Early or Delayed Onset of Food Intake in Time-Restricted Eating: Associations with Markers of Obesity in a Secondary Analysis of Two Pilot Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Recruiting
2.2. Intervention
2.3. Data Assessment
2.4. Statistical Analysis
3. Results
3.1. Follow-Up Data
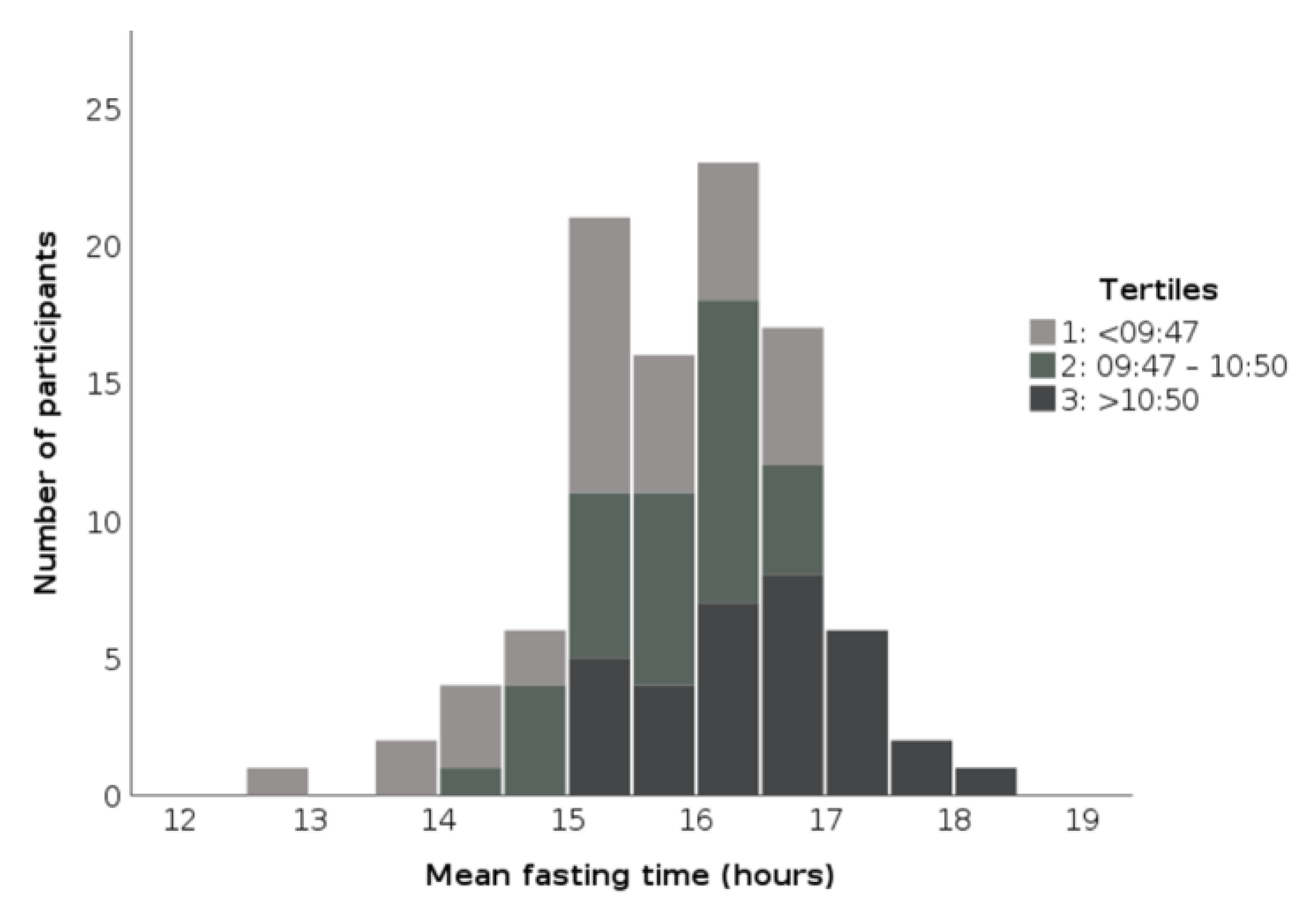
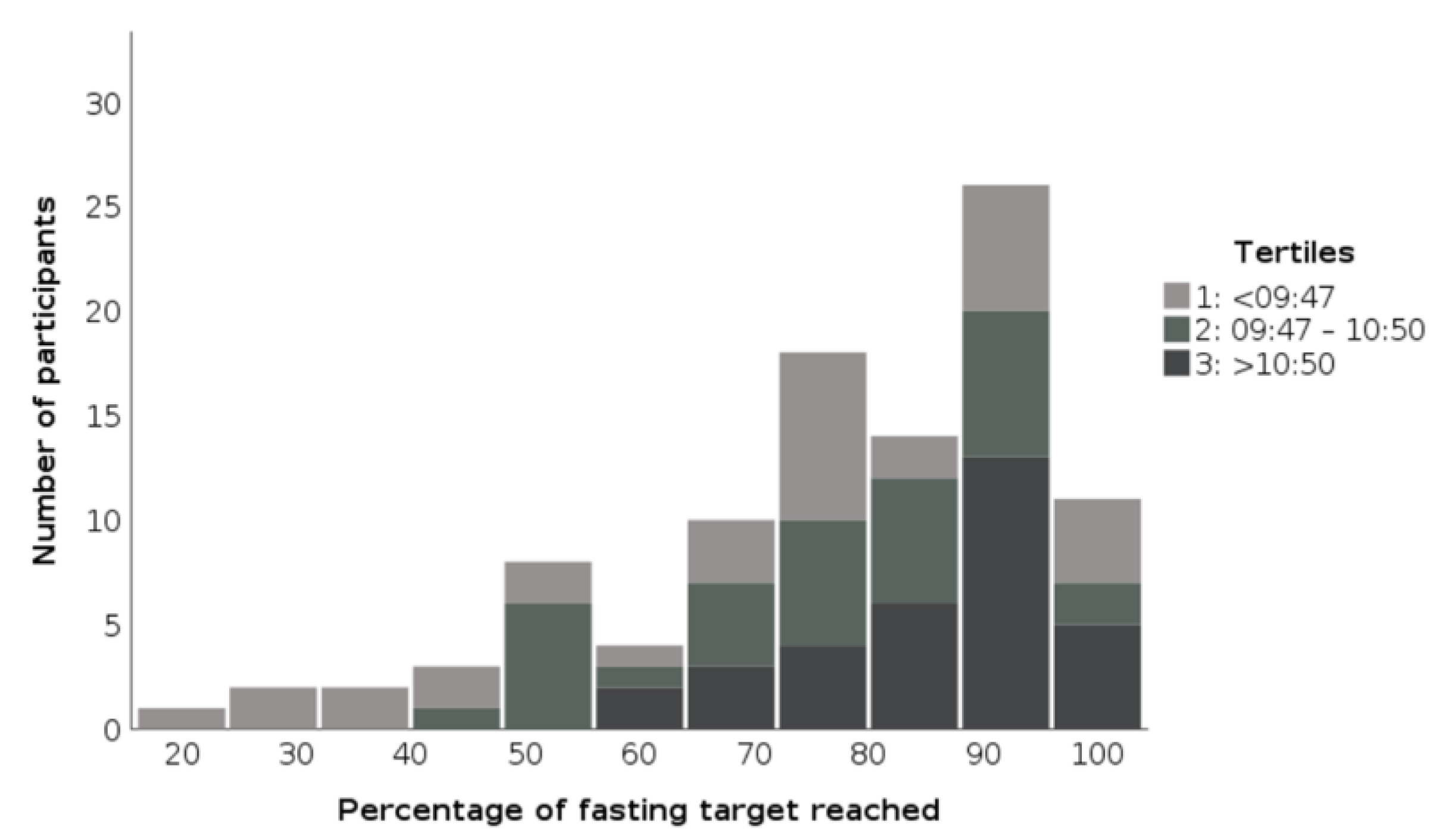
3.2. Diaries
4. Discussion
4.1. Results in the Context of Current Research
4.1.1. Health-Related Quality of Life
4.1.2. Timing of Food Intake
4.1.3. Sleep and Active Phase
4.2. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fryar, C.D.; Carroll, M.D.; Afful, J. Prevalence of Overweight, Obesity, and Severe Obesity among Adults Aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats; 2020. Available online: https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult.htm (accessed on 2 June 2021). [CrossRef]
- Eurostat Data Browser: Body Mass Index (BMI) by Sex, Age and Educational Attainment Level. 2021. Available online: https://ec.europa.eu/eurostat/databrowser/view/hlth_ehis_bm1e/default/table?lang=en (accessed on 16 September 2021).
- World Health Organization (WHO). European Health Information Gateway: Obesity. 2020. Available online: https://gateway.euro.who.int/en/indicators/h2020_9-obesity/visualizations/#id=17080 (accessed on 16 September 2021).
- Wilhelmi De Toledo, F.; Buchinger, A.; Burggrabe, H.; Hölz, G.; Kuhn, C.; Lischka, E.; Lischka, N.; Lützner, H.; May, W.; Ritzmann-Widderich, M.; et al. Fasting therapy—An expert panel update of the 2002 consensus guidelines. Komplement 2013, 20, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Amigo, I.; Fernández, C. Effects of diets and their role in weight control. Psychol. Health Med. 2007, 12, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Cameron, R.P.; Killen, J.D.; Hayward, C.; Taylor, C.B. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J. Consult. Clin. Psychol 1999, 67, 967–974. [Google Scholar] [CrossRef] [PubMed]
- Cherkas, A.; Golota, S. An intermittent exhaustion of the pool of glycogen in the human organism as a simple universal health promoting mechanism. Med. Hypotheses 2014, 82, 387–389. [Google Scholar] [CrossRef]
- Manoogian, E.N.C.; Panda, S. Circadian rhythms, time-restricted feeding, and healthy aging. Ageing Res. Rev. 2017, 39, 59–67. [Google Scholar] [CrossRef]
- Gabel, K.; Varady, K.A. Current research: Effect of time restricted eating on weight and cardiometabolic health. J. Physiol. 2020, 1–14. [Google Scholar] [CrossRef]
- Rothschild, J.; Hoddy, K.K.; Jambazian, P.; Varady, K.A. Time-restricted feeding and risk of metabolic disease: A review of human and animal studies. Nutr. Rev. 2014, 72, 308–318. [Google Scholar] [CrossRef]
- Kesztyüs, D.; Cermak, P.; Gulich, M.; Kesztyüs, T. Adherence to time-restricted feeding and impact on abdominal obesity in primary care patients: Results of a pilot study in a pre-post design. Nutrients 2019, 11, 2854. [Google Scholar] [CrossRef] [Green Version]
- Kesztyüs, D.; Fuchs, M.; Cermak, P.; Kesztyüs, T. Associations of time-restricted eating with health-related quality of life and sleep in adults: A secondary analysis of two pre-post pilot studies. BMC Nutr. 2020, 6, 4–11. [Google Scholar] [CrossRef]
- Kesztyüs, D.; Vorwieger, E.; Schönsteiner, D.; Gulich, M.; Kesztyüs, T. Applicability of time restricted eating for the prevention of lifestyle-dependent diseases in a working population: Results of a pilot study in a pre-post design. GMS 2021, 19, Doc04. [Google Scholar] [CrossRef]
- Charlot, A.; Hutt, F.; Sabatier, E.; Zoll, J. Beneficial effects of early time-restricted feeding on metabolic diseases: Importance of aligning food habits with the circadian clock. Nutrients 2021, 13, 1405. [Google Scholar] [CrossRef]
- Tippairote, T.; Janssen, S.; Chunhabundit, R. Restoration of metabolic tempo through time-restricted eating (TRE) as the preventive measure for metabolic diseases. Crit. Rev. Food Sci. Nutr. 2021, 61, 2444–2453. [Google Scholar] [CrossRef]
- Richter, J.; Herzog, N.; Janka, S.; Baumann, T.; Kistenmacher, A.; Oltmanns, K.M. Twice as High Diet-Induced Thermogenesis After Breakfast vs Dinner On High-Calorie as Well as Low-Calorie Meals. J. Clin. Endocrinol. Metab. 2020, 105, 1–11. [Google Scholar] [CrossRef]
- Poggiogalle, E.; Jamshed, H.; Peterson, C.M. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism 2018, 84, 11–27. [Google Scholar] [CrossRef] [Green Version]
- Ni, Y.; Wu, L.; Jiang, J.; Yang, T.; Wang, Z.; Ma, L.; Zheng, L.; Yang, X.; Wu, Z.; Fu, Z. Late-Night Eating-Induced Physiological Dysregulation and Circadian Misalignment Are Accompanied by Microbial Dysbiosis. Mol. Nutr. Food Res. 2019, 63, 1–14. [Google Scholar] [CrossRef]
- Thomas, E.A.; Zaman, A.; Cornier, M.A.; Catenacci, V.A.; Tussey, E.J.; Grau, L.; Arbet, J.; Broussard, J.L.; Rynders, C.A. Later meal and sleep timing predicts higher percent body fat. Nutrients 2021, 13, 73. [Google Scholar] [CrossRef]
- Queiroz, J.D.N.; Macedo, R.C.O.; Tinsley, G.M.; Reischak-Oliveira, A. Time-restricted eating and circadian rhythms: The biological clock is ticking. Crit. Rev. Food Sci. Nutr. 2020, 1–13. [Google Scholar] [CrossRef]
- Ashwell, M.; Hsieh, S.D. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int. J. Food Sci. Nutr. 2005, 56, 303–307. [Google Scholar] [CrossRef]
- Barton, G.R.; Sach, T.H.; Doherty, M.; Avery, A.J.; Jenkinson, C.; Muir, K.R. An assessment of the discriminative ability of the EQ-5D index, SF-6D, and EQ VAS, using sociodemographic factors and clinical conditions. Eur. J. Health Econ. 2008, 9, 237–249. [Google Scholar] [CrossRef]
- Gill, S.; Panda, S. A Smartphone App Reveals Erratic Diurnal Eating Patterns in Humans that Can Be Modulated for Health Benefits. Cell Metab. 2015, 22, 789–798. [Google Scholar] [CrossRef] [Green Version]
- Regmi, P.; Heilbronn, L.K. Time-Restricted Eating: Benefits, Mechanisms, and Challenges in Translation. IScience 2020, 23, 101161. [Google Scholar] [CrossRef]
- Heilbronn, L.K.; Regmi, P. Will Delaying Breakfast Mitigate the Metabolic Health Benefits of Time-Restricted Eating? Obesity 2020, 28, S6–S7. [Google Scholar] [CrossRef]
- Moon, S.; Kang, J.; Kim, S.H.; Chung, H.S.; Kim, Y.J.; Yu, J.M.; Cho, S.T.; Oh, C.M.; Kim, T. Beneficial effects of time-restricted eating on metabolic diseases: A systemic review and meta- analysis. Nutrients 2020, 12, 1267. [Google Scholar] [CrossRef]
- Després, J.P. Obesity and cardiovascular disease: Weight loss is not the only target. Can. J. Cardiol. 2015, 31, 216–222. [Google Scholar] [CrossRef]
- FDA. Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims Guidance for Industry. 2009. Available online: http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf (accessed on 2 June 2021).
- Ogden, J. QALYs and their role in the NICE decision-making process. Prescriber 2017, 28, 41–43. [Google Scholar] [CrossRef]
- Nugraha, B.; Ghashang, S.K.; Hamdan, I.; Gutenbrunner, C. Effect of Ramadan fasting on fatigue, mood, sleepiness, and health-related quality of life of healthy young men in summer time in Germany: A prospective controlled study. Appetite 2017, 111, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Crose, A.; Alvear, A.; Singroy, S.; Wang, Q.; Manoogian, E.; Panda, S.; Mashek, D.G.; Chow, L.S. Time-Restricted Eating Improves Quality of Life Measures in Overweight Humans. Nutrients 2021, 13, 1430. [Google Scholar] [CrossRef] [PubMed]
- Anton, S.D.; Lee, S.A.; Donahoo, W.T.; McLaren, C.; Manini, T.; Leeuwenburgh, C.; Pahor, M. The effects of time restricted feeding on overweight, older adults: A pilot study. Nutrients 2019, 11, 1500. [Google Scholar] [CrossRef] [Green Version]
- Parr, E.B.; Devlin, B.L.; Lim, K.H.C.; Moresi, L.N.Z.; Geils, C.; Brennan, L.; Hawley, J.A. Time-Restricted Eating as a Nutrition Strategy for Individuals with Type 2 Diabetes: A Feasibility Study. Nutrients 2020, 12, 3228. [Google Scholar] [CrossRef]
- Schroder, J.D.; Falqueto, H.; Mância, A.; Zanini, D.; de Oliveira, T.; de Sá, C.A.; Cardoso, A.M.; Manfredi, L.H. Effects of time-restricted feeding in weight loss, metabolic syndrome and cardiovascular risk in obese women. J. Transl. Med. 2021, 19, 3. [Google Scholar] [CrossRef]
- Allison, K.C.; Hopkins, C.M.; Ruggieri, M.; Spaeth, A.M.; Ahima, R.S.; Zhang, Z.; Taylor, D.M.; Goel, N. Prolonged, Controlled Daytime versus Delayed Eating Impacts Weight and Metabolism. Curr. Biol. 2021, 31, 650–657.e3. [Google Scholar] [CrossRef]
- Singh, R.B.; Cornelissen, G.; Mojto, V.; Fatima, G.; Wichansawakun, S.; Singh, M.; Kartikey, K.; Sharma, J.P.; Torshin, V.I.; Chibisov, S.; et al. Effects of circadian restricted feeding on parameters of metabolic syndrome among healthy subjects. Chronobiol. Int. 2020, 37, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Jamshed, H.; Beyl, R.A.; Della Manna, D.L.; Yang, E.S.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves 24-Hour Glucose Levels and Affects Markers of the Circadian Clock, Aging, and Autophagy in Humans. Nutrients 2019, 11, 1234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lowe, D.A.; Wu, N.; Rohdin-Bibby, L.; Moore, A.H.; Kelly, N.; Liu, Y.E.; Philip, E.; Vitinhoff, E.; Heymsfield, S.B.; Olgin, J.E.; et al. Effects of Time-Restricted Eating on Weight Loss and Other Metabolic Parameters in Women and Men with Overweight and Obesity: The TREAT Randomized Clinical Trial. JAMA Intern. Med. 2020, 941, 1–9. [Google Scholar] [CrossRef]
- Tinsley, G.M.; Peterson, C.M.; Horne, B.D. Caution against Overinterpreting Time-Restricted Eating Results. JAMA Intern. Med. 2021, 181, 877–878. [Google Scholar] [CrossRef]
- Sutton, E.F.; Beyl, R.; Early, K.S.; Cefalu, W.T.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metab. 2018, 27, 1212–1221. [Google Scholar] [CrossRef] [Green Version]
- Gabel, K.; Hoddy, K.; Haggerty, N.; Song, J.; Kroeger, C.; Trepanowski, J.F.; Panda, S.; Varady, K.A. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: A pilot study. Nutr. Health Aging 2018, 4, 345–353. [Google Scholar] [CrossRef]
- de Oliveira Maranhão Pureza, I.R.; Macena, M.d.L.; da Silva Junior, A.E.; Praxedes, D.R.S.; Vasconcelos, L.G.L.; Bueno, N.B. Effect of early time-restricted feeding on the metabolic profile of adults with excess weight: A systematic review with meta-analysis. Clin. Nutr. 2021, 40, 1788–1799. [Google Scholar] [CrossRef]
| Female (n = 83) | Male (n = 16) | Total (n = 99) | |
|---|---|---|---|
| Age, years m (sd) | 49.5 (9.8) | 49.1 (14.6) | 49.9 (10.8) |
| University employees, n (%) | 53 (63.9) | 8 (50.0) | 61 (61.6) |
| Weight, kg m (sd) | 76.2 (16.1) 1 | 97.2 (22.0) | 79.3 (18.5) |
| Waist circumference, cm m (sd) | 94.1 (14.2) 2 | 107.3 (17.0) | 95.7 (18.5) |
| BMI, kg/m2 m (sd) | 27.8 (5.9) | 30.0 (5.3) | 28.0 (5.7) |
| WHtR, m (sd) | 0.57 (0.09) | 0.60 (0.09) | 0.57 (0.09) |
| Overweight, n (%) | 24 (28.9) | 6 (37.5) | 30 (30.3) |
| Obesity, n (%) | 25 (30.1) | 7 (43.8) | 32 (32.2) |
| Abdominal obesity, n (%) | 59 (71.1) | 15 (93.8) | 74 (74.7) |
| TCHOL, mmol/L m (sd) | 5.5 (1.0) | 5.0 (1.1) | 5.4 (1.0) |
| HDL, mmol/L m (sd) | 1.7 (0.4) 1 | 1.2 (0.4) | 1.6 (0.4) |
| LDL, mmol/L m (sd) | 3.5 (1.0) | 3.3 (1.1) | 3.5 (1.0) |
| Triglycerides, mmol/L m (sd) | 1.2 (0.6) 1 | 2.0 (0.9) | 1.4 (0.7) |
| LDL/HDL, m (sd) | 2.3 (0.9) 3 | 2.9 (1.1) | 2.3 (1.0) |
| Triglycerides/HDL, m (sd) | 0.8 (0.6) 1 | 2.1 (1.5) | 1.0 (0.9) |
| HRQoL, m (sd) * | 71.8 (14.0) | 72.5 (12.2) | 72.2 (13.8) |
| Daily eating time, m (sd) ** | 12.4 (1.9) | 12.8 (2.2) | 12.4 (1.9) |
| Tertiles of Beginning of the Eating Phase | ||||
|---|---|---|---|---|
| Before 09:47 | 09:47–10:50 | After 10:50 | p-Value | |
| Number of participants | 33 | 33 | 33 | |
| GPs practice, n (%) | 15 (46) | 7 (21) | 16 (49) | 0.044 a |
| Age, years m (sd) | 50.6 (11.7) | 47.2 (10.3) | 48.9 (10.5) | 0.711 |
| Female, n (%) | 26 (85) | 28 (89) | 29 (88) | 0.593 |
| Weight, kg m (sd) | 78.5 (20.4) | 80.0 (19.4) | 79.3 (16.1) | 0.687 |
| Waist circumference, cm m (sd) | 96.0 (15.4) | 94.4 (15.4) | 96.7 (14.8) | 0.594 |
| BMI, kg/m2 m (sd) | 27.9 (5.8) | 27.5 (5.4) | 28.7 (6.1) | 0.563 |
| WHtR, m (sd) | 0.57 (0.08) | 0.56 (0.09) | 0.58 (0.10) | 0.439 |
| Overweight, n (%) | 9 (27) | 9 (27) | 12 (36) | 0.650 |
| Obesity, n (%) | 9 (27) | 11 (33) | 12 (36) | 0.724 |
| Abdominal obesity, n (%) | 25 (76) | 23 (70) | 26 (79) | 0.688 |
| TCHOL, mmol/L m (sd) | 5.6 (1.2) | 5.3 (0.8) | 5.4 (0.9) | 0.413 |
| HDL, mmol/L m (sd) | 1.5 (0.4) | 1.7 (0.5) | 1.7 (0.4) | 0.049 a |
| LDL, mmol/L m (sd) | 3.6 (1.2) | 3.4 (0.8) | 3.4 (0.9) | 0.429 |
| Triglycerides, mmol/L m (sd) | 1.7 (1.0) b | 1.2 (0.5) | 1.1 (0.4) | 0.020 |
| LDL/HDL, m (sd) | 2.6 (0.9) | 2.1 (0.8) | 2.2 (1.1) | 0.040 a |
| Triglycerides/HDL, m (sd) | 1.5 (1.3) b | 0.8 (0.4) | 0.7 (0.4) | 0.014 |
| HRQoL, m (sd) * | 74.6 (11.9) | 75.5 (13.1) | 66.6 (14.9) | 0.046 a |
| Daily eating time, m (sd) ** | 12.7 (1.9) | 12.4 (1.8) | 12.0 (2.0) | 0.286 |
| Chronotype, n (%) ** | ||||
| Owl | 6 (18) | 11 (34) | 11 (33) | |
| Lark | 23 (70) | 15 (47) | 12 (36) | 0.079 |
| Neither | 4 (12) | 6 (19) | 10 (30) | |
| Tertiles of Beginning of the Eating Phase | ||||
| Before 09:47 | 09:47–10:50 | After 10:50 | p-Value | |
| Weight, kg m (sd) | 77.2 (21.0) | 78.4 (19.2) | 77.7 (15.7) | 0.698 |
| Waist circumference, cm m (sd) | 93.0 (14.9) | 91.6 (14.7) | 93.0 (13.7) | 0.722 |
| BMI, kg/m2 m (sd) | 27.4 (5.9) | 27.0 (5.3) | 28.1 (5.9) | 0.515 |
| WHtR, m (sd) | 0.56 (0.08) | 0.54 (0.08) | 0.56 (0.09) | 0.460 |
| Overweight, n (%) | 5 (15) | 7 (21) | 14 (42) | 0.030 a |
| Obesity, n (%) | 10 (30) | 10 (30) | 11 (33) | 0.954 |
| Abdominal obesity, n (%) | 25 (76) | 21 (64) | 25 (76) | 0.451 |
| TCHOL, mmol/L m (sd) | 5.7 (1.3) | 5.6 (0.9) | 5.6 (1.1) | 0.864 |
| HDL, mmol/L m (sd) | 1.5 (0.4) | 1.7 (0.5) | 1.7 (0.4) | 0.085 |
| LDL, mmol/L m (sd) | 3.7 (1.1) | 3.4 (0.8) | 3.6 (1.0) | 0.579 |
| Triglycerides, mmol/L m (sd) | 1.6 (0.9) | 1.5 (1.0) | 1.2 (0.5) | 0.293 |
| LDL/HDL, m (sd) | 2.6 (0.9) | 2.2 (0.8) | 2.3 (0.9) | 0.099 |
| Triglycerides/HDL, m (sd) | 1.3 (1.1) | 1.1. (1.3) | 0.6 (0.4) | 0.228 |
| HRQoL, m (sd) * | 79.9 (11.6) | 82.8 (9.2) | 76.1 (11.9) c 1 | 0.048 |
| Δ Weight, kg m (sd) | −1.3 (2.8) b 2 | −1.6 (2.0) b 2 | −1.6 (2.5) b 3 | 0.895 |
| Δ Waist circumference, cm m (sd) | −3.0 (3.6) b 5 | −2.8 (3.7) b 4 | −3.7 (3.5) b 2 | 0.536 |
| Δ BMI, m (sd) | −0.5 (1.0) b 4 | −0.5 (0.7) b 4 | −0.6 (0.9) b 3 | 0.918 |
| Δ WHtR, m (sd) | −0.018 (0.022) b 5 | −0.017 (0.022) b 4 | −0.023 (0.022) b 5 | 0.523 |
| Δ TCHOL, mmol/L m (sd) | 0.12 (0.43) | 0.30 (0.48) b 6 | 0.23 (0.56) | 0.320 |
| Δ HDL, mmol/L m (sd) | 0.03 (0.13) | 0.00 (0.14) | −0.02 (0.17) | 0.461 |
| Δ LDL, mmol/L m (sd) | 0.05 (0.43) | 0.05 (0.38) | 0.20 (0.59) | 0.332 |
| Δ Triglycerides, mmol/L m (sd) | −0.17 (0.44) | 0.24 (0.80) | 0.05 (0.41) | 0.044 a |
| Δ HRQoL, m (sd) ** | 5.4 (8.4) b 6 | 8.0 (13.1) b 7 | 10.1 (15.5) b 8 | 0.479 |
| Tertiles of Beginning of the Eating Phase | ||||
| Before 09:47 | 09:47–10:50 | After 10:50 | p-Value | |
| Number of documented days | 87.7 (9.4) | 88.9 (6.7) | 89.4 (5.9) | 0.409 |
| Sleep duration, h m (sd) | 7.4 (0.6) | 7.5 (0.5) | 7.3 (0.7) | 0.206 |
| Sleep quality, m (sd) | 72.0 (15.1) | 72.7 (12.9) | 70.1 (15.6) | 0.749 |
| Time of first meal, m (sd) | 8.82 (0.91) | 10.26 (0.33) | 12.05 (0.69) | <0.001 |
| Time of last meal, m (sd) | 17.39 (1.33) | 18.53 (0.76) | 19.51 (0.84) | <0.001 |
| Eating phase, h m (sd) | 8.6 (1.0) | 8.3 (0.7) | 7.5 (0.8) a | <0.001 |
| Fasting phase, h m (sd) | 15.4 (1.0) | 15.7 (0.6) | 16.5 (0.8) a | <0.001 |
| Fasting target reached, % m (sd) | 70.5 (23.7) | 75.6 (16.0) | 85.5 (11.6) b | 0.013 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kesztyüs, D.; Cermak, P.; Kesztyüs, T.; Barzel, A. Early or Delayed Onset of Food Intake in Time-Restricted Eating: Associations with Markers of Obesity in a Secondary Analysis of Two Pilot Studies. Int. J. Environ. Res. Public Health 2021, 18, 9935. https://doi.org/10.3390/ijerph18189935
Kesztyüs D, Cermak P, Kesztyüs T, Barzel A. Early or Delayed Onset of Food Intake in Time-Restricted Eating: Associations with Markers of Obesity in a Secondary Analysis of Two Pilot Studies. International Journal of Environmental Research and Public Health. 2021; 18(18):9935. https://doi.org/10.3390/ijerph18189935
Chicago/Turabian StyleKesztyüs, Dorothea, Petra Cermak, Tibor Kesztyüs, and Anne Barzel. 2021. "Early or Delayed Onset of Food Intake in Time-Restricted Eating: Associations with Markers of Obesity in a Secondary Analysis of Two Pilot Studies" International Journal of Environmental Research and Public Health 18, no. 18: 9935. https://doi.org/10.3390/ijerph18189935
APA StyleKesztyüs, D., Cermak, P., Kesztyüs, T., & Barzel, A. (2021). Early or Delayed Onset of Food Intake in Time-Restricted Eating: Associations with Markers of Obesity in a Secondary Analysis of Two Pilot Studies. International Journal of Environmental Research and Public Health, 18(18), 9935. https://doi.org/10.3390/ijerph18189935






