Physical, Perceptual, Socio-Relational, and Affective Skills of Five-Year-Old Children Born Preterm and Full-Term According to Their Body Mass Index
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
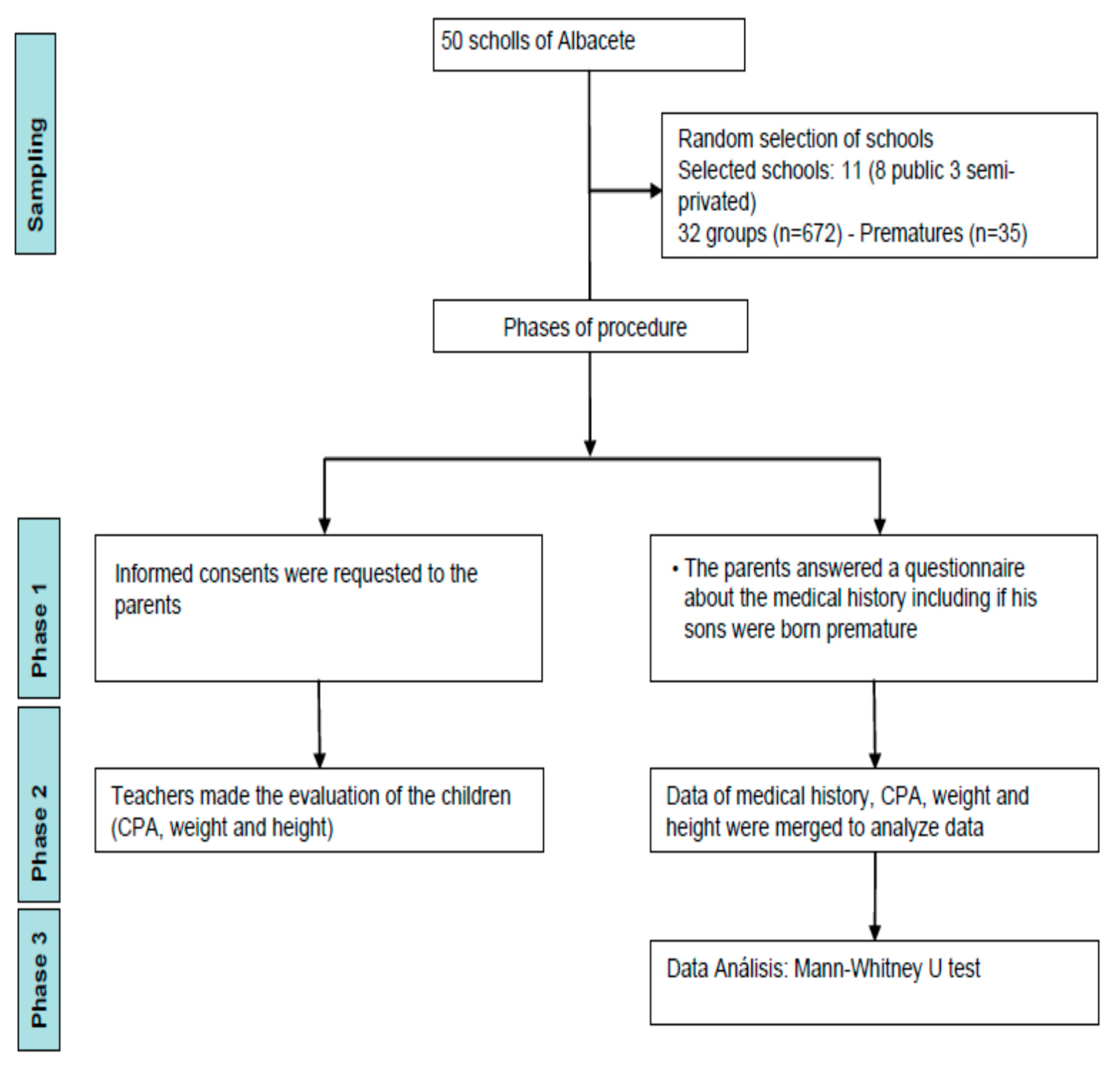
2.2. Procedure
2.3. Instruments
2.4. Statistical Analysis
3. Results
3.1. Differences between Preterm and Full-Term According to the BMI
3.2. Overall Difference between Preterm and Full-Term Children
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ionio, C.; Lista, G.; Mascheroni, E.; Olivari, M.; Confalonieri, E.; Mastrangelo, M.; Brazzoduro, V.; Balestriero, M.; Banfi, A.; Bonanomi, A.; et al. Premature birth: Complexities and difficulties in building the mother-child relationship. J. Reprod. Infant Psychol. 2017, 35, 509–523. [Google Scholar] [CrossRef]
- Roz-Faraco, C.C.; Pascual-Gomez, I. Application of an observation system in the practice of psychomotor circuits in early education. Rev. Cercet. Interv. Soc. 2019, 66, 315–327. [Google Scholar] [CrossRef]
- Foulder-Hughes, L.; Cooke, R. Motor, cognitive, and behavioural disorders in children born very preterm. Dev. Med. Child. Neurol. 2003, 45, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Gil-Madrona, P.; Contreras, O.R.; Roblizo, M.J.; Gómez, I. Potencial pedagógico de la educación física en la educación infantil: Atributos y convicciones. Infanc. Aprendiz. 2008, 31, 165–178. [Google Scholar]
- Marret, S.; Marchand-Martin, L.; Picaud, J.C.; Hascoët, J.M.; Arnaud, C.; Rozé, J.C.; Truffert, P.; Larroque, B.; Kaminski, M.; Ancel, P.Y.; et al. Brain Injury in Very Preterm Children and Neurosensory and Cognitive Disabilities during Childhood: The EPIPAGE Cohort Study. PLoS ONE 2013, 8, e62683. [Google Scholar] [CrossRef] [Green Version]
- Bourke, J.; Wong, K.; Srinivasjois, R.; Pereira, G.; Shepherd, C.C.; White, S.W.; Leonard, H. Predicting long-term survival without major disability for infants born preterm. J. Pediatr. 2019, 215, 90–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romero-Martínez, S.J.; Ordóñez-Camacho, X.G.; Gil-Madrona, P. Development of the checklist of psychomotor activities for 5-to 6-year-old children. Percept. Mot. Ski 2018, 125, 1070–1092. [Google Scholar] [CrossRef] [PubMed]
- Malatesta, C.Z.; Culver, C.; Tesman, J.R.; Shepard, B.; Fogel, A.; Reimers, M.; Zivin, G. The development of emotion expression during the first two years of life. Monogr. Soc. Res. Child Dev. 1989, 12, 123–136. [Google Scholar] [CrossRef]
- Spittle, A.J.; Orton, J. Cerebral palsy and developmental coordination disorder in children born preterm. Semin. Fetal Neonatal Med. 2014, 19, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Caravaca, J. Atención Temprana y Niños Prematuros; EAE: Madrid, Spain, 2011. [Google Scholar]
- Torrioli, M.G.; Frisone, M.F.; Bonvini, L.; Luciano, R.; Pasca, M.G.; Lepori, R.; Guzzetta, F. Perceptual-motor, visual and cognitive ability in very low birthweight preschool children without neonatal ultrasound abnormalities. Brain Dev. 2000, 22, 163–168. [Google Scholar] [CrossRef]
- Blencowe, H.; Cousens, S.; Oestergaard, M.; Chou, D.; Moller, A.B.; Narwal, R.; Adler, A.; Garcia, C.V.; Rohde, S.; Say, L.; et al. National, regional and worldwide estimates of preterm birth. Lancet 2012, 379, 2162–2172. [Google Scholar] [CrossRef] [Green Version]
- Piek, J.P.; Dawson, L.; Smith, L.M.; Gasson, N. The role of early fine and gross motor development on later motor and cognitive ability. Hum. Mov. Sci. 2008, 27, 668–681. [Google Scholar] [CrossRef] [PubMed]
- De Kieviet, J.F.; Piek, J.P.; Aarnoudse-Moens, C.S.; Oosterlaan, J. Motor development in very preterm and very low-birth-weight children from birth to adolescence: A meta-analysis. JAMA New Open 2009, 302, 2235–2242. [Google Scholar] [CrossRef]
- Gil-Madrona, P.; Romero-Martínez, S.J.; Sáez-Gallego, N.M.; Ordóñez-Camacho, X.G. Psychomotor limitations of overweight and obese five-year-old children: Influence of body mass indices on motor, perceptual, and social-emotional skills. Int. J. Environ. Res. Public Health 2019, 16, 427. [Google Scholar] [CrossRef] [Green Version]
- Spittle, A.J.; Anderson, P.J.; Lee, K.J.; Ferretti, C.; Eeles, A.; Orton, J.; Boyd, R.N.; Doyle, L.W. Preventive care at home for very preterm infants improves infant and caregiver outcomes at two (2) years. Pediatrics 2010, 126, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Sailer, U.; Flanagan, J.R.; Johansson, R.S. Eye-hand coordination during learning of a novel visomotor task. J. Neurosci. 2005, 25, 8833–8842. [Google Scholar] [CrossRef] [Green Version]
- Albacete City Council. Public and Private Schools in the Province of Albacete. Available online: http://www.albacete.es/es/webs-municipales/educacion/primaria-y-secundaria/colegios-publicosy-concertados (accessed on 17 July 2017).
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA New Open 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Available online: https://www.who.int/pmnch/media/news/2012/borntoosoon_execsum_es.pdf (accessed on 2 April 2021).
- World Health Organization (WHO). Obesity: Preventing and Managing the Global Epidemic; Suiza: Geneva, Switzerland, 2000. [Google Scholar]
- Montero, I.; León, O.G. A guide for naming research studies in Psychology. Int. J. Clin. Health Psychol. 2007, 7, 847–862. [Google Scholar]
- Blauw-Hospers, C.H.; de Graaf-Peters, V.B.; Dirks, T.; Bos, A.F.; Hadders-Algra, M. Does early intervention in infants at high risk for a developmental motor disorder improve motor and cognitive development? Neurosci. Biobehav. Rev. 2007, 31, 1201–1212. [Google Scholar] [CrossRef]
- Marlow, N. Neurocognitive outcome after very preterm birth. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, F224–F228. [Google Scholar] [CrossRef] [PubMed]
- Wolke, D.; Samara, M.; Bracewell, M.; Marlow, N.; EPICure Study Group. Specific language difficulties and school achievement in children born at 25 weeks of gestation or less. Arch. Dis. Child 2008, 152, 256–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López de la Fuente, M. Teorías del control motor, principios de aprendizaje motor y concepto Bobath. Rev. TOG 2013, 10, 1–27. [Google Scholar]
- Williams, J.; Holmes, C.A. Improving the early detection of children with subtle developmental problems. J. Child Health Care 2004, 8, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.M. Atención a la Diversidad en el Aula de Educación Infantil; Paraninfo: Madrid, Spain, 2015. [Google Scholar]
- Spittle, A.; Orton, J.; Anderson, P.J.; Boyd, R.; Doyle, L.W. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst. Rev. 2015, 11, 013745. [Google Scholar] [CrossRef] [PubMed]
- Arbones-Fernández, B. Detección, Prevención y Tratamiento de Dificultades del Aprendizaje. Como Descubrir, Tratar y Prevenir los Problemas en la Escuela; Gesgiblo: Vigo, Spain, 2005. [Google Scholar]
- Severson, H.H.; Walker, H.M.; Hope-Doolittle, J.; Kratochwill, T.R.; Gresham, F.M. Proactive, early screening to detect behaviorally at-risk students: Issues, approaches, emerging innovations, and professional practices. J. Sch. Psychol. 2007, 45, 193–223. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.C.M.; Wilson, P.H.; Westenberg, Y.; Duysens, J. Fine motor deficiencies in children with developmental coordination disorder and learning disabilities: An underlying open-loop control deficit. Hum. Mov. Sci. 2003, 22, 495–513. [Google Scholar] [CrossRef]
- Bermúdez, O.G.; Quintana, F.C.; de los Ángeles Sosa, M.; de la Cruz, J.; Mañas, M.; García, M.P. Alteraciones neuropsicológicas y emocionales en niños prematuros de muy bajo peso al nacer. Rev. Argent. Cienc. Comport. 2012, 4, 3–10. [Google Scholar]
- Piek, J.P.; Dyck, M.J. Sensory-motor deficits in children with developmental coordination disorder, attention deficit hyperactivity disorder and autistic disorder. Hum. Mov. Sci. 2004, 23, 475–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schonhaut, L.; Armijo, I.; Schönstedt, M.; Alvarez, J.; Cordero, M. Validity of the ages and stages questionnaires in term and preterm infants. Pediatrics 2013, 131, e1468–e1474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pritchard, V.E.; Clark, C.A.; Liberty, K.; Champion, P.R.; Wilson, K.; Woodward, L.J. Early school-based learning difficulties in children born very preterm. Early Hum. Dev. 2009, 85, 215–224. [Google Scholar] [CrossRef]
- Ishizaki, Y.; Nagahama, T.; Kaneko, K. Mental health of mothers and their premature infants for the prevention of child abuse and maltreatment. Health 2013, 5, 612–615. [Google Scholar] [CrossRef] [Green Version]
| BMI | Descriptive Statistics | |||||||
|---|---|---|---|---|---|---|---|---|
| Scale | Skill | n | Mean (SD) | Range | Me | G1 | G2 | |
| Physical | LT | 13 | Severely/moderately underweight | 24.92 (3.14) | 107.35 | 23 | 1.692 | 1.671 |
| 22 | Normal/overweight/obese | 25.27 (3.60) | 118.27 | 24 | 1.662 | 1.893 | ||
| DC | 13 | Severely/moderately underweight | 25.38 (4.95) | 105.33 | 27 | −1.134 | 0.284 | |
| 22 | Normal/overweight/obese | 26.18 (3.67) | 106.24 | 27 | −0.546 | −0.992 | ||
| ME | 13 | Severely/moderately underweight | 13.46 (2.33) | 134.77 | 15 | −1.412 | 1.140 | |
| 22 | Normal/overweight/obese | 12.91 (2.63) | 132.20 | 14 | −0.008 | -0.327 | ||
| Motor | TCP | 13 | Severely/moderately underweight | 13.69 (2.17) | 185.14 | 15 | −1.853 | 3.067 |
| 22 | Normal/overweight/obese | 12.32 (2.62) | 186.33 | 12 | −0.833 | 0.128 | ||
| BAL | 13 | Severely/moderately underweight | 21.15 (5.44) | 143.14 | 24 | −1.320 | −0.453 | |
| 22 | Normal/overweight/obese | 20.86 (4.32) | 131.29 | 21.5 | −1.342 | 2.289 | ||
| SUM | 13 | Severely/moderately underweight | 98.62 (12.05) | 157.88 | 104 | −1.407 | 0.616 | |
| 22 | Normal/overweight/obese | 97.55 (12.60) | 125.21 | 100 | −0.297 | −0.428 | ||
| Perceptive motor | RC | 13 | Severely/moderately underweight | 13.26 (3.19) | 117.35 | 15 | 1.732 | 1.262 |
| 22 | Normal/overweight/obese | 12.83 (2.45) | 106.47 | 13.5 | −0.884 | −0.552 | ||
| BI | 13 | Severely/moderately underweight | 17.62 (5.04) | 156.22 | 20 | −2.131 | 3.365 | |
| 22 | Normal/overweight/obese | 17.41 (3.54) | 141.25 | 19 | −1.475 | 1.164 | ||
| MD | 13 | Severely/moderately underweight | 12.62 (3.45) | 194.57 | 15 | −1.292 | 0.154 | |
| 22 | Normal/overweight/obese | 12.14 (3.01) | 133.30 | 14 | −0.987 | −0.136 | ||
| VMC | 13 | Severely/moderately underweight | 23.54 (4.53) | 103.04 | 24 | −1.380 | 1.663 | |
| 22 | Normal/overweight/obese | 24.73 (6.08) | 131.09 | 26.5 | −1.566 | −1.193 | ||
| SO | 13 | Severely/moderately underweight | 9.00 (1.29) | 133.04 | 10 | −1.410 | −1.824 | |
| 22 | Normal/overweight/obese | 8.91 (1.99) | 131.39 | 9.5 | −0.913 | −1.149 | ||
| SUM | 13 | Severely/moderately underweight | 76.00 (15.27) | 128.98 | 82 | −1.884 | 2.514 | |
| 22 | Normal/overweight/obese | 76.05 (14.37) | 125.27 | 82 | −0.919 | −0.478 | ||
| Emotional–social | EC | 13 | Severely/moderately underweight | 24.85 (4.53) | 133.14 | 26 | −1.310 | 0.616 |
| 22 | Normal/overweight/obese | 23.41 (6.08) | 121.49 | 24 | −1.066 | 0.665 | ||
| SR | 13 | Severely/moderately underweight | 19.46 (3.30) | 133.04 | 21 | −1.650 | 1.864 | |
| 22 | Normal/overweight/obese | 18.82 (4.22) | 131.39 | 18.5 | −0.319 | 0.498 | ||
| SUM | 13 | Severely/moderately underweight | 44.31 (7.13) | 133.98 | 47 | −1.704 | 2.294 | |
| 22 | Normal/overweight/obese | 42.23 (10.36) | 115.27 | 42 | −0.719 | 0.068 | ||
| BMI | Descriptive Statistics | |||||||
|---|---|---|---|---|---|---|---|---|
| Scale | Skill | n | Mean (DT) | Range | Me | G1 | G2 | |
| Physical-motor | LT | 87 | Severely/moderately underweight | 25.16 (4.77) | 106.25 | 23 | 0.533 | 0.036 |
| 550 | Normal/overweight/obese | 27.49 (5.12) | 174.84 | 27 | −0.014 | −1.002 | ||
| DC | 87 | Severely/moderately underweight | 26.25 (3.57) | 147.45 | 27 | −0.897 | 0.329 | |
| 550 | Normal/overweight/obese | 27.31 (3.11) | 121.32 | 29 | −0.195 | −0.647 | ||
| ME | 87 | Severely/moderately underweight | 13.82 (1.92) | 174.17 | 15 | −1.982 | 3.866 | |
| 550 | Normal/overweight/obese | 13.84 (2.24) | 123.20 | 14 | −1.607 | −3.196 | ||
| TCP | 87 | Severely/moderately underweight | 13.21 (2.58) | 185.24 | 14 | −1.053 | 0.391 | |
| 550 | Normal/overweight/obese | 12.90 (2.03) | 179.13 | 13 | −0.266 | −0.180 | ||
| BAL | 87 | Severely/moderately underweight | 21.82 (3.86) | 184.34 | 23 | −1.410 | 0.183 | |
| 550 | Normal/overweight/obese | 21.46 (3.36) | 141.19 | 22 | −0.666 | −0.080 | ||
| SUM | 87 | Severely/moderately underweight | 100.25 (11.85) | 148.98 | 104 | −1.347 | 2.644 | |
| 550 | Normal/overweight/obese | 103 (10.71) | 114.37 | 102 | −0.883 | 1.809 | ||
| Perceptual-motor | RC | 87 | Severely/moderately underweight | 13.34 (2.46) | 107.25 | 15 | −1.477 | 1.572 |
| 550 | Normal/overweight/obese | 13.09 (2.24) | 106.37 | 14 | −1.144 | 0.762 | ||
| BI | 87 | Severely/moderately underweight | 18.62 (2.87) | 147.12 | 20 | −2.301 | 4.745 | |
| 550 | Normal/overweight/obese | 19.13 (2.00) | 127.55 | 20 | −1.745 | 8.047 | ||
| MD | 87 | Severely/moderately underweight | 13.49 (2.36) | 134.57 | 15 | −1.869 | 1.725 | |
| 550 | Normal/overweight/obese | 13.65 (1.68) | 133.80 | 14 | −0.787 | 0.763 | ||
| VMC | 87 | Severely/moderately underweight | 24.95 (4.28) | 185.04 | 25 | −0.701 | −0.067 | |
| 550 | Normal/overweight/obese | 26.72 (3.30) | 188.13 | 27 | −1.295 | 0.542 | ||
| SO | 87 | Severely/moderately underweight | 8.85 (3.73) | 133.04 | 9 | −2.130 | 4.983 | |
| 550 | Normal/overweight/obese | 9.36 (4.11) | 148.09 | 10 | −2.273 | 2.419 | ||
| SUM | 87 | Severely/moderately underweight | 79.26 (9.70) | 128.98 | 82 | −1.764 | 2.781 | |
| 550 | Normal/overweight/obese | 81.95 (8.57) | 134.27 | 84 | −1.339 | 6.148 | ||
| Emotional–social | EC | 87 | Severely/moderately underweight | 25.74 (3.63) | 137.22 | 26 | −1.352 | 0.258 |
| 550 | Normal/overweight/obese | 26.86 (3.66) | 140.53 | 28 | −1.269 | 4.352 | ||
| SR | 87 | Severely/moderately underweight | 20.21 (2.89) | 134.25 | 21 | −0.568 | 0.183 | |
| 550 | Normal/overweight/obese | 20.76 (3.08) | 133.95 | 21 | −0.289 | 1.259 | ||
| SUM | 87 | Severely/moderately underweight | 45.94 (5.87) | 138.12 | 47 | −1.224 | 2.487 | |
| 550 | Normal/overweight/obese | 47.29 (6.15) | 141.04 | 49 | −0.690 | 3.348 | ||
| Descriptive Statistics | |||||||
|---|---|---|---|---|---|---|---|
| Scale | Skill | Prematurity Condition | Mean (SD) | Range | Me | G1 | G2 |
| Physical-motor | LT | Full-term | 25.14 (3.39) | 24 | 288.40 | 1.632 | 1.620 |
| Preterm | 25.14 (3.39) | 24 | 288.40 | 1.632 | 1.620 | ||
| DC | Full-term | 27.14 (3.20) | 28 | 350.08 | −1.189 | 1.045 | |
| Preterm | 25.89 (4.14) | 27 | 289.04 | −0.927 | 0.100 | ||
| ME | Full-term | 13.81 (1.56) | 14 | 348.68 | −1.669 | −1.100 | |
| Preterm | 13.11 (2.50) | 15 | 315.43 | 3.423 | −0.075 | ||
| TCP | Full-term | 12.95 (2.12) | 13 | 346.93 | −1.010 | 0.928 | |
| Preterm | 12.83 (2.52) | 14 | 348.29 | −1.061 | 0.383 | ||
| BAL | Full-term | 21.49 (3.44) | 22 | 347.41 | −0.734 | 0.023 | |
| Preterm | 20.97 (4.69) | 22 | 339.20 | −1.259 | 0.995 | ||
| SUM | Full-term | 102.35 (10.69) | 103 | 350.78 | −0.943 | 1.867 | |
| Preterm | 97.94 (12.23) | 101 | 275.87 | −0.627 | −0.322 | ||
| Perceptual-motor | RC | Full-term | 13.14 (2.29) | 14 | 346.50 | −0.627 | −0.322 |
| Preterm | 13.00 (2.71) | 15 | 356.49 | −1.239 | 0.399 | ||
| BI | Full-term | 19.04 (2.13) | 20 | 350.46 | −1.706 | −1.805 | |
| Preterm | 17.49 (4.09) | 20 | 281.87 | 14.052 | 2.320 | ||
| MD | Full-term | 13.63 (1.79) | 14 | 350.64 | −1.732 | 4.075 | |
| Preterm | 12.31 (3.14) | 14 | 278.59 | −0.918 | −0.628 | ||
| VMC | Full-term | 26.44 (3.52) | 27 | 351.11 | −0.908 | −2.902 | |
| Preterm | 24.29 (5.51) | 26 | 269.71 | −1.268 | 1.218 | ||
| SO | Full-term | 9.29 (1.38) | 10 | 349.45 | −1.110 | 0.453 | |
| Preterm | 8.94 (1.34) | 10 | 300.99 | 0.398 | 0.778 | ||
| SUM | Full-term | 81.53 (8.86) | 83 | 350.39 | −1.488 | 5.618 | |
| Preterm | 76.03 (14.49) | 81 | 283.29 | 0.999 | 0.198 | ||
| Emotional–social | EC | Full-term | 26.36 (3.60) | 27 | 351.56 | 3.104 | 23.94 |
| Preterm | 23.94 (5.74) | 25 | 261.19 | −1.244 | 1.360 | ||
| SR | Full-term | 20.61 (2.83) | 21 | 349.19 | −1.244 | 1.360 | |
| Preterm | 19.80 (3.49) | 21 | 305.87 | 0.966 | 0.800 | ||
| SUM | Full-term | 46.97 (5.83) | 48 | 351.00 | −1.244 | 5.253 | |
| Preterm | 40.75 (8.70) | 45 | 271.73 | 1.360 | 0.611 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gil-Madrona, P.; Romero-Martínez, S.J.; Roz-Faraco, C.C. Physical, Perceptual, Socio-Relational, and Affective Skills of Five-Year-Old Children Born Preterm and Full-Term According to Their Body Mass Index. Int. J. Environ. Res. Public Health 2021, 18, 3769. https://doi.org/10.3390/ijerph18073769
Gil-Madrona P, Romero-Martínez SJ, Roz-Faraco CC. Physical, Perceptual, Socio-Relational, and Affective Skills of Five-Year-Old Children Born Preterm and Full-Term According to Their Body Mass Index. International Journal of Environmental Research and Public Health. 2021; 18(7):3769. https://doi.org/10.3390/ijerph18073769
Chicago/Turabian StyleGil-Madrona, Pedro, Sonia J. Romero-Martínez, and Carmen C. Roz-Faraco. 2021. "Physical, Perceptual, Socio-Relational, and Affective Skills of Five-Year-Old Children Born Preterm and Full-Term According to Their Body Mass Index" International Journal of Environmental Research and Public Health 18, no. 7: 3769. https://doi.org/10.3390/ijerph18073769
APA StyleGil-Madrona, P., Romero-Martínez, S. J., & Roz-Faraco, C. C. (2021). Physical, Perceptual, Socio-Relational, and Affective Skills of Five-Year-Old Children Born Preterm and Full-Term According to Their Body Mass Index. International Journal of Environmental Research and Public Health, 18(7), 3769. https://doi.org/10.3390/ijerph18073769







