Medical Applications of Nonadditive Entropies †
Abstract
1. Introduction
2. Medical Applications
2.1. Image Processing
2.2. Signal Processing
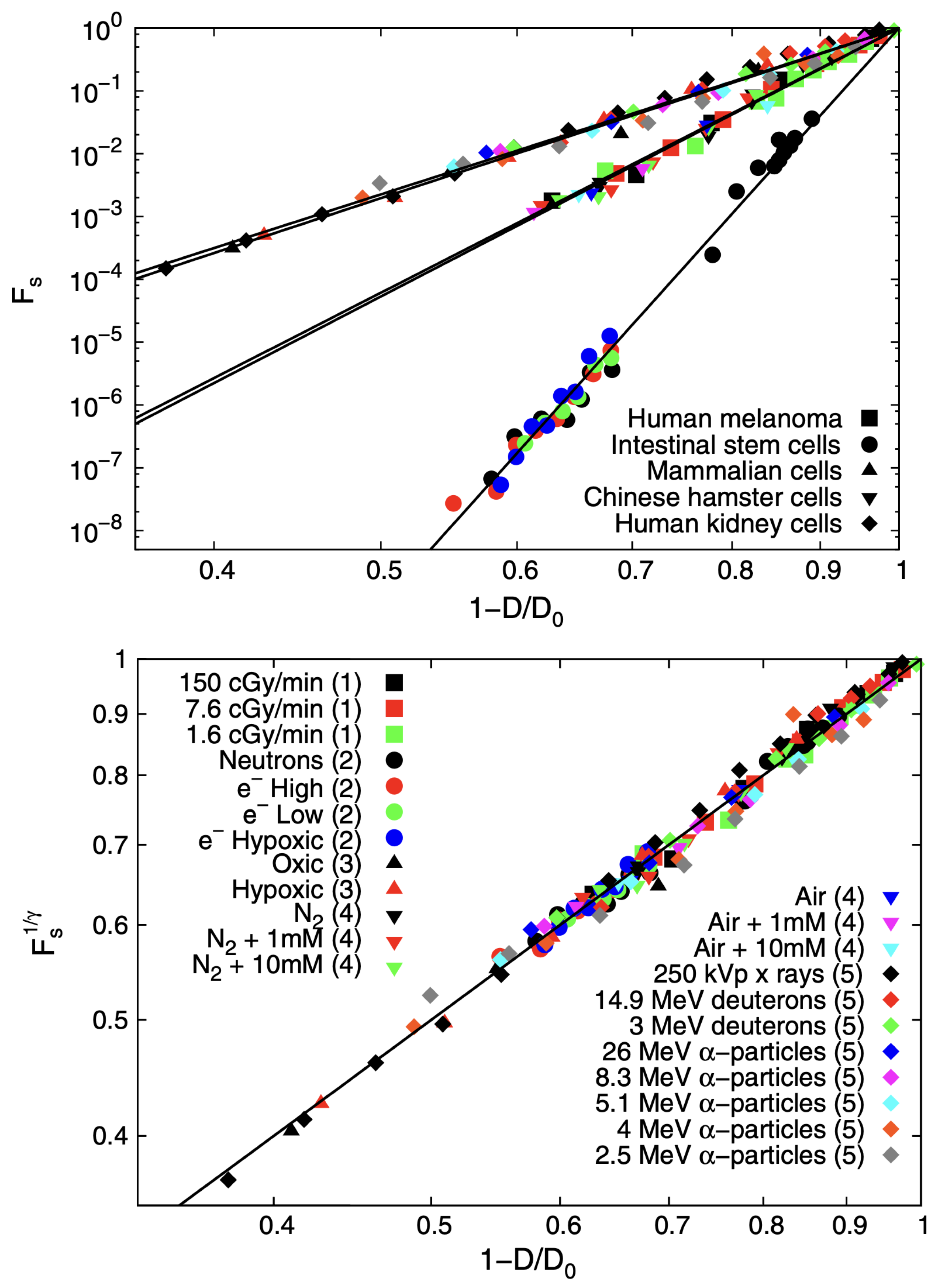
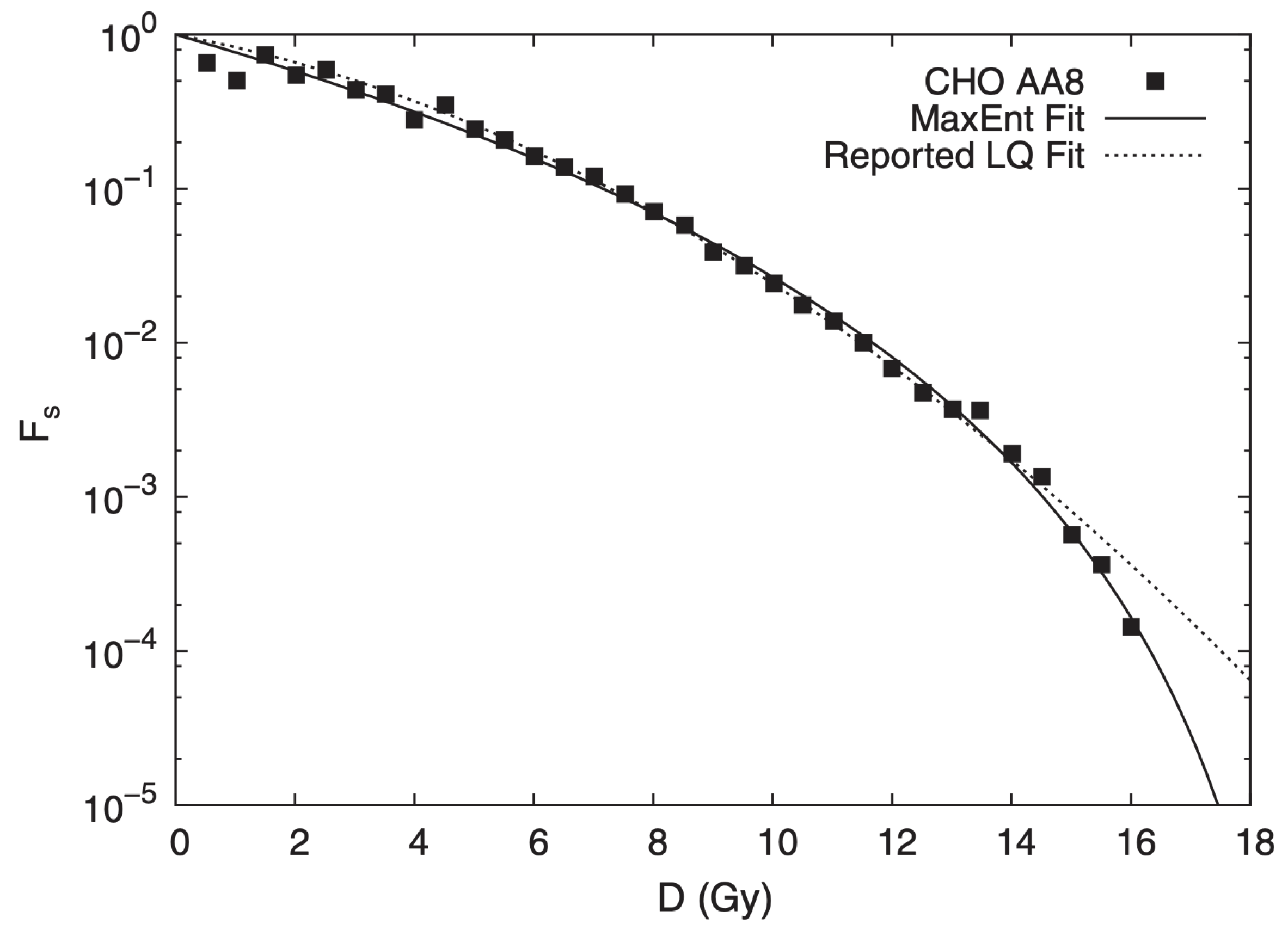
2.3. Tissue Radiation Response
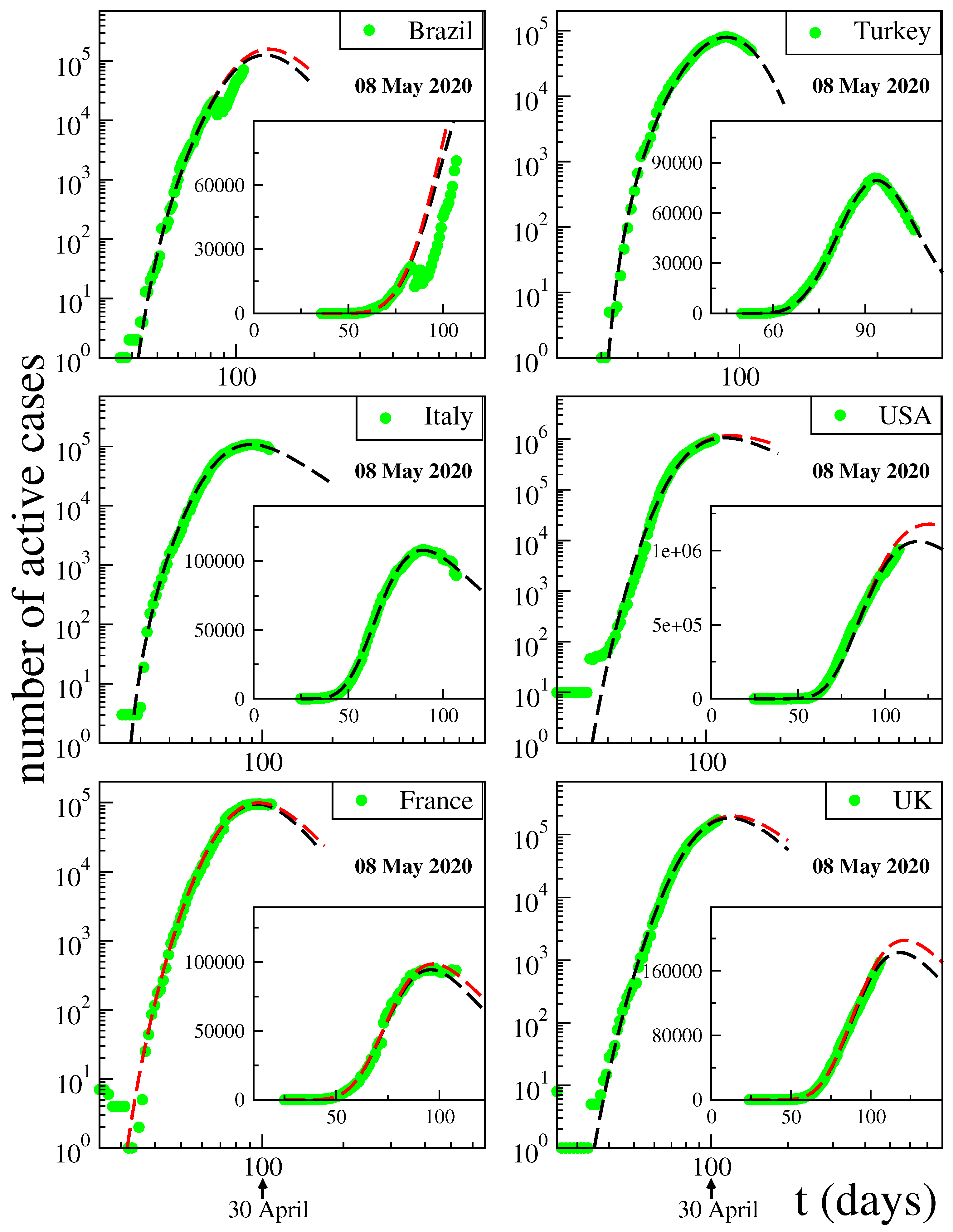
3. Modeling of Disease Kinetics
4. Final Remarks
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tsallis, C. Entropy. Encyclopedia 2022, 2, 264–300. [Google Scholar] [CrossRef]
- Tsallis, C. Possible generalization of Boltzmann-Gibbs statistics. J. Stat. Phys. 1988, 52, 479–487. [Google Scholar] [CrossRef]
- Penrose, O. Foundations of Statistical Mechanics: A Deductive Treatment; Pergamon: Oxford, UK, 1970; p. 167. [Google Scholar]
- Gell-Mann, M.; Tsallis, C. (Eds.) Nonextensive Entropy—Interdisciplinary Applications; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Tsallis, C. Nonextensive Statistical Mechanics—Approaching a Complex World, 1st ed.; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Regularly Updated Bibliography. Available online: http://tsallis.cat.cbpf.br/biblio.htm (accessed on 23 March 2023).
- Pendrill, L.; Espinoza, A.; Wadman, J.; Nilsask, F.; Wretborn, J.; Ekelund, U.; Pahlm, U. Reducing search times and entropy in hospital emergency departments with real-time location systems. IISE Trans. Healthc. Syst. Eng. 2021, 11, 305–315. [Google Scholar] [CrossRef]
- Melin, J.; Cano, S.J.; Floel, A.; Goschel, L.; Pendrill, L.R. The role of entropy in construct specification equations (CSE) to improve the validity of memory tests: Extension to word lists. Entropy 2022, 24, 934. [Google Scholar] [CrossRef] [PubMed]
- Dakhale, B.J.; Sharma, M.; Arif, M.; Asthana, K.; Bhurane, A.A.; Kothari, A.G.; Acharya, U.R. An automatic sleep-scoring system in elderly women with osteoporosis fractures using frequency localized finite orthogonal quadrature Fejer Korovkin kernels. Med. Eng. Phys. 2023, 112, 103956. [Google Scholar] [CrossRef]
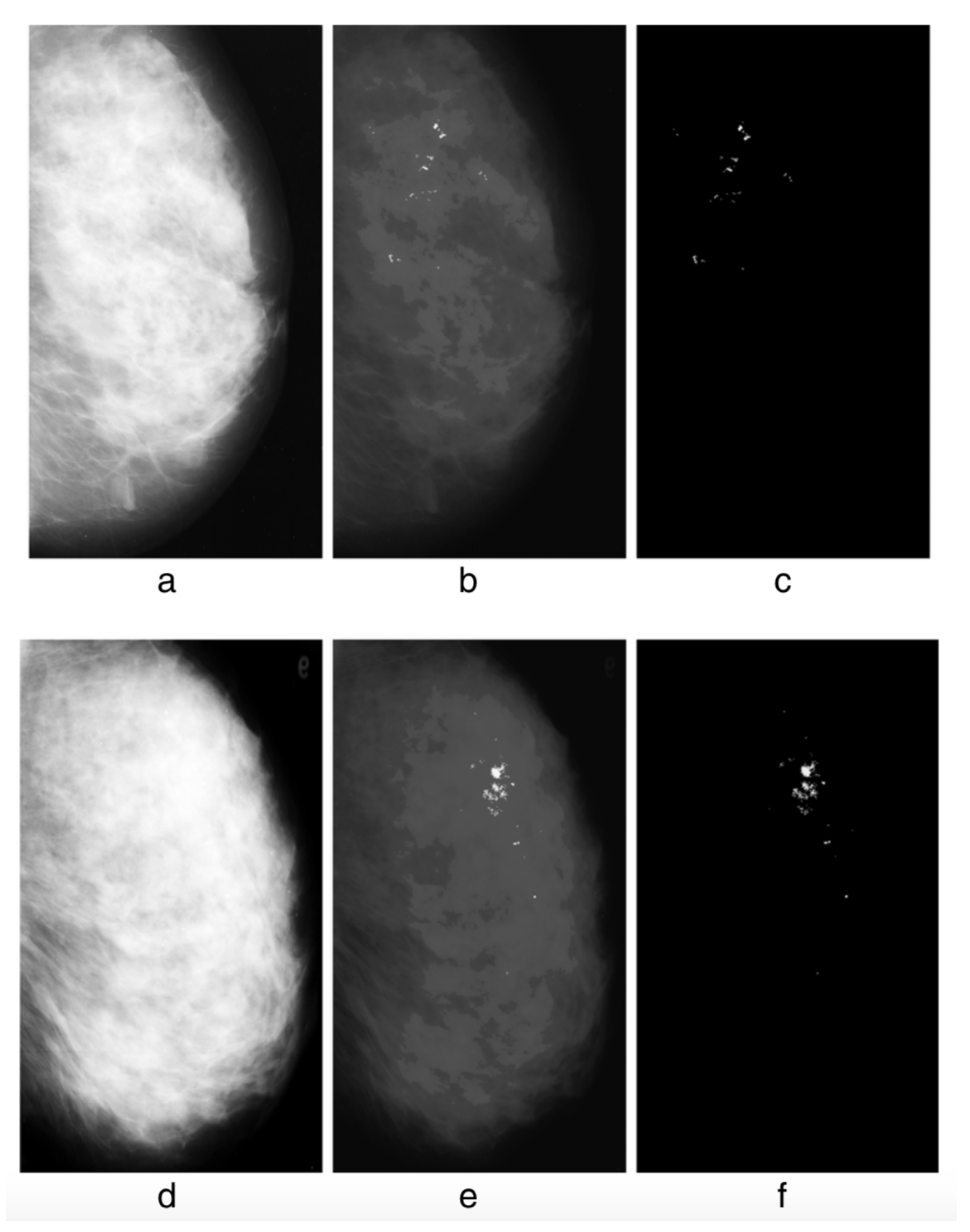
- Mohanalin, J.; Beenamol, M.; Kalra, P.K.; Kumar, N. A novel automatic microcalcification detection technique using Tsallis entropy and a type II fuzzy index. Comput. Math. Appl. 2010, 60, 2426–2432. [Google Scholar] [CrossRef]
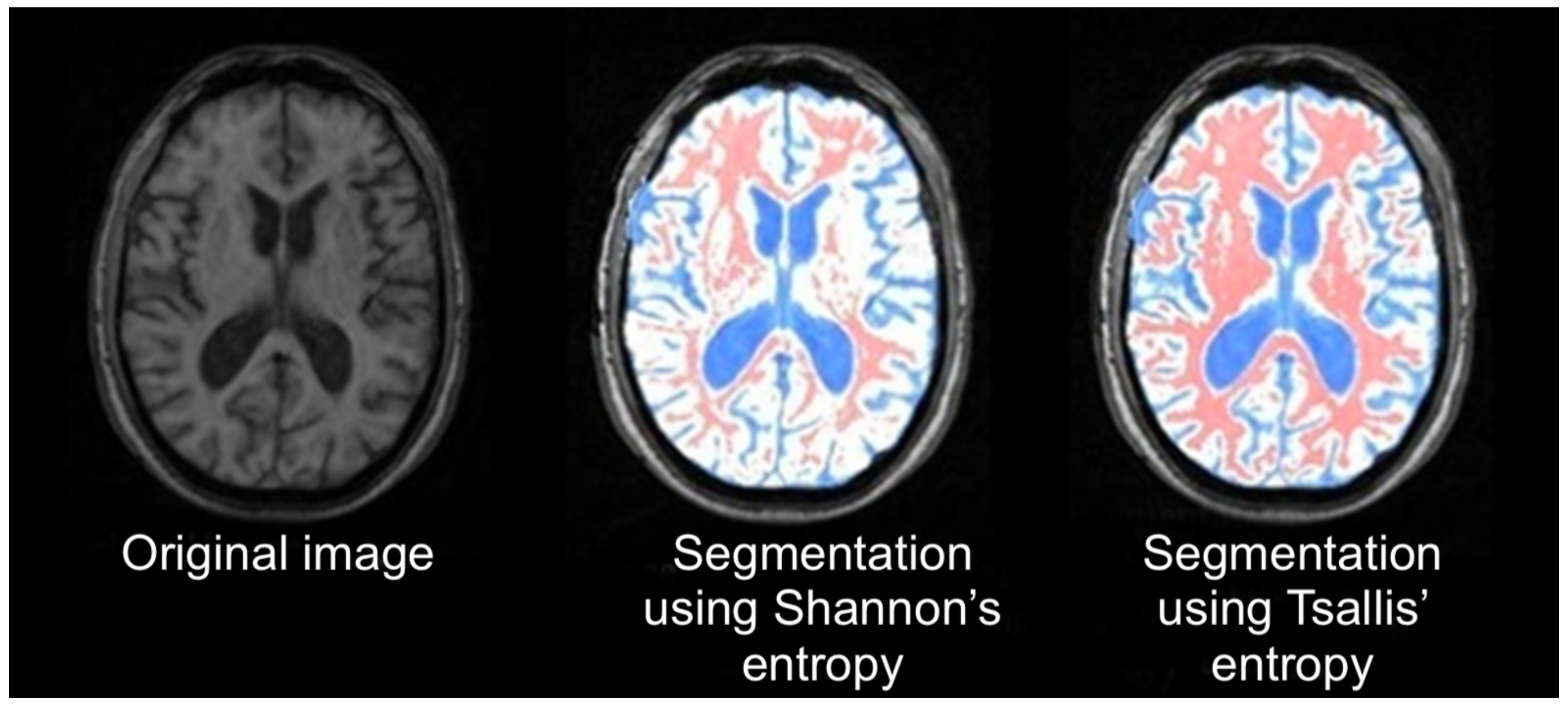
- Diniz, P.R.B.; Murta, L.O.; Brum, D.G.; de Araujo, D.B.; Santos, A.C. Brain tissue segmentation using q-entropy in multiple sclerosis magnetic resonance images. Braz. Med. Biol. Res. 2010, 43, 77–84. [Google Scholar] [CrossRef]
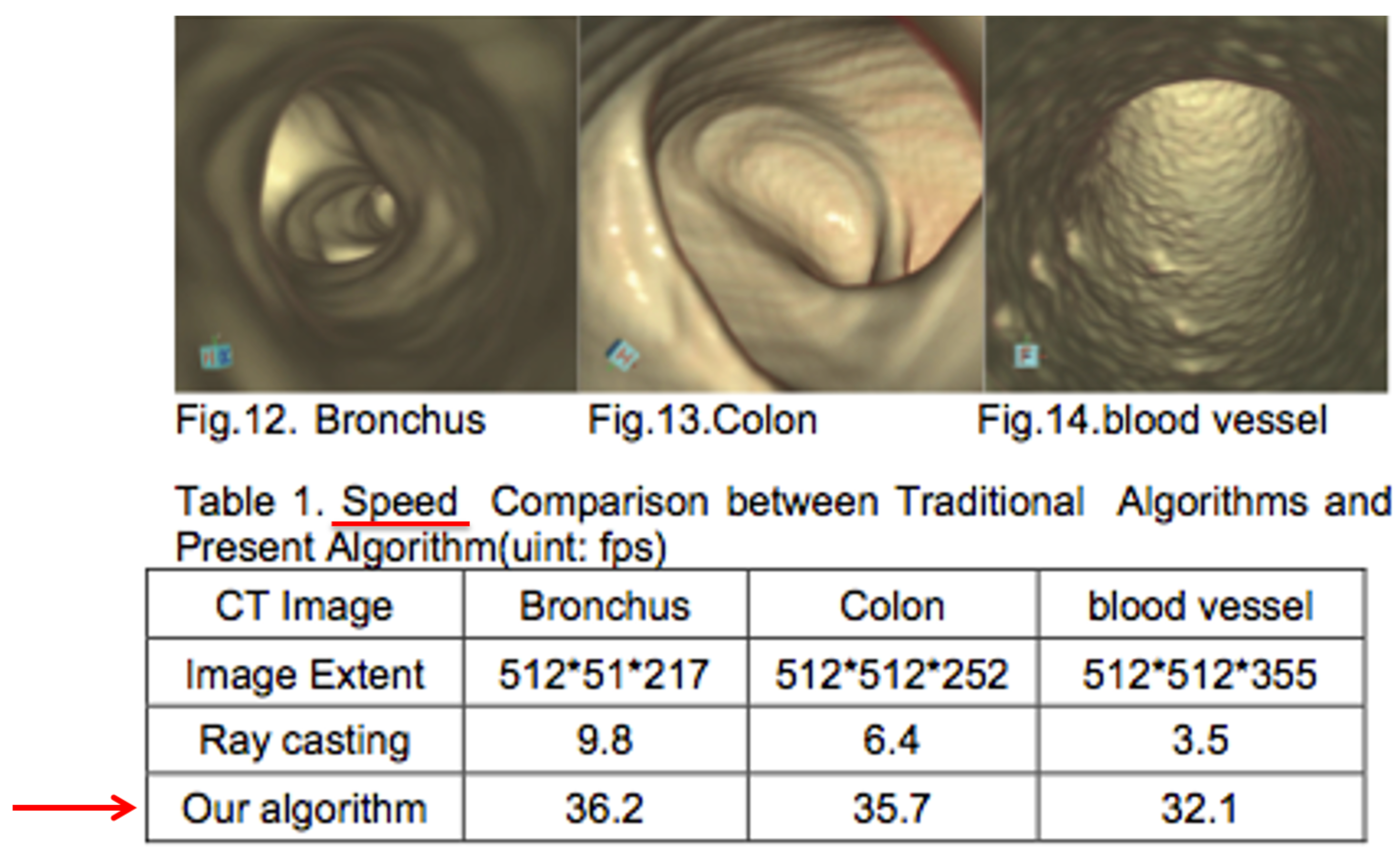
- Shi, W.L.; Li, Y.; Miao, Y.; Hu, Y. Research on the key technology of image guided surgery. Electr. Rev. 2012, 88, 29–33. [Google Scholar]
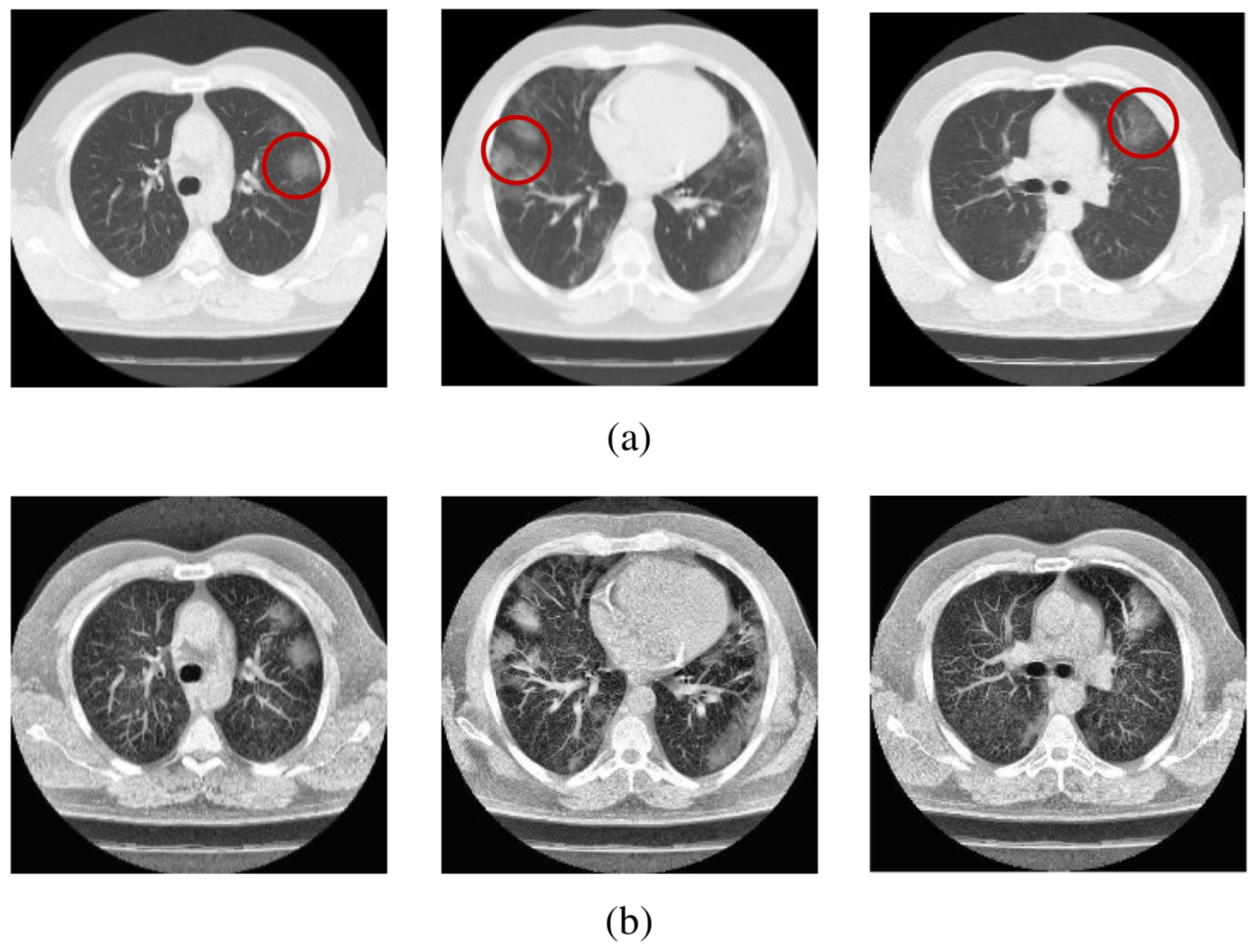
- Al-Azawi, R.J.; Al-Saidi, N.M.G.; Jalab, H.A.; Kahtan, H.; Ibrahim, R.W. Efficient classification of COVID-19 CT scans by using q-transform model for feature extraction. PeerJ. Comput. Sci. 2021, 7, e553. [Google Scholar] [CrossRef]
- Silva, I.; Moody, G.B.; Celi, L. Improving the quality of ECGs collected using mobile phones: The Physionet/Computing in Cardiology Challenge 2011. Comput. Cardiol. 2011, 273–276. [Google Scholar]
- Rautaharju, P.M. Eyewitness to history: Landmarks in the development of computerized electrocardiography. J. Electrocardiol. 2016, 49, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Van der Bijl, K.; Elgendi, M.; Menon, C. Automatic ECG quality assessment techniques: A systematic review. Diagnostics 2022, 12, 2578. [Google Scholar] [CrossRef] [PubMed]
- Stracina, T.; Ronzhina, M.; Redina, R.; Novakova, M. Golden standard or obsolete method? Review of ECG applications in clinical and experimental context. Front. Physiol. 2022, 13, 613. [Google Scholar] [CrossRef]
- Siontis, K.C.; Noseworthy, P.A.; Attia, Z.I.; Friedman, P.A. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat. Rev. Cardiol. 2021, 18, 465–478. [Google Scholar] [CrossRef]
- Kanani, P.; Padole, M. ECG heartbeat arrhythmia classification using time-series augmented signals and deep learning approach. Procedia Comput. Sci. 2020, 171, 524–531. [Google Scholar] [CrossRef]
- Rathi, R.; Yagnik, N.; Tiwari, S.; Sharma, C. Analysis of statistical models for fast time series ECG classifications. Eng. Lett. 2022, 30, 1–12. [Google Scholar]
- Abdulghani, A.M.; Casson, A.J.; Rodriguez-Villegas, E. Compressive sensing scalp EEG signals: Implementations and practical performance. Med. Biol. Eng. Comput. 2012, 50, 1137–1145. [Google Scholar] [CrossRef]
- Chávez, M.; Martinerie, J.; Le Van Quyen, M. Statistical assessment of nonlinear causality: Application to epileptic EEG signals. J. Neurosci. Methods 2003, 124, 113–128. [Google Scholar] [CrossRef]
- Cook, M.J.; O’Brien, T.J.; Berkovic, S.M.; Murphy, M.; Morokoff, A.; Fabinyi, G.; D’Souza, W.; Yerra, R.; Archer, J.; Litewka, L.; et al. Prediction of seizure likelihood with a long-term, implanted seizure advisory system in patients with drug-resistant epilepsy: A first-in-man study. Lancet Neurol. 2013, 12, 563–571. [Google Scholar] [CrossRef]
- Devarajan, K.; Jyostna, E.; Jayasri, K.; Balasampath, V. EEG-based epilepsy detection and prediction. Int. J. Eng. Technol. 2014, 6, 212. [Google Scholar] [CrossRef]
- Aslam, M.H.; Usman, S.M.; Khalid, S.; Anwar, A.; Alroobaea, R.; Hussain, S.; Almotiri, J.; Ullah, S.S.; Yasin, A. Classification of EEG signals for prediction of epileptic seizures. Appl. Sci. 2022, 12, 7251. [Google Scholar] [CrossRef]
- Gajic, D.; Djurovic, Z.; Di Gennaro, S.; Gustafsson, F. Classification of EEG signals for detection of epileptic seizures based on wavelets and statistical pattern recognition. Biomed. Eng. Appl. Basis Commun. 2014, 26, 1450021. [Google Scholar] [CrossRef]
- Hernández, D.E.; Trujillo, L.; Flores, E.Z.; Villanueva, O.M.; Romo-Fewell, O. Detecting epilepsy in EEG signals using time, frequency and time-frequency domain features. In Computer Science and Engineering-Theory and Applications; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Coelho, V.N.; Coelho, I.M.; Coelho, B.N.; Souza, M.J.; Guimarães, F.G.; Luz, E.D.; Barbosa, A.C.; Coelho, M.N.; Netto, G.G.; Costa, R.C.; et al. EEG time series learning and classification using a hybrid forecasting model calibrated with GVNS. Electron. Notes Discret. Math. 2017, 58, 79–86. [Google Scholar] [CrossRef]
- Zeger, S.L.; Irizarry, R.; Peng, R.D. On time series analysis of public health and biomedical data. Annu. Rev. Public Health 2006, 27, 57–79. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S. Time series analysis and some applications in medical research. J. Math. Stat. Stud. 2022, 3, 31–36. [Google Scholar] [CrossRef]
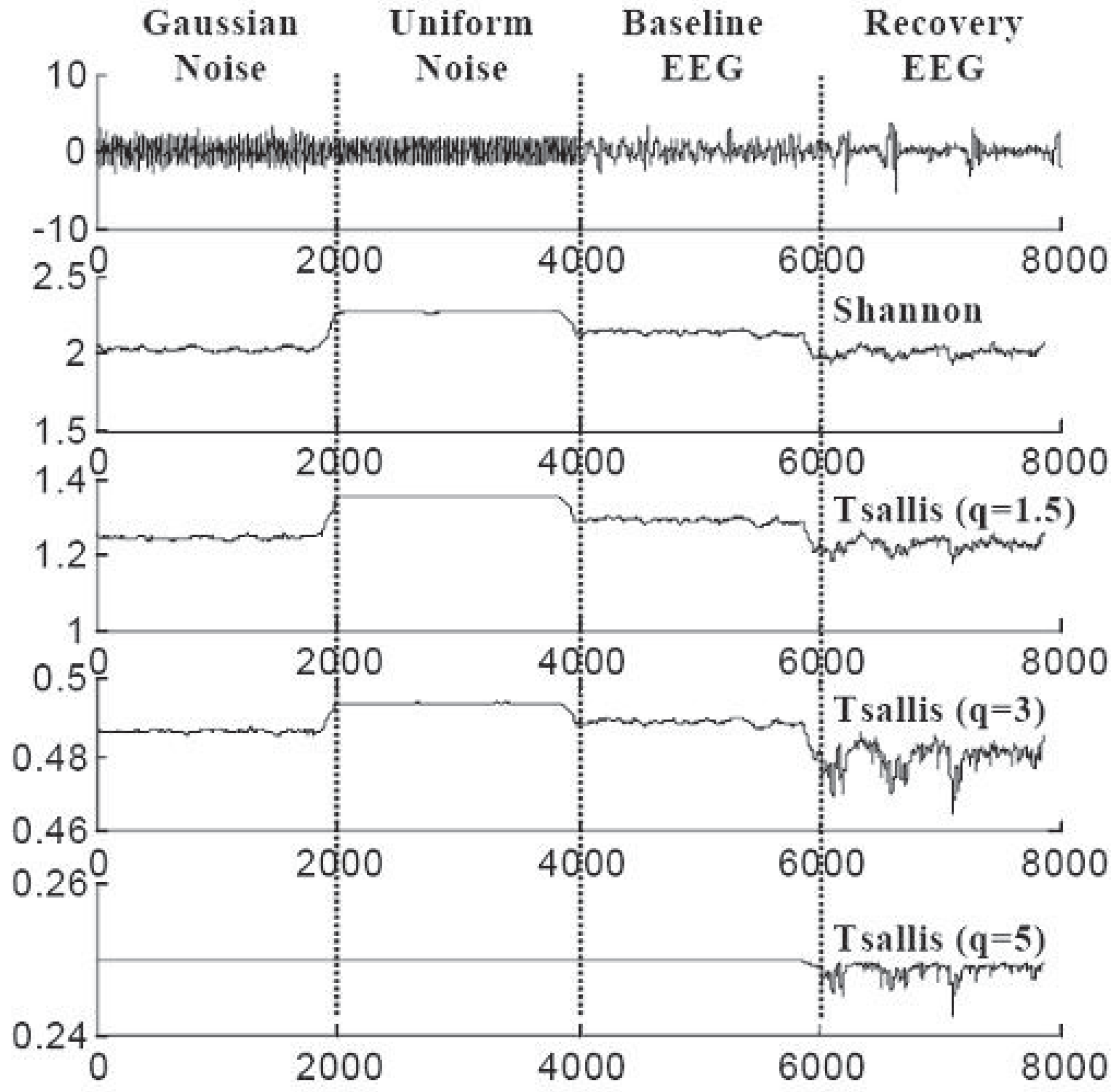
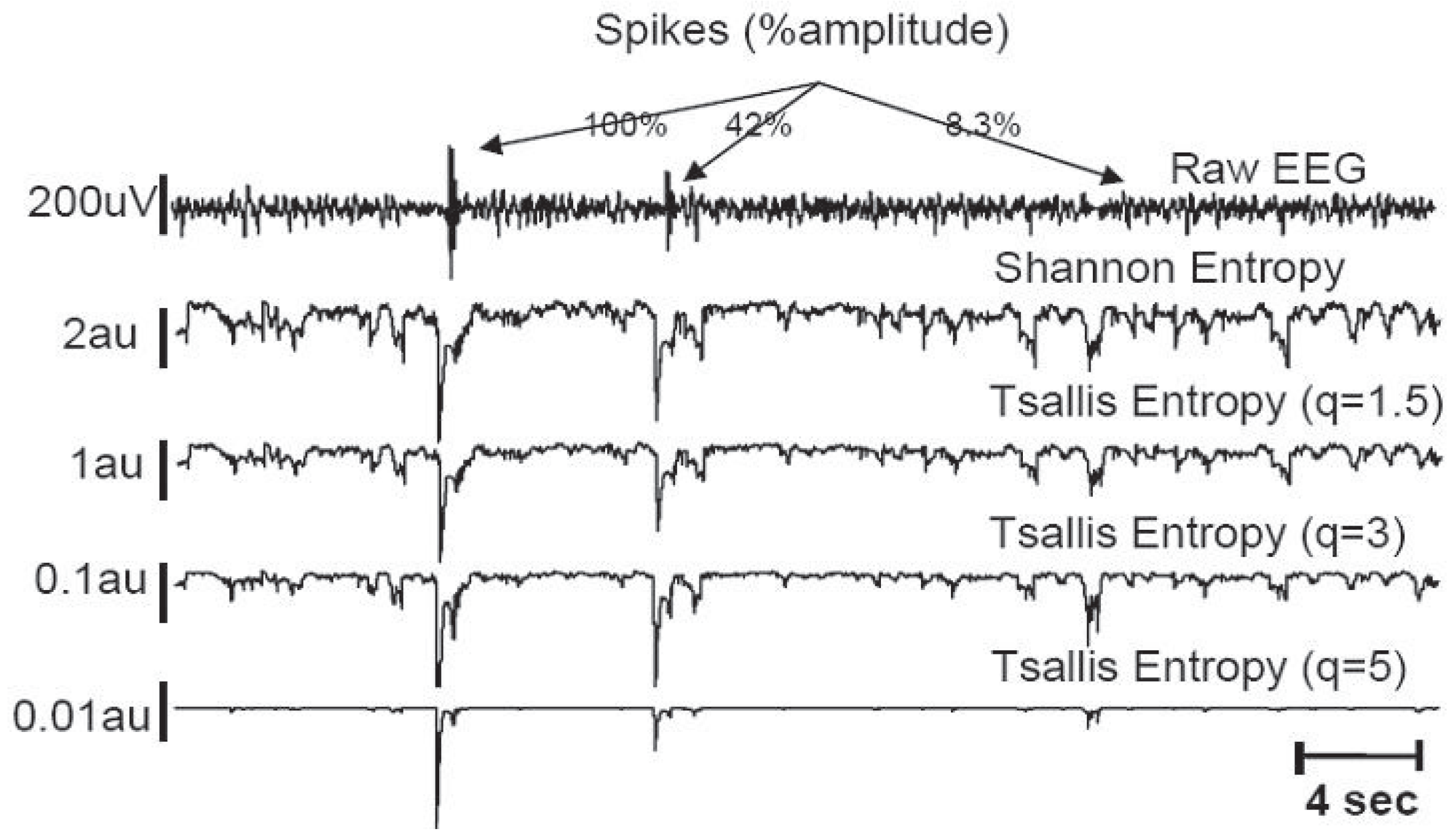
- Bezerianos, A.; Tong, S.; Thakor, N. Time-dependent entropy estimation of EEG rhythm changes following brain ischemia. Ann. Biomed. Eng. 2003, 31, 221–232. [Google Scholar] [CrossRef]
- Tong, S.; Zhu, Y.; Geocadin, R.G.; Hanley, D.; Thakor, N.V.; Bezerianos, A. Monitoring brain injury with Tsallis entropy. In Proceedings of the 23rd IEEE Engineering in Medicine and Biology Society Annual Conference, Instanbul, Turkey, 26–28 October 2001. [Google Scholar]
- Bezerianos, A.; Tong, S.; Zhu, Y.; Thakor, N.V. Nonadditive information theory for the analyses of brain rythms. In Proceedings of the 23rd IEEE Engineering in Medicine and Biology Society Annual Conference, Instanbul, Turkey, 26–28 October 2001. [Google Scholar]
- Thakor, N.V.; Paul, J.; Tong, S.; Zhu, Y.; Bezerianos, A. Entropy of brain rhythms: Normal versus injury EEG. In Proceedings of the 11th IEEE Signal Processing Workshop, Stockholm, Sweden, 8 August 2001; pp. 261–264. [Google Scholar]
- Bezerianos, A.; Tong, S.; Paul, J.; Zhu, Y.; Thakor, N.V. Information measures of brain dynamics. In Proceedings of the 5th EURASIP Biennal International Workshop on Nonlinear Signal and Image Processing (NSP-01), Baltimore, MD, USA, 3–6 June 2001. [Google Scholar]
- Cimponeriu, L.; Tong, S.; Bezerianos, A.; Thakor, N.V. Synchronization and information processing across the cerebral cortexfollowing cardiac arrest injury. In Proceedings of the 24th Engineering in Medicine & Biology Society Conference, San Antonio, TX, USA, 26–28 October 2002. [Google Scholar]
- Tong, S.; Bezerianos, A.; Paul, J.; Zhu, Y.; Thakor, N. Nonextensive entropy measure of EEG following brain injury from cardiac arrest. Phys. A 2002, 305, 619–628. [Google Scholar] [CrossRef]
- Tong, S.; Bezerianos, A.; Malhotra, A.; Zhu, Y.; Thakor, N. Parameterized entropy analysis of EEG following hypoxic-ischemic brain injury. Phys. Lett. A 2003, 314, 354–361. [Google Scholar] [CrossRef]
- Geocadin, R.G.; Tong, S.; Bezerianos, A.; Smith, S.; Iwamoto, T.; Thakor, N.V.; Hanley, D.F. Approaching brain injury after cardiac arrest: From bench to bedside. In Proceedings of the Neuroengineering Workshop, Capri, Italy, 20–22 March 2003; pp. 277–280. [Google Scholar]
- Thakor, N.; Tong, S. Advances in quantitative electroencephalogram analysis methods. Annu. Rev. Biomed. Eng. 2004, 6, 453. [Google Scholar] [CrossRef]
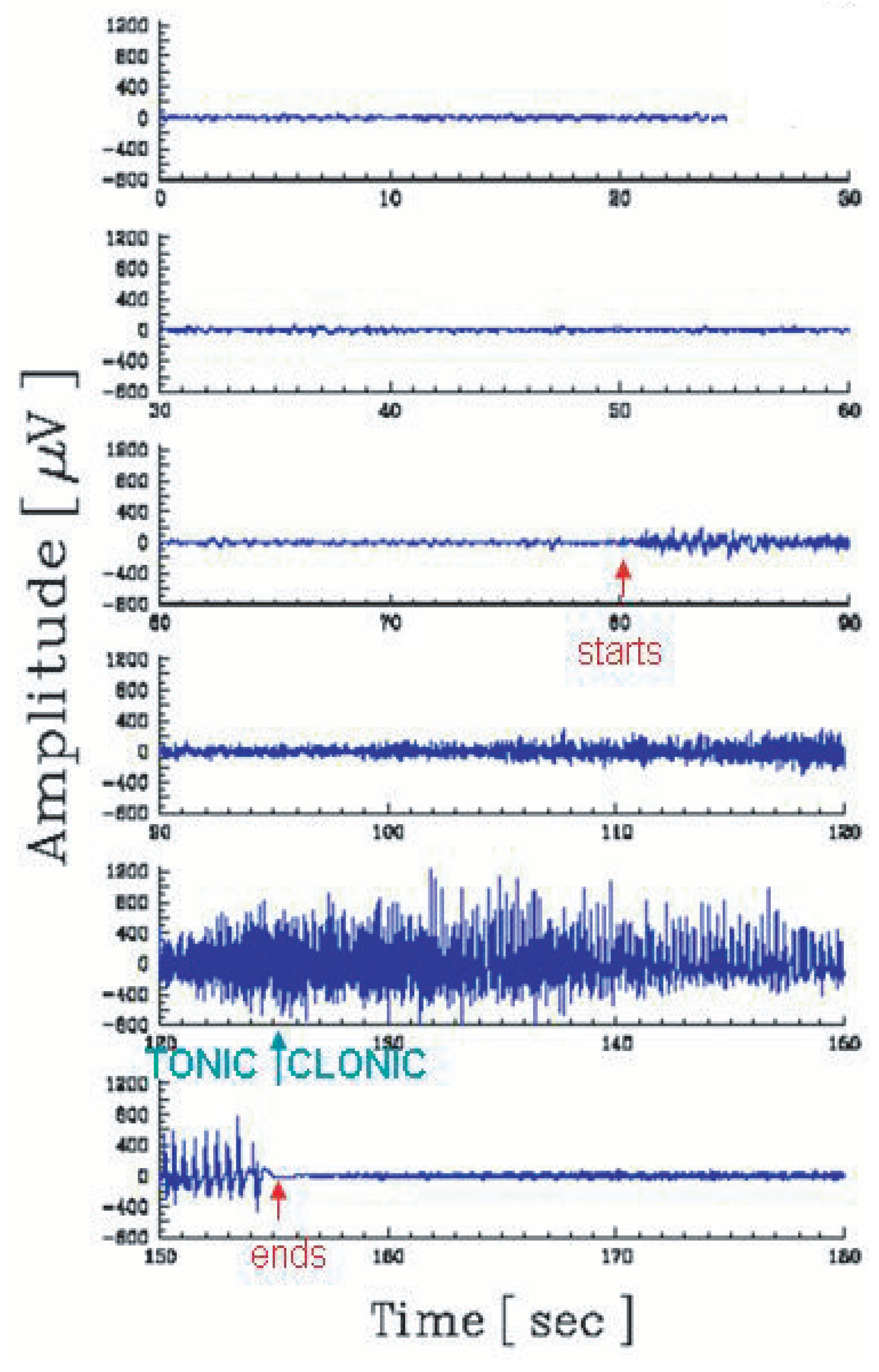
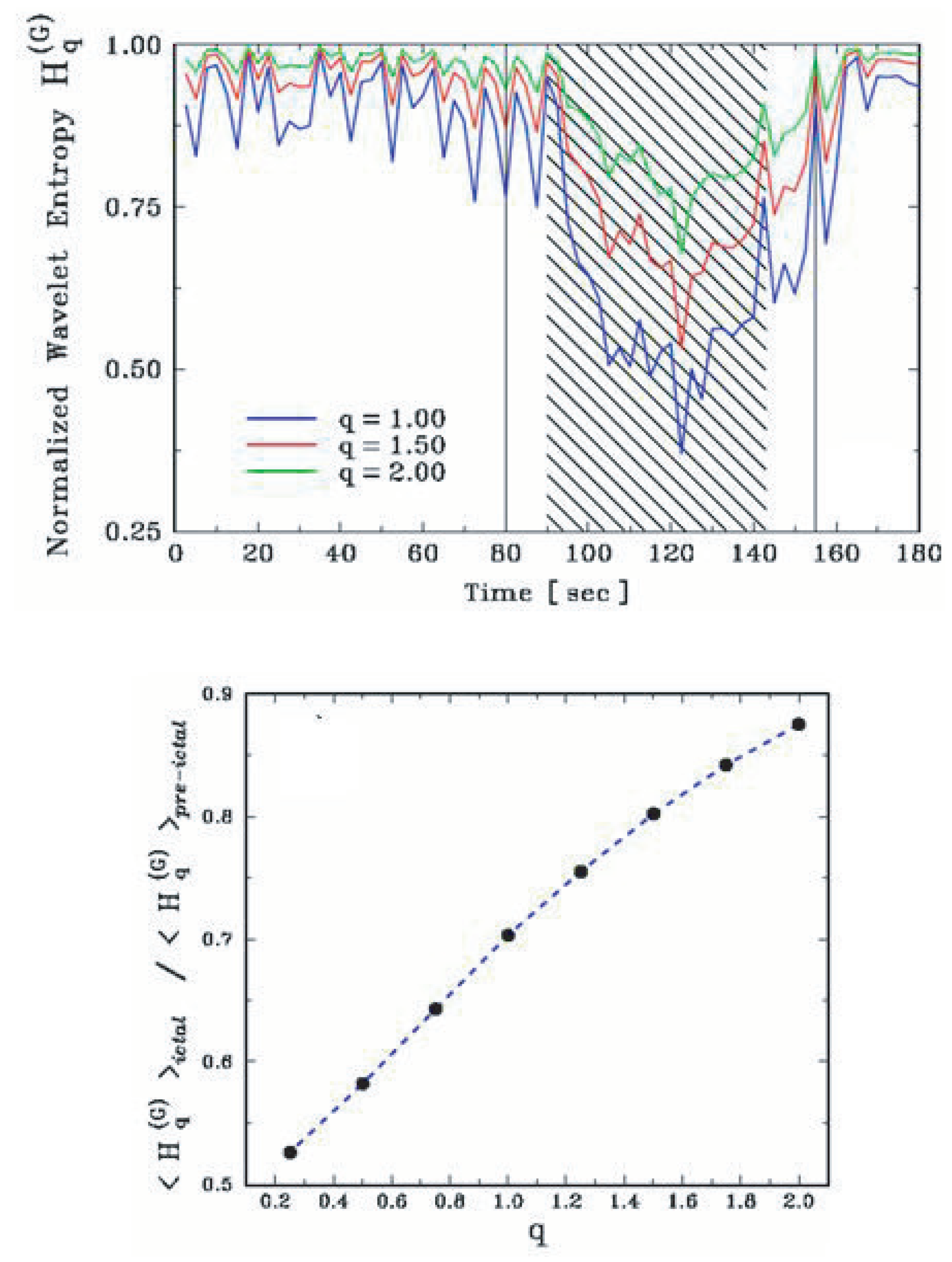
- Gao, J.; Tung, W.W.; Cao, Y.; Hu, J.; Qi, Y. Power-law sensitivity to initial conditions in a time series with applications to epileptic seizure detection. Phys. A 2005, 353, 613. [Google Scholar] [CrossRef]
- Plastino, A.; Rosso, O.A. Entropy and statistical complexity in brain activity. Europhys. News 2005, 36, 224. [Google Scholar] [CrossRef]
- Cai, S.M.; Jiang, Z.H.; Zhou, T.; Zhou, P.L.; Yang, H.J.; Wang, B.H. Scale invariance of human electroencephalogram signals in sleep. Phys. Rev. E 2007, 76, 061903. [Google Scholar] [CrossRef] [PubMed]
- Poza, J.; Hornero, R.; Escudero, J.; Fernandez, A.; Sanchez, C.I. Regional analysis of spontaneous MEG rhythms in patients with Alzheimer’s desease using spectral entropies. Ann. Biomed. Eng. 2008, 36, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Sotolongo-Grau, O.; Rodriguez-Perez, D.; Antoranz, J.C.; Sotolongo-Costa, O. Tissue Radiation Response with Maximum Tsallis Entropy. Phys. Rev. Lett. 2010, 105, 158105. [Google Scholar] [CrossRef]
- Tsallis, C.; Tirnakli, U. Predicting COVID-19 peaks around the world. Front. Phys. 2020, 8, 217. [Google Scholar] [CrossRef]
- Tirnakli, U.; Tsallis, C. Epidemiological model with anomalous kinetics–Early stages of the COVID-19 pandemic. Front. Phys. 2020, 8, 613168. [Google Scholar] [CrossRef]
- Available online: https://www.worldometers.info/coronavirus/#countries (accessed on 21 March 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsallis, C.; Pasechnik, R. Medical Applications of Nonadditive Entropies. Entropy 2023, 25, 578. https://doi.org/10.3390/e25040578
Tsallis C, Pasechnik R. Medical Applications of Nonadditive Entropies. Entropy. 2023; 25(4):578. https://doi.org/10.3390/e25040578
Chicago/Turabian StyleTsallis, Constantino, and Roman Pasechnik. 2023. "Medical Applications of Nonadditive Entropies" Entropy 25, no. 4: 578. https://doi.org/10.3390/e25040578
APA StyleTsallis, C., & Pasechnik, R. (2023). Medical Applications of Nonadditive Entropies. Entropy, 25(4), 578. https://doi.org/10.3390/e25040578









