Abstract
The emergence of online medical teams (OMTs) as a multidisciplinary approach to addressing complex health issues has gained increasing academic recognition. However, the factors influencing patient adoption of medical advice in this new communication context remain underexplored. This study investigates how multi-doctor involvement in OMTs affects patient adoption of medical advice and examines the moderating roles of leader participation, disciplinary diversity, and illness complexity. The results indicate that multi-doctor involvement positively influences patient adoption of medical advice. This relationship is strengthened by leader participation and disciplinary diversity, while illness complexity exerts no significant moderating effect. As the first study to explore patient adoption of medical advice in the OMT context, these findings advance theoretical understanding and offer practical implications for improving online healthcare services.
1. Introduction
Team-based collaboration has long been recognized as an effective approach to enhancing knowledge sharing, decision-making, and service quality in healthcare [1]. With the rapid advancement of digital health technologies, online healthcare communities (OHCs) have emerged as critical platforms for delivering remote care, enabling doctors and patients to interact without temporal or geographic constraints [2]. However, due to the limited doctor availability and declining service efficiency (https://www.36kr.com/p/1724943990785, accessed on 27 August 2025), some OHC platforms have introduced team-based online consultation (OTC), where multiple doctors form a virtual team to jointly diagnose and advise patients. Unlike traditional one-on-one consultations, OTC involves structured, team-based interactions in which doctors from the same or different specialties jointly respond to patient inquiries. By integrating diverse disciplinary expertise, this collaborative mode has the potential to enhance the accuracy, comprehensiveness, and credibility of medical advice, thereby improving the overall quality of care delivered. According to relevant statistics, the number of patients receiving team-based consultations on a leading online healthcare platform in China grew by nearly eightfold within one year, highlighting the practical significance and growing prevalence of medical teams in online healthcare (https://www.iyiou.com/news/20200105121542, accessed on 27 August 2025).
In the OTC platforms, patient adoption of online medical advice is a critical indicator of the effectiveness of online medical teams (OMTs). Specifically, higher levels of adoption reflect patients’ trust in the medical team, their perceived credibility of the advice, and their willingness to act on the recommendations provided. Such adoption contributes to improved individual health outcomes and enhances the overall quality and perceived value of online healthcare services. Conversely, low levels of adoption may signal dissatisfaction, confusion, or a lack of confidence in the consultation process, potentially undermining the impact of OMTs and weakening patient engagement. In addition, while prior studies have focused on behavioral and psychological mechanisms of patient adoption, they have largely overlooked the unique features of the OMT context. Therefore, exploring the factors influencing patient adoption of online medical advice in OMTs is vital for enhancing digital healthcare delivery and improving platform effectiveness.
Patient adoption of online medical advice is understood to be influenced by the multi-doctor involvement in OMTs. Multi-doctor involvement represents a core feature of team-based online consultations and shows a fundamental transformation from individual to collaborative models of digital healthcare delivery. In team-based consultations, multiple doctors work collaboratively to assess patient concerns and deliver more comprehensive guidance. Specifically, doctor collaboration in OMTs often follows an open and voluntary model, in which one doctor initiates the response and other team members subsequently contribute complementary knowledge [3]. This process allows patients to access diverse clinical perspectives, compare alternative recommendations, and select the advice that best fits their condition. Such interaction not only improves the perceived professionalism and trustworthiness of the medical guidance but also helps reduce ambiguity, thereby increasing the patient adoption of medical advice [4]. Additionally, prior studies have demonstrated the theoretical significance and practical effectiveness of multi-doctor involvement in online healthcare settings [1]. However, existing research has predominantly focused on outcomes such as team performance [5] or patient satisfaction [6], with limited attention to how multi-doctor involvement influences patient behaviors, particularly their decision to adopt online medical advice. Given the increasing prevalence of OMTs and the broader shift toward collaborative care models in digital health platforms, it is necessary to investigate whether and how multi-doctor involvement influences patient decision-making in this context.
Beyond multi-doctor involvement, team composition and illness characteristics may also shape patient adoption of medical advice. Team composition reflects team diversity in OMTs. Team composition reflects the internal diversity and functional structure of OMTs, which can significantly affect how patients perceive the credibility, comprehensiveness, and satisfaction of medical consultations [4]. For instance, leadership participation is often associated with higher professional titles or senior positions with greater clinical authority and experience. Patients tend to place greater trust in advice provided or endorsed by such authoritative figures, increasing the likelihood of adoption [1]. Similarly, disciplinary diversity refers to the involvement of doctors from different specialties, which enables the delivery of more personalized medical advice [7]. This diversity not only improves the informational richness of the consultation but also enhances the perceived value of the advice, thereby promoting patient adherence. Besides, illness characteristics such as illness complexity may play a critical role in shaping patient adoption of medical advice. Patients with more complex or uncertain conditions may be more sensitive to how well the team’s advice addresses their specific concerns, which in turn affects their adoption behavior [8]. Considering this, our research questions are the following:
- RQ1. Does multi-doctor involvement facilitate patient adoption of medical advice?
- RQ2. Is the impact of multi-doctor involvement on patient adoption of medical advice contingent on team composition and illness characteristics?
To address the proposed research questions, this study investigates how multi-doctor involvement in OMTs influences patient adoption of medical advice, with particular attention to the moderating roles of leader participation, disciplinary diversity, and illness complexity. We empirically test our model using data from one of China’s leading online healthcare platforms. The dataset comprises 107,860 consultation records from 2180 OMTs and 8689 doctors, spanning the period from 2017 to 2023. The results indicate that multi-doctor involvement significantly enhances patient adoption of medical advice. Furthermore, this relationship is positively moderated by both leader participation and disciplinary diversity, while illness complexity shows no significant moderating effect.
Our study offers several theoretical contributions. First, it is the first to empirically investigate how multi-doctor involvement influences patient adoption of medical advice, enriching our understanding of patient decision-making in online healthcare settings. Second, it identifies leader participation and disciplinary diversity as significant moderators in this relationship, while illness complexity finds no significance, thereby clarifying the boundary conditions under which multi-doctor involvement affects patient adoption of medical advice.
Furthermore, the study provides practical insights for OHC platforms managers. First, given the positive effect of multi-doctor involvement, platforms should implement tools and features that facilitate team formation and visible collaborative responses to enhance patient trust and engagement. Second, platforms should prioritize assigning experienced leaders and promoting disciplinary diversity within teams to improve the coherence and reliability of medical advice. Policies or algorithms that support such team structures can significantly improve the effectiveness of online medical teams and increase patient adoption of medical advice.
2. Literature Review
2.1. Online Medical Teams
As work processes become increasingly decentralized and globalized, many organizations have adopted virtual teams to navigate dynamic environments. Virtual teams—distributed groups that collaborate via electronic media such as email and instant messaging—are not a binary classification but rather a dimensional attribute of team organization [9]. While virtual teams enable the integration of diverse resources to achieve organizational goals, they also face challenges such as communication barriers and difficulties in building trust [10]. Various factors—including technology, culture, trust, and affect—can influence the processes and outcomes of virtual collaboration [11]. This study extends the exploration of virtual teams by focusing on their effectiveness in e-health platforms.
OHCs refer to online systems that integrate and deliver medical services and health management through technologies such as telemedicine and electronic health records [12,13]. Researchers have explored these systems from various perspectives, including how platforms offering social support and empowerment influence doctor-patient relationships [14]. Interpersonal interactions within the platform are also found to enhance patient trust in and satisfaction with doctors [15]. With the rapid development of OHC, virtual organizations have emerged in large numbers. Among these, OMTs have become a core organizational form within OHCs. OMTs typically consist of multiple doctors and assistants who collaborate across hierarchical levels to provide remote consultations and formulate medical recommendations [16]. Distinct from traditional one-on-one consultations, OMTs are characterized by “multi-doctor collaboration on a single patient case,” emphasizing interprofessional integration and team-based care [17].
Scholars have examined OMTs from multiple perspectives. Ref. [18] demonstrated that both intrinsic and extrinsic motivations, along with social interactions, influence doctor participation in OMTs. Some studies focus on team-level characteristics. For instance, Yang et al. (2021) [5] showed that both reputation diversity and experience diversity positively affect team performance, and highlighted the impact of “star doctors”. Other work has explored how intra-team disparities in departments and titles affect team dissolution [19]. Additional research investigates the dual-role phenomenon—where doctors engage in both team-based and individual online consultations—and its “spillover effects” on personal performance. For example, team capital (i.e., status and decision-making power) and peer effects among doctors have been found to significantly influence individual online performance [1,20]. Ref. [21] also demonstrated that benevolence, integrity, and competence displayed during OMT participation impact personal performance.
A parallel stream of research focuses on patients. Ref. [22] found that responses from multiple doctors significantly improve patient satisfaction, moderated by team composition and response quality, while delayed replies undermine satisfaction [4]. Participation in OMTs also affects the linguistic concreteness and emotional intensity of doctor-patient communication, which in turn influences patient satisfaction. While existing studies have primarily examined patient satisfaction, little attention has been paid to how OMTs influence patient adoption of medical advice. Compared to patient satisfaction, patient adoption is the behavioral outcome in online consultations, reflecting whether patients absorb professional knowledge that can improve their health. This study aims to address this gap.
2.2. Patient Adoption of Online Medical Advice
Information adoption refers to the process by which individuals accept and internalize information, subsequently influencing their attitudes or behaviors [23]. Theories in information systems and behavioral science have proposed several models to explain adoption behaviors, among which the Information Adoption Model (IAM) is particularly influential. IAM integrates elements from the Technology Acceptance Model (TAM) and the Elaboration Likelihood Model (ELM). According to IAM, the level of elaboration determines the persuasion route: deep processing activates the central route, emphasizing argument quality, while shallow processing triggers the peripheral route, relying on source credibility [24].
Online medical advice adoption has become a major focus in health informatics [25,26]. Numerous studies, grounded in IAM and related theories, have examined various factors that influence patient adoption of online medical advice. These factors can be categorized into several dimensions, as follows: information quality and source credibility [27,28], emotional support [29,30,31], as well as contextual moderators such as time pressure [32] and illness privacy [33]. In terms of patient engagement, studies have shown that patient empowerment, satisfaction with doctors, and commitment positively influence treatment compliance [34]. Other research has found that online medical advice presented in a structured sequence is more likely to be adopted by patients [29]. The links between social support, engagement behaviors [35,36], and treatment compliance have also been validated [37], as well as the impact of patients’ information-seeking styles on their adherence [38].
Building on the above review, existing research has primarily explored patient information adoption through behavioral and psychological mechanisms, yet has overlooked the distinct features of the OMT context compared to traditional one-on-one consultations, as well as the additional factors introduced by team-based care. So, this study addresses gaps in the OMTs context by examining two categories of factors influencing patient adoption: individual-level illness complexity and team-level characteristics, including disciplinary diversity and the presence of team leadership—dimensions that remain underexplored in existing literature. Unlike individual consultations, OMTs offer collaborative medical recommendations from multiple doctors, providing comprehensive professional support for complex cases. This model also introduces new variables that may influence patient adoption, for instance, the presence of a team leader and the disciplinary diversity. Prior research suggests that team leaders influence cognitive, motivational, emotional, and coordination processes within teams, thereby enhancing performance [39,40]. Reputable and expert members can foster creativity and engagement among team members [41], although power-holding individuals may also overestimate their own judgment and discount others’ input, potentially impairing team decisions [42]. Accordingly, the impact of team leadership on patient adoption behavior in OMTs warrants further investigation. Similarly, team diversity may shape patient perceptions and decision-making. While some studies suggest that diverse perspectives enhance innovation and decision quality, others highlight risks such as relational conflict [43]. Ref. [5] found that experience diversity improves OMT performance, but given the differences in measurement and focus, further research is needed to explore how disciplinary diversity influences patient adoption of medical advice.
Another critical factor is the complexity of the patient’s illness. Research shows that patient adherence tends to increase with illness severity [44]. Patients with more serious conditions are also more likely to actively seek health information [45], and benefit more from doctor support in terms of satisfaction [46]. Moreover, severely ill patients react more strongly to perceived doctor unfairness [47]. Existing studies have examined the differential effects of disease types—such as physical vs. psychological conditions [48,49], and chronic illnesses [50,51,52,53]—within OHCs. However, unlike traditional one-on-one consultations, OMTs involve doctors from multiple departments collaborating on complex cases, making it difficult to classify them under a single disease category. Therefore, existing typologies of disease types are not well-suited for the OMT context. Building on these findings, this study examines how disease complexity moderates the adoption of online medical advice. Finally, regarding measurement, prior studies have typically relied on dichotomous variables [27] or Likert scales [28,30] to capture adoption. While useful, these approaches introduce a degree of subjectivity. To enhance measurement accuracy, this study constructs a domain-specific adoption dictionary through multi-round manual coding, enabling high-precision text-based identification and quantification of patient behavior.
2.3. Summary
This study is situated at the intersection of research on virtual teams and information adoption, focusing on how patients adopt medical advice in the context of OMTs. While previous research has examined the organizational structure and performance of OMTs and identified key adoption antecedents such as information quality and source credibility, the core behavioral outcome—adoption itself—has been underexplored. Moreover, existing studies on patient adoption often assume a one-on-one consultation model, providing limited insight into the collaborative dynamics of multi-doctor consultations.
In highly collaborative OMT settings, the roles and characteristics of team members may significantly influence patient adoption behavior. Additionally, patient-level factors, especially condition complexity, may moderate how patients process and respond to medical advice. Methodologically, it advances the literature by introducing a high-precision, text-based adoption measurement approach. By combining insights from the virtual team and information adoption literature, this study identifies critical influencing factors within OMTs and introduces a novel measurement strategy, contributing to a deeper theoretical understanding and more precise behavioral analysis of patient adoption mechanisms. Figure 1 presents a summary of the research gap.
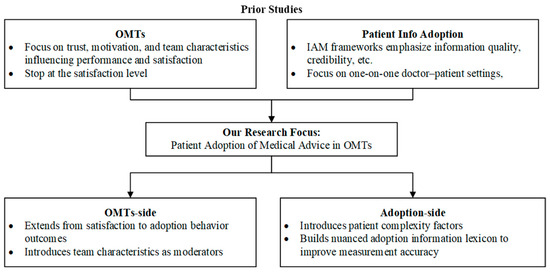
Figure 1.
Summary of the Literature Review.
3. Development of Hypotheses
This study examines how multi-doctor involvement within OMTs affects patients’ adoption of medical advice. Drawing on prior research in OMTs and digital health behavior, we develop a conceptual model that integrates both team-level and patient-level factors to explain the factors of patient adoption of medical care.
At the core of our framework is multi-doctor involvement, which reflects the shift from single-doctor consultations to collaborative, team-based care. This construct captures the extent of professional collaboration among doctors and serves as a key predictor of patient behavior [1]. When multiple doctors are involved, patients are exposed to diverse medical perspectives, which helps reduce ambiguity and increase the credibility of the advice. Therefore, we suggest that the multi-doctor involvement enhances both the informational richness and perceived reliability, thereby increasing the patient adoption of medical advice.
To explore the conditions under which this effect becomes more or less pronounced, we incorporate three moderating variables into our model. At the team level, leader participation presents the engagement of senior or specialized doctors who enhance the credibility and coherence of the team’s medical recommendations. When such figures are actively involved in the consultation, their collaboration reinforces the perceived authority of the advice, thereby strengthening the positive relationship between multi-doctor involvement and patient adoption. Meanwhile, disciplinary diversity captures the range of medical specialties represented within the team, enabling more comprehensive and multidimensional responses to patient concerns. Therefore, a broader disciplinary consultation might enhance the positive impact of multi-doctor involvement on patient adoption. At the patient level, we examine illness complexity, which reflects the extent to which a patient’s condition involves multiple symptom descriptions or diagnostic uncertainty. In such cases, patients may rely more heavily on diverse expertise to make decisions. As a result, we propose that illness complexity reinforces the positive effect of multi-doctor involvement on the patient adoption of medical advice.
In summary, this framework enables a nuanced investigation of both the direct influence of multi-doctor involvement on patient adoption and the boundary conditions that shape its effectiveness. The model also offers practical insights on online health communities, team structure, and patient decision-making in digital care environments, as illustrated in Figure 2.
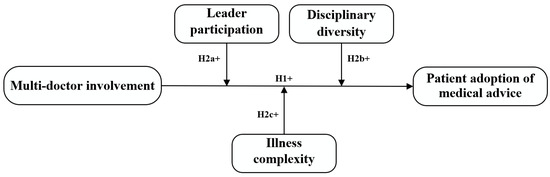
Figure 2.
Research model.
3.1. Multi-Doctor Involvement and Patient Adoption of Online Medical Advice
The core mission of OTC is to enhance the capacity for diagnosing and managing patient illness conditions through multidisciplinary medical expertise, thereby delivering high-quality care [5]. The participation of multiple doctors in an OTC enhances the diversity of expertise and perspectives available to the patient, which can improve the comprehensiveness and credibility of medical recommendations [54]. The presence of multiple doctors signals a higher level of professional commitment and collective decision-making, which may strengthen patient trust and confidence in the recommendations provided [6]. As a result, patients are more inclined to accept and follow medical advice when multiple doctors actively contribute to the consultation. Given this, we posit the following hypothesis.
H1.
Multi-doctor involvement positively influences patient adoption of medical advice.
3.2. Moderating Effects
Leader participation. Within OMTs, leaders typically represent the most experienced and clinically proficient members. Their direct participation in patient consultations and provision of medical recommendations plays a pivotal role in delivering high-quality OTC and ensuring diagnostic accuracy [55]. Furthermore, as figures of authority who command substantial patient trust and credibility, OMT leaders may significantly enhance patient compliance. We therefore hypothesize that patient willingness to adopt team-based treatment recommendations increases when the OMT leader actively participates in the consultation process. As such, we posit the following hypothesis.
H2a.
Leader participation positively moderates the relationship between multi-doctor involvement and patient adoption of medical advice.
Disciplinary diversity. During OTCs, the management of complex medical conditions frequently necessitates the integration of multidisciplinary expertise. This collaborative knowledge synthesis provides critical cognitive support for problem-solving and yields more comprehensive clinical perspectives [6]. Collaboration among professionals from diverse disciplines leverages a wider range of expertise than homogeneous teamwork, ultimately enhancing decision-making quality. By integrating multidisciplinary perspectives, this approach combines varied professional knowledge bases, stimulating creative synergies through cross-disciplinary idea exchange. Such intellectual diversity not only generates innovative solutions to complex medical challenges but also optimizes therapeutic outcomes and strengthens diagnostic and problem-solving capabilities [22].
H2b.
Disciplinary diversity positively moderates the relationship between multi-doctor involvement and patient adoption of medical advice.
Illness complexity. Patients seeking OMT consultations present with varying levels of illness severity. Those confronting more advanced or complex conditions typically experience greater clinical uncertainty and psychological distress [8]. This heightened vulnerability may intensify their demand for authoritative medical guidance, particularly from highly specialized and credible sources like OMTs. Within this context, patients with more severe medical conditions demonstrate a heightened need for reliable professional advice, consequently exhibiting a greater propensity to adopt treatment recommendations provided through OMTs, particularly when multiple doctors contribute their expert opinions. We therefore draw the following hypothesis.
H2c.
Illness complexity positively moderates the relationship between multi-doctor involvement and patient adoption of medical advice.
4. Methodology
4.1. Research Context and Data Collection
Data for this study were sourced from a prominent OHC in China, which was launched in 2006 and has attracted over 290,000 doctors serving more than 89 million patients by September 2024. The online medical team service on this OHC commenced in 2017, allowing doctors to initiate their own online medical team or join existing teams formed by their peers. Patients can access and buy team consultation services through a doctor’s homepage, on which a link to the online medical teams that the doctor has joined is provided. In August 2023, we developed a Python 3.9-based web crawler to collect comprehensive information on all OMTs available on the platform. The collected data encompassed dialogue records from online team consultations and information at the team level. After cleaning up the data that had missing values, our dataset involved 107,860 consultations. The time scope of our investigation spanned from 2017 to 2023.
4.2. Measures
The dependent variable in our study is patient adoption of medical advice. Given the absence of objective indicators reflecting whether patients adopt the advice, we employed text analysis to capture this construct, measured by the log-transformed frequency of adoption-related terms appearing in patients’ responses to doctors’ collective recommendations within an OMT. These words are identified using a self-constructed lexicon. To construct a reliable dictionary of adoptive expressions, this study recruited three research assistants. They were informed that the purpose of the annotation was to develop a dictionary related to patients’ health information adoption, without being exposed to any specific hypotheses. In each round, all three assistants independently annotated consultation records from 100 patients. Upon completion of each round, their annotations were aggregated to calculate inter-coder reliability. The team then discussed their coding criteria before proceeding to the next round. If no new adoptive expressions emerged in the subsequent round, the annotation process was concluded; otherwise, additional rounds were conducted. Discrepancies were resolved through systematic discussion and voting among the coders. In the first round of back-to-back annotation, 16 adoptive expressions were identified. A 10% random sample of the annotated data was selected for cross-coding comparison, yielding a kappa coefficient greater than 0.75, indicating acceptable inter-coder reliability. The second round resulted in 18 additional expressions, again meeting the reliability threshold. In the third round, 8 new expressions were identified, followed by 2 in the fourth round. The fifth round produced no new expressions, marking the end of the annotation process. In total, across five iterative rounds, 44 adoptive expressions were identified and annotated. The independent variable, Multi-doctor involvement, is a binary variable where a value of 1 indicates that multiple doctors participated in the OTC, while 0 indicates that only a single doctor was involved. Leader participation reflects the engagement of the OMT’s leading doctor in the consultation, coded as 1 if the leading doctor responded and 0 otherwise. Disciplinary diversity captures the knowledge diversity of the participating doctors; it is assigned a value of 1 if the doctors come from multiple medical departments and 0 if they belong to the same department. Illness complexity refers to the complexity of a patient’s condition, particularly the extent to which it involves multiple symptoms or comorbidities [45]. Following existing literature, we measured it by counting the number of symptom-related words in the patient’s initial inquiry [56]. These symptom-related words are identified using a well-established Chinese medical lexicon, which has been validated in the context of online health services and widely used in previous studies to assess illness characteristics and severity [56]. Several control variables were also incorporated into the model, including patients’ sex (Sex) and age (Age), the online medical team’s size (Team size), and the service price (Price), given that prior research indicates that these factors may significantly influence patient decisions during OTCs [22]. Table 1 summarizes the descriptive statistics of all variables.

Table 1.
Descriptive Statistics.
4.3. Analysis and Results
The models were hierarchically constructed and tested. Model 1 included only control variables; Model 2 incorporated control variables, independent variables, and moderating variables; and Models 3 to 6 explored the moderating effects by integrating the interaction terms. We utilized a linear model for analysis. STATA 17 was used to perform these regressions.
The results are shown in Table 2. From Model 2, we can see that Multi-doctor involvement was positively associated with log adoption (β = 0.017, p < 0.01), which supported H1. In terms of the moderating effects, we found that Leader participation strengthened the impact of Multi-doctor involvement on log adoption (β = 0.010, p < 0.01). Simultaneously, Disciplinary diversity enhanced the effect of Multi-doctor involvement on log adoption (β = 0.008, p < 0.01); thus, H2a and H2b were supported. Furthermore, Illness complexity shows no significant moderating effects (β = 0.000, p > 0.1); thus, H2c is rejected.

Table 2.
Regression results.
4.4. Robustness Checks
We conducted two robustness checks to ensure the reliability of our findings. First, in the primary analysis, we employed log-transformed adoption word counts as the dependent variable measure. For robustness assessment, we altered the specification of the dependent variable by using raw adoption word counts to measure patient adoption of medical advice. As shown in Table 3, the results remain consistent with our prior findings.

Table 3.
Alternative Measurement.
Second, we employed Structural Equation Modeling (SEM) to conduct the analysis, using the SmartPLS software (version 4.0) for model estimation. A bootstrapping procedure with 5000 resamples was performed to assess the significance of the path coefficients. As shown in Table 4 and Figure 3 and Figure 4, the results are consistent with our main findings.

Table 4.
SEM Results (Main Effect), SEM Results (Moderating Effect).
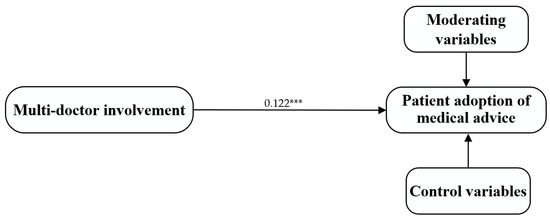
Figure 3.
SEM Results (Main Effect). Notes: *** p < 0.01, ** p < 0.05, * p < 0.1.
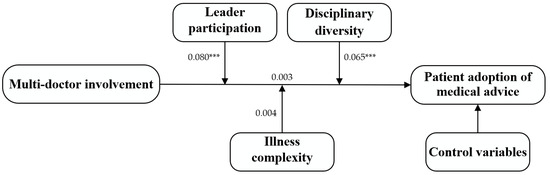
Figure 4.
SEM Results (Moderating Effect). Notes: *** p < 0.01, ** p < 0.05, * p < 0.1.
5. Discussion and Conclusions
5.1. Key Findings
This study investigates how multi-doctor involvement within OMTs influences patient adoption of medical advice and further examines the moderating roles of leader participation, disciplinary diversity, and illness complexity. This study enriches the literature on OMTs and virtual team collaboration in healthcare, offering practical insights for online health platforms to enhance patient compliance and optimize the effectiveness of online medical consultations. Based on the empirical analysis, this study reveals three key findings, as follows:
First, the results demonstrate that multi-doctor involvement has a significant positive effect on patient adoption of medical advice. When multiple doctors engage in an online consultation, patients are more likely to perceive the advice as comprehensive, authoritative, and trustworthy, thereby increasing their likelihood of adopting advice. Previous literature has extensively documented the benefits of doctor collaboration in online medical teams [57], but the focus has primarily been on team performance [20] or patient satisfaction [4]. In contrast, few studies have empirically examined how multi-doctor involvement influences patients’ actual decision-making behaviors in digital consultation settings. Our study addresses this gap by examining the effect of multi-doctor involvement on patient adoption of medical advice.
Second, the study identifies leader participation and disciplinary diversity as key moderators that strengthen the relationship between multi-doctor involvement and patient adoption of medical advice. On the one hand, active participation by team leaders with higher professional authority enhances the coherence and credibility of the consultation, which increases patient confidence and reinforces the effect of collaborative advice, consistent with previous findings [7]. On the other hand, disciplinary diversity brings together doctors from different specialties, enabling more comprehensive and multifaceted responses to patient inquiries. This breadth of expertise improves the informational quality of the consultation and makes the advice more persuasive and actionable for patients, thereby promoting patient adoption of medical advice. These findings are consistent with prior research emphasizing the importance of disciplinary diversity in improving decision quality and patient outcomes in online medical settings [22].
Third, our study examines the role of illness complexity, which has been widely recognized as an important determinant of patient behavior [45]. Interestingly, our results indicate that illness complexity does not significantly moderate the relationship between team collaboration and patient adoption in the context of asynchronous online consultations. This suggests that in asynchronous online consultations, patients lack sufficient contextual and interactive cues to fully comprehend or evaluate the complexity of their condition. Instead, they rely on more visible cues (e.g., doctors’ titles, specialties, and team structure) to assess the credibility of medical advice. Consequently, their likelihood of adopting advice provided by multi-doctor teams remains relatively stable, regardless of perceived illness complexity.
5.2. Theoretical Contributions
This study makes several significant theoretical contributions. First, our study enriches previous research on OMTs. Prior research has primarily examined the impact of multi-doctor involvement on team-level processes [1,55,58] and patient outcomes [4,6], but has paid limited attention to the patient adoption of medical advice. To address this gap, we empirically examine the relationship between multi-doctor involvement and patient adoption behavior. Our findings show that such involvement positively influences patient adoption of medical advice, indicating that collaborative doctor participation can improve patient compliance in OMTs. This insight broadens our understanding of how doctor collaboration affects patient decision-making.
Second, this study identifies leader participation and disciplinary diversity as key moderating factors, thereby uncovering important boundary conditions in the relationship between multi-doctor involvement and patient adoption of medical advice. Specifically, our findings demonstrate that both leader participation and disciplinary diversity strengthen the positive effect of multi-doctor involvement on patient adoption, whereas illness complexity has no significant moderating effect. It suggests that enhancing team leadership [7] and promoting multi-disciplinary collaboration [22] can be effective strategies for improving patient compliance, regardless of case complexity. As OHCs increasingly adopt the OMT model, it becomes essential to understand the contextual factors that condition the effectiveness of multi-doctor involvement in promoting patient adoption. These insights offer practical guidance for optimizing team structures in digital healthcare settings.
5.3. Practical Implications
Our study sheds light on several managerial implications for OHC platform managers. First, the significant positive effect of multi-doctor involvement on patient adoption of medical advice underscores the importance of team-based consultation. To support this, OHC managers should develop system functionalities that facilitate coordinated multi-doctor responses, including tools for assembling consultation teams, co-authoring medical advice, and highlighting collaborative responses within the platform interface. By enhancing the visibility and credibility of multi-doctor input, platforms can improve patient engagement and trust in the advice provided.
Second, given the positive moderating effects of leader participation and disciplinary diversity, platform managers should strategically consider both leadership structure and specialty composition when forming online medical teams. Appointing clear team leaders can enhance the coherence and authority of the consultation. At the same time, including doctors from multiple specialties broadens the team’s expertise and better meets diverse patient needs. Platform-level policies or algorithms that promote such team configurations can strengthen the impact of OMTs and increase patient adoption of medical advice.
5.4. Limitations and Future Research
While this study provides valuable insights into how multi-doctor involvement promotes patient adoption of online medical advice, several limitations should be acknowledged. First, the dataset used in this study was obtained exclusively from one of the largest and most active online healthcare communities in China. Although the platform offers a rich context for examining team-based online consultations, the findings may not be fully generalizable to other platforms, healthcare systems, or cultural settings. Future research could test the robustness of our conclusions by using data from different online health communities or conducting cross-national comparisons to enhance external validity.
Second, this study investigates the factors influencing patients’ adoption of medical advice, focusing on multi-doctor involvement as the primary predictor, with leader participation, disciplinary diversity, and illness complexity as moderating variables. Nevertheless, we acknowledge that other factors—such as patients’ cognitive attitude [59], semantic features of the consultation [22], and privacy concerns (e.g., the privacy paradox) [60]—may also play important roles in shaping patient adoption behavior. Future research could incorporate such factors to develop a more comprehensive understanding of patient decision-making in online healthcare environments.
Third, although our study leverages a large-scale dataset of online medical consultation platforms, the data were obtained through web crawling and represent secondary observational data. While we have conducted robustness checks and controlled for key covariates to reduce potential confounding bias, unobserved factors—such as patients’ disease type, psychological mechanisms, or symptom duration—may still influence their adoption of medical advice [61]. To strengthen causal inference, future research could adopt longitudinal designs, quasi-experimental methods, or a self-reported survey to more precisely identify the causal effects of multi-doctor involvement on patient decision-making.
Author Contributions
Conceptualization, X.Z. and S.W.; methodology, S.W.; software, S.W.; validation, S.W.; formal analysis, X.Z. and S.W.; investigation, X.Z. and S.W.; resources, X.Z. and S.W.; data curation, X.Z. and S.W.; writing—original draft preparation, S.W., L.Z., C.F., X.Z. and D.H.; writing—reviewing and editing, S.W., L.Z., C.F., X.Z. and D.H.; visualization, S.W., C.F., L.Z., X.Z. and D.H.; supervision, L.Z., X.Z. and D.H.; project administration, X.Z. and D.H.; funding acquisition, D.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Natural Science Foundation grant number 72202108 and 72271131, and MOE Humanities and Social Sciences Research Planning Fund grant number 24YJA630128.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Zhang, X.; Pu, J.; Lu, Y.; Guo, F. Team makes you better: Evidence from online medical consultation platforms. Inf. Syst. Res. 2025. [Google Scholar] [CrossRef]
- Zhang, X.; Lai, K.-H.; Guo, X. Promoting China’s mHealth market: A policy perspective. Health Policy Technol. 2017, 6, 383–388. [Google Scholar] [CrossRef]
- Tan, H.; Zhang, X.; Yang, Y. Satisfaction or gratitude? Exploring the disparate effects of physicians’ knowledge sharing on patients’ service evaluation in online medical consultations. Inf. Syst. J. 2023, 33, 1186–1211. [Google Scholar] [CrossRef]
- Zhang, Y.; Sun, F.; Zhang, X.; Ma, X. Are multiple information sources better? The effect of multiple physicians in online medical teams on patient satisfaction. Inf. Process. Manag. 2025, 62, 103889. [Google Scholar] [CrossRef]
- Yang, H.; Yan, Z.; Jia, L.; Liang, H. The impact of team diversity on physician teams’ performance in online health communities. Inf. Process. Manag. 2021, 58, 102421. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, X. Exploring the impact of team engagement on patient satisfaction: Insights from social support and transactive memory system. Aslib J. Inf. Manag. 2024. [Google Scholar] [CrossRef]
- Du, W.; Liu, W.; Guo, X.; Vogel, D. How team diversity influences online medical team service performance through shared leadership: An input-process-output perspective. Group Decis. Negot. 2024, 33, 27–54. [Google Scholar] [CrossRef]
- Li, J.; Tang, J.; Yen, D.C.; Liu, X. Disease risk and its moderating effect on the e-consultation market offline and online signals. Inf. Technol. People 2019, 32, 1065–1084. [Google Scholar] [CrossRef]
- Hertel, G.; Geister, S.; Konradt, U. Managing virtual teams: A review of current empirical research. Hum. Resour. Manag. Rev. 2005, 15, 69–95. [Google Scholar] [CrossRef]
- Dulebohn, J.H.; Hoch, J.E. Virtual teams in organizations. Hum. Resour. Manag. Rev. 2017, 27, 569–574. [Google Scholar] [CrossRef]
- Martins, L.L.; Gilson, L.L.; Maynard, M.T. Virtual Teams: What do we know and where do we go from here? J. Manag. 2004, 30, 805–835. [Google Scholar] [CrossRef]
- Wu, H.; Lu, N. Service provision, pricing, and patient satisfaction in online health communities. Int. J. Med. Inform. 2018, 110, 77–89. [Google Scholar] [CrossRef]
- Yan, Z.; Wang, T.; Chen, Y.; Zhang, H. Knowledge sharing in online health communities: A social exchange theory perspective. Inf. Manag. 2016, 53, 643–653. [Google Scholar] [CrossRef]
- Audrain-Pontevia, A.-F.; Menvielle, L. Do online health communities enhance patient–physician relationship? An assessment of the impact of social support and patient empowerment. Health Serv. Manag. Res. 2018, 31, 154–162. [Google Scholar] [CrossRef]
- Audrain-Pontevia, A.-F.; Menvielle, L. Effects of interpersonal trust among users of online health communities on patient trust in and satisfaction with their physician. Int. J. Technol. Assess. Health Care 2018, 34, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Zhang, X.; Wang, W.H.; You, X. How online healthcare team evolve into organization: A social network analysis. Digit. Health 2024, 10. [Google Scholar] [CrossRef]
- Li, J.; Wu, H.; Deng, Z.; Lu, N.; Evans, R.; Xia, C. How professional capital and team heterogeneity affect the demands of online team-based medical service. BMC Med. Inform. Decis. Mak. 2019, 19, 119. [Google Scholar] [CrossRef]
- Liu, H.; Perera, S.C.; Wang, J.-J.; Leonhardt, J.M. Physician engagement in online medical teams: A multilevel investigation. J. Bus. Res. 2023, 157, 113588. [Google Scholar] [CrossRef]
- Li, J.; Wu, H.; Deng, Z.; Evans, R.D.; Hong, Z.; Liu, S. Why online medical teams disband? The role of team diversity and leadership type. Inf. Technol. People 2021, 34, 1175–1199. [Google Scholar] [CrossRef]
- Wang, J.-J.; Liu, H.; Ye, J. The impact of individual and team professional capital on physicians’ performance in online health-care communities: A cross-level investigation. Internet Res. 2023, 33, 152–177. [Google Scholar] [CrossRef]
- Du, W.; Guo, X.; Wu, T.; Liu, W.; Vogel, D. The impact of online medical team participation on physicians’ individual online service. Electron. Commer. Res. Appl. 2024, 68, 101468. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, X. Exploring the impact of online medical team engagement on patient satisfaction: A semantic features perspective. Healthcare 2024, 12, 1113. [Google Scholar] [CrossRef]
- Wang, Y. Information adoption model, a review of the literature. J. Econ. Bus. Manag. 2016, 4, 618–622. [Google Scholar] [CrossRef]
- Sussman, S.W.; Siegal, W.S. Informational influence in organizations: An integrated approach to knowledge adoption. Inf. Syst. Res. 2003, 14, 47–65. [Google Scholar] [CrossRef]
- Yang, Y.; Zhu, X.; Song, R.; Zhang, X.; Guo, F. Not just for the money? An examination of the motives behind physicians’ sharing of paid health information. J. Inf. Sci. 2023, 49, 145–163. [Google Scholar] [CrossRef]
- Guo, F.; Zhou, A.; Zhang, X.; Xu, X.; Liu, X. Fighting rumors to fight COVID-19: Investigating rumor belief and sharing on social media during the pandemic. Comput. Hum. Behav. 2023, 139, 107521. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, X.; Fan, W. User adoption of physician’s replies in an online health community: An empirical study. J. Assoc. Inf. Sci. Technol. 2020, 71, 1179–1191. [Google Scholar] [CrossRef]
- Zhou, T. Understanding online health community users’ information adoption intention: An elaboration likelihood model perspective. Online Inf. Rev. 2022, 46, 134–146. [Google Scholar] [CrossRef]
- Wu, B.; Liu, Q.B.; Guo, X.; Yang, C. Investigating patients’ adoption of online medical advice. Decis. Support Syst. 2024, 176, 114050. [Google Scholar] [CrossRef]
- Fan, H.; Lederman, R. Online health communities: How do community members build the trust required to adopt information and form close relationships? Eur. J. Inf. Syst. 2018, 27, 62–89. [Google Scholar] [CrossRef]
- Jin, J.; Yan, X.; Li, Y.; Li, Y. How users adopt healthcare information: An empirical study of an online Q&A community. Int. J. Med. Inform. 2016, 86, 91–103. [Google Scholar] [CrossRef]
- Chou, C.-H.; Wang, Y.-S.; Tang, T.-I. Exploring the determinants of knowledge adoption in virtual communities: A social influence perspective. Int. J. Inf. Manag. 2015, 35, 364–376. [Google Scholar] [CrossRef]
- Li, C.-R.; Zhang, E.; Han, J.-T. Adoption of online follow-up service by patients: An empirical study based on the elaboration likelihood model. Comput. Hum. Behav. 2021, 114, 106581. [Google Scholar] [CrossRef]
- Audrain-Pontevia, A.-F.; Menvielle, L.; Ertz, M. Effects of three antecedents of patient compliance for users of peer-to-peer online health communities: Cross-sectional study. J. Med. Internet Res. 2019, 21, e14006. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhao, K.; Street, N. Social Support and User Engagement in Online Health Communities; Springer International Publishing: Cham, Switzerland, 2014; pp. 97–110. [Google Scholar]
- Wang, X.; Zhao, K.; Street, N. Analyzing and predicting user participations in online health communities: A social support perspective. J. Med. Internet Res. 2017, 19, e130. [Google Scholar] [CrossRef]
- Tewari, S.P.; Misra, R.; Nagdev, K.; Sharma, H. Role of online health communities in patient compliance: A social support perspective. J. Syst. Inf. Technol. 2024, 26, 562–585. [Google Scholar] [CrossRef]
- Lu, X. The effects of patient health information seeking in online health communities on patient compliance in China: Social Perspective. J. Med. Internet Res. 2023, 25, e38848. [Google Scholar] [CrossRef]
- Zaccaro, S.J.; Rittman, A.L.; Marks, M.A. Team leadership. Leadersh. Q. 2001, 12, 451–483. [Google Scholar] [CrossRef]
- Schaubroeck, J.; Lam, S.S.K.; Peng, A.C. Cognition-based and affect-based trust as mediators of leader behavior influences on team performance. J. Appl. Psychol. 2011, 96, 863–871. [Google Scholar] [CrossRef]
- Zhang, X.; Bartol, K.M. Linking empowering leadership and employee creativity: The influence of psychological empowerment, intrinsic motivation, and creative process engagement. Acad. Manag. J. 2010, 53, 107–128. [Google Scholar] [CrossRef]
- See, K.E.; Morrison, E.W.; Rothman, N.B.; Soll, J.B. The detrimental effects of power on confidence, advice taking, and accuracy. Organ. Behav. Hum. Decis. Process. 2011, 116, 272–285. [Google Scholar] [CrossRef]
- Verwijs, C.; Russo, D. The Double-edged sword of diversity: How diversity, conflict, and psychological safety impact software teams. IEEE Trans. Softw. Eng. 2024, 50, 141–157. [Google Scholar] [CrossRef]
- Dimatteo, M.R.; Haskard, K.B.; Williams, S.L. Health beliefs, disease severity, and patient adherence. Med. Care 2007, 45, 521–528. [Google Scholar] [CrossRef]
- Alasmari, A.; Zhou, L. Share to Seek: The effects of disease complexity on health information—Seeking behavior. J. Med. Internet Res. 2021, 23, e21642. [Google Scholar] [CrossRef]
- Chen, S.; Guo, X.; Wu, T.; Ju, X. Exploring the online doctor-patient interaction on patient satisfaction based on text mining and empirical analysis. Inf. Process. Manag. 2020, 57, 102253. [Google Scholar] [CrossRef]
- Zhang, X.; Guo, X.; Lai, K.-h.; Yi, W. How does online interactional unfairness matter for patient–doctor relationship quality in online health consultation? The contingencies of professional seniority and disease severity. Eur. J. Inf. Syst. 2018, 28, 336–354. [Google Scholar] [CrossRef]
- Yao, Z.; Ni, Z.; Zhang, B.; Du, J. Do informational and emotional elements differ between online psychological and Physiological disease communities in China? A comparative study of depression and diabetes. Int. J. Environ. Res. Public Health 2022, 19, 2167. [Google Scholar] [CrossRef]
- Jing, L.; Shan, W.; Evans, R.; Shi, X. To continue consultation or not? How physicians’ information cues affect patients continued online consultation behavior. Electron. Commer. Res. 2024. [Google Scholar] [CrossRef]
- Green, B.M.; Van Horn, K.T.; Gupte, K.; Evans, M.; Hayes, S.; Bhowmick, A. Assessment of adaptive engagement and support model for people with chronic health conditions in online health communities: Combined content analysis. J. Med. Internet Res. 2020, 22, e17338. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-J.; Chen, Y.-M.; Talley, P.C.; Kuo, K.-M. Does online community participation contribute to medication adherence? An empirical study of patients with chronic diseases. Int. J. Environ. Res. Public Health 2021, 18, 5100. [Google Scholar] [CrossRef]
- Vainauskienė, V.; Vaitkienė, R. Foresight study on online health community: The perspective of knowledge empowerment for patients with chronic diseases. Int. J. Health Plan. Manag. 2022, 37, 2354–2375. [Google Scholar] [CrossRef]
- Willis, E.; Royne, M.B. Online health communities and chronic disease self-management. Health Commun. 2017, 32, 269–278. [Google Scholar] [CrossRef]
- Rosell, L.; Alexandersson, N.; Hagberg, O.; Nilbert, M. Benefits, barriers and opinions on multidisciplinary team meetings: A survey in Swedish cancer care. BMC Health Serv. Res. 2018, 18, 249. [Google Scholar] [CrossRef]
- Wang, S. Knowledge collaboration and online medical teams’ performance: A multiple participation perspective. Int. J. Product. Perform. Manag. 2024, 73, 3213–3230. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, X.; Meng, F. Convergent or not? The effect of linguistic convergence on the effectiveness of online physician-patient communication. Ind. Manag. Data Syst. 2025, 125, 875–898. [Google Scholar] [CrossRef]
- Zhou, L.; Sun, F.; Yang, B.; Zhang, X. The Effect of Physician Collaboration on Consultation Efficiency in Online Medical Teams; Springer Nature: Cham, Switzerland, 2025; pp. 62–73. [Google Scholar]
- Liu, H.; Perera, S.C.; Wang, J.-J. Does the physicians’ medical team joining behavior affect their performance on an online healthcare platform? Evidence from two quasi-experiments. Transp. Res. Part E Logist. Transp. Rev. 2023, 171, 103040. [Google Scholar] [CrossRef]
- Wang, L.; Wu, T.; Guo, X.; Zhang, X.; Li, Y.; Wang, W. Exploring mHealth monitoring service acceptance from a service characteristics perspective. Electron. Commer. Res. Appl. 2018, 30, 159–168. [Google Scholar] [CrossRef]
- Zhang, X.; Guo, X.; Guo, F.; Lai, K.-H. Nonlinearities in personalization-privacy paradox in mHealth adoption: The mediating role of perceived usefulness and attitude. Technol. Health Care 2014, 22, 515–529. [Google Scholar] [CrossRef]
- Liu, J.; Kong, J.; Zhang, X. Study on differences between patients with physiological and psychological diseases in online health communities: Topic analysis and sentiment analysis. Int. J. Environ. Res. Public Health 2020, 17, 1508. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).