Patients’ Use and Perceptions of a Drug-Drug Interaction Database: A Survey of Janusmed Interactions
Abstract
1. Introduction
- Q1: What kind of information do patients want?
- Q2: How do patients perceive the content and usability?
- Q3: How would patients react if they found DDI in their medication?
- Q4: Is there a perceived need for a “patient version” of the database Janusmed interactions?
2. Materials and Methods
2.1. Participants, Inclusion and Exclusion
2.2. The Questionnaire
2.3. Analysis
2.4. Ethical Considerations
3. Results
3.1. Reasons for Using Janusmed Interactions
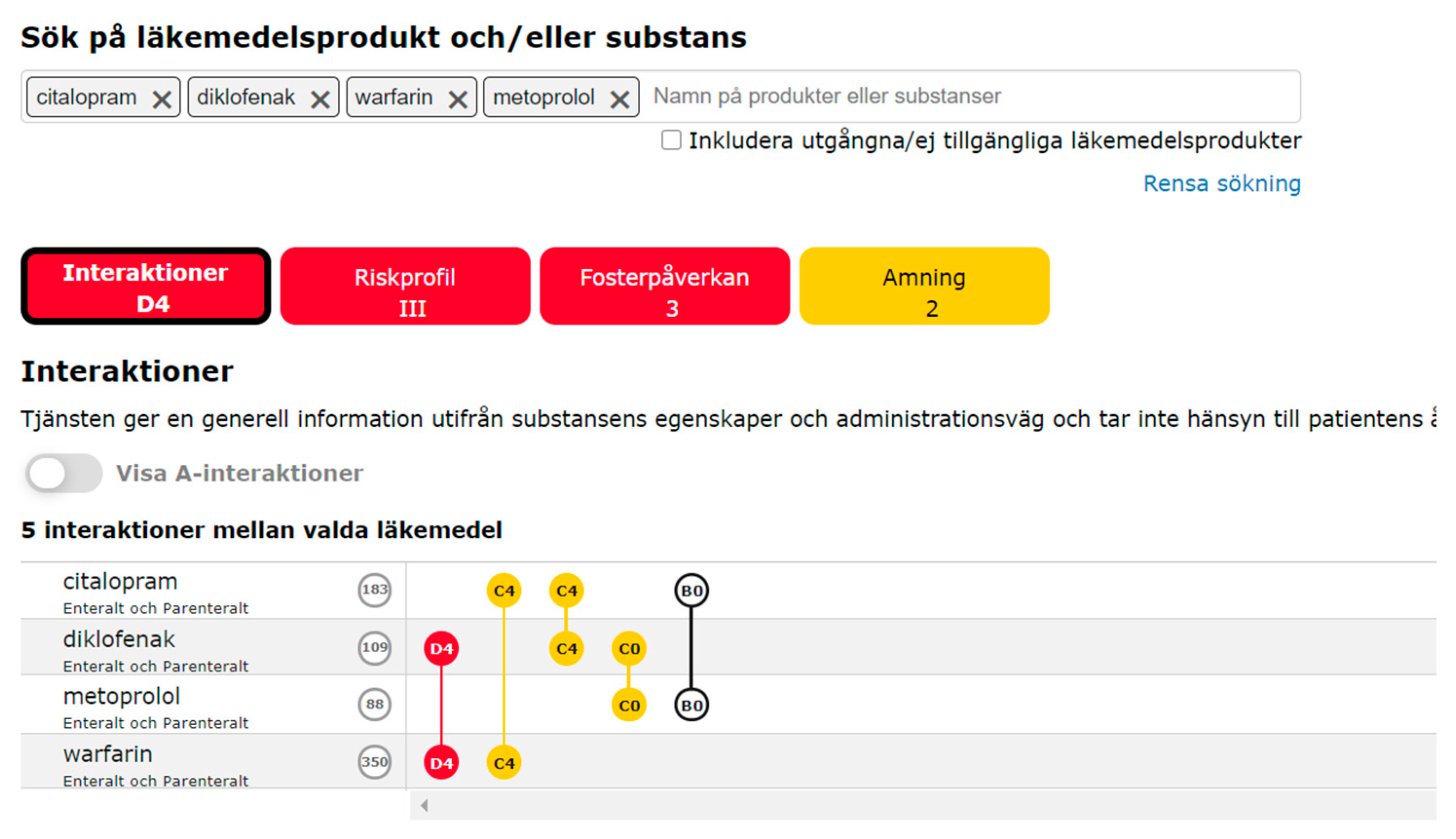
3.2. Patients’ Perceptions of Janusmed Interactions
3.3. (Re) Actions When Finding an Interaction
3.4. Other Information Sources Used by Patients
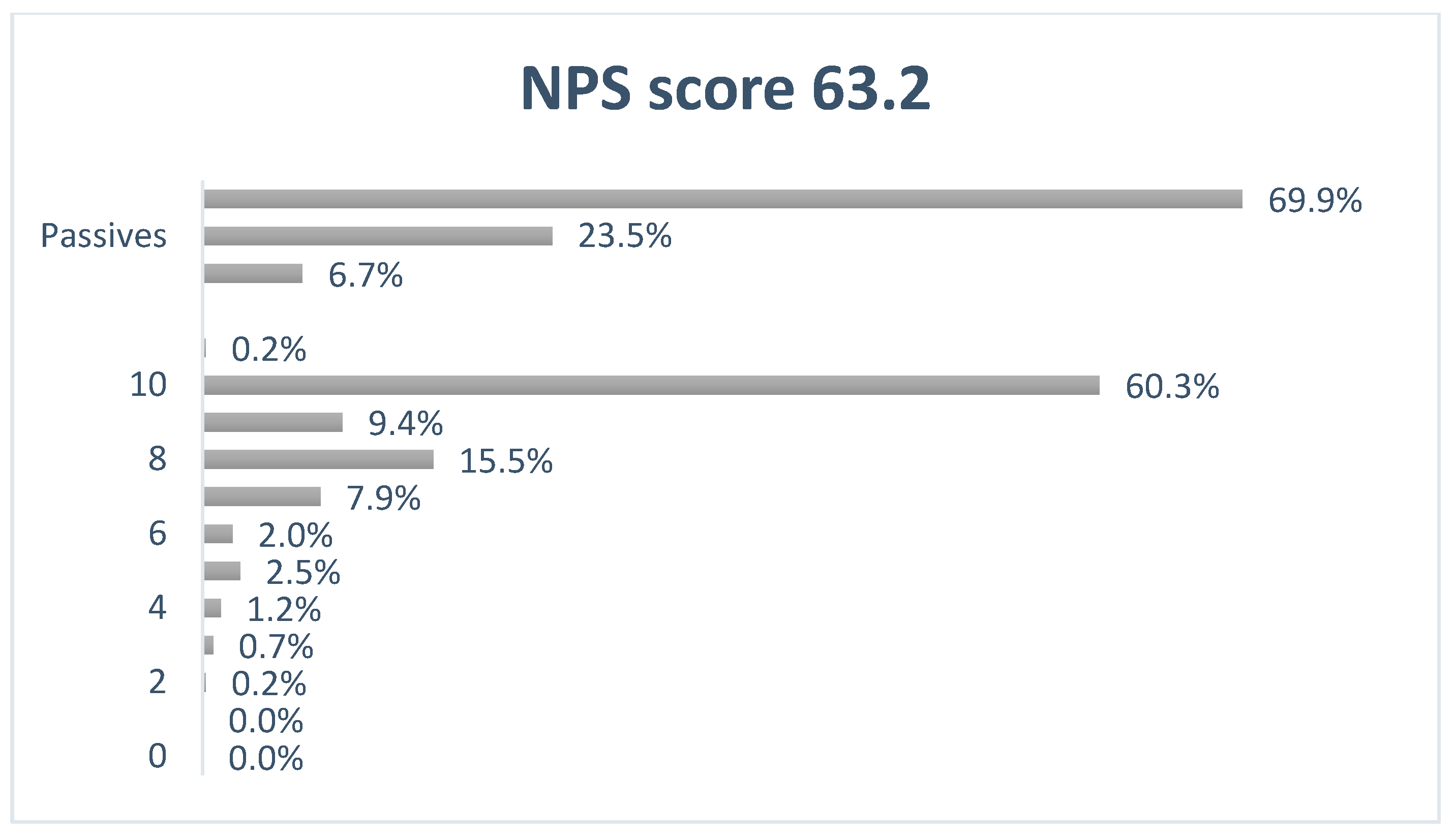
3.5. User Satisfaction—Net Promotor Score
4. Discussion
4.1. Patient Information Needs
4.2. Sources of Information
4.3. Handling Interactions
4.4. Heading For a “Patient Edition” of Janusmed Interactions
4.5. Method Discussion
4.6. Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dechanont, S.; Maphanta, S.; Butthum, B.; Kongkaew, C. Hospital Admissions/Visits Associated with Drug-Drug Interactions: A Systematic Review and Meta-Analysis. Pharmacoepidemiol. Drug Saf. 2014, 23, 489–497. [Google Scholar] [CrossRef]
- Avery, A.J.; Sheikh, A.; Hurwitz, B.; Smeaton, L.; Chen, Y.-F.; Howard, R.; Cantrill, J.; Royal, S. Safer Medicines Management in Primary Care. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2002, 52, S17–S22. [Google Scholar]
- Böttiger, Y.; Laine, K.; Andersson, M.L.; Korhonen, T.; Molin, B.; Ovesjö, M.-L.; Tirkkonen, T.; Rane, A.; Gustafsson, L.L.; Eiermann, B. SFINX—A Drug-Drug Interaction Database Designed for Clinical Decision Support Systems. Eur. J. Clin. Pharmacol. 2009, 65, 627–633. [Google Scholar] [CrossRef]
- Lenssen, R.; Heidenreich, A.; Schulz, J.B.; Trautwein, C.; Fitzner, C.; Jaehde, U.; Eisert, A. Analysis of Drug-Related Problems in Three Departments of a German University Hospital. Int. J. Clin. Pharm. 2016, 38, 119–126. [Google Scholar] [CrossRef]
- Neuvonen, P.J.; Niemi, M.; Backman, J.T. Drug Interactions with Lipid-Lowering Drugs: Mechanisms and Clinical Relevance. Clin. Pharmacol. Ther. 2006, 80, 565–581. [Google Scholar] [CrossRef]
- Juurlink, D.N.; Mamdani, M.; Kopp, A.; Laupacis, A.; Redelmeier, D.A. Drug-Drug Interactions among Elderly Patients Hospitalized for Drug Toxicity. JAMA 2003, 289, 1652–1658. [Google Scholar] [CrossRef]
- Seidling, H.; Schmitt, S.; Bruckner, T.; Kaltschmidt, J.; Pruszydlo, M.; Senger, C.; Bertsche, T.; Walter-Sack, I.; Haefeli, W. Patient-Specific Electronic Decision Support Reduces Prescription of Excessive Doses. Qual. Saf. Health Care 2010, 19, e15. [Google Scholar] [CrossRef][Green Version]
- Monteith, S.; Glenn, T.; Gitlin, M.; Bauer, M. Potential Drug Interactions with Drugs Used for Bipolar Disorder: A Comparison of 6 Drug Interaction Database Programs. Pharmacopsychiatry 2020, 53, 220–227. [Google Scholar] [CrossRef]
- Sönnerstam, E.; Sjölander, M.; Lövheim, H.; Gustafsson, M. Clinically Relevant Drug–Drug Interactions among Elderly People with Dementia. Eur. J. Clin. Pharmacol. 2018, 74, 1351–1360. [Google Scholar] [CrossRef]
- Söksida|Janusmed. Available online: https://janusmed.sll.se/#/home (accessed on 7 December 2020).
- Böttiger, Y.; Laine, K.; Korhonen, T.; Lähdesmäki, J.; Shemeikka, T.; Julander, M.; Edlert, M.; Andersson, M.L. Development and Pilot Testing of PHARAO—A Decision Support System for Pharmacological Risk Assessment in the Elderly. Eur. J. Clin. Pharmacol. 2018, 74, 365–371. [Google Scholar] [CrossRef]
- Shemeikka, T.; Bastholm-Rahmner, P.; Elinder, C.-G.; Vég, A.; Törnqvist, E.; Cornelius, B.; Korkmaz, S. A Health Record Integrated Clinical Decision Support System to Support Prescriptions of Pharmaceutical Drugs in Patients with Reduced Renal Function: Design, Development and Proof of Concept. Int. J. Med. Inf. 2015, 84, 387–395. [Google Scholar] [CrossRef]
- Karlsson Lind, L.; von Euler, M.; Korkmaz, S.; Schenck-Gustafsson, K. Sex Differences in Drugs: The Development of a Comprehensive Knowledge Base to Improve Gender Awareness Prescribing. Biol. Sex Differ. 2017, 8, 32. [Google Scholar] [CrossRef]
- Nörby, U.; Källén, K.; Eiermann, B.; Korkmaz, S.; Winbladh, B.; Gustafsson, L.L. Drugs and Birth Defects: A Knowledge Database Providing Risk Assessments Based on National Health Registers. Eur. J. Clin. Pharmacol. 2013, 69, 889–899. [Google Scholar] [CrossRef]
- Hammar, T.; Hellström, L.; Ericson, L. The Use of a Decision Support System in Swedish Pharmacies to Identify Potential Drug-Related Problems—Effects of a National Intervention Focused on Reviewing Elderly Patients’ Prescriptions. Pharmacy 2020, 8, 118. [Google Scholar] [CrossRef]
- Garg, A.X.; Adhikari, N.K.J.; McDonald, H.; Rosas-Arellano, M.P.; Devereaux, P.J.; Beyene, J.; Sam, J.; Haynes, R.B. Effects of Computerized Clinical Decision Support Systems on Practitioner Performance and Patient Outcomes: A Systematic Review. JAMA 2005, 293, 1223–1238. [Google Scholar] [CrossRef]
- Eiermann, B.; Rahmner, P.B.; Korkmaz, S.; Landberg, C.; Lilja, B.; Shemeikka, T.; Veg, A.; Wettermark, B.; Gustafsson, L.L. Knowledge Bases for Clinical Decision Support in Drug Prescribing—Development, Quality Assurance, Management, Integration, Implementation and Evaluation of Clinical Value. Decis. Support Syst. 2010. [Google Scholar] [CrossRef]
- Kusch, M.; Haefeli, W.E.; Seidling, H.M. How to Meet Patients’ Individual Needs for Drug Information—A Scoping Review. Patient Prefer. Adherence 2018, 12, 2339–2355. [Google Scholar] [CrossRef]
- Adam, T.J.; Vang, J. Content and Usability Evaluation of Patient Oriented Drug-Drug Interaction Websites. AMIA Annu. Symp. Proc. AMIA Symp. 2015, 2015, 287–296. [Google Scholar]
- Vingen, D.; Andrews, E.J.; Ferati, M. Usability in Patient-Oriented Drug Interaction Checkers—A Scandinavian Sampling and Heuristic Evaluation. Informatics 2020, 7, 42. [Google Scholar] [CrossRef]
- FASS Allmänhet—Startsida. Available online: https://www.fass.se/LIF/startpage (accessed on 18 December 2020).
- Hämeen-Anttila, K.; Pietilä, K.; Pylkkänen, L.; Pohjanoksa-Mäntylä, M. Internet as a Source of Medicines Information (MI) among Frequent Internet Users. Res. Soc. Adm. Pharm. 2018, 14, 758–764. [Google Scholar] [CrossRef]
- Anker, A.E.; Reinhart, A.; Feeley, T. Health Information Seeking: A Review of Measures and Methods. Patient Educ. Couns. 2011. [Google Scholar] [CrossRef] [PubMed]
- Lambert, S.D.; Loiselle, C.G. Health Information—Seeking Behavior. Qual. Health Res. 2007, 17, 1006–1019. [Google Scholar] [CrossRef]
- Kim, B.Y.; Sharafoddini, A.; Tran, N.; Wen, E.Y.; Lee, J. Consumer Mobile Apps for Potential Drug-Drug Interaction Check: Systematic Review and Content Analysis Using the Mobile App Rating Scale (MARS). JMIR MHealth UHealth 2018, 6, e74. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Hoti, K.; Hughes, J.D.; Emmerton, L. Dr Google and the Consumer: A Qualitative Study Exploring the Navigational Needs and Online Health Information-Seeking Behaviors of Consumers with Chronic Health Conditions. J. Med. Internet Res. 2014, 16, e262. [Google Scholar] [CrossRef] [PubMed]
- Monkman, H.; Kushniruk, A.W.; Barnett, J.; Borycki, E.M.; Greiner, L.E.; Sheets, D. Are Health Literacy and EHealth Literacy the Same or Different? Stud. Health Technol. Inform. 2017, 245, 178–182. [Google Scholar]
- Morrow, D.G.; Weiner, M.; Steinley, D.; Young, J.; Murray, M.D. Patients’ Health Literacy and Experience with Instructions: Influence Preferences for Heart Failure Medication Instructions. J. Aging Health 2007, 19, 575–593. [Google Scholar] [CrossRef]
- Pang, P.C.-I.; Chang, S.; Verspoor, K.; Pearce, J. Designing Health Websites Based on Users’ Web-Based Information-Seeking Behaviors: A Mixed-Method Observational Study. J. Med. Internet Res. 2016, 18, e145. [Google Scholar] [CrossRef]
- Heponiemi, T.; Jormanainen, V.; Leemann, L.; Manderbacka, K.; Aalto, A.-M.; Hyppönen, H. Digital Divide in Perceived Benefits of Online Health Care and Social Welfare Services: National Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e17616. [Google Scholar] [CrossRef]
- Andersson, J. Svenskarna och Internet 2019; World Internet Project; Internetstiftelsen: Stockholm Sweden, 2019; Available online: https://svenskarnaochinternet.se/rapporter/svenskarna-och-internet-2019/ (accessed on 8 December 2020).
- Rahmner, P.B.; Lundborg, M. Ansvaret för samlad läkemedelslista ska vara tydligt. Läkartidningen 2011, 108, 1250–1252. Available online: https://lakartidningen.se/klinik-och-vetenskap-1/2011/05/ansvaret-for-samlad-lakemedelslista-ska-vara-tydligt/ (accessed on 20 December 2020).
- Rahmner, P.B.; Gustafsson, L.L.; Holmstrom, I.; Rosenqvist, U.; Tomson, G. Whose Job Is It Anyway? Swedish General Practitioners’ Perception of Their Responsibility for the Patient’s Drug List. Ann. Fam. Med. 2010, 8, 40–46. [Google Scholar] [CrossRef]
- Ko, Y.; Malone, D.C.; Skrepnek, G.H.; Armstrong, E.P.; Murphy, J.E.; Abarca, J.; Rehfeld, R.A.; Reel, S.J.; Woosley, R.L. Prescribers’ Knowledge of and Sources of Information for Potential Drug-Drug Interactions: A Postal Survey of US Prescribers. Drug Saf. 2008, 31, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Hammar, T.; Ekedahl, A.; Petersson, G. Implementation of a Shared Medication List: Physicians’ Views on Availability, Accuracy and Confidentiality. Int. J. Clin. Pharm. 2014, 36, 933–942. [Google Scholar] [CrossRef] [PubMed]
- Vacher, R.; Lagarce, L.; Ghamrawi, S.; Laugier-Castellan, D.; Vial, T.; Bagheri, H.; Babin, M.; Briet, M. Drug Interactions Related to Self-Medication: A French Pharmacovigilance Database Study. Fundam. Clin. Pharmacol. 2020, 34, 623–631. [Google Scholar] [CrossRef] [PubMed]
- Oedekoven, M.; Herrmann, W.J.; Ernsting, C.; Schnitzer, S.; Kanzler, M.; Kuhlmey, A.; Gellert, P. Patients’ Health Literacy in Relation to the Preference for a General Practitioner as the Source of Health Information. BMC Fam. Pract. 2019, 20. [Google Scholar] [CrossRef] [PubMed]
- Heringa, M.; Floor-Schreudering, A.; De Smet, P.A.G.M.; Bouvy, M.L. Aspects Influencing Patients’ Preferences for the Management of Drug-Drug Interactions: A Focus Group Study. Patient Educ. Couns. 2018, 101, 723–729. [Google Scholar] [CrossRef]
- Heringa, M.; Floor-Schreudering, A.; Wouters, H.; De Smet, P.A.G.M.; Bouvy, M.L. Preferences of Patients and Pharmacists with Regard to the Management of Drug-Drug Interactions: A Choice-Based Conjoint Analysis. Drug Saf. 2018, 41, 179–189. [Google Scholar] [CrossRef]
- Measuring Your Net Promoter ScoreSM. Available online: https://www.netpromotersystem.com/about/measuring-your-net-promoter-score/ (accessed on 8 December 2020).
- Sandelowski, M. Whatever Happened to Qualitative Description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Nörby, U.; Källén, K.; Shemeikka, T.; Korkmaz, S.; Winbladh, B. Pregnant Women’s View on the Swedish Internet Resource Drugs and Birth Defects Intended for Health Care Professionals. Acta Obstet. Gynecol. Scand. 2015, 94, 960–968. [Google Scholar] [CrossRef]
- Roshanov, P.S.; Fernandes, N.; Wilczynski, J.M.; Hemens, B.J.; You, J.J.; Handler, S.M.; Nieuwlaat, R.; Souza, N.M.; Beyene, J.; Spall, H.G.C.V.; et al. Features of Effective Computerised Clinical Decision Support Systems: Meta-Regression of 162 Randomised Trials. BMJ 2013, 346, f657. [Google Scholar] [CrossRef]
- Hammar, T.; Nilsson, A.-L.; Hovstadius, B. Patients’ Views on Electronic Patient Information Leaflets. Pharm. Pract. 2016, 14, 702. [Google Scholar] [CrossRef]
- Ho, C.-H.; Ko, Y.; Tan, M.-L. Patient Needs and Sources of Drug Information in Singapore: Is the Internet Replacing Former Sources? Ann. Pharmacother. 2009, 43, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Haverhals, L.M.; Lee, C.A.; Siek, K.A.; Darr, C.A.; Linnebur, S.A.; Ruscin, J.M.; Ross, S.E. Older Adults with Multi-Morbidity: Medication Management Processes and Design Implications for Personal Health Applications. J. Med. Internet Res. 2011, 13, e44. [Google Scholar] [CrossRef] [PubMed]
- Indermitte, J.; Reber, D.; Beutler, M.; Bruppacher, R.; Hersberger, K.E. Prevalence and Patient Awareness of Selected Potential Drug Interactions with Self-Medication. J. Clin. Pharm. Ther. 2007, 32, 149–159. [Google Scholar] [CrossRef] [PubMed]
| Question | Possible Answers (Multiple Choice) | Multiple Answers Possible | Possible to Comment in Free Text | |
|---|---|---|---|---|
| 1 | In which capacity do you use Janusmed interactions? | (a) Privately (b) In my profession | No | No |
| 2 | How old are you | (a) under 18 years (b) 19–39 years (c) 40–59 years (d) 60–80 years (e) over 80 years | No | No |
| 3 | In which region are you located? | (a) Blekinge (b) Dalarna (c) Gotland (d) Halland (e) Jämtland Härjedalen (f) Jönköpings län (g) Kalmar län (h) Kronoberg (i) Norrbotten (j) Skåne (k) Stockholm (l) Sörmland (m) Uppsala (n) Värmland (o) Västerbotten (p) Västmanland (q) Örebro län (r) Östergötland (s) Västra Götaland (t) located outside of Sweden | No | No |
| 4 | How often do you use Janusmed interactions? | (a) Multiple times a day (b) Once a day (c) A few times a week (d) A few times a month (e) A few times a year (f) Never | No | No |
| 5 | Why do you use Janusmed interactions? | (a) To check if my prescribed medication have interactions (b) To check if my prescribed medication interact with OTC drugs I have/plan to buy (c) To check if my OTC medication have interactions (d) To check if my medication interact with food/drink (e) To check if my medication interact with alcohol (f) To check if my medication interact with naturopathic drugs (g) To check interactions for a friend or relative (h) I look with my HCP to discuss my treatment (i) To learn more about drug interactions (j) Other | Yes | Yes |
| 6 | Are there any areas you miss/want more information about in Janusmed interaction? | (a) No, nothing (b) Food/drink (c) Alcohol (d) Herbal remedies (e) Dietary supplements (f) Other | Yes | Yes |
| 7 | Do you think Janusmed interactions is easy to use? | (a) Yes (b) No (c) Don’t know | No | Yes |
| 8 | Do you think the texts are easy to understand? | (a) Yes (b) No (c) Don’t know | No | Yes |
| 9 | If you had prescribed medication and found out they interacted how do you think you would react? | (a) Talk with my prescriber (b) Discontinue the treatment on my own (c) Make changes in the treatment on my own (d) Wouldn’t do anything (e) Other (f) I don’t know | Yes | Yes |
| 10 | Do you use any other sources to check for drug interactions? | (a) Yes (b) No | No | Yes |
| 11 | Would you use a version of Janusmed interactions specifically aimed at the public? | (a) Yes (b) No (c) I don’t know | No | No |
| 12 | On a scale from 0–10 how likely is it that you would recommend Janusmed interactions to a friend or colleague? | A scale of 0 to 10 | No | No |
| Q4: How Often Do You Use Janusmed Interactions? | n | % |
|---|---|---|
| Multiple times a day | 1 | 0.2 |
| Once a day | 2 | 0.5 |
| A few times a week | 10 | 2.5 |
| A few times a month | 125 | 30.8 |
| A few times a year | 268 | 66.0 |
| Total | 406 | 100.0 |
| Why Do You Use Janusmed Interactions? | Total (n) | Total (%) |
|---|---|---|
| (a) To check if my prescribed medication has interactions | 340 | 83.7 |
| (b) To check if my prescribed medication interacts with OTC drugs I have/plan to buy | 243 | 59.9 |
| (c) To check if my OTC medication have interactions | 132 | 32.5 |
| (d) To check if my medication interacts with food/drink | 115 | 28.3 |
| (e) To check if my medication interacts with alcohol | 83 | 20.4 |
| (f) To check if my medication interacts with herbal remedies | 110 | 27.1 |
| (g) To check interactions for a friend or relative | 180 | 44.3 |
| (h) I look with my caregiver to discuss my treatment | 19 | 4.7 |
| (i) To learn more about drug interactions | 162 | 39.9 |
| (j) Other | 30 | 7.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Justad, H.; Askfors, Y.; Shemeikka, T.; Andersson, M.L.; Hammar, T. Patients’ Use and Perceptions of a Drug-Drug Interaction Database: A Survey of Janusmed Interactions. Pharmacy 2021, 9, 23. https://doi.org/10.3390/pharmacy9010023
Justad H, Askfors Y, Shemeikka T, Andersson ML, Hammar T. Patients’ Use and Perceptions of a Drug-Drug Interaction Database: A Survey of Janusmed Interactions. Pharmacy. 2021; 9(1):23. https://doi.org/10.3390/pharmacy9010023
Chicago/Turabian StyleJustad, Hanna, Ylva Askfors, Tero Shemeikka, Marine L. Andersson, and Tora Hammar. 2021. "Patients’ Use and Perceptions of a Drug-Drug Interaction Database: A Survey of Janusmed Interactions" Pharmacy 9, no. 1: 23. https://doi.org/10.3390/pharmacy9010023
APA StyleJustad, H., Askfors, Y., Shemeikka, T., Andersson, M. L., & Hammar, T. (2021). Patients’ Use and Perceptions of a Drug-Drug Interaction Database: A Survey of Janusmed Interactions. Pharmacy, 9(1), 23. https://doi.org/10.3390/pharmacy9010023





