, characterizations and comparative evaluations of clotrimazole-loaded SLNs and NLCs? Eur. J. Pharm. Sci. 2012, 47, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.G.; Jeong, J.H.; Kim, S.R.; Lee, K.M.; Ahn, B.K.; Kang, M.H.; Choi, Y.W. Topical formulation of retinyl retinoate employing nanostructured lipid carriers. J. Pharm. Investig. 2012, 42, 243–250. [Google Scholar] [CrossRef]
- Pople, P.V.; Singh, K.K. Development and evaluation of colloidal modified nanolipid carrier: Application to topical delivery of tacrolimus, Part II—In vivo assessment, drug targeting, efficacy, and safety in treatment for atopic dermatitis. Eur. J. Pharm. Biopharm. 2013, 84, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Pople, P.V.; Singh, K.K. Targeting tacrolimus to deeper layers of skin with improved safety for treatment of atopic dermatitis. Int. J. Pharm. 2010, 398, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Lombardi Borgia, S.; Regehly, M.; Sivaramakrishnan, R.; Mehnert, W.; Korting, H.C.; Danker, K.; Röder, B.; Kramer, K.D.; Schäfer-Korting, M. Lipid nanoparticles for skin penetration enhancement-correlation to drug localization within the particle matrix as determined by fluorescence and parelectric spectroscopy. J. Control. Release 2005, 10, 151–163. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.-Y.; Zhao, J.-H.; Feng, N.-P.; Weng, H.-T.; Zhang, Y.-T.; Shi, X.-Q. Study on the Stability of Podophyllotoxin Solution. J. Nanjing TCM Univ. 2011, 27, 80–82. [Google Scholar]
- Hu, K.; Zhu, L.; Liang, H.; Hu, F.; Feng, J. Improved antitumor efficacy and reduced toxicity of liposomes containing bufadienolides. Arch. Pharm. Res. 2011, 34, 1487–1494. [Google Scholar] [CrossRef] [PubMed]
- Ema, M.; Matsuda, A.; Kobayashi, N.; Naya, M.; Nakanishi, J. Evaluation of dermal and eye irritation and skin sensitization due to carbon nanotubes. Regul. Toxicol. Pharmacol. 2011, 61, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Sample Availability: Samples of the compounds (podophyllotoxin, etc.) are available from the authors.
| Drug and Excipients (g/100 mL) | POD-NLCformulation 1 | POD-NLCformulation 2 |
|---|---|---|
| POD | 0.37 | 0.52 |
| Compritol® 888 ATO | 4.30 | 10.0 |
| Labrasol® | 0.76 | 1.8 |
| Cremophor® RH40 | 5.02 | 11.7 |
| SPC | 2.51 | 5.85 |
| Drug and Excipients (g/100 mL) | NR-NLCformulation 1 | NR-NLCformulation 2 |
|---|---|---|
| Nile red | 0.005 | 0.005 |
| Compritol® 888 ATO | 3.54 | 8.2 |
| Labrasol® | 0.76 | 1.8 |
| Cremophor® RH40 | 5.02 | 11.7 |
| SPC | 2.51 | 5.85 |
© 2016 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, J.; Piao, X.; Shi, X.; Si, A.; Zhang, Y.; Feng, N. Podophyllotoxin-Loaded Nanostructured Lipid Carriers for Skin Targeting: In Vitro and In Vivo Studies. Molecules 2016, 21, 1549. https://doi.org/10.3390/molecules21111549
Zhao J, Piao X, Shi X, Si A, Zhang Y, Feng N. Podophyllotoxin-Loaded Nanostructured Lipid Carriers for Skin Targeting: In Vitro and In Vivo Studies. Molecules. 2016; 21(11):1549. https://doi.org/10.3390/molecules21111549
Chicago/Turabian StyleZhao, Jihui, Xianghua Piao, Xiaoqin Shi, Aiyong Si, Yongtai Zhang, and Nianping Feng. 2016. "Podophyllotoxin-Loaded Nanostructured Lipid Carriers for Skin Targeting: In Vitro and In Vivo Studies" Molecules 21, no. 11: 1549. https://doi.org/10.3390/molecules21111549
APA StyleZhao, J., Piao, X., Shi, X., Si, A., Zhang, Y., & Feng, N. (2016). Podophyllotoxin-Loaded Nanostructured Lipid Carriers for Skin Targeting: In Vitro and In Vivo Studies. Molecules, 21(11), 1549. https://doi.org/10.3390/molecules21111549






