Hybridized Zoonotic Schistosoma Infections Result in Hybridized Morbidity Profiles: A Clinical Morbidity Study amongst Co-Infected Human Populations of Senegal
Abstract
1. Introduction
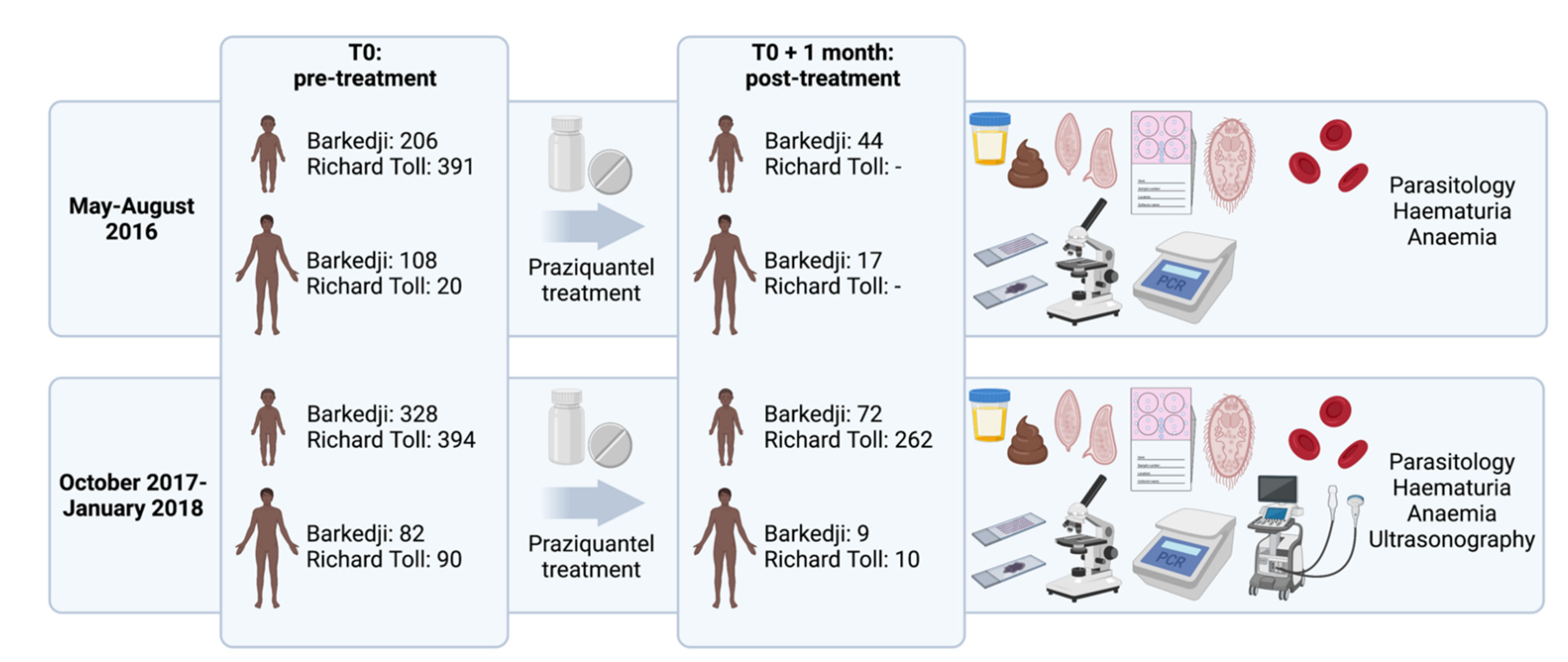
2. Materials and Methods
2.1. Study Sites and Populations
2.2. Parasitological and Molecular Procedures
2.3. Clinical Procedures
2.4. Statistical Analyses
2.5. Ethics Statement
3. Results
3.1. Prevalence of Infection and Morbidity
3.2. Impact of Single and Mixed Urogenital and Intestinal Infection on Morbidity
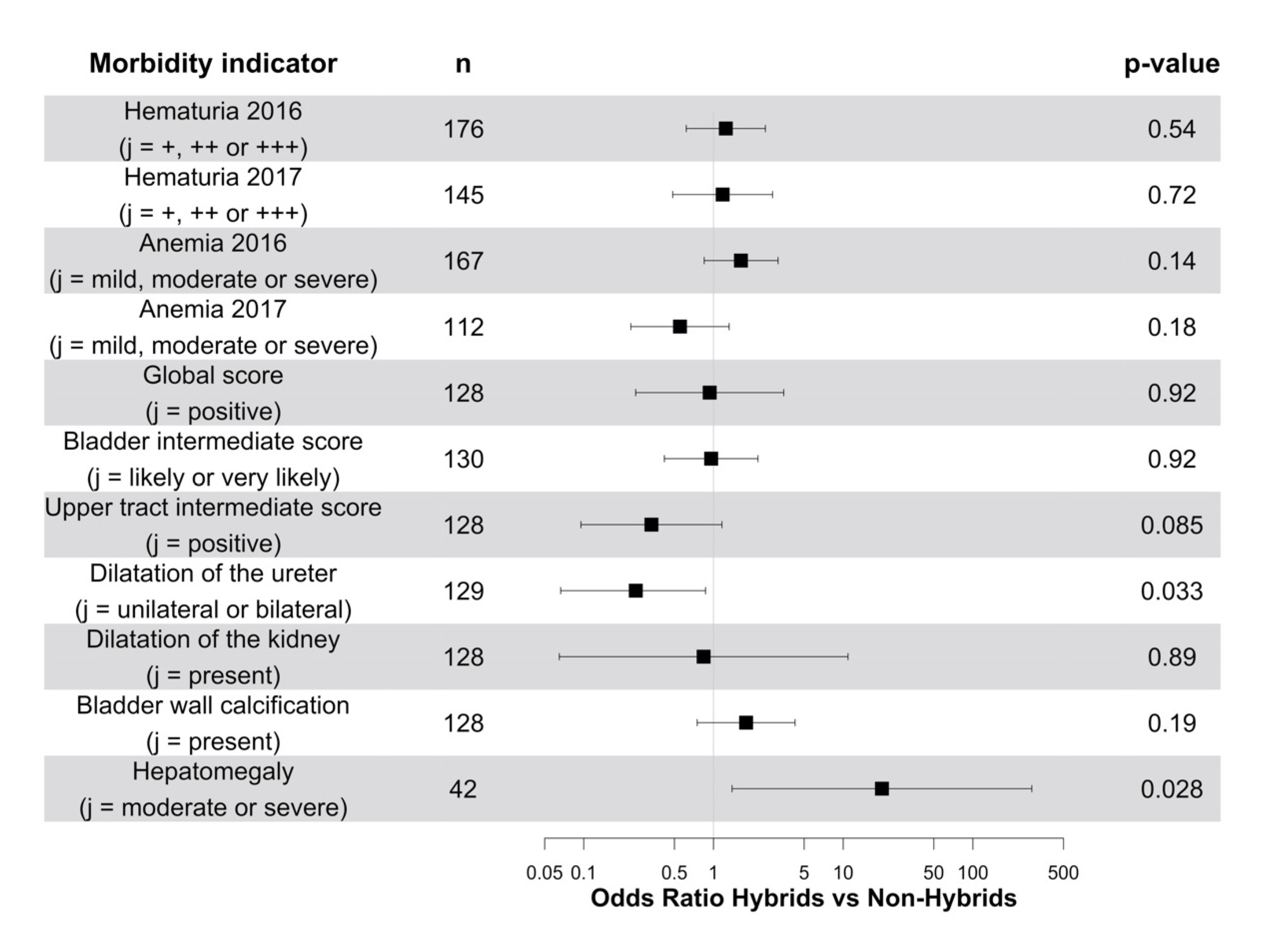
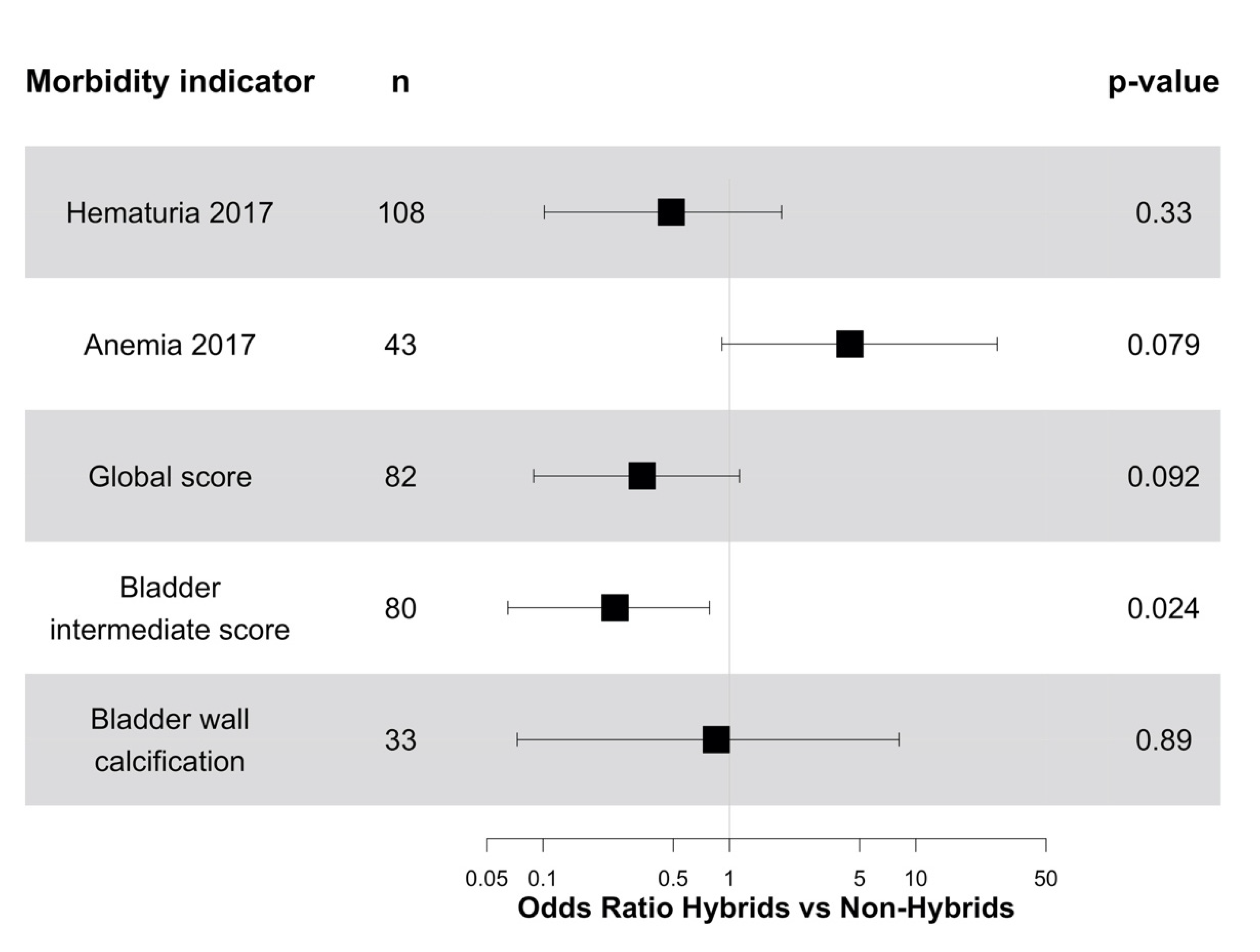
3.3. Impact of Infection by Sh-Sb Hybrids on Morbidity
3.4. Impact of Treatment on Infection and Morbidity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Petney, T.N.; Andrews, R.H. Multiparasite Communities in Animals and Humans: Frequency, Structure and Pathogenic Significance. Int. J. Parasitol. 1998, 28, 377–393. [Google Scholar] [CrossRef]
- Jones, K.E.; Patel, N.G.; Levy, M.A.; Storeygard, A.; Balk, D.; Gittleman, J.L.; Daszak, P. Global Trends in Emerging Infectious Diseases. Nature 2008, 451, 990–993. [Google Scholar] [CrossRef]
- King, K.C.; Stelkens, R.B.; Webster, J.P.; Smith, D.F.; Brockhurst, M.A. Hybridization in Parasites: Consequences for Adaptive Evolution, Pathogenesis, and Public Health in a Changing World. PLoS Pathog. 2015, 11, e1005098. [Google Scholar] [CrossRef]
- Racimo, F.; Sankararaman, S.; Nielsen, R.; Huerta-Sánchez, E. Evidence for Archaic Adaptive Introgression in Humans. Nat. Rev. Genet. 2015, 16, 359–371. [Google Scholar] [CrossRef] [PubMed]
- Mavárez, J.; Salazar, C.A.; Bermingham, E.; Salcedo, C.; Jiggins, C.D.; Linares, M. Speciation by Hybridization in Heliconius Butterflies. Nature 2006, 441, 868–871. [Google Scholar] [CrossRef] [PubMed]
- Van den Broeck, F.; Savill, N.J.; Imamura, H.; Sanders, M.; Maes, I.; Cooper, S.; Mateus, D.; Jara, M.; Adaui, V.; Arevalo, J.; et al. Ecological Divergence and Hybridization of Neotropical Leishmania Parasites. Proc. Natl. Acad. Sci. USA 2020, 117, 25159–25168. [Google Scholar] [CrossRef] [PubMed]
- Easton, A.; Gao, S.; Lawton, S.P.; Bennuru, S.; Khan, A.; Dahlstrom, E.; Oliveira, R.G.; Kepha, S.; Porcella, S.F.; Webster, J.P.; et al. Molecular Evidence of Hybridization between Pig and Human Ascaris Indicates an Interbred Species Complex Infecting Humans. Elife 2020, 9, e61562. [Google Scholar] [CrossRef]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries 1990–2010: A Systematic Analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- Van der Werf, M.J.; de Vlas, S.J.; Brooker, S.; Looman, C.W.N.; Nagelkerke, N.J.D.; Habbema, J.D.F.; Engels, D. Quantification of Clinical Morbidity Associated with Schistosome Infection in Sub-Saharan Africa. Acta Trop. 2003, 86, 125–139. [Google Scholar] [CrossRef]
- WHO. Prevention and Control of Schistosomiasis and Soil-Transmitted Helminthiasis: Report of a WHO Expert Committee; WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 2002; p. 57. [Google Scholar]
- Picquet, M.; Ernould, J.C.; Vercruysse, J.; Southgate, V.R.; Mbaye, A.; Sambou, B.; Niang, M.; Rollinson, D. The Epidemiology of Human Schistosomiasis in the Senegal River Basin. Trans. R. Soc. Trop. Med. Hyg. 1996, 90, 340–346. [Google Scholar] [CrossRef]
- Boissier, J.; Grech-Angelini, S.; Webster, B.L.; Allienne, J.-F.; Huyse, T.; Mas-Coma, S.; Toulza, E.; Barré-Cardi, H.; Rollinson, D.; Kincaid-Smith, J.; et al. Outbreak of Urogenital Schistosomiasis in Corsica (France): An Epidemiological Case Study. Lancet Infect. Dis. 2016, 16, 971–979. [Google Scholar] [CrossRef]
- Webster, J.P.; Borlase, A.; Rudge, J.W. Who Acquires Infection from Whom and How? Disentangling Multi-Host and Multi-Mode Transmission Dynamics in the ‘Elimination’ Era. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2017, 372, 20160091. [Google Scholar] [CrossRef]
- Gouvras, A.N.; Kariuki, C.; Koukounari, A.; Norton, A.J.; Lange, C.N.; Ireri, E.; Fenwick, A.; Mkoji, G.M.; Webster, J.P. The Impact of Single versus Mixed Schistosoma Haematobium and S. Mansoni Infections on Morbidity Profiles amongst School-Children in Taveta, Kenya. Acta Trop. 2013, 128, 309–317. [Google Scholar] [CrossRef]
- Meurs, L.; Mbow, M.; Vereecken, K.; Menten, J.; Mboup, S.; Polman, K. Epidemiology of Mixed Schistosoma Mansoni and Schistosoma Haematobium Infections in Northern Senegal. Int. J. Parasitol. 2012, 42, 305–311. [Google Scholar] [CrossRef]
- Koukounari, A.; Donnelly, C.A.; Sacko, M.; Keita, A.D.; Landouré, A.; Dembelé, R.; Bosqué-Oliva, E.; Gabrielli, A.F.; Gouvras, A.; Traoré, M.; et al. The Impact of Single versus Mixed Schistosome Species Infections on Liver, Spleen and Bladder Morbidity within Malian Children Pre- and Post-Praziquantel Treatment. BMC Infect. Dis. 2010, 10, 227. [Google Scholar] [CrossRef] [PubMed]
- Cunin, P.; Tchuenté, L.-A.T.; Poste, B.; Djibrilla, K.; Martin, P.M.V. Interactions between Schistosoma Haematobium and Schistosoma Mansoni in Humans in North Cameroon. Trop. Med. Int. Health 2003, 8, 1110–1117. [Google Scholar] [CrossRef]
- Knowles, S.C.L.; Webster, B.L.; Garba, A.; Sacko, M.; Diaw, O.T.; Fenwick, A.; Rollinson, D.; Webster, J.P. Epidemiological Interactions between Urogenital and Intestinal Human Schistosomiasis in the Context of Praziquantel Treatment across Three West African Countries. PLoS Negl. Trop. Dis. 2015, 9, e0004019. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wu, X.; Li, X.; Zheng, X.; Wang, F.; Qi, Z.; Huang, M.; Zou, Y. Imported Schistosomiasis: A New Public Health Challenge for China. Front. Med. 2020, 7, 553487. [Google Scholar] [CrossRef] [PubMed]
- Le Govic, Y.; Kincaid-Smith, J.; Allienne, J.-F.; Rey, O.; de Gentile, L.; Boissier, J. Schistosoma Haematobium–Schistosoma Mansoni Hybrid Parasite in Migrant Boy, France, 2017. Emerg. Infect. Dis. 2019, 25, 365–367. [Google Scholar] [CrossRef] [PubMed]
- Beltrame, A.; Buonfrate, D.; Gobbi, F.; Angheben, A.; Marchese, V.; Monteiro, G.B.; Bisoffi, Z. The Hidden Epidemic of Schistosomiasis in Recent African Immigrants and Asylum Seekers to Italy. Eur. J. Epidemiol. 2017, 32, 733–735. [Google Scholar] [CrossRef]
- Lingscheid, T.; Kurth, F.; Clerinx, J.; Marocco, S.; Trevino, B.; Schunk, M.; Muñoz, J.; Gjørup, I.E.; Jelinek, T.; Develoux, M.; et al. Schistosomiasis in European Travelers and Migrants: Analysis of 14 Years TropNet Surveillance Data. Am. J. Trop. Med. Hyg. 2017, 97, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Léger, E.; Borlase, A.; Fall, C.B.; Diouf, N.D.; Diop, S.D.; Yasenev, L.; Catalano, S.; Thiam, C.T.; Ndiaye, A.; Emery, A.; et al. Prevalence and Distribution of Schistosomiasis in Human, Livestock, and Snail Populations in Northern Senegal: A One Health Epidemiological Study of a Multi-Host System. Lancet Planet. Health 2020, 4, e330–e342. [Google Scholar] [CrossRef]
- Léger, E.; Webster, J.P. Hybridizations within the Genus Schistosoma: Implications for Evolution, Epidemiology and Control. Parasitology 2017, 144, 65–80. [Google Scholar] [CrossRef] [PubMed]
- Huyse, T.; Webster, B.L.; Geldof, S.; Stothard, J.R.; Diaw, O.T.; Polman, K.; Rollinson, D. Bidirectional Introgressive Hybridization between a Cattle and Human Schistosome Species. PLoS Pathog. 2009, 5, e1000571. [Google Scholar] [CrossRef]
- Boon, N.A.M.; Van Den Broeck, F.; Faye, D.; Volckaert, F.A.M.; Mboup, S.; Polman, K.; Huyse, T. Barcoding Hybrids: Heterogeneous Distribution of Schistosoma Haematobium × Schistosoma Bovis Hybrids across the Senegal River Basin. Parasitology 2018, 145, 634–645. [Google Scholar] [CrossRef]
- Webster, B.L.; Diaw, O.T.; Seye, M.M.; Webster, J.P.; Rollinson, D. Introgressive Hybridization of Schistosoma Haematobium Group Species in Senegal: Species Barrier Break down between Ruminant and Human Schistosomes. PLoS Negl. Trop. Dis. 2013, 7, e2110. [Google Scholar] [CrossRef]
- Stothard, J.R.; Kayuni, S.A.; Al-Harbi, M.H.; Musaya, J.; Webster, B.L. Future Schistosome Hybridizations: Will All Schistosoma Haematobium Hybrids Please Stand-Up! PLoS Negl. Trop. Dis. 2020, 14, e0008201. [Google Scholar] [CrossRef]
- Boissier, J.; Moné, H.; Mitta, G.; Bargues, M.D.; Molyneux, D.; Mas-Coma, S. Schistosomiasis Reaches Europe. Lancet Infect. Dis. 2015, 15, 757–758. [Google Scholar] [CrossRef]
- Gaye, A.M.; Doh, K.; Thiam, I.; Bentefouet, L.; Woto-Gaye, G. Bilharziose et cancer: Une association fortuite ou une relation de cause à effet [Schistosomiasis and cancer: A fortuitous association or relationships cause and effect]. Bull. Cancer 2016, 103, 806–807. [Google Scholar] [CrossRef]
- Colley, D.G.; Bustinduy, A.L.; Secor, W.E.; King, C.H. Human Schistosomiasis. Lancet 2014, 383, 2253–2264. [Google Scholar] [CrossRef]
- Webster, B.L.; Southgate, V.R.; Tchuenté, L.-A.T. Mating Interactions between Schistosoma Haematobium and S. Mansoni. J. Helminthol. 1999, 73, 351–356. [Google Scholar] [CrossRef]
- Wright, C.A.; Ross, G.C. Hybrids between Schistosoma Haematobium and S. Mattheei and Their Identification by Isoelectric Focusing of Enzymes. Trans. R. Soc. Trop. Med. Hyg. 1980, 74, 326–332. [Google Scholar] [CrossRef]
- WHO. Ending the Neglect to Attain the Sustainable Development Goals—A Road Map for Neglected Tropical Diseases 2021–2030; World Health Organization: Geneva, Switzerland, 2020; p. 55. [Google Scholar]
- Rey, O.; Webster, B.L.; Huyse, T.; Rollinson, D.; Van den Broeck, F.; Kincaid-Smith, J.; Onyekwere, A.; Boissier, J. Population Genetics of African Schistosoma Species. Infect. Genet. Evol. 2021, 89, 104727. [Google Scholar] [CrossRef] [PubMed]
- Webster, B.L.; Alharbi, M.H.; Kayuni, S.; Makaula, P.; Halstead, F.; Christiansen, R.; Juziwelo, L.; Stanton, M.C.; LaCourse, E.J.; Rollinson, D.; et al. Schistosome Interactions within the Schistosoma Haematobium Group, Malawi. Emerg. Infect. Dis. 2019, 25, 1245–1247. [Google Scholar] [CrossRef]
- Rey, O.; Toulza, E.; Chaparro, C.; Allienne, J.-F.; Kincaid-Smith, J.; Mathieu-Begné, E.; Allan, F.; Rollinson, D.; Webster, B.L.; Boissier, J. Diverging Patterns of Introgression from Schistosoma Bovis across S. Haematobium African Lineages. PLOS Pathog. 2021, 17, e1009313. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.L. Natural Hybridization and the Evolution of Domesticated, Pest and Disease Organisms. Mol. Ecol. 2004, 13, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- French, M.D.; Churcher, T.S.; Basáñez, M.-G.; Norton, A.J.; Lwambo, N.J.S.; Webster, J.P. Reductions in Genetic Diversity of Schistosoma Mansoni Populations under Chemotherapeutic Pressure: The Effect of Sampling Approach and Parasite Population Definition. Acta Trop. 2013, 128, 196–205. [Google Scholar] [CrossRef]
- WHO. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Available online: http://www.who.int/vmnis/indicators/haemoglobin/en/ (accessed on 6 February 2020).
- WHO. Ultrasound in Schistosomiasis: A Practical Guide to the Standard Use of Ultrasonography for Assessment of Schistosomiasis-Related Morbidity; UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases; World Health Organization: Niamey, Niger, 1996; p. 55. [Google Scholar]
- Richter, J.; Domingues, A.L.D.; Barata, C.H.; Prata, A.R.; Lambertucci, J.R. Report of the Second Satellite Symposium on Ultrasound in Schistosomiasis. Mem. Inst. Oswaldo Cruz 2001, 96, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Montresor, A.; Crompton, D.W.T.; Hall, A.; Bundy, D.A.P.; Savioli, L. Guidelines for the Evaluation of Soil-Transmitted Helminthiasis and Schistosomiasis at Community Level: A Guide for Managers of Control Programmes; Technical Documents; World Health Organization: Geneva, Switzerland, 1998; p. 45. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Christensen, R.H.B. Ordinal-Regression Models for Ordinal Data; R Package Version 2019.12-10. 2019. Available online: https://cran.r-project.org/web/packages/ordinal/index.html (accessed on 3 June 2020).
- Christensen, R.H.B. Cumulative Link Models for Ordinal Regression with the R Package Ordinal. Available online: https://cran.r-project.org/web/packages/ordinal/vignettes/clm_article.pdf (accessed on 3 June 2020).
- WHO. WHO Assessing the Efficacy of Anthelminthic Drugs against Schistosomiasis and Soil-Transmitted Helminthiases; World Health Organization: Geneva, Switzerland, 2013; ISBN 978-92-4-156455-7. [Google Scholar]
- Meurs, L.; Mbow, M.; Vereecken, K.; Menten, J.; Mboup, S.; Polman, K. Bladder Morbidity and Hepatic Fibrosis in Mixed Schistosoma Haematobium and S. Mansoni Infections: A Population-Wide Study in Northern Senegal. PLoS Negl. Trop. Dis. 2012, 6, e1829. [Google Scholar] [CrossRef] [PubMed]
- Garba, A.; Pion, S.; Cournil, A.; Milet, J.; Schneider, D.; Campagne, G.; Chippaux, J.-P.; Boulanger, D. Risk Factors for Schistosoma Haematobium Infection and Morbidity in Two Villages with Different Transmission Patterns in Niger. Acta Trop. 2010, 115, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Koukounari, A.; Gabrielli, A.F.; Toure, S.; Bosque-Oliva, E.; Zhang, Y.; Sellin, B.; Donnelly, C.A.; Fenwick, A.; Webster, J.P. Schistosoma Haematobium Infection and Morbidity before and after Large-Scale Administration of Praziquantel in Burkina Faso. J. Infect. Dis. 2007, 196, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Koukounari, A.; Sacko, M.; Keita, A.D.; Gabrielli, A.F.; Landouré, A.; Dembelé, R.; Clements, A.C.; Whawell, S.; Donnelly, C.A.; Fenwick, A.; et al. Assessment of Ultrasound Morbidity Indicators of Schistosomiasis in the Context of Large-Scale Programs Illustrated with Experiences from Malian Children. Am. J. Trop. Med. Hyg. 2006, 75, 1042–1052. [Google Scholar] [CrossRef] [PubMed]
- Delegue, P.; Picquet, M.; Shaw, D.J.; Vercruysse, J.; Sambou, B.; Ly, A. Morbidity Induced by Schistosoma Haematobium Infections, as Assessed by Ultrasound before and after Treatment with Praziquantel, in a Recently Expanded Focus (Senegal River Basin). Ann. Trop. Med. Parasitol. 1998, 92, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Sarr, S.A.; Camara, R.; Hicham, F.-F.; Fall, C.B.; Sylla, I.S.; Aw, F.; Bodian, M.; Ndiaye, M.B.; Mbaye, A.; Kane, A.; et al. Characteristics of the Heart of School-Age Children in a Schistosomiasis Endemic Area in Senegal. World J. Cardiovasc. Dis. 2018, 8, 441–451. [Google Scholar] [CrossRef][Green Version]
- Lô, G.; Sow-Sall, A.; Diop-Ndiaye, H.; Babacar, N.; Diouf, N.N.; Daffé, S.M.; Ndao, B.; Thiam, M.; Mbow, M.; Soumboundou, M.B.; et al. Hepatitis B Virus (HBV) Infection amongst Children in Senegal: Current Prevalence and Seroprotection Level. Pan Afr. Med. J. 2019, 32, 140. [Google Scholar] [CrossRef]
- Thiam, L.; Dramé, A.; Coly, I.Z.; Diouf, F.N.; Seck, N.; Boiro, D.; Ndongo, A.A.; Basse, I.; Niang, N.; Deme/Ly, I.; et al. Profils épidemiologiques, cliniques et hématologiques de la drépanocytose homozygote SS en phase inter critique chez l’enfant à Ziguinchor, Sénégal. Pan Afr. Med. J. 2017, 28, 208. [Google Scholar] [CrossRef]
- Cellule de Lutte Contre la Malnutrition. Plan Stratégique Multisectoriel de la Nutrition du Sénégal, 2017-2021; Global Database on the Implementation of Nutrition Action (GINA); WHO: Geneva, Switzerland, 2017; p. 116. [Google Scholar]
- Platt, R.N.; McDew-White, M.; Le Clec’h, W.; Chevalier, F.D.; Allan, F.; Emery, A.M.; Garba, A.; Hamidou, A.A.; Ame, S.M.; Webster, J.P.; et al. Ancient Hybridization and Adaptive Introgression of an Invadolysin Gene in Schistosome Parasites. Mol. Biol. Evol. 2019, 36, 2127–2142. [Google Scholar] [CrossRef]
| Year | Morbidity Indicator | Children | Adults | ||
|---|---|---|---|---|---|
| Barkedji | Richard Toll | Barkedji | Richard Toll | ||
| 2016 | Hematuria | 34% (n = 203) | 62% (n = 376) | 40% (n = 105) | 75% (n = 20) |
| Anemia | 43% (n = 148) | 51% (n = 382) | 36% (n = 45) | - | |
| Total examined 1 | N = 203 | N = 391 | N = 108 | N = 20 | |
| 2017 | Hematuria | 28% (n = 326) | 73% (n = 368) | 40% (n = 80) | 39% (n = 82) |
| Anemia | - | 54% (n = 374) | - | 74% (n = 43) | |
| Global score 2 | 25% (n = 297) | 65% (n = 335) | 32% (n = 19) | 41% (n = 41) | |
| Bladder intermediate score | 21% (n = 303) | 48% (n = 335) | 16% (n = 19) | 15% (n = 41) | |
| Upper tract intermediate score | 5% (n = 297) | 15% (n = 335) | 0% (n = 19) | 2% (n = 41) | |
| Bladder wall calcification | 6% (n = 297) | 27% (n = 335) | 0% (n = 19) | 20% (n = 41) | |
| Hepatomegaly | 69% (n = 109) | 89% (n = 99) | 0% (n = 2) | 100% (n = 12) | |
| Abnormal size of the right liver lobe | 0.7% (n = 144) | 2.3% (n = 222) | 50% (n = 2) | 0% (n = 44) | |
| Dilatation of the portal vein | 0% (n = 147) | 0% (n = 220) | 0% (n = 2) | 0% (n = 46) | |
| Splenomegaly | 0.8% (n = 128) | 1.5% (n = 201) | 0% (n = 2) | 0% (n = 3) | |
| Total examined 1 | N = 328 | N = 391 | N = 80 | N = 86 | |
| Hematuria 2016 | ||||
|---|---|---|---|---|
| Sh and Sh-Sb Urogenital Infection Intensity | ||||
| None | Light | Heavy | ||
| Sm intestinal infection intensity | None | 1 | 7.19 [5.14–10.1] (p < 0.0001) | 51.7 [26.4–101] (p < 0.0001) |
| Light | 1.05 [0.46–2.39] (p = 0.91) | 8.62 [5.09–14.6] (p < 0.0001) | 70.8 [29.0–173] (p < 0.0001) | |
| Moderate | 1.10 [0.21–5.73] (p = 0.91) | 10.3 [4.30–24.9] (p < 0.0001) | 97.1 [22.0–429] (p < 0.0001) | |
| Heavy | 1.16 [0.10–13.7] (p = 0.91) | 12.4 [3.51–43.8] (p < 0.0001) | 133 [15.3–1159] (p < 0.0001) | |
| Hematuria 2017 | ||||
| Sh and Sh-Sb urogenital infection intensity | ||||
| None | Light | Heavy | ||
| Sm intestinal infection intensity | None | 1 | 6.37 [4.33–9.39] (p < 0.0001) | 40.6 [18.7–88.2] (p < 0.0001) |
| Light | 1.31 [0.53–3.24] (p = 0.56) | 5.78 [3.37–9.89] (p < 0.0001) | 25.5 [9.73–66.6] (p < 0.0001) | |
| Moderate | 1.72 [0.28–10.5] (p = 0.56) | 5.24 [2.18–12.6] (p = 0.00021) | 15.9 [3.13–81.3] (p = 0.00086) | |
| Heavy | 2.26 [0.15–34.1] (p = 0.56) | 4.75 [1.35–16.7] (p = 0.015) | 9.99 [0.90–111] (p = 0.061) | |
| Global Score (j = Positive) 1 | ||||
|---|---|---|---|---|
| Sh and Sh-Sb Urogenital Infection Intensity | ||||
| None | Light | Heavy | ||
| Sm intestinal infection intensity | None | 1 | 6.25 [3.76–10.4] (p < 0.0001) | 39.0 [14.1–108] (p < 0.0001) |
| Light | 0.57 [0.10–3.22] (p = 0.52) | 5.96 [2.87–12.4] (p < 0.0001) | 62.8 [9.18–430] (p < 0.0001) | |
| Moderate | 0.32 [0.01–10.4] (p = 0.52) | 5.69 [1.68–19.3] (p = 0.0053) | 101 [2.73–3,743] (p = 0.012) | |
| Heavy | 0.18 [0.001–33.3] (p = 0.52) | 5.44 [0.92–31.9] (p = 0.061) | 163 [0.74–35,730] (p = 0.064) | |
| Bladder Intermediate Score (j = likely or very likely) | ||||
| Sh and Sh-Sb urogenital infection intensity | ||||
| None | Light | Heavy | ||
| Sm intestinal infection intensity | None | 1 | 4.61 [3.04–6.98] (p < 0.0001) | 21.2 [9.23–48.8] (p < 0.0001) |
| Light | 0.50 [0.12–2.08] (p = 0.34) | 6.37 [3.36–12.1] (p < 0.0001) | 80.5 [20.3–319] (p < 0.0001) | |
| Moderate | 0.25 [0.01–4.32] (p = 0.34) | 8.81 [3.07–25.3] (p < 0.0001) | 306 [25.2–3,703] (p < 0.0001) | |
| Heavy | 0.13 [0.002–8.99] (p = 0.34) | 12.2 [2.69–55.2] (p = 0.0012) | 1160 [28.8–46,760] (p = 0.00018) | |
| Upper Tract Intermediate Score (j = positive) | ||||
| Sh and Sh-Sb urogenital infection intensity | ||||
| None | Light | Heavy | ||
| Sm intestinal infection intensity | None | 1 | 1.70 [1.03–2.80] (p = 0.039) | 2.88 [1.06–7.85] (p = 0.039) |
| Light | 0.80 [0.17–3.67] (p = 0.77) | 1.54 [0.69–3.42] (p = 0.29) | 2.96 [0.82–10.7] (p = 0.098) | |
| Moderate | 0.63 [0.03–13.5] (p = 0.77) | 1.39 [0.36–5.37] (p = 0.63) | 3.04 [0.34–26.9] (p = 0.32) | |
| Heavy | 0.51 [0.005–49.4] (p = 0.77) | 1.26 [0.18–8.85] (p = 0.82) | 3.12 [0.13–77.5] (p = 0.49) | |
| Bladder Wall Calcification (j = present) | ||||
| Sh and Sh-Sb urogenital infection intensity | ||||
| None | Light | Heavy | ||
| Sm intestinal infection intensity | None | 1 | 2.47 [1.49–4.09] (p = 0.00045) | 6.10 [2.22–16.7] (p = 0.00045) |
| Light | 0.22 [0.04–1.21] (p = 0.082) | 1.77 [0.79–3.99] (p = 0.17) | 14.2 [3.67–55.1] (p = 0.00012) | |
| Moderate | 0.05 [0.002–1.46] (p = 0.082) | 1.27 [0.33–4.97] (p = 0.73) | 33.2 [3.11–355] (p = 0.0038) | |
| Heavy | 0.01 [0.0001–1.76] (p = 0.082) | 0.91 [0.13–6.49] (p = 0.93) | 77.5 [2.31–2,600] (p = 0.015) | |
| Year | Praziquantel Efficacy | Children | Adults | ||
|---|---|---|---|---|---|
| Barkedji | Richard Toll | Barkedji | Richard Toll | ||
| 2016 | Cure rate | 81% (n = 42) | - | 81% (n = 16) | - |
| Egg reduction rate | 97.8% | - | 100% | - | |
| 2017 | Cure rate | 77% (n = 71) | 79% (n = 258) | 62% (n = 8) | 78% (n = 9) |
| Egg reduction rate | 98.2% | 99.5% | 99.1% | 95.1% | |
| Year | Morbidity Indicator | Children | Adults | ||
|---|---|---|---|---|---|
| Barkedji | Richard Toll | Barkedji | Richard Toll | ||
| 2016 | Hematuria | 77% (n = 35) | - | 71% (n = 14) | - |
| Anemia | - | - | - | - | |
| 2017 | Hematuria | 89% (n = 44) | 84% (n = 195) | 86% (n = 7) | 50% (n = 4) |
| Anemia | - | 51% (n = 106) | - | - | |
| Global score 1 | 63% (n = 19) | 69% (n = 166) | 100% (n = 1) | 75% (n = 4) | |
| Bladder intermediate score | 45% (n = 22) | 66% (n = 155) | 100% (n = 1) | 100% (n = 3) | |
| Upper tract intermediate score | 100% (n = 5) | 87% (n = 39) | 0% (n = 1) | 0% (n = 4) | |
| Bladder wall calcification | 100% (n = 6) | 59% (n = 68) | - | 100% (n = 2) | |
| Hepatomegaly | - | - | - | - | |
| Morbidity Indicator | n | Type of Infection | |||
|---|---|---|---|---|---|
| Hematuria 2017 | 167 | Sh and Sh-Sb urogenital infection intensity | |||
| Light | Heavy | ||||
| 0.76 [0.31–2.27] (p = 0.72) | 0.57 [0.09–5.17] (p = 0.72) | ||||
| Sm intestinal infection intensity | |||||
| Light | Moderate | Heavy | |||
| 1.29 [0.56–3.28] (p = 0.51) | 1.67 [0.31–10.8] (p = 0.51) | 2.17 [0.17–35.4] (p = 0.51) | |||
| Anemia 2017 | 78 | Sh and Sh-Sb urogenital infection intensity | |||
| Light | Heavy | ||||
| 1.50 [0.45–3.15] (p = 0.73) | 2.25 [0.20–9.92] (p = 0.73) | ||||
| Sm intestinal infection intensity | |||||
| Light | Moderate | Heavy | |||
| 1.44 [0.76–2.98] (p = 0.24) | 2.09 [0.58–8.87] (p = 0.24) | 3.01 [0.44–26.4] (p = 0.24) | |||
| Global score 1 | 125 | Sh and Sh-Sb urogenital infection intensity | |||
| Light | Heavy | ||||
| 3.82 [1.32–11.1] (p = 0.014) | 14.6 [1.74–122] (p = 0.014) | ||||
| Sm intestinal infection intensity | |||||
| Light | Moderate | Heavy | |||
| 1.72 [0.76–3.89] (p = 0.19) | 2.97 [0.58–15.1] (p = 0.19) | 5.13 [0.45–58.9] (p = 0.19) | |||
| Bladder intermediate score | 119 | Sh and Sh-Sb urogenital infection intensity | |||
| Light | Heavy | ||||
| 3.80 [1.31–11.0] (p = 0.014) | 14.5 [1.72–121] (p = 0.014) | ||||
| Sm intestinal infection intensity | |||||
| Light | Moderate | Heavy | |||
| 1.57 [0.73–3.40] (p = 0.25) | 2.46 [0.53–11.5] (p = 0.25) | 3.87 [0.38–39.1] (p = 0.25) | |||
| Bladder wall calcification | 46 | Sh and Sh-Sb urogenital infection intensity | |||
| Light | Heavy | ||||
| 1.38 [0.44–4.75] (p = 0.59) | 1.91 [0.19–22.6] (p = 0.59) | ||||
| Sm intestinal infection intensity | |||||
| Light | Moderate | Heavy | |||
| 1.29 [0.53–4.14] (p = 0.60) | 1.67 [0.29–17.2] (p = 0.60) | 2.16 [0.15–71.] (p = 0.60) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fall, C.B.; Lambert, S.; Léger, E.; Yasenev, L.; Garba, A.D.; Diop, S.D.; Borlase, A.; Catalano, S.; Faye, B.; Walker, M.; et al. Hybridized Zoonotic Schistosoma Infections Result in Hybridized Morbidity Profiles: A Clinical Morbidity Study amongst Co-Infected Human Populations of Senegal. Microorganisms 2021, 9, 1776. https://doi.org/10.3390/microorganisms9081776
Fall CB, Lambert S, Léger E, Yasenev L, Garba AD, Diop SD, Borlase A, Catalano S, Faye B, Walker M, et al. Hybridized Zoonotic Schistosoma Infections Result in Hybridized Morbidity Profiles: A Clinical Morbidity Study amongst Co-Infected Human Populations of Senegal. Microorganisms. 2021; 9(8):1776. https://doi.org/10.3390/microorganisms9081776
Chicago/Turabian StyleFall, Cheikh B., Sébastien Lambert, Elsa Léger, Lucy Yasenev, Amadou Djirmay Garba, Samba D. Diop, Anna Borlase, Stefano Catalano, Babacar Faye, Martin Walker, and et al. 2021. "Hybridized Zoonotic Schistosoma Infections Result in Hybridized Morbidity Profiles: A Clinical Morbidity Study amongst Co-Infected Human Populations of Senegal" Microorganisms 9, no. 8: 1776. https://doi.org/10.3390/microorganisms9081776
APA StyleFall, C. B., Lambert, S., Léger, E., Yasenev, L., Garba, A. D., Diop, S. D., Borlase, A., Catalano, S., Faye, B., Walker, M., Sene, M., & Webster, J. P. (2021). Hybridized Zoonotic Schistosoma Infections Result in Hybridized Morbidity Profiles: A Clinical Morbidity Study amongst Co-Infected Human Populations of Senegal. Microorganisms, 9(8), 1776. https://doi.org/10.3390/microorganisms9081776






