Determinants of Indoor NO2 and PM2.5 Concentration in Senior Housing with Gas Stoves
Abstract
:1. Introduction
1.1. Nitrogen Dioxide
1.2. Particulate Matter
1.3. Gas Stoves’ Impact on Indoor NO2 and PM2.5
2. Materials and Methods
2.1. Environmental Sampling
2.2. Statistical Analysis
3. Results
3.1. Characteristics of Participants and Homes
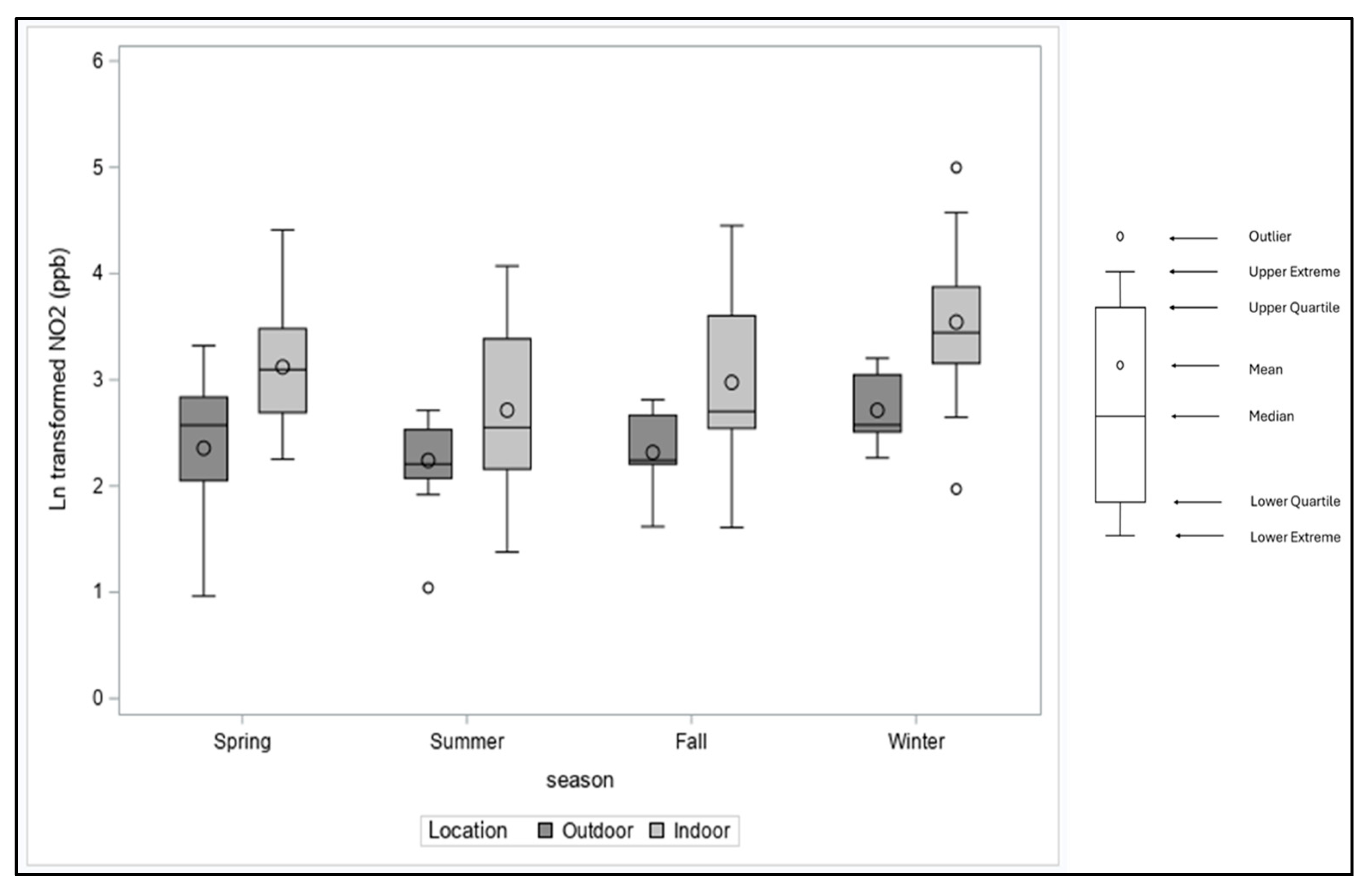
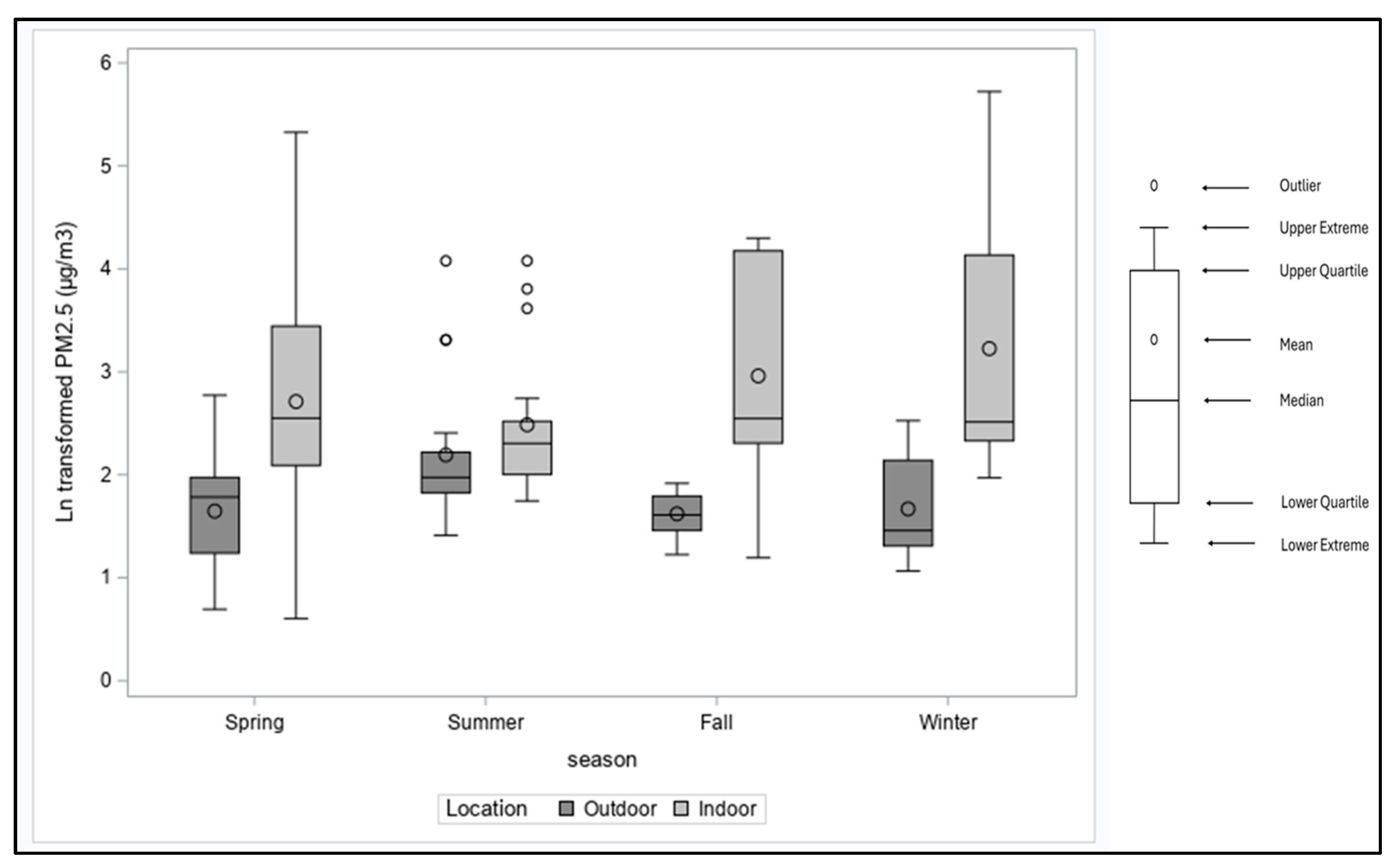
3.2. Indoor and Outdoor NO2 and PM2.5 Concentrations
3.3. Predictors of Indoor NO2 and PM2.5
4. Discussion
4.1. Stove Usage Impact on Indoor NO2 and PM2.5
4.2. Seasonal Variation in NO2 and PM2.5
4.3. Other Factors That Influence Indoor NO2 and PM2.5
4.4. Potential Interventions
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tham, K.W. Indoor air quality and its effects on humans—A review of challenges and developments in the last 30 years. Energy Build. 2016, 130, 637–650. [Google Scholar] [CrossRef]
- Jones, A.P. Indoor air quality and health. Atmos. Environ. 1999, 33, 4535–4564. [Google Scholar] [CrossRef]
- Seguel, J.M.; Merrill, R.; Seguel, D.; Campagna, A.C. Indoor Air Quality. Am. J. Lifestyle Med. 2017, 11, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Ole Fanger, P. What is IAQ? Indoor Air 2006, 16, 328–334. [Google Scholar] [CrossRef]
- Cincinelli, A.; Martellini, T. Indoor Air Quality and Health. Int. J. Environ. Res. Public Health 2017, 14, 1286. [Google Scholar] [CrossRef]
- United States, Environmental Protection Agency (U.S E.P.A). National Ambient Air Quality Standards (NAAQS) Table; EPA: Washington, DC, USA, 2023.
- Sundell, J. On the history of indoor air quality and health. Indoor Air 2004, 14, 51–58. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Giagloglou, E.; Steinle, S.; Davis, A.; Sleeuwenhoek, A.; Galea, K.S.; Dixon, K.; Crawford, J.O. Indoor Exposure to Selected Air Pollutants in the Home Environment: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8972. [Google Scholar] [CrossRef]
- Gilbert, N.L.; Gauvin, D.; Guay, M.; Héroux, M.E.; Dupuis, G.; Legris, M.; Chan, C.C.; Dietz, R.N.; Lévesque, B. Housing characteristics and indoor concentrations of nitrogen dioxide and formaldehyde in Quebec City, Canada. Environ. Res. 2006, 102, 1–8. [Google Scholar] [CrossRef]
- Nicole, W. Cooking up indoor air pollution: Emissions from natural gas stoves. Environ. Health Perspect. 2014, 122, A27. [Google Scholar] [CrossRef]
- Schlesinger, R.B.; Lippmann, M. Nitrogen oxides. Environ. Toxic. 2020, 721–781. [Google Scholar] [CrossRef]
- Balmes, J.R.; Holm, S.M.; McCormack, M.C.; Hansel, N.N.; Gerald, L.B.; Krishnan, J.A. Cooking with Natural Gas: Just the Facts, Please. Am. J. Respir. Crit. Care Med. 2023, 207, 996–997. [Google Scholar] [CrossRef] [PubMed]
- Belanger, K.; Gent, J.F.; Triche, E.W.; Bracken, M.B.; Leaderer, B.P. Association of Indoor Nitrogen Dioxide Exposure with Respiratory Symptoms in Children with Asthma. Am. J. Respir. Crit. Care Med. 2006, 173, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Hansel, N.N.; Breysse, P.N.; McCormack, M.C.; Matsui, E.C.; Curtin-Brosnan, J.; Williams, D.L.; Moore, J.L.; Cuhran, J.L.; Diette, G.B. A longitudinal study of indoor nitrogen dioxide levels and respiratory symptoms in inner-city children with asthma. Environ. Health Perspect. 2008, 116, 1428–1432. [Google Scholar] [CrossRef]
- Keet, C.A.; Keller, J.P.; Peng, R.D. Long-Term Coarse Particulate Matter Exposure Is Associated with Asthma among Children in Medicaid. Am. J. Respir. Crit. Care Med. 2018, 197, 737–746. [Google Scholar] [CrossRef]
- Xu, X.; Zhang, J.; Yang, X.; Zhang, Y.; Chen, Z. The Role and Potential Pathogenic Mechanism of Particulate Matter in Childhood Asthma: A Review and Perspective. J. Immunol. Res. 2020, 2020, 8254909. [Google Scholar] [CrossRef]
- Kim, S.-H.; Yang, H.-J.; Jang, A.-S.; Kim, S.-H.; Song, W.-J.; Kim, T.-B.; Ye, Y.-M.; Yoo, Y.; Yu, J.; Yoon, J.-S.; et al. Effects of particulate matter in ambient air on the development and control of asthma. Allergy Asthma Amp Respir. Dis. 2015, 3, 313. [Google Scholar] [CrossRef]
- Kang, I.; McCreery, A.; Azimi, P.; Gramigna, A.; Baca, G.; Hayes, W.; Crowder, T.; Scheu, R.; Evens, A.; Stephens, B. Impacts of residential indoor air quality and environmental risk factors on adult asthma-related health outcomes in Chicago, IL. J. Expo. Sci. Environ. Epidemiol. 2023, 33, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Hesterberg, T.W.; Bunn, W.B.; McClellan, R.O.; Hamade, A.K.; Long, C.M.; Valberg, P.A. Critical review of the human data on short-term nitrogen dioxide (NO2) exposures: Evidence for NO2 no-effect levels. Crit. Rev. Toxicol. 2009, 39, 743–781. [Google Scholar] [CrossRef]
- Tong, X.; Wang, B.; Dai, W.-T.; Cao, J.-J.; Ho, S.S.H.; Kwok, T.C.Y.; Lui, K.-H.; Lo, C.-M.; Ho, K.F. Indoor air pollutant exposure and determinant factors controlling household air quality for elderly people in Hong Kong. Air Qual. Atmos. Health 2018, 11, 695–704. [Google Scholar] [CrossRef]
- Lim, J.-M.; Jeong, J.-H.; Lee, J.-H.; Moon, J.-H.; Chung, Y.-S.; Kim, K.-H. The analysis of PM2.5 and associated elements and their indoor/outdoor pollution status in an urban area. Indoor Air 2011, 21, 145–155. [Google Scholar] [CrossRef]
- Lim, Y.H.; Hersoug, L.G.; Lund, R.; Bruunsgaard, H.; Ketzel, M.; Brandt, J.; Jørgensen, J.T.; Westendorp, R.; Andersen, Z.J.; Loft, S. Inflammatory markers and lung function in relation to indoor and ambient air pollution. Int. J. Hyg. Env. Health 2022, 241, 113944. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Wen, Q.; Zhang, R. Sources, health effects and control strategies of indoor fine particulate matter (PM2.5): A review. Sci. Total Environ. 2017, 586, 610–622. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Ou, C.; Magana-Arachchi, D.; Vithanage, M.; Vanka, K.S.; Palanisami, T.; Masakorala, K.; Wijesekara, H.; Yan, Y.; Bolan, N.; et al. Indoor Particulate Matter in Urban Households: Sources, Pathways, Characteristics, Health Effects, and Exposure Mitigation. Int. J. Environ. Res. Public. Health 2021, 18, 11055. [Google Scholar] [CrossRef] [PubMed]
- Jang, A.; Haryanto, B. Air Pollution—A Comprehensive Perspective; Haryanto, B., Ed.; IntechOpen: London, UK, 2012. [Google Scholar]
- Leikauf, G.D.; Kim, S.-H.; Jang, A.-S. Mechanisms of ultrafine particle-induced respiratory health effects. Exp. Mol. Med. 2020, 52, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Song, D.; Park, S.; Choi, Y. Particulate matter generation in daily activities and removal effect by ventilation methods in residential building. Air Qual. Atmos. Health 2021, 14, 1665–1680. [Google Scholar] [CrossRef]
- Singer, B.C.; Pass, R.Z.; Delp, W.W.; Lorenzetti, D.M.; Maddalena, R.L. Pollutant concentrations and emission rates from natural gas cooking burners without and with range hood exhaust in nine California homes. Build. Environ. 2017, 122, 215–229. [Google Scholar] [CrossRef]
- Lebel, E.D.; Finnegan, C.J.; Ouyang, Z.; Jackson, R.B. Methane and NOx Emissions from Natural Gas Stoves, Cooktops, and Ovens in Residential Homes. Environ. Sci. Technol. 2022, 56, 2529–2539. [Google Scholar] [CrossRef]
- Paulin, L.M.; Williams, D.L.; Peng, R.; Diette, G.B.; McCormack, M.C.; Breysse, P.; Hansel, N.N. 24-h Nitrogen dioxide concentration is associated with cooking behaviors and an increase in rescue medication use in children with asthma. Environ. Res. 2017, 159, 118–123. [Google Scholar] [CrossRef]
- Lin, W.; Brunekreef, B.; Gehring, U. Meta-analysis of the effects of indoor nitrogen dioxide and gas cooking on asthma and wheeze in children. Int. J. Epidemiol. 2013, 42, 1724–1737. [Google Scholar] [CrossRef]
- Zota, A.; Adamkiewicz, G.; Levy, J.I.; Spengler, J.D. Ventilation in public housing: Implications for indoor nitrogen dioxide concentrations. Indoor Air 2005, 15, 393–401. [Google Scholar] [CrossRef]
- Zusman, M.; Gassett, A.J.; Kirwa, K.; Barr, R.G.; Cooper, C.B.; Han, M.K.; Kanner, R.E.; Koehler, K.; Ortega, V.E.; Paine, R.; et al. Modeling residential indoor concentrations of PM2.5, NO2, NOx, and secondhand smoke in the Subpopulations and Intermediate Outcome Measures in COPD (SPIROMICS) Air study. Indoor Air 2021, 31, 702–716. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Samet, J.M. A review of the epidemiological evidence on health effects of nitrogen dioxide exposure from gas stoves. J. Environ. Med. 1999, 1, 173–187. [Google Scholar] [CrossRef]
- Levy, J.I.; Lee, K.; Spengler, J.D.; Yanagisawa, Y. Impact of residential nitrogen dioxide exposure on personal exposure: An international study. J. Air Waste Manag. Assoc. 1998, 48, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Scott Downen, R.; Dong, Q.; Chorvinsky, E.; Li, B.; Tran, N.; Jackson, J.H.; Pillai, D.K.; Zaghloul, M.; Li, Z. Personal NO2 sensor demonstrates feasibility of in-home exposure measurements for pediatric asthma research and management. J. Expo. Sci. Environ. Epidemiol. 2022, 32, 312–319. [Google Scholar] [CrossRef]
- Abdel-Salam, M.M.M. Outdoor and indoor factors influencing particulate matter and carbon dioxide levels in naturally ventilated urban homes. J. Air Waste Manag. Assoc. 2021, 71, 60–69. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Villanueva, F.; Ródenas, M.; Ruus, A.; Saffell, J.; Gabriel, M.F. Sampling and analysis techniques for inorganic air pollutants in indoor air. Appl. Spectrosc. Rev. 2022, 57, 531–579. [Google Scholar] [CrossRef]
- Wang, J.; Du, W.; Lei, Y.; Chen, Y.; Wang, Z.; Mao, K.; Tao, S.; Pan, B. Quantifying the dynamic characteristics of indoor air pollution using real-time sensors: Current status and future implication. Environ. Int. 2023, 175, 107934. [Google Scholar] [CrossRef]
- Mukerjee, S.; Smith, L.A.; Norris, G.A.; Morandi, M.T.; Gonzales, M.; Noble, C.A.; Neas, L.M.; Ozkaynak, A.H. Field method comparison between passive air samplers and continuous monitors for Vocs and NO2 in El Paso, Texas. J. Air Waste Manag. Assoc. 2004, 54, 307–319. [Google Scholar] [CrossRef]
- LogTag North America Inc. Available online: https://logtagrecorders.com/product/trix-8/ (accessed on 11 March 2024).
- Semple, S.; Apsley, A.; Maccalman, L. An inexpensive particle monitor for smoker behaviour modification in homes. Tob. Control 2013, 22, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Franken, R.; Maggos, T.; Stamatelopoulou, A.; Loh, M.; Kuijpers, E.; Bartzis, J.; Steinle, S.; Cherrie, J.W.; Pronk, A. Comparison of methods for converting Dylos particle number concentrations to PM2.5 mass concentrations. Indoor Air 2019, 29, 450–459. [Google Scholar] [CrossRef]
- Dacunto, P.J.; Klepeis, N.E.; Cheng, K.C.; Acevedo-Bolton, V.; Jiang, R.T.; Repace, J.L.; Ott, W.R.; Hildemann, L.M. Determining PM2.5 calibration curves for a low-cost particle monitor: Common indoor residential aerosols. Environ. Sci. Process Impacts 2015, 17, 1959–1966. [Google Scholar] [CrossRef]
- Steinle, S.; Reis, S.; Sabel, C.E.; Semple, S.; Twigg, M.M.; Braban, C.F.; Leeson, S.R.; Heal, M.R.; Harrison, D.; Lin, C.; et al. Personal exposure monitoring of PM2.5 in indoor and outdoor microenvironments. Sci. Total Environ. 2015, 508, 383–394. [Google Scholar] [CrossRef]
- Klepeis, N.E.; Hughes, S.C.; Edwards, R.D.; Allen, T.; Johnson, M.; Chowdhury, Z.; Smith, K.R.; Boman-Davis, M.; Bellettiere, J.; Hovell, M.F. Promoting smoke-free homes: A novel behavioral intervention using real-time audio-visual feedback on airborne particle levels. PLoS ONE 2013, 8, e73251. [Google Scholar] [CrossRef]
- Gillespie-Bennett, J.; Pierse, N.; Wickens, K.; Crane, J.; Nicholls, S.; Shields, D.; Boulic, M.; Viggers, H.; Baker, M.; Woodward, A. Sources of nitrogen dioxide (NO2) in New Zealand homes: Findings from a community randomized controlled trial of heater substitutions. Indoor Air 2008, 18, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Kornartit, C.; Sokhi, R.S.; Burton, M.A.; Ravindra, K. Activity pattern and personal exposure to nitrogen dioxide in indoor and outdoor microenvironments. Environ. Int. 2010, 36, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Mercado, I.; Canuz, E.; Smith, K.R. Temperature dataloggers as stove use monitors (SUMs): Field methods and signal analysis. Biomass Bioenergy 2012, 47, 459–468. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Global Air Quality Guidelines: Particulate Matter (Pm2.5 And Pm10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Ng, T.P.; Seet, C.S.; Tan, W.C.; Foo, S.C. Nitrogen dioxide exposure from domestic gas cooking and airway response in asthmatic women. Thorax 2001, 56, 596–601. [Google Scholar] [CrossRef]
- Hansel, N.N.; McCormack, M.C.; Belli, A.J.; Matsui, E.C.; Peng, R.D.; Aloe, C.; Paulin, L.; Williams, D.A.L.; Diette, G.B.; Breysse, P.N. In-Home Air Pollution Is Linked to Respiratory Morbidity in Former Smokers with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2013, 187, 1085–1090. [Google Scholar] [CrossRef]
- Baxter, L.K.; Clougherty, J.E.; Laden, F.; Levy, J.I. Predictors of concentrations of nitrogen dioxide, fine particulate matter, and particle constituents inside of lower socioeconomic status urban homes. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Zhao, B. Indoor sources strongly contribute to exposure of Chinese urban residents to PM2.5 and NO2. J. Hazard. Mater. 2022, 426, 127829. [Google Scholar] [CrossRef]
- Lee, K.; Levy, J.I.; Yanagisawa, Y.; Spengler, J.D.; Billick, I.H. The Boston Residential Nitrogen Dioxide Characterization Study: Classification and Prediction of Indoor NO2 Exposure. J. Air Waste Manag. Assoc. 1998, 48, 736–742. [Google Scholar] [CrossRef]
- Paulin, L.M.; Diette, G.B.; Scott, M.; McCormack, M.C.; Matsui, E.C.; Curtin-Brosnan, J.; Williams, D.L.; Kidd-Taylor, A.; Shea, M.; Breysse, P.N.; et al. Home interventions are effective at decreasing indoor nitrogen dioxide concentrations. Indoor Air 2014, 24, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Marbury, M.C.; Harlos, D.P.; Samet, J.M.; Spengler, J.D. Indoor Residential NO2 Concentrations in Albuquerque, New Mexico. J. Air Waste Manag. Assoc. 1988, 38, 392–398. [Google Scholar] [CrossRef]
- Paulin, L.M.; Samet, J.M.; Rice, M.B. Gas Stoves and Respiratory Health: Decades of Data, but Not Enough Progress. Ann. Am. Thorac. Soc. 2023, 20, 1697–1699. [Google Scholar] [CrossRef] [PubMed]
- Chao, C.Y.H.; Law, A. A study of personal exposure to nitrogen dioxide using passive samplers. Build. Environ. 2000, 35, 545–553. [Google Scholar] [CrossRef]
- Dėdelė, A.; Miškinytė, A. Seasonal variation of indoor and outdoor air quality of nitrogen dioxide in homes with gas and electric stoves. Environ. Sci. Pollut. Res. 2016, 23, 17784–17792. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Qi, M.; Chen, Y.; Shen, H.; Liu, J.; Huang, Y.; Chen, H.; Liu, W.; Wang, X.; Liu, J.; et al. Influences of ambient air PM2.5 concentration and meteorological condition on the indoor PM2.5 concentrations in a residential apartment in Beijing using a new approach. Environ. Pollut. 2015, 205, 307–314. [Google Scholar] [CrossRef]
- Sørensen, M.; Loft, S.; Andersen, H.V.; Raaschou-Nielsen, O.; Skovgaard, L.T.; Knudsen, L.E.; Nielsen, I.V.; Hertel, O. Personal exposure to PM2.5, black smoke and NO2 in Copenhagen: Relationship to bedroom and outdoor concentrations covering seasonal variation. J. Expo. Sci. Environ. Epidemiol. 2005, 15, 413–422. [Google Scholar] [CrossRef]
- Clougherty, J.E.; Houseman, E.A.; Levy, J.I. Source apportionment of indoor residential fine particulate matter using land use regression and constrained factor analysis. Indoor Air 2011, 21, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Uchiyama, S.; Tomizawa, T.; Tokoro, A.; Aoki, M.; Hishiki, M.; Yamada, T.; Tanaka, R.; Sakamoto, H.; Yoshida, T.; Bekki, K.; et al. Gaseous chemical compounds in indoor and outdoor air of 602 houses throughout Japan in winter and summer. Environ. Res. 2015, 137, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Zhao, B. Relationship between indoor and outdoor NO2: A review. Build. Environ. 2020, 180, 106909. [Google Scholar] [CrossRef]
- Cattaneo, A.; Peruzzo, C.; Garramone, G.; Urso, P.; Ruggeri, R.; Carrer, P.; Cavallo, D.M. Airborne particulate matter and gaseous air pollutants in residential structures in Lodi province, Italy. Indoor Air 2011, 21, 489–500. [Google Scholar] [CrossRef] [PubMed]
- Karr, G.; Quivet, E.; Ramel, M.; Nicolas, M. Sprays and diffusers as indoor air fresheners: Exposure and health risk assessment based on measurements under realistic indoor conditions. Indoor Air 2022, 32, e12923. [Google Scholar] [CrossRef]
- Li, S.; Cao, S.; Duan, X.; Zhang, Y.; Gong, J.; Xu, X.; Guo, Q.; Meng, X.; Bertrand, M.; Zhang, J.J. Long-term exposure to PM2.5 and Children’s lung function: A dose-based association analysis. J. Thorac. Dis. 2020, 12, 6379–6395. [Google Scholar] [CrossRef]
- Steinemann, A. Ten questions concerning air fresheners and indoor built environments. Build. Environ. 2017, 111, 279–284. [Google Scholar] [CrossRef]
- Goodman, N.; Nematollahi, N.; Agosti, G.; Steinemann, A. Evaluating air quality with and without air fresheners. Air Qual. Atmos. Health 2020, 13, 1–4. [Google Scholar] [CrossRef]
- Nazaroff, W.W.; Weschler, C.J. Cleaning products and air fresheners: Exposure to primary and secondary air pollutants. Atmos. Environ. 2004, 38, 2841–2865. [Google Scholar] [CrossRef]
- Jung, Y.-R.; Park, H.-H.; Oh, Y.-H.; Kim, S.-G.; Sohn, J.-R.; Kim, S.-H.; Yu, Y.-J.; Bae, G.-N.; Kim, M.-G. Emission characteristics of volatile organic compounds from air fresher using small emission chamber. J. Korean Soc. Environ. Eng. 2011, 33, 183–190. [Google Scholar] [CrossRef]
- Kim, S.; Hong, S.-H.; Bong, C.-K.; Cho, M.-H. Characterization of air freshener emission: The potential health effects. J. Toxicol. Sci. 2015, 40, 535–550. [Google Scholar] [CrossRef] [PubMed]
- Nørgaard, A.W.; Kudal, J.D.; Kofoed-Sørensen, V.; Koponen, I.K.; Wolkoff, P. Ozone-initiated VOC and particle emissions from a cleaning agent and an air freshener: Risk assessment of acute airway effects. Environ. Int. 2014, 68, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Askariyeh, M.H.; Zietsman, J.; Autenrieth, R. Traffic contribution to PM2.5 increment in the near-road environment. Atmos. Environ. 2020, 224, 117113. [Google Scholar] [CrossRef]
- Ni, Y.; Shi, G.; Qu, J. Indoor PM2. 5, tobacco smoking and chronic lung diseases: A narrative review. Environ. Res. 2020, 181, 108910. [Google Scholar] [CrossRef]
- Sureda, X.; Martínez-Sánchez, J.M.; López, M.J.; Fu, M.; Agüero, F.; Saltó, E.; Nebot, M.; Fernández, E. Secondhand smoke levels in public building main entrances: Outdoor and indoor PM2.5 assessment. Tob. Control 2012, 21, 543–548. [Google Scholar] [CrossRef]
- Fabian, P.; Adamkiewicz, G.; Levy, J.I. Simulating indoor concentrations of NO2 and PM2.5 in multifamily housing for use in health-based intervention modeling. Indoor Air 2012, 22, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Mullen, N.A.; Li, J.; Russell, M.L.; Spears, M.; Less, B.D.; Singer, B.C. Results of the California Healthy Homes Indoor Air Quality Study of 2011-2013: Impact of natural gas appliances on air pollutant concentrations. Indoor Air 2016, 26, 231–245. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, B.; Wang, J.; Zhao, B. Health benefits and cost of using air purifiers to reduce exposure to ambient fine particulate pollution in China. J. Hazard. Mater. 2021, 414, 125540. [Google Scholar] [CrossRef] [PubMed]
- Klepeis, N.E.; Bellettiere, J.; Hughes, S.C.; Nguyen, B.; Berardi, V.; Liles, S.; Obayashi, S.; Hofstetter, C.R.; Blumberg, E.; Hovell, M.F. Fine particles in homes of predominantly low-income families with children and smokers: Key physical and behavioral determinants to inform indoor-air-quality interventions. PLoS ONE 2017, 12, e0177718. [Google Scholar] [CrossRef]
- Nishihama, Y.; Jung, C.-R.; Nakayama, S.F.; Tamura, K.; Isobe, T.; Michikawa, T.; Iwai-Shimada, M.; Kobayashi, Y.; Sekiyama, M.; Taniguchi, Y.; et al. Indoor air quality of 5,000 households and its determinants. Part A: Particulate matter (PM2.5 and PM10–2.5) concentrations in the Japan Environment and Children’s Study. Environ. Res. 2021, 198, 111196. [Google Scholar] [CrossRef]
| Variables | Categories | n = 73 | % |
|---|---|---|---|
| Season of environmental sampling in homes | Winter | 14 | 19 |
| Spring | 32 | 44 | |
| Summer | 18 | 25 | |
| Fall | 9 | 12 | |
| What type of housing is this? | Townhouse | 20 | 27 |
| Apartment Building | 53 | 73 | |
| Kitchen Characteristics | |||
| How do you light the stove burners? | Autoignition | 68 | 93.15 |
| Pilot light | 5 | 6.85 | |
| Is there a working hood or vent present? | Yes (recirculating vent) | 34 | 46.58 |
| No | 39 | 53.42 | |
| The Kitchen layout is: | A room with entire-height walls separate from the living area | 43 | 58.90 |
| A room with a wall open to the living area | 30 | 41.10 | |
| Does tobacco smoke enter your apartment from other apartments or outside? | Yes | 37 | 50.68 |
| No | 34 | 46.58 | |
| Missing | 2 | 2.74 | |
| Does your vacuum cleaner have a HEPA filter? | Yes | 13 | 17.81 |
| No | 58 | 79.45 | |
| Missing | 2 | 2.74 | |
| How often is air freshener used in your house? | <6 days/week | 49 | 67.12 |
| 6–7 days/week | 22 | 30.14 | |
| Missing | 2 | 2.74 | |
| Wall-to-wall carpeting in the living area? | Yes | 32 | 43.84 |
| No | 39 | 53.42 | |
| Missing | 2 | 2.74 | |
| Area rug in living space? | Yes | 17 | 23.29 |
| No | 53 | 72.60 | |
| Missing | 3 | 4.11 | |
| Do trucks typically drive on your street? | Yes, often | 35 | 47.95 |
| Yes, occasionally | 23 | 31.51 | |
| No | 11 | 15.07 | |
| Missing | 4 | 5.48 | |
| Are any of these close to your apartment? | Dry cleaner | 55 | 75.34 |
| Gas Station | 68 | 93.15 | |
| Restaurant | 68 | 93.15 | |
| Bakery | 57 | 78.08 | |
| Auto body shop | 57 | 78.08 | |
| Truck loading/unloading area | 63 | 86.30 | |
| City bus stop | 70 | 95.89 | |
| n | Mean (SD) | Range | |||
|---|---|---|---|---|---|
| Average indoor temperature (°C) | 73 | 24.0 (2.3) | 18.1–32.0 | ||
| Average indoor humidity (g/m3) | 73 | 43.6 (12.0) | 22.8–66.7 | ||
| Fraction of stove use | 72 | 0.3 (0.2) | 0–0.8 | ||
| n | GM (GSD) | Range | Mean (SD) | p-value | |
| NO2 (ppb) | |||||
| Indoor | 73 | 21.8 (2.1) | 4.0–148.0 | 28.6 (24.5) | |
| Outdoor | 69 | 10.9 (1.7) | 2.6–27.7 | 12.4 (5.9) | |
| Paired t-test * | 69 | <0.0001 | |||
| PM2.5 (µg/m3) | |||||
| Indoor | 73 | 16.2 (2.7) | 1.8–305.4 | 30.4 (48.2) | |
| Outdoor | 71 | 5.9 (1.8) | 2.0–59.0 | 7.3 (7.6) | |
| Paired t-test * | 71 | <0.0001 |
| 95% CI | |||||
|---|---|---|---|---|---|
| Exposure Determinant | n | Estimate | Lower | Upper | p-Value |
| Stove Use | 72 | 0.17 | −0.57 | 0.92 | 0.65 |
| Outdoor NO2 | 69 | 0.16 | −0.16 | 0.48 | 0.33 |
| Season (ref = winter) | 73 | ||||
| Fall * | −0.57 | −1.13 | −0.003 | 0.05 | |
| Spring * | −0.42 | −0.85 | 0.0002 | 0.05 | |
| Summer * | −0.83 | −1.30 | −0.36 | 0.001 | |
| Stove Type (ref Autoignition) * | 73 | 0.68 | −0.04 | 1.33 | 0.04 |
| Average Temperature (°C) | 73 | −0.02 | −0.10 | 0.05 | 0.58 |
| Average Humidity | 73 | −0.01 | −0.02 | 0.004 | 0.16 |
| Vent (ref—yes) No | 73 | −0.08 | −0.42 | 0.25 | 0.62 |
| Room Type (ref—Wall separates kitchen and living area) | 73 | −0.11 | −0.45 | 0.23 | 0.53 |
| Outside Tobacco Smoke (ref—No) Yes | 71 | 0.05 | −0.29 | 0.39 | 0.78 |
| Vacuum with HEPA Filter (ref—yes) No | 73 | −0.16 | −0.61 | 0.28 | 0.47 |
| Air Freshener Use (ref ≤ 6 day/weeks) 6–7 days/week | 71 | −0.25 | −0.61 | 0.12 | 0.18 |
| Trucks Nearby (ref—No) Yes | 69 | 0.33 | −0.13 | 0.78 | 0.16 |
| Gas Station Nearby (ref—No) Yes | 73 | −0.43 | −1.08 | 0.23 | 0.20 |
| 95% CI | |||||
|---|---|---|---|---|---|
| Exposure Determinant | n | Estimate | Lower | Upper | p-Value |
| Stove Use | 72 | −0.20 | −1.25 | 0.86 | 0.71 |
| Outdoor PM2.5 | 71 | −0.14 | −0.55 | 0.27 | 0.51 |
| Season (ref = winter) Fall | 73 | ||||
| Fall | −0.27 | −1.08 | 0.55 | 0.52 | |
| Spring | −0.51 | −1.13 | 0.10 | 0.10 | |
| Summer * | −0.74 | −1.43 | −0.06 | 0.03 | |
| Stove Type (ref Autoignition) | 73 | −0.48 | −1.39 | 0.43 | 0.30 |
| Average Temperature (°C) | 73 | −0.10 | −0.20 | 0.003 | 0.06 |
| Average Humidity | 73 | −0.02 | −0.03 | 0.003 | 0.11 |
| Vent (ref yes) | 73 | −0.34 | −0.79 | 0.12 | 0.15 |
| Room Type (ref Wall separates kitchen and living area) | 73 | 0.09 | −0.38 | 0.56 | 0.70 |
| Outside Tobacco Smoke (ref No) Yes | 71 | −0.04 | −0.51 | 0.43 | 0.86 |
| Vacuum with HEPA filter (ref Yes) No | 71 | 0.46 | −0.15 | 1.06 | 0.14 |
| Wall-to-Wall Carpet (ref No) Yes | 71 | 0.03 | −0.44 | 0.51 | 0.89 |
| Air Freshener Use (ref ≤ 6 days/week) 6–7 days/week * | 71 | 0.77 | 0.29 | 1.25 | 0.0016 |
| Trucks Nearby (ref—No) Yes | 69 | −0.12 | −0.78 | 0.54 | 0.73 |
| Gas Station Nearby (ref—No) Yes * | 73 | 1.13 | 0.25 | 2.01 | 0.01 |
| 95% CI | |||||
|---|---|---|---|---|---|
| Exposure Determinant | n | Estimate | Lower | Upper | p-Value |
| Stove Use Fraction | 72 | 0.24 | −0.41 | 0.90 | 0.47 |
| Season (ref = winter) Fall * | −0.67 | −1.19 | −0.16 | 0.01 | |
| Spring * | −0.51 | −0.89 | −0.12 | 0.01 | |
| Summer * | −0.99 | −1.43 | −0.55 | <0.0001 | |
| Stove Type (ref = autoignition) Pilot Light * | 1.04 | 0.46 | 1.62 | 0.0004 | |
| 95% CI | |||||
|---|---|---|---|---|---|
| Exposure Determinant | n | Estimate | Lower | Upper | p-Value |
| Stove Use Fraction | 70 | −0.15 | −1.14 | 0.84 | 0.76 |
| Season (ref = winter) Fall | −0.31 | −1.08 | 0.46 | 0.43 | |
| Spring * | −0.58 | −1.16 | 0.01 | 0.05 | |
| Summer * | −0.69 | −1.35 | −0.04 | 0.04 | |
| Air Freshener Use (ref = never) 6–7 days/week * | 0.79 | 0.32 | 1.26 | 0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kadiri, K.; Turcotte, D.; Gore, R.; Bello, A.; Woskie, S.R. Determinants of Indoor NO2 and PM2.5 Concentration in Senior Housing with Gas Stoves. Toxics 2024, 12, 901. https://doi.org/10.3390/toxics12120901
Kadiri K, Turcotte D, Gore R, Bello A, Woskie SR. Determinants of Indoor NO2 and PM2.5 Concentration in Senior Housing with Gas Stoves. Toxics. 2024; 12(12):901. https://doi.org/10.3390/toxics12120901
Chicago/Turabian StyleKadiri, Khafayat, David Turcotte, Rebecca Gore, Anila Bello, and Susan R. Woskie. 2024. "Determinants of Indoor NO2 and PM2.5 Concentration in Senior Housing with Gas Stoves" Toxics 12, no. 12: 901. https://doi.org/10.3390/toxics12120901
APA StyleKadiri, K., Turcotte, D., Gore, R., Bello, A., & Woskie, S. R. (2024). Determinants of Indoor NO2 and PM2.5 Concentration in Senior Housing with Gas Stoves. Toxics, 12(12), 901. https://doi.org/10.3390/toxics12120901







