Overweight and Obesity in Patients with Congenital Heart Disease: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
- “congenital heart disease” OR “congenital heart defect” AND
- “overweight” OR “obesity” OR “adiposity” OR “body constitution”
2.2. Data Collection
3. Results
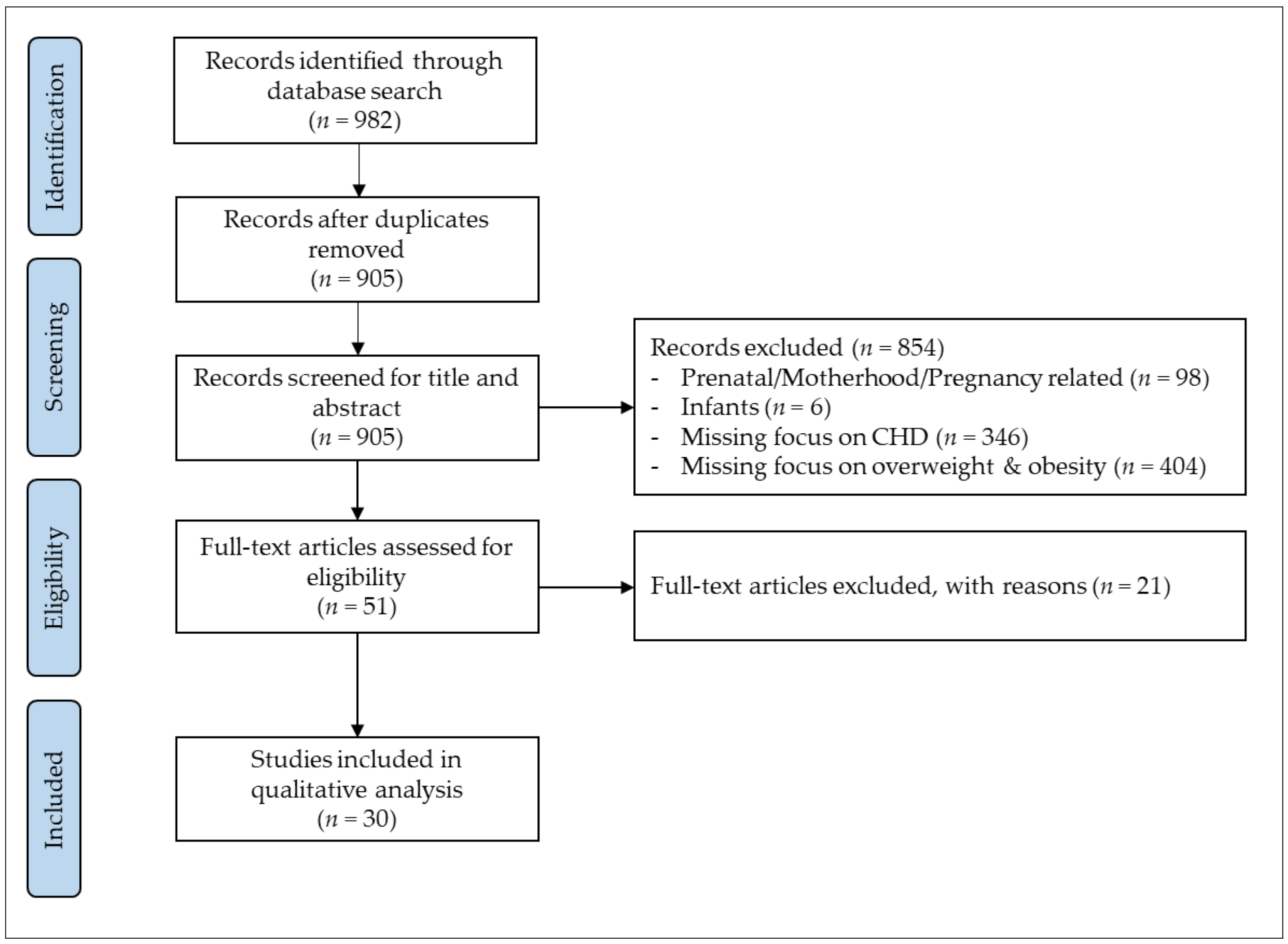
3.1. Study Inclusion
3.2. Study Characteristics
3.3. Measuring Overweight & Obesity
3.4. Study Quality
3.5. Overweight and Obesity in Children with CHD
3.6. Overweight and Obesity in Adults with CHD
3.7. Longitudinal Development of Overweight and Obesity
4. Discussion
Limitations and Further Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of over-weight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [Green Version]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Lawman, H.G.; Fryar, C.D.; Kruszon-Moran, D.; Kit, B.K.; Flegal, K.M. Trends in obesity prevalence among chil-dren and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016, 315, 2292–2299. [Google Scholar] [CrossRef] [PubMed]
- Suchindran, C.; North, K.E.; Popkin, B.M.; Gordon-Larsen, P. Association of Adolescent Obesity With Risk of Severe Obesity in Adulthood. JAMA 2010, 304, 2042–2047. [Google Scholar]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G. A comparative risk assessment of burden of dis-ease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef] [Green Version]
- Khairy, P.; Ionescu-Ittu, R.; Mackie, A.; Abrahamowicz, M.; Pilote, L.; Marelli, A.J. Changing Mortality in Congenital Heart Disease. J. Am. Coll. Cardiol. 2010, 56, 1149–1157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- St-Pierre, J.; Poirier, P. What Nature Used to Allow to Die, Don’t Let Modern Habits Damage After Repair: Preventable Obe-sity Risk in Congenital Heart Disease. Can. J. Cardiol. 2015, 31, 109–111. [Google Scholar] [CrossRef]
- Lui, G.K.; Fernandes, S.; McElhinney, D.B. Management of Cardiovascular Risk Factors in Adults With Congenital Heart Disease. J. Am. Hear. Assoc. 2014, 3, e001076. [Google Scholar] [CrossRef] [Green Version]
- Verheugt, C.L.; Uiterwaal, C.S.P.M.; Van Der Velde, E.T.; Meijboom, F.J.; Pieper, P.G.; van Dijk, A.; Vliegen, H.W.; Grobbee, D.E.; Mulder, B.J. Mortality in adult congenital heart disease. Eur. Hear. J. 2010, 31, 1220–1229. [Google Scholar] [CrossRef] [Green Version]
- Wellnitz, K.; Harris, I.S.; Sapru, A.; Fineman, J.R.; Radman, M. Longitudinal development of obesity in the post-Fontan population. Eur. J. Clin. Nutr. 2015, 69, 1105–1108. [Google Scholar] [CrossRef] [Green Version]
- Diller, G.-P.; Kempny, A.; Alonso-Gonzalez, R.; Swan, L.; Uebing, A.; Li, W.; Babu-Narayan, S.; Wort, S.J.; Dimopoulos, K.; Gatzoulis, M.A. Survival Prospects and Circumstances of Death in Contemporary Adult Congenital Heart Disease Patients Under Follow-Up at a Large Tertiary Centre. Circulation 2015, 132, 2118–2125. [Google Scholar] [CrossRef] [Green Version]
- Costello, C.L.; Gellatly, M.; Daniel, J.; Justo, R.N.; Weir, K. Growth Restriction in Infants and Young Children with Congenital Heart Disease. Congenit. Hear. Dis. 2015, 10, 447–456. [Google Scholar] [CrossRef]
- Zomer, A.C.; Vaartjes, I.; Uiterwaal, C.S.; van der Velde, E.T.; Sieswerda, G.-J.T.; Wajon, E.M.; Plomp, K.; van Bergen, P.F.; Verheugt, C.L.; Krivka, E.; et al. Social Burden and Lifestyle in Adults With Congenital Heart Disease. Am. J. Cardiol. 2012, 109, 1657–1663. [Google Scholar] [CrossRef]
- Brida, M.; Dimopoulos, K.; Kempny, A.; Liodakis, E.; Alonso-Gonzalez, R.; Swan, L.; Uebing, A.; Baumgartner, H.; Gatzoulis, M.A.; Diller, G.-P. Body mass index in adult congenital heart disease. Heart 2017, 103, 1250–1257. [Google Scholar] [CrossRef] [PubMed]
- Uman, L.S. Systematic reviews and meta-analyses. J. Can. Acad. Child. Adolesc. Psychiatry 2011, 20, 57. [Google Scholar]
- National Heart, Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies 2014. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 1 June 2021).
- Aguilar, D.C.; Raff, G.W.; Tancredi, D.; Griffin, I.J. Childhood growth patterns following congenital heart disease. Cardiol. Young 2015, 25, 1044–1053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avitabile, C.M.; Leonard, M.B.; Zemel, B.S.; Brodsky, J.L.; Lee, D.; Dodds, K.; Hayden-Rush, C.; Whitehead, K.K.; Goldmuntz, E.; Paridon, S.M.; et al. Lean mass deficits, vitamin D status and exercise capacity in children and young adults after Fontan palliation. Heart 2014, 100, 1702–1707. [Google Scholar] [CrossRef] [Green Version]
- Barbiero, S.M.; D’Azevedo Sica, C.; Schuh, D.S.; Cesa, C.C.; de Oliveira Petkowicz, R.; Pellanda, L.C. Overweight and obesity in children with congenital heart disease: Combination of risks for the future? BMC Pediatrics 2014, 14, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barbour-Tuck, E.; Boyes, N.G.; Tomczak, C.R.; Lahti, D.S.; Baril, C.L.; Pockett, C.; Runalls, S.; Kakadekar, A.; Pharis, S.; Bradley, T.J.; et al. A cardiovascular disease risk factor in chil-dren with congenital heart disease: Unmasking elevated waist circumference-a CHAMPS* study *CHAMPS: Children’s Healthy-Heart Activity Monitoring Program in Saskatchewan. BMC Cardiovasc. Disord. 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Briston, D.A.; Sabanayagam, A.; Zaidi, A.N. Observations on obesity patterns in tetralogy of Fallot patients from childhood to adulthood. Cardiol. Young 2017, 27, 890–894. [Google Scholar] [CrossRef]
- Buys, R.; Budts, W.; Delecluse, C.; Vanhees, L. Exercise Capacity, Physical Activity, and Obesity in Adults With Repaired Aortic Coarctation. J. Cardiovasc. Nurs. 2013, 28, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-A.; Wang, J.-K.; Lue, H.-C.; Hua, Y.-C.; Chang, M.-H.; Wu, M.-H. A Shift from Underweight to Overweight and Obesity in Asian Children and Adolescents with Congenital Heart Disease. Paediatr. Périnat. Epidemiol. 2012, 26, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.T.; Hong, B.; Patterson, L.; Petit, C.J.; Ham, J.N. High Overweight and Obesity in Fontan Patients: A 20-Year History. Pediatr. Cardiol. 2016, 37, 192–200. [Google Scholar] [CrossRef]
- Fedchenko, M.; Mandalenakis, Z.; Dellborg, H.; Hultsberg-Olsson, G.; Björk, A.; Eriksson, P.; Dellborg, M. Cardiovascular risk factors in adults with coarctation of the aorta. Congenit. Hear. Dis. 2019, 14, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.C.; Voss, C.; Rankin, K.; Aminzadah, B.; Gardner, R.; Mackie, A.S. Modifiable cardiovascular risk factors in adolescents and adults with congenital heart disease. Congenit. Hear. Dis. 2018, 13, 563–570. [Google Scholar] [CrossRef]
- Jackson, J.L.; Fox, K.R.; Cotto, J.; Harrison, T.M.; Tran, A.H.; Keim, S.A. Obesity across the lifespan in congenital heart disease survi-vors: Prevalence and correlates. Heart Lung 2020, 49, 788–794. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.L.; Harrison, T.; Keim, S. Differences in Obesity Among Black and White Children, Adolescents, and Adults With Congenital Heart Disease. J. Cardiovasc. Nurs. 2019, 34, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Lerman, J.B.; Parness, I.A.; Shenoy, R.U. Body Weights in Adults With Congenital Heart Disease and the Obesity Frequency. Am. J. Cardiol. 2017, 119, 638–642. [Google Scholar] [CrossRef]
- Lui, G.K.; Rogers, I.S.; Ding, V.Y.; Hedlin, H.K.; MacMillen, K.; Maron, D.J.; Sillman, C.; Romfh, A.; Dade, T.C.; Haeffele, C.; et al. Risk Estimates for Atherosclerotic Cardiovascular Disease in Adults With Congenital Heart Disease. Am. J. Cardiol. 2017, 119, 112–118. [Google Scholar] [CrossRef] [Green Version]
- Malavazos, A.; Capitanio, G.; Chessa, M.; Matelloni, I.A.; Milani, V.; Stella, E.; Al Kassem, L.; Sironi, F.; Boveri, S.; Giamberti, A.; et al. Body mass index stratification in hospitalized Italian adults with congenital heart disease in relation to complexity, diagnosis, sex and age. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 367–377. [Google Scholar] [CrossRef]
- O’Byrne, M.L.; McBride, M.G.; Paridon, S.; Goldmuntz, E. Association of Habitual Activity and Body Mass Index in Survivors of Congenital Heart Surgery: A Study of Children and Adolescents With Tetralogy of Fallot, Transposition of the Great Arteries, and Fontan Palliation. World J. Pediatr. Congenit. Hear. Surg. 2018, 9, 177–184. [Google Scholar] [CrossRef]
- Perin, F.; Blesa, C.C.; Cobo, I.; Maldonado, J. Overweight and obesity in children treated for congenital heart disease. An. de Pediatría 2018, 90, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Pike, N.A.; Evangelista, L.; Doering, L.V.; Eastwood, J.-A.; Lewis, A.B.; Child, J.S. Sex and Age Differences in Body-Image, Self-Esteem, and Body Mass Index in Adolescents and Adults After Single-Ventricle Palliation. Pediatr. Cardiol. 2012, 33, 705–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powell, A.W.; Wittekind, S.G.; Alsaied, T.; Lubert, A.M.; Chin, C.; Veldtman, G.R.; Cordina, R.; Katz, D.A.; Mays, W.A.; Knecht, S.K.; et al. Body Composition and Exercise Performance in Youth With a Fontan Circulation: A Bio-Impedance Based Study. J. Am. Hear. Assoc. 2020, 9, e018345. [Google Scholar]
- Ray, T.D.; Green, A.; Henry, K. Physical activity and obesity in children with congenital cardiac disease. Cardiol. Young 2011, 21, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Sandberg, C.; Rinnström, D.; Dellborg, M.; Thilén, U.; Sörensson, P.; Nielsen, N.E.; Christersson, C.; Wadell, K.; Johansson, B. Height, weight and body mass index in adults with congenital heart disease. Int. J. Cardiol. 2015, 187, 219–226. [Google Scholar] [CrossRef]
- Smith-Parrish, M.; Yu, S.; Rocchini, A. Obesity and Elevated Blood Pressure following Repair of Coarctation of the Aorta. J. Pediatr. 2014, 164, 1074–1078.e1. [Google Scholar] [CrossRef]
- Steele, J.M.; Preminger, T.J.; Erenberg, F.G.; Wang, L.; Dell, K.; Alsaied, T.; Zahka, K.G. Obesity trends in children, adolescents, and young adults with congenital heart disease. Congenit. Hear. Dis. 2019, 14, 517–524. [Google Scholar] [CrossRef]
- Welisch, E.; Rauch, R.; Seabrook, J.A.; Filler, M.G.; Norozi, K. Are the children and adolescents with congenital heart disease living in Southwestern Ontario really overweight and obese? Cardiol. Young 2013, 24, 848–853. [Google Scholar] [CrossRef]
- Yang, F.-L.; Gau, B.-S.; Yang, H.-L.; Lin, M.-T.; Moons, P. Energy Balance-Related Behaviors and Body Mass Index in Asian School-Aged Children With Congenital Heart Disease. J. Cardiovasc. Nurs. 2020, 35, 291–299. [Google Scholar] [CrossRef]
- Zaqout, M.; Vandekerckhove, K.; Michels, N.; Demulier, L.; Bove, T.; François, K.; de Backer, J.; de Henauw, S.; de Wolf, D. Body mass index in adults with congenital heart disease. Congenit. Hear. Dis. 2019, 14, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Deen, J.F.; Krieger, E.; Slee, A.E.; Arslan, A.; Arterburn, D.; Stout, K.K.; Portman, M.A. Metabolic Syndrome in Adults With Congenital Heart Disease. J. Am. Hear. Assoc. 2016, 5, e001132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamayo, C.; Manlhiot, C.; Patterson, K.; Lalani, S.; McCrindle, B.W. Longitudinal evaluation of the prevalence of over-weight/obesity in children with congenital heart disease. Can. J. Cardiol. 2015, 31, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, S.J.; Pianelli, A.J.; Tanga, S.R.; Parness, I.A.; Shenoy, R.U. Risk factors for development of obesity in an ethnically diverse CHD population. Cardiol. Young 2019, 29, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Sen, A.; Norat, T.; Janszky, I.; Romundstad, P.; Tonstad, S.; Vatten, L.J. Body mass index, abdominal fatness, and heart failure incidence and mortality: A systematic review and dose-response meta-analysis of prospective studies. Circulation 2016, 133, 639–649. [Google Scholar] [CrossRef]
- Fantuzzi, G.; Mazzone, T. Adipose tissue and atherosclerosis: Exploring the connection. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 996–1003. [Google Scholar] [CrossRef]
- O’Byrne, M.L.; Kim, S.; Hornik, C.P.; Yerokun, B.A.; Matsouaka, R.A.; Jacobs, J.P.; Jacobs, M.L.; Jonas, R.A. Effect of obesity and underweight status on perioperative outcomes of congenital heart operations in children, adolescents, and young adults: An analysis of data from the society of thoracic surgeons database. Circulation 2017, 136, 704–718. [Google Scholar] [CrossRef]
- Garcia, R.U.; Balakrishnan, P.L.; Aggarwal, S. Does obesity affect the short-term outcomes after cardiothoracic surgery in adoles-cents with congenital heart disease? Cardiol. Young 2020, 30, 372–376. [Google Scholar] [CrossRef]
| Study | CHD, n (♀) | Control Group, n (♀) | CHD Diagnosis or Severity (n) | Age ± SD (Range), y | Reference | Body Constitution | Prevalence (%) Overweight/Obesity (Both) | Results |
|---|---|---|---|---|---|---|---|---|
| PEDIATRIC CHD (n = 15) | ||||||||
| Tamayo et al., 2015 [44] | 725 (319) | - | ASD (116), VSD (152), AVSD (116), TGA (138), UVH (73), ToF/DORV (130) | Median age at complete repair 0.6 | Center of Disease Control Atlanta | * | 28/17 | Proportion of overweight & obesity increased over time (p = 0.02). Patients with TGA showed higher BMI at any time point compared with other cardiac diagnoses (p < 0.001). |
| Wellnitz et al., 2015 [10] |
84 (40) | - | undergoing Fontan palliation | At Fontan surgery: 4.72 (IQR: 3.51–5.14) |
Centers for Disease Control | * |
(Fontan: 10.7 1 y after: 20.3 5 y after: 30) | Time of Fontan: lower percentage of overweight/obesity compared with US children (10.7% versus 30.4%). 1 y after Fontan: overweight/obese children increased to 20.3%. 5 y after Fontan: increased to 30%. Increase in BMI after Fontan significantly associated with Hispanic ethnicity (p < 0.001). |
| Powell et al., 2020 [35] | 47 (22) | 165 (86) age-matched | Fontan circulation | 15.0 ± 3.1 | - | BIA | 23/- | Patients with Fontan had similar BMI as normal controls, but had higher body fat percentage (p = 0.03), lower lean muscle mass (p = 0.005) and skeletal muscle mass (p = 0.004). |
| O’Byrne et al., 2018 [32] | 253 (106) | - | ToF (78), TGA (20), Fontan (74) | 13.1 ± 2.9 | United States Centers for Disease Control | * | 15/11 | Increasing exercise duration was associated with lower BMI (p = 0.01). Restriction to mild exertion and participation in low-intensity exercise were both associated with increased BMI. |
| Aguilar et al., 2015 [17] | 551 (251) | - | CoA (79), VSD (281), ToF (66), TGA (65), SV (34), HLHS (26) | Median 7.5 | Center for Disease Control & Prevention Growth Chart | - | 2–7 y: BMI Z-score increased during early childhood in VSD, and ♀ patients with CoA or HLHS. 8–15 y: BMI Z-score increased in those with CoA and ToF. 2–20 y: BMI Z-score gain between 2–20 y was increased in CoA (♀ only), HLHS (♀ only) VSD, and decreased in SV (♀only) and TGA. | |
| Barbour-Tuck et al., 2020 [20] | 32 (12) |
23 (10) age- and sex matched | Fontan (7), ToF (5), HT (4), TGA (3), ASD (2), PS (2), VSD (1), CoA (2), AS (1), TA (1), CM (2), DORF (2) | 10.9 ± 2.6 | - |
WC & DXA | Mean BMI 18.9 ± 4.7 kg/m2 | CHD participants had a significantly greater waist circumference than controls when controlling for sex, birth weight, physical activity, and total lean mass. CHD and control groups were similar in BMI, total fat mass, total lean mass, percent fat mass, percent lean mass. |
| Welisch et al., 2013 [40] | 1080 (483) | 1083 (472) | VSD, ASD, PDA (146); Fallot, TGA, TAC, VD, AVSD, CoA (369); VD (271), F&M&S (40), Shunt (227), other (27) | 9.0 ± 4.7 | Center for Disease Control and Prevention BMI curve | * | (18.2) | No significant difference concerning weight category between CHD and healthy controls. No difference in overweight/obesity prevalence between operated and non-operated CHD. Age and gender not risk factors for being overweight/obese. |
| Barbiero et al., 2014 [19] | 316 (140) | - | VSD (76), ASD (61), ToF (43), PA (6), others (130) | 2–5 y: 67 6–11 y: 138 12–18 y: 111 | according to the WHO-2006/07 | * | 17.4/9.5 | Excess weight was more common among ♂ (60%). Family history of obesity was associated with excess weight (p = 0.001). In patients with cyanotic lesions, overweight was less frequent than in acyanotic (23.3% vs. 27.7%). |
| Briston et al., 2017 [21] | 137 (66) | 1:1 age-matched controls | ToF | NR | - | ** | 19/19 | In the first 5 y of age and in the first 5 y postoperatively, the ToF cohort had a significantly lower BMI compared with the control group (p = 0.042 and p = 0.028). Afterward, no sig. difference between CHD & healthy controls (p = 0.079). |
| Chen et al., 2012 [23] | Child: 705 (368) Adolescent: 219 (192) | Child: 18,753 (7798) Adolescent: 15,014 (7666) | VSD (319), ASD II (209), PVD (99), PDA (72), AVD (38), CAVF (15), ToF (65) ECD (17), TGA (14), VSD with CoA (13), CoA (12), VSD with R (12), PA (7), EBS (8), Other (22) | Child: 6.4 ± 0.5 Adolescent: 15.5 ± 0.6 | Nutrition and Health Survey in Taiwan | * | (Child: 14.5, Adolescent: 26.5%) | The prevalence of overweight/obesity in CHD adolescents close to controls. In ♀ fewer CHD children were overweight/obese (12.2% vs. 18.7%, p = 0.002). ♂ with moderate to severe CHD had a lower prevalence of overweight/obesity (p = 0.025). Children with cyanotic CHD had significantly lower prevalence of overweight/ obesity (1.5% vs. 15.5%, p = 0.003) than those with non-cyanotic. |
| Perin et al., 2019 [33] | 220 (95) | 220 (93) | No residual defect (142), residual defects (58), UVH (20) | 11.4 ± 2.8 | 2007 World Health Organization growth charts | * | (35.4) | Higher prevalence of obesity in CHD patients (22.7%) compared to 15.5% in healthy subjects (p = 0.015). Higher proportion of obese children in the age 6–11 subgroup (28.6%) compared to the age 12–17 subgroup (16%, p = 0.006). |
| Ray et al., 2011 [36] | 84 (33) | - | Mild (21.5%), Moderate (16.7%), Surgically (40.5%), Complex (21.4%) | 12 ± 1.4 | Centers for Disease Control and Prevention | * | 9.5/26.2 | % of children who were overweight/obese ranged from 22% to 44%, with the lowest incidence in those with moderate disease or that were surgically corrected and the highest incidence in those with mild disease. |
| Steele et al., 2019 [39] | 968 (419) | - | Cyanotic (232), Repaired or palliated (719), Acyanotic (217), Electrophysiologic (184) | 13.3 (8.8–16.4) | Center for Disease Control | * | 31.5/16.4 | Children with overweight/obesity were older (p < 0.001), had lower median household income (p = 0.031), and more often complex CHD (p = 0.008). Children with CHD have an increased risk of becoming overweight & obese in early childhood. |
| Yang et al., 2020 [41] | 97 (45) | - | ASD (33), VSD (30), PDA (9), TGA (9), ToF (12), Endocardial cushion defect (4) | 9.7 ± 1.5 | 50th-percentile BMI for Taiwanese children | * | (14.4) | BMI did not differ between CHD and children in the general population. Greater obesity in children with mild heart disease (p = 0.04). Sedentary behaviors, cardiomegaly, and the NYHA class II–IV were associated with being overweight/obese. |
| Smith-Parris et al., 2014 [38] | 160 (59) | Adult with AS, PS or ASD | Underwent CoA repair | median age at follow-up of 14 y (range, 4.6–36.7 y) | National Health & Nutrition Examination Survey | * | (47) | At age 5 y, patients with CoA had significantly greater BMI z-scores compared with age-sex matched normal data (p < 0.001). The proportion of excess weight in COA significantly increased over time (p < 0.001). Adults with repaired COA developed obesity at a greater rate than those with either AS (p = 0.004) or with PS or ASD (p < 0.001). |
| CHILDREN & ADULTS (n = 6) | ||||||||
| Chung et al., 2016 [24] | Child: 395 Adult: 129 (58) | - | Fontan circulation | Child: 2–5 y: 401 6–11 y: 333 12–19 y: 217 Adult: 27.8 ± 6.8 | Center for Disease Control | * | Adults: 22/17 (Children: 15) | The likelihood of being overweight/obese as an adult was three times higher if there was a BMI ≥ 85th percentile in childhood (p < 0.01). Pediatric rates of overweight/obesity comparable to healthy controls. No race or gender differences between overweight/ obese. Overweight/obesity in adulthood was associated with lower heart failure rates (4 vs.19%, p = 0.03). |
| Avitabile et al., 2014 [18] | 50 (24) | 992 healthy controls | Fontan Median 9.3 years from Fontan | Median: 11.5 (5.1–33.5) | 2000 National Center for Health growth statistics | DXA | BMI z-Score: 0.15 ± 0.98 | BMI Z-scores did not differ between Fontan and healthy controls (0.15 ±0.98 vs 0.35 ± 1.02, p = 0.18). Whole-body lean mass Z-scores were lower in the Fontan participants compared with reference (p = 0.003). |
| Jackson et al., 2019 [28] | 4496 (2158) | - | 36% simple, 50% moderate, 14% complex | 6–12 y: 1327 13–18 y:1005 19–39 y:1312 40+ y: 842 | Centers for Disease Control and Prevention | ** | White&Black: 6–12 y: 15/19 & 18/15 13–18 y: 18/20 & 21/27 19–39 y: 31/27 & 28/42 40+: 34/40 & 32/52 | White children with CHD had a higher prevalence of obesity (18.6%) compared to healthy controls (13.8%) (p < 0.01). White young adults with CHD had a lower prevalence of obesity (27.4%) as compared with white young controls (31.1%) (p < 0.01). No differences between white CHD & healthy adolescents (19.8% vs. 20.8%), as well as black CHD survivors of all ages. Blacks with CHD had a 58% increased risk of obesity in young adulthood and 33% in late adulthood. |
| Harris et al., 2018 [26] |
Youth:
88 (36) Adult: 102 (47) | - | Youth: 32% mild, 40% moderate, 28% complex Adult: 30% mild, 47% moderate, 23% complex | Youth: 17.2 ± 1.1 Adults: 35.4 ± 12.9 | International Obesity Task Force criteria | ** | Youth: 10/11 Adults: 30/22 | More adults than youth overweight/obese (52% vs. 22%, p < 0.001). Group mean BMI and prevalence of weight categories were not different by sex in adults, but in youth, more ♀ than ♂ were overweight/ obese (33% vs. 13%, p = 0.026). |
| Weinreb et al., 2019 [45] | 223 (97) | 223 1:1 age, sex & race matched controls | 34% simple, 32% moderate, 34% complex | 5–11 y 95 11–15 y: 64 16–20 y: 64 | Commission for Disease Control BMI | * | (25) | Mean BMI% did not differ between CHD sample and paired controls over a 5 y period. Significant increased BMI% change in the age cohort of 5–10 y (p = 0.04), in ♂ sex (p = 0.01) and status-post surgery (p = 0.02). |
| Jackson et al., 2020 [27] | 3790 (1868) | - | 36% simple, 50% moderate, 14% severe | 6–18 y: 1927 19–39 y: 1139 40+ y: 724 | Center for Disease Control & Prevention | * | Youth: 17/18 Young adults: 30/30 Adult: 33/40 | The proportion of individuals with overweight/obesity increased with age (p < 0.001). A higher proportion of individuals with moderate lesion severity (29%) had obesity compared to simple (24%) and complex (18%, p < 0.001) lesion severity |
| ADULTS (n = 9) | ||||||||
| Lerman et al., 2017 [29] | 1451 (719) | 1451 (719) age, gender & race-matched | Simple (1007), Complex (299), Unclassified (145) | 52 ± 20 | - | ** | 33.5/25.6 | ACHD were equally as likely to be overweight/obese as controls; ACHD decreased the prevalence of morbid obesity. Age correlated with increased BMI in ACHD and controls (p < 0.001). BMI was similar across all disease severity groupings. Hispanic patients were more likely to be obese than white patients (p = 0.02) & controls (p = 0.01). |
| Buys et al., 2013 [22] | 103 (33) | - | CoA | 28.7 ± 6.3 | Belgian health survey | ** | ♂: 27/7 ♀:18/12 | Weight status was similar to the overall Belgian population, with a tendency toward higher BMI. A tendency towards higher incidence in obesity in ♀ patients. |
| Lui et al., 2017 [8] | 178 (87) | - | Fallot (26%), TGA (20%), Fontan with UVH (15%) | 37.1 ± 12.6 | - | ** | 53/21 | Excess adiposity was the most common risk factor for developing atherosclerotic cardiovascular disease in ACHD. |
| Pike et al., 2012 [34] | 54 (28) | 66 age, sex, ethnicity, family, region & education | Fontan | 26 ± 9 | Center for Disease Control | * | (21) | No sex differences in BMI in the SVCHD group. Patients >21 y higher BMI compared with patients ≤ 21 years of age (p = 0.01). |
| Fedchenko et al., 2019 [25] | 72 (30) | - | CoA | median 43.5 (20–71) | - | ** | 38.9/9.7 | Cardiovascular risk factors were prevalent among patients with CoA. |
| Zaqout et al., 2019 [42] | 539 (248) | 1737 (896) from Belgium | VSD (78), ASD (54), VPS (30), PDA (14), MVD (9), AS/AR (86), CoA/VSD (73), TOF (74), AVSD (34), TGA (14), TGA/ ASO (16), TCPC (30), TrA (6), PA/DORV (21) | 32.0 ± 9.3 | - | ** | 23.7/10 | ACHD patients had lower BMI than healthy controls (p = 0.012). BMI was positively associated with age (p < 0.001). Men in the mild & severe group (p = 0.007; p = 0.023) and women in the severe group (p < 0.001) had lower BMI compared to the reference group. Men with VSD, CoA and Fontan and women with Fontan had lower BMI than controls. |
| Deen et al., 2016 [43] | 448 (230) | 448 sex & age matched | ToF (95), VD (86), AAA (77), TGA (51), Fontan (43), VSD (21), AVSD (21), ccTGA (20), APVR (20), EBS (16), ASD (11), CAA (8), TAC (7), EM (8), PA (8), other (51) | 32.4 ± 11.3 | International Diabetes Foundation Criteria | ** | -/16.1 | The obesity rate was similar between matched ACHD and healthy controls. Metabolic syndrome was more common in ACHD patients than in controls (15.0% versus 7.4%). Obese ACHD patients were more likely to have metabolic syndrome than obese controls (93.1% vs. 44%). |
| Sandberg et al., 2015 [37] | 2424 (1021) | 4605 age-stratified | Fontan (97), AS (122), ToF (238), PA/DORV (81), CoA (414), VSD (497), ASD (414), AS/AR (561) | 18–50 y | - | ** | Simple: 24.0 ± 4.6 kg/m2 Complex: 22.6 ± 4.2 kg/m2 | Men with PA/DORV, AS/AR, and Fontan/TCPC had a lower prevalence of overweight/obesity (p < 0.001) than healthy controls. No differences in BMI in CoA, VSD, ASD, or AS/AR and intervention vs. no intervention. Complex lesions: age & cardiovascular medication associated with a lower BMI. Simple lesion: age, impaired NYHA class, and cardiovascular medication associated with higher BMI. |
| Malavazos et al., 2019 [31] | 1388 (776) | 145,992 sex & age-stratified | Septal heart defects & left-to-right shunt (864), conotruncal heart disease (209), valve defects & aortic defects (247), UVH (68) | 41.5 ± 13.2 | - | ** | 26.7/9.6 | Lower prevalence of overweight in ACHD (27%) and in great complexity class (16%) compared to Italian reference (32%). In great complexity class, the prevalence of obesity was significantly lower (3.1%). Men were more likely to be overweight than women in ACHD population (34.64% vs. 20.49%). Overweight/Obesity increased with age. |
| Study | Type | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pediatric CHD (n = 15) | ||||||||||||||||
| Barbour-Tuck et al., 2020 [20] | CSS | ✔ | ✔ | CD | - | - | - | - | ✔ | - | - | ✔ | - | NA | ✔ | Fair |
| Powell et al., 2020 [35] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Good |
| Yang et al., 2020 [41] | CSS | ✔ | ✔ | - | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Fair |
| Perin et al., 2019 [33] | CSS | ✔ | ✔ | ✔ | - | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Fair |
| Steele et al., 2019 [39] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | ✔ | ✔ | - | NA | ✔ | Good |
| O’Byrne et al., 2018 [32] | CSS | ✔ | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | - | ✔ | - | NA | ✔ | Fair |
| Briston et al., 2017 [21] | CSS | ✔ | ✔ | CD | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Good |
| Aguilar et al., 2015 [17] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | ✔ | ✔ | - | NA | ✔ | Good |
| Tamayo et al., 2015 [44] | CS | ✔ | ✔ | CD | ✔ | - | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | - | NA | ✔ | Good |
| Wellniz et al., 2015 [10] | CS | ✔ | ✔ | - | ✔ | - | ✔ | ✔ | - | ✔ | ✔ | ✔ | - | NR | ✔ | Fair |
| Barbiero et al., 2014 [19] | CSS | ✔ | ✔ | CD | ✔ | ✔ | - | - | - | ✔ | - | ✔ | - | NA | ✔ | Fair |
| Smith-Parrish et al., 2014 [38] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | ✔ | ✔ | - | NA | ✔ | Good |
| Welisch et al., 2013 [40] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | NA | ✔ | - | NA | ✔ | Good |
| Chen et al., 2012 [23] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Good |
| Ray et al., 2011 [36] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Fair |
| Pediatric & ACHD (n = 6) | ||||||||||||||||
| Jackson et al., 2020 [27] | CSS | ✔ | - | CD | ✔ | - | - | - | - | ✔ | NA | ✔ | - | NA | ✔ | Fair |
| Jackson et al., 2019 [28] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Good |
| Weinreb et al., 2019 [45] | CS | ✔ | ✔ | ✔ | ✔ | - | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | - | NA | ✔ | Good |
| Harris et al., 2018 [26] | CSS | ✔ | ✔ | CD | ✔ | - | - | - | ✔ | ✔ | NA | ✔ | - | NA | - | Poor |
| Chung et al., 2016 [24] | CSS | ✔ | ✔ | CD | ✔ | - | - | - | ✔ | ✔ | ✔ | ✔ | - | NA | ✔ | Good |
| Avitabile et al., 2014 [18] | CSS | ✔ | ✔ | CD | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Fair |
| ACHD (n = 9) | ||||||||||||||||
| Fedchenko et al., 2019 [25] | CSS | ✔ | ✔ | - | ✔ | - | - | - | - | ✔ | - | ✔ | - | NA | - | Poor |
| Malavazoz et al., 2019 [31] | CSS | ✔ | ✔ | CD | ✔ | - | - | - | ✔ | ✔ | NA | ✔ | - | NA | ✔ | Good |
| Zaqout et al., 2019 [42] | CSS | ✔ | ✔ | ✔ | - | - | - | - | ✔ | ✔ | - | ✔ | - | NA | - | Poor |
| Lerman et al., 2017 [29] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | NA | ✔ | - | NA | ✔ | Good |
| Lui et al., 2017 [8] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | - | Poor |
| Deen et al., 2016 [43] | CS | ✔ | ✔ | ✔ | - | - | ✔ | NA | ✔ | ✔ | NA | ✔ | - | NA | ✔ | Good |
| Sandberg et al., 2015 [37] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | ✔ | ✔ | NA | ✔ | - | NA | - | Poor |
| Buys et al., 2013 [22] | CSS | ✔ | ✔ | ✔ | ✔ | - | - | - | NA | ✔ | NA | ✔ | - | ✔ | - | Poor |
| Pike et al., 2012 [34] | CSS | ✔ | ✔ | CD | ✔ | - | - | - | ✔ | ✔ | - | ✔ | - | NA | ✔ | Good |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Willinger, L.; Brudy, L.; Meyer, M.; Oberhoffer-Fritz, R.; Ewert, P.; Müller, J. Overweight and Obesity in Patients with Congenital Heart Disease: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9931. https://doi.org/10.3390/ijerph18189931
Willinger L, Brudy L, Meyer M, Oberhoffer-Fritz R, Ewert P, Müller J. Overweight and Obesity in Patients with Congenital Heart Disease: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(18):9931. https://doi.org/10.3390/ijerph18189931
Chicago/Turabian StyleWillinger, Laura, Leon Brudy, Michael Meyer, Renate Oberhoffer-Fritz, Peter Ewert, and Jan Müller. 2021. "Overweight and Obesity in Patients with Congenital Heart Disease: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 18: 9931. https://doi.org/10.3390/ijerph18189931
APA StyleWillinger, L., Brudy, L., Meyer, M., Oberhoffer-Fritz, R., Ewert, P., & Müller, J. (2021). Overweight and Obesity in Patients with Congenital Heart Disease: A Systematic Review. International Journal of Environmental Research and Public Health, 18(18), 9931. https://doi.org/10.3390/ijerph18189931






