Antimicrobial, Cytotoxicity and Phytochemical Screening of Jordanian Plants Used in Traditional Medicine
Abstract
:1. Introduction
2. Results and Discussion
| Plant scientific name, family,
voucher numbers | Local name | Parts used | Traditional and/or
medicinal use | Mode of use |
|---|---|---|---|---|
| Populus alba L. Salicaceae, MAHAS 2 | Al-Hoor
al-abyad | Flowers | Depurative, tooth decay, skin lesions and herpes. | Decoction, infusion/oral |
| Teucrium polium L. Labiatae, MAHAS 9 | Jeada | Aerial parts | Anti-inflammatory, spasm, flatulence, diabetes, necrosis and kidney stones | Infusion |
| Salvia pinardi L. Labiatae, MAHAS 10 | Miramia | Aerial parts | Sedative, for wound healing and herpes | Infusion |
| Syringa vulgaris L. Oleaceae, MAHAS 11 | Lailac | Aerial parts, seeds | Antihelminthic, anti-febrifuge, dry skin, and in the treatment of malaria | Infusion, topical |
| Phagnalon rupstre L. Asteraceae, MAHAS 12 | Kadha | Aerial parts | Any disease of unknown reason, inflammation, rheumatism,
migraine, depression, scalp infection. | Decoction, infusion/oral |
| Inula viscosa (L.) Ait. Compositae, MAHAS 13 | Taioon | Flowers | Anthelmintic, for lung cancer, muscle relaxant | Decoction |
| Luffa cylindrica L. Araceae, MAHAS 14 | Louf | Aerial parts | Treatment of cancer, post-delivery pain, inflammation, infections | Oral/ infusion |
| Pterocephalus pulverulentus Boiss Dipsacaceae, MAHAS 15 | Abu Moch | Aerial parts | Ulceration | Gargle |
| Mirabilis jalapa L. Nyctaginaceae, MAHAS 16 | Chap-Zarief | Aerial parts, roots, stems | Antiseptic, antiviral, fungicide, antiabortive,
useful in epilepsy and chronic bronchitis | Oral/infusion |
| Narcissus tazetta L. Amaryllidaceae, MAHAS 17 | Narjes | Aerial parts,flowers | Anticancer, antiinflammatory, memorigenic, and sedative | Infusion |
| Verbascum sinaiticum L. Scrophulariaceae MAHAS 18 | Al-Omaya | Flowers,
aerial parts | Neural pain, herpes and bronchitis. | Decoction |
| Rosa damascena Mill. Rosaceae, MAHAS 19 | Ward Demashqi | Receptacles, seeds | Antibacterial, treatment of cardiac diseases, colon cancer | Decoction |
| Ononis sicula Desf. Fabaceae, A O 298 | Shibreq | Aerial parts | Skin cancer, lesions | Topical/wash |
| Ononis hirta L. Fabaceae, A O 297 | Showk Al-Jamal | Aerial parts | Skin cancer, necrosis, herpes, cold sores | Mouth and skin wash |
| Plant | % Inhibition | ||||||
|---|---|---|---|---|---|---|---|
| P.a | E.c | S.t | B.c | MRSA | C.a | A.n | |
| Inula viscosa (f) | 96.12 | 9.88 | 99.12 | 101.57 | 92.43 | 22.13 | 17.46 |
| Rosa damascena (s) | 25.50 | 18.50 | 11.45 | 17.97 | 45.95 | 31.30 | 25.67 |
| Rosa damascena (r) | 80.49 | 60.69 | 100.82 | 101.09 | 95.75 | 98.87 | 30.72 |
| Ononis hirta (a.p) | 45.89 | 12.49 | 93.40 | 81.91 | -72.82 | 40.23 | 17.34 |
| Ononis sicula (a.p) | 60.75 | 21.28 | 79.03 | 74.67 | -60.23 | 25.40 | 19.68 |
| Syringa vulgaris (s) | 43.56 | -1.41 | -33.60 | -20.75 | -12.76 | 12.92 | 14.18 |
| Syringa vulgaris (a.p) | 46.98 | -8.60 | -2.22 | -34.08 | -42.32 | 16.74 | 23.25 |
| Populus alba (f) | 40.12 | 31.38 | 39.11 | 43.00 | 34.65 | 28.27 | 18.25 |
| Teucrium polium (a.p) | 56.54 | 25.84 | 80.08 | 94.27 | 3.53 | 19.33 | 16.45 |
| Salvia pinardi (a.p) | 28.71 | -68.30 | 43.99 | 45.38 | 28.73 | -49.76 | -50.68 |
| Phagnalon rupstre (a.p) | 19.51 | -24.10 | 77.86 | 71.71 | -63.28 | -5.66 | -8.70 |
| Luffa cylindrica (a.p) | 9.09 | -35.07 | 43.93 | 39.20 | 38.38 | 5.34 | 0.87 |
| Verbascum sinaiticum(f) | 58.31 | 18.02 | 99.42 | -56.69 | 70.54 | 35.46 | 29.57 |
| Narcissus tazetta (f) | 46.98 | 21.93 | -32.65 | -36.61 | -30.08 | 12.34 | 1.60 |
| Narcissus tazetta (a.p) | 52.23 | 44.08 | 70.50 | 75.93 | 48.96 | 99.23 | 5.69 |
| Mirabilis jalapa (ro) | 35.48 | 26.93 | -14.02 | -11.46 | 13.17 | 27.97 | 10.11 |
| Mirabilis jalapa (a.p) | 13.75 | 5.32 | -53.86 | -56.70 | -33.92 | 17.90 | 2.54 |
| Mirabilis jalapa (st) | 40.56 | 17.37 | -28.27 | 15.26 | -8.51 | 16.87 | -5.60 |
| Pterocephalus pulverulentus (a.p) | 43.02 | 5.65 | 3.45 | 40.82 | 26.24 | 28.98 | 13.32 |
| Plant Extract | Test Microorganisms | ||||||
|---|---|---|---|---|---|---|---|
| MRSA | E.c | P.a | S.t | B.c | C.a | ||
| R.d (r) | Eth. | > 1000 | > 1000 | > 1000 | > 1000 | 1000 | 250 |
| But. | 500 | > 1000 | 125 | 62.5 | 250 | 1000 | |
| Aqu. | 500 | > 1000 | 250 | 250 | 500 | 125 | |
| Met. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | 1000 | |
| Hex. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | |
| I.v (f) | Eth. | > 1000 | > 1000 | > 1000 | > 1000 | 1000 | ND |
| But. | 250 | > 1000 | 500 | 125 | 250 | ND | |
| Aqu. | > 1000 | > 1000 | 250 | > 1000 | > 1000 | ND | |
| Met. | 500 | > 1000 | 1000 | > 1000 | 1000 | ND | |
| Hex. | 1000 | > 1000 | > 1000 | 1000 | 500 | ND | |
| P.r (ap) | Eth. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND |
| But. | > 1000 | > 1000 | > 1000 | 1000 | > 1000 | ND | |
| Aqu. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| Met. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| Hex. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| O.h (ap) | Eth. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND |
| But. | > 1000 | > 1000 | 500 | > 1000 | > 1000 | ND | |
| Aqu. | > 1000 | > 1000 | 125 | > 1000 | > 1000 | ND | |
| Met. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| Hex. | > 1000 | > 1000 | 125 | > 1000 | > 1000 | ND | |
| T.p (ap) | Eth. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND |
| But. | > 1000 | > 1000 | 250 | > 1000 | > 1000 | ND | |
| Aqu. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| Met. | > 1000 | > 1000 | 1000 | > 1000 | > 1000 | ND | |
| Hex. | > 1000 | > 1000 | 125 | > 1000 | > 1000 | ND | |
| O.s (ap) | Eth. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND |
| But. | > 1000 | > 1000 | 500 | > 1000 | > 1000 | ND | |
| Aqu. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| Met. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| Hex. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| V.s (f) | Eth. | > 1000 | > 1000 | > 1000 | 1000 | 1000 | ND |
| But. | > 1000 | > 1000 | > 1000 | 1000 | 1000 | ND | |
| Aqu. | 1000 | 1000 | > 1000 | 1000 | 1000 | ND | |
| Met. | > 1000 | > 1000 | > 1000 | 1000 | 1000 | ND | |
| Hex. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | ND | |
| N.t (a.p) | Eth. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | 500 |
| But. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | 125 | |
| Aqu. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | 500 | |
| Met. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | |
| Hex. | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | > 1000 | |
| Tetracycline | ND | 8 | 8 | 4 | ND | ND | |
| Penicillin G | 10 | ND | ND | ND | 8 | ND | |
| Nystatin | ND | ND | ND | ND | ND | 8 | |
| Plant | IC50 (μg/mL) ± S.D |
|---|---|
| Inula viscosa (flowers) | 202.43 ± 3.70 |
| Rosa damascena (receptacles) | 454.11± 2.87 |
| Ononis hirta (aerial parts) | 72.50 ± 1.34 |
| Ononis sicula (aerial parts) | 325.17 ± 3.00 |
| Phagnalon rupstre (aerial parts) | 197.23 ± 4.2 |
| Narcissus tazetta (aerial parts) | 131.01 ± 5.20 |
| Verbascum sinaiticum(flower) | 367.11 ± 2.70 |
| Teucrium polium (aerial parts) | 110.03 ± 1.50 |
| Plant | alkaloids | flavonoids | terpenoids |
|---|---|---|---|
| Ononis hirta (aerial parts) | + | + | + |
| Verbascum sinaiticum (flowers) | - | + | + |
| Inula viscosa (flowers) | - | + | + |
| Ononis sicula (aerial parts) | - | + | + |
| Narcissus tazetta (aerial parts) | + | + | + |
| Rosa damascena (receptacles) | - | + | + |
| Phagnalon rupustre (aerial parts) | - | + | + |
| Teucrium polium (aerial parts) | - | + | + |
3. Conclusions
4. Experimental
4.1. Plant material
4.2. Plant extraction and fractionation
4.3. Microbial strains
4.4. Antibacterial assay.
4.5. Antifungal assay
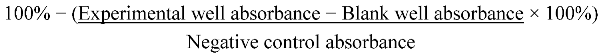
4.6. Cytotoxicity study
4.7. Phytochemical screening
Acknowledgments
- Sample Availability: Samples of the different plant extracts are available from the authors.
References
- Cowan, M.M. Plant products as antimicrobial agents. Clin. Microbiol. Rev. 1999, 12, 564–582. [Google Scholar]
- Pareke, J.; Chanda, S. In vitro screening of antibacterial activity of aqueous and alcoholic extracts of various Indian plant species against selected pathogens from Enterobacteriaceae. AJMR 2007, 1, 92–99. [Google Scholar]
- Alanis, A.L. Resistance to antibiotics: are we in the post-antibiotic era? Arch. Med. Res. 2005, 36, 697–705. [Google Scholar] [CrossRef]
- Ficker, C.E.; Arnason, J.T.; Vindas, P.S.; Alvarez, L.P.; Akpagana, K.; Gbeassor, M. Inhibition of human pathogenic fungi by ethnobotanically selescted plant extracts. Mycoses 2005, 46, 29–37. [Google Scholar]
- Ahmed, I.; Mehmood, Z.; Mohammad, F. Screening of some Indian medicinal plants for their antimicrobial properties. J. Ethnopharmacol. 1998, 62, 183–193. [Google Scholar] [CrossRef]
- Ghosh, A.; Das, B.K.; Roy, A.; Mandal, B.; Chandra, G. Antibacterial activity of some medicinal plant extracts. J. Nat. Med. 2008, 62, 259–262. [Google Scholar] [CrossRef]
- Eloff, J.N. Which extractant should be used for the screening and isolation of antimicrobial components from plants? J. Ethnopharmacol. 1998, 60, 1–8. [Google Scholar] [CrossRef]
- Quiroga, E.N.; Sampietro, A.R.; Vattuone, M.A. Screening antifungal activities of selected medicinal plants. J. Ethnopharmacol. 2001, 74, 89–96. [Google Scholar] [CrossRef]
- Al-Eisawi, D. List of Jordan vascular plants. Mitteilungen Botanik Munchen. 1982, 18, 79–182. [Google Scholar]
- Aburjai, T.; Hudaib, M.; Tayyem, R.; Yousef, M.; Qishawi, M. Ethnopharmacological survey of medicinal herbs in Jordan, the Ajloun heights region. J. Ethnopharmacol. 2007, 110, 294–304. [Google Scholar] [CrossRef]
- Mahasneh, A.; El-Oqlah, A. Antimicrobial activity of extracts of herbal plants used in the traditional medicine in Jordan. J. Ethnopharmacol. 1999, 64, 271–276. [Google Scholar] [CrossRef]
- AL-Hussaini, R.; Mahasneh, A.M. Microbial growth and quorum sensing antagonist activities of herbal plant extracts. Molecules 2009, 14, 3425–3435. [Google Scholar] [CrossRef]
- Al-Qura’n, S. Ethnopharmacological survey of wild medicinal plants in Showbak, Jordan. J. Ethnopharmacol. 2009, 123, 45–50. [Google Scholar] [CrossRef]
- Hudaib, M.; Mohammad, M.; Bustanji, Y.; Tayyem, R.; Yousef, M.; Abuirjeie, M.; Aburjai, T. Ethnopharmacological survey of medicinal plants in Jordan, Mujib nature reserve and surrounding area. J. Ethnopharmacol. 2008, 120, 63–71. [Google Scholar] [CrossRef]
- Al-Fatimi, M.; Wurster, M.; Shröder, G.; Lindequist, U. Antioxidant, antimicrobial, and cytotoxic activities of selected medicinal plants from Yeme. J. Ethnopharmacol. 2007, 111, 657–666. [Google Scholar] [CrossRef]
- Rojas, J.J.; Ochoa, V.J.; Ocampo, S.A.; Munoz, J.F. Screening for antimicrobial activity of ten medicinal plants used in Colombian folkloric medicine. A possible alternative in the treatment of non-nosocomial infections. BMC Complement. Altern. Med. 2006, 6, 2–10. [Google Scholar]
- Buwa, L.V.; Staden, J.V. Antibacterial and antifungal activity of traditionalmedicinal plants used against venereal diseases in South Africa. J. Ethnopharmacol. 2006, 103, 139–142. [Google Scholar] [CrossRef]
- Aliero, A.A.; Afolayan, A.J. Antimicrobial activity of Solanum tomentosum. Afr. J. Biotechnol. 2006, 5, 369–372. [Google Scholar]
- Mc Cutchon, A.R.; Ellis, S.M.; Hancock, R.E.W.; Towers, G.H.N. Antibiot screening of medicinal plants of the British Columbian native peoples. J. Ethnopharmacol. 1992, 37, 213–223. [Google Scholar] [CrossRef]
- Srinivasan, D.; Nathan, S.; Suresh, T.; Perumalsamy, L.P. Antimicrobial activity of certain Indian medicinal plants used in folkloric medicine. J. Ethnopharmacol. 2001, 74, 217–220. [Google Scholar] [CrossRef]
- Regasini, L.O.; Cotinguiba, F.; Morandim, A.A.; Kato, M.J.; Scorzoni, L.; Mendes-Gianni, M.J.; Bolzani, V.S.; Furian, M. Antimicrobial activity of Piper arboretum and Piper tuberculatum (Piperaceae) against opportunistic yeasts. Afr. J. Biotechnol. 2009, 8, 2866–2870. [Google Scholar]
- Helmerhorst, E.J.; Reijnders, I.M.; Hof, W.V.T.; Smith, I.S.; Veerman, E.C.J.; Amerongen, A.V.N. Amphotericin B and fluconazole-resistant Candida spp, Aspergillus fumigatus and other newly emerging pathogenic fungi are susceptible to basic antifungal peptides. Antimicrib. Agents Chemother. 1999, 43, 702–704. [Google Scholar]
- Masoko, P.; Mmushi, T.J.; Mogashoa, M.M.; Mokgotho, M.P.; Mampuru, L.J.; Howard, R.L. In vitro evaluation of the antifungal activity of Sclerocarya birrea extracts against pathogenic yeast. Afr. J. Biotechnol. 2008, 7, 3521–3526. [Google Scholar]
- Adegoke, A.A.; Adebayo-Tayo, B.C. Antimicrobial activity and phytochemical analysis of leaf extracts of Lasienthera africanum. Afr. J. Biotechnol. 2009, 6, 77–80. [Google Scholar]
- Aridogan, B.C.; Baydar, H.; Kaya, S.; Demirci, M.; Ozbasar, D.; Mumca, E. Antimicrobial activity and chemical composition of some essential oils. Arch. Pharm. Res. 2002, 25, 360–364. [Google Scholar]
- Tsai, T.; Tsai, T.H.; Wu, W.; Tseng, J.; Tsai, P. In vitro antimicrobial and anti- inflammatory effects of herbs against Proionibacterium acnes. Food Chem. 2010, 119, 964–968. [Google Scholar] [CrossRef]
- Kornienko, A.; Evidente, A. Chemistry, biology, and medicinal potentials of Narciclasine and its congeners. Chem. Rev. 2008, 108, 1982–2014. [Google Scholar] [CrossRef]
- Ncube, N. S.; Afolayan, A.J.; Okoh, A.I. Assessment techniques of antimicrobial properties of natural compounds of plant origin: current methods and future trends. Afr. J. Biotechnol. 2008, 17, 1797–1806. [Google Scholar]
- Alviano, D.S.; Alviano, C.S. Plant extracts: search for new alternatives to treat microbial diseases. Curr. Pharm. Biotechnol. 2009, 10, 106–121. [Google Scholar] [CrossRef]
- Cushnie, T.P.; Lamb, A.J. Antimicrobial activity of flavonoids. Int. J. Antimicro. Ag. 2005, 26, 343–356. [Google Scholar] [CrossRef]
- Rauha, J.; Remes, S.; Heinonen, M; Hopia, A.; Kahkonen, M., Kujala; Pihlaja, K.; Vuorela, H.; Vuorela, P. Antimicrobial effects of Finnish plant extracts containing flavonoids and other phenolic compounds. Int. J. Food Microbiol. 2000, 56, 3–12. [Google Scholar]
- Valsaraj, R.; Pushpangadan, P.; Smitt, U.W.; Adsersen, A.; Christensen, S.B.; Sittie, A.; Nyman, U.; Nielsen, C.; Olsen, C.E. New anti-HIV-1, antimalarial, and antifungal compounds from Terminalia bellerica. J. Nat. Prod. 1997, 60, 739–742. [Google Scholar]
- Wachter, G.A.; Hoffmann, J.J.; Furbacher, T.; Blake, M.E.; Timmmermann, B.N. Antibacterial and antifungal flavanones from Eysenhardtia texana. Phytochemistry 1999, 52, 1469–1471. [Google Scholar] [CrossRef]
- Scorzoni, L.; Benaducci, T.; Almeida, A.M.F.; Silva, D.H.S.; Bolzani, V.S.; Mendes- Giannini, M.J.S. Comparative study of disk diffusion and microdilution methods for evaluation of antifungal activity of natural compounds against medical yeast Candida spp and Cryptococcus spp. J. Basic. Appl. Pharm. Sci. 2007, 28, 25–34. [Google Scholar]
- Balajee, S.A.; Marr, K.A. Conidial viability assay for rapid susceptibility testing of Aspergillus species. J. Clin. Microbiol. 2002, 40, 2741–2745. [Google Scholar] [CrossRef]
- Lau, C.S.; Ho, C.Y.; Kim, C.F.; Leung, K.N.; Fung, K.P.; Tse, T.F.; Chan, H.L.; Chow, M.S. Cytotoxic activities of Coriolus versicolor (Yunzhi) extract on human leukemia and lymphoma cells by induction of apoptosis. Life Sci. 2004, 75, 797–808. [Google Scholar] [CrossRef]
© 2010 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Talib, W.H.; Mahasneh, A.M. Antimicrobial, Cytotoxicity and Phytochemical Screening of Jordanian Plants Used in Traditional Medicine. Molecules 2010, 15, 1811-1824. https://doi.org/10.3390/molecules15031811
Talib WH, Mahasneh AM. Antimicrobial, Cytotoxicity and Phytochemical Screening of Jordanian Plants Used in Traditional Medicine. Molecules. 2010; 15(3):1811-1824. https://doi.org/10.3390/molecules15031811
Chicago/Turabian StyleTalib, Wamidh H., and Adel M. Mahasneh. 2010. "Antimicrobial, Cytotoxicity and Phytochemical Screening of Jordanian Plants Used in Traditional Medicine" Molecules 15, no. 3: 1811-1824. https://doi.org/10.3390/molecules15031811
APA StyleTalib, W. H., & Mahasneh, A. M. (2010). Antimicrobial, Cytotoxicity and Phytochemical Screening of Jordanian Plants Used in Traditional Medicine. Molecules, 15(3), 1811-1824. https://doi.org/10.3390/molecules15031811




