The doMESTIC RISK Tool: Prioritising Home-Care Patients for Clinical Pharmacy Services with the Help of a Delphi Study
Abstract
:1. Introduction
Aims
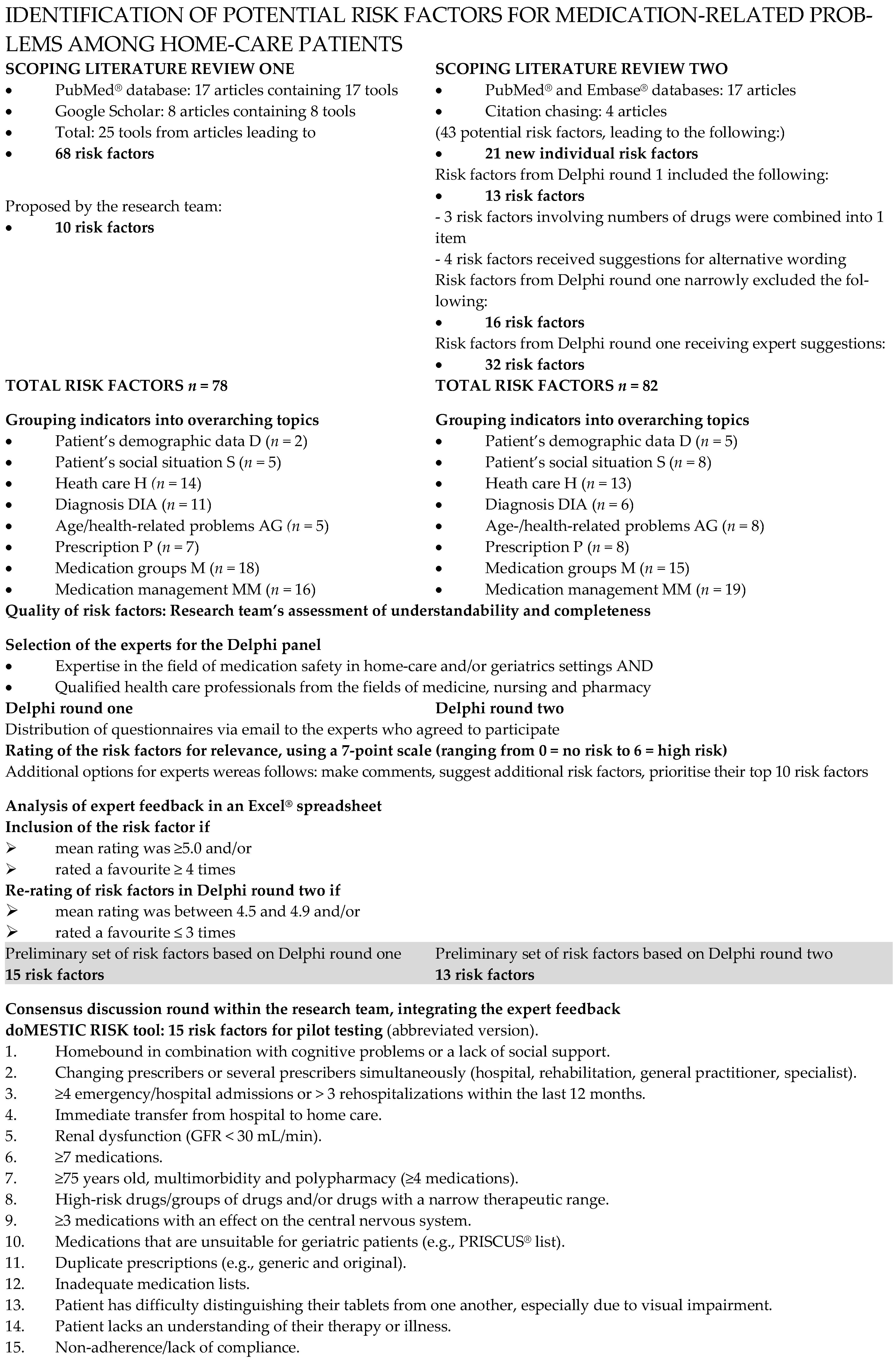
2. Materials and Methods
2.1. Scoping Literature Review One—Identifying Existing Tools and the Risk Factors Covered
2.2. Delphi Round One
2.3. Scoping Literature Review—Individual Risk Factors
2.4. Delphi Round Two
2.5. Consensus Round
3. Results
3.1. Scoping Literature Review—Existing Tools and Their Risk Factor Items
3.2. Delphi Round One
3.3. Scoping Literature Review for Individual Risk Factors
3.4. Delphi Round Two
3.5. Consensus Round
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
References
- van Mil, J.W.; Westerlund, L.O.; Hersberger, K.E.; Schaefer, M.A. Drug-related problem classification systems. Ann. Pharmacother. 2004, 38, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Massetti, C.; Kaiser, E.; Hedinger-Grogg, B.; Luterbacher, S.; Hersberger, K. Medication safety in the home care setting: Error-prone process steps. Pflege 2012, 25, 261–269. [Google Scholar] [CrossRef]
- Meyer-Massetti, C.; Meier, C.R.; Guglielmo, B.J. The scope of drug-related problems in the home care setting. Int. J. Clin. Pharm. 2018, 40, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.W.; Cullen, D.J.; Laird, N.; A Petersen, L.; Small, S.D.; Servi, D.; Laffel, G.; Sweitzer, B.J.; Shea, B.F.; Hallisey, R. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA 1995, 274, 29–34. [Google Scholar] [CrossRef]
- American College of Clinical Pharmacy. The definition of clinical pharmacy. Pharmacotherapy 2008, 28, 816–817. [Google Scholar] [CrossRef]
- Studer, H.; Imfeld-Isenegger, T.L.; Beeler, P.E.; Ceppi, M.G.; Rosen, C.; Bodmer, M.; Boeni, F.; Hersberger, K.E.; Lampert, M.L. The impact of pharmacist-led medication reconciliation and interprofessional ward rounds on drug-related problems at hospital discharge. Int. J. Clin. Pharm. 2023, 45, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Jermini, M.; Fonzo-Christe, C.; Blondon, K.; Milaire, C.; Stirnemann, J.; Bonnabry, P.; Guignard, B. Financial impact of medication reviews by clinical pharmacists to reduce in-hospital adverse drug events: A return-on-investment analysis. Int. J. Clin. Pharm. 2024, 46, 496–505. [Google Scholar] [CrossRef]
- Onatade, R.; Appiah, S.; Stephens, M.; Garelick, H. Evidence for the outcomes and impact of clinical pharmacy: Context of UK hospital pharmacy practice. Eur. J. Hosp. Pharm. 2018, 25, e21–e28. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Massetti, C.; Hofstetter, V.; Hedinger-Grogg, B.; Meier, C.R.; Guglielmo, B.J. Medication-related problems during transfer from hospital to home care: Baseline data from Switzerland. Int. J. Clin. Pharm. 2018, 40, 1614–1620. [Google Scholar] [CrossRef]
- Nydahl, P.; Borromeo, R.C.; Carrigan, T.; Dokken, H.; Fischer, U.; Kocks, A.; Kolbe, N.; Luboeinski, J.; Przylepa, K.; Safari, S.R.; et al. World views on shortage in nursing resource: Challenges and opportunities. Z. Evidenz Fortbild. Qual. Gesundheitswesen 2024, 188, 35–40. [Google Scholar] [CrossRef]
- Reeves, S.; Pelone, F.; Harrison, R.; Goldman, J.; Zwarenstein, M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2017, 6, CD000072. [Google Scholar] [CrossRef]
- Sekanina, U.; Tetzlaff, B.; Mazur, A.; Huckle, T.; Kuhn, A.; Dano, R.; Höckelmann, C.; Scherer, M.; Balzer, K.; Köpke, S.; et al. Interprofessional collaboration in the home care setting: Perspectives of people receiving home care, relatives, nurses, general practitioners, and therapists-results of a qualitative analysis. BMC Prim. Care 2024, 25, 79. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, C.; Atzeni, G.; Berchtold, P. Challenges in interprofessionalism in Swiss health care: The practice of successful interprofessional collaboration as experienced by professionals. Swiss Med. Wkly. 2017, 147, w14525. [Google Scholar] [PubMed]
- Déry, J.; Ruiz, A.; Routhier, F.; Gagnon, M.-P.; Côté, A.; Ait-Kadi, D.; Bélanger, V.; Deslauriers, S.; Lamontagne, M.-E. Patient prioritization tools and their effectiveness in non-emergency healthcare services: A systematic review protocol. Syst. Rev. 2019, 8, 78. [Google Scholar] [CrossRef]
- Junger, S.; Payne, S.A.; Brine, J.; Radbruch, L.; Brearley, S.G. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat. Med. 2017, 31, 684–706. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological frame-work. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Parameswaran Nair, N.; Chalmers, L.; Connolly, M.; Bereznicki, B.J.; Peterson, G.M.; Curtain, C.; Castelino, R.L.; Bereznicki, L.R. Prediction of Hospitalization due to Adverse Drug Reactions in Elderly Community-Dwelling Patients (The PADR-EC Score). PLoS ONE 2016, 11, e0165757. [Google Scholar] [CrossRef]
- Pammett, R.T.; Blackburn, D.; Taylor, J.; Mansell, K.; Kwan, D.; Papoushek, C.; Jorgenson, D. Evaluation of a Community Pharmacy-Based Screening Questionnaire to Identify Patients at Risk for Drug Therapy Problems. Pharmacotherapy 2015, 35, 881–886. [Google Scholar] [CrossRef]
- Dimitrow, M.S.; Mykkanen, S.I.; Leikola, S.N.; Kivela, S.L.; Lyles, A.; Airaksinen, M.S. Content validation of a tool for assessing risks for drug-related problems to be used by practical nurses caring for home-dwelling clients aged >/=65 years: A Delphi survey. Eur. J. Clin. Pharmacol. 2014, 70, 991–1002. [Google Scholar] [CrossRef]
- Makowsky, M.J.; Cor, K.; Wong, T. Exploring Electronic Medical Record and Self-Administered Medication Risk Screening Tools in a Primary Care Clinic. J. Manag. Care Spec. Pharm. 2017, 23, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Alassaad, A.; Melhus, H.; Hammarlund-Udenaes, M.; Bertilsson, M.; Gillespie, U.; Sundstrom, J. A tool for prediction of risk of rehospitalisation and mortality in the hospitalised elderly: Secondary analysis of clinical trial data. BMJ Open 2015, 5, e007259. [Google Scholar] [CrossRef] [PubMed]
- Snyder, M.E.; Pater, K.S.; Frail, C.K.; Hudmon, K.S.; Doebbeling, B.N.; Smith, R.B. Utility of a brief screening tool for medication-related problems. Res. Social. Adm. Pharm. 2015, 11, 253–264. [Google Scholar] [CrossRef]
- Ploenzke, C.; Kemp, T.; Naidl, T.; Marraffa, R.; Bolduc, J. Design and implementation of a targeted approach for pharmacist-mediated medication management at care transitions. J. Am. Pharm. Assoc. 2016, 56, 303–309. [Google Scholar] [CrossRef]
- Rovers, J.; Hagel, H. Self-assessment tool for screening patients at risk for drug therapy problems. J. Am. Pharm. Assoc. 2012, 52, 646–652. [Google Scholar] [CrossRef]
- Gusdal, A.K.; Beckman, C.; Wahlstrom, R.; Tornkvist, L. District nurses’ use for an assessment tool in their daily work with elderly patients’ medication management. Scand. J. Public Health 2011, 39, 354–360. [Google Scholar] [CrossRef]
- Singh, R.; McLean-Plunckett, E.A.; Kee, R.; Wisniewski, A.; Cadzow, R.; Okazaki, S.; Fox, C.; Singh, G. Experience with a trigger tool for identifying adverse drug events among older adults in ambulatory primary care. Qual. Saf. Health Care 2009, 18, 199–204. [Google Scholar] [CrossRef]
- Cullinan, S.; O’Mahony, D.; O’Sullivan, D.; Byrne, S. Use of a frailty index to identify potentially inappropriate prescribing and adverse drug reaction risks in older patients. Age Ageing 2016, 45, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Onder, G.; Petrovic, M.; Tangiisuran, B.; Meinardi, M.C.; Markito-Notenboom, W.P.; Somers, A.; Rajkumar, C.; Bernabei, R.; van der Cammen, T.J.M. Development and validation of a score to assess risk of adverse drug reactions among in-hospital patients 65 years or older: The GerontoNet ADR risk score. Arch. Intern. Med. 2010, 170, 1142–1148. [Google Scholar] [CrossRef]
- Kaufmann, C.P.; Stampfli, D.; Mory, N.; Hersberger, K.E.; Lampert, M.L. Drug-Associated Risk Tool: Development and validation of a self-assessment questionnaire to screen for hospitalised patients at risk for drug-related problems. BMJ Open 2018, 8, e016610. [Google Scholar] [CrossRef]
- Falconer, N.; Nand, S.; Liow, D.; Jackson, A.; Seddon, M. Development of an electronic patient prioritization tool for clinical pharmacist interventions. Am. J. Health Syst. Pharm. 2014, 71, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Doucette, W.R.; Chang, E.H.; Pendergast, J.F.; Wright, K.B.; Chrischilles, E.A.; Farris, K.B. Development and initial assessment of the medication user self-evaluation (MUSE) tool. Clin. Ther. 2013, 35, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Resar, R. Outpatient Adverse Event Trigger Tool: Institute for Healthcare Improvement IHI in association with Kaiser Permanente and Baylor Health Care System. 2016. Available online: www.ihi.org (accessed on 24 February 2025).
- Barnett, N.; Athwal, D.; Rosenbloom, K. Medicines-related admissions: You can identify patients to stop that happening. Pharm. J. 2011, 286, 471–472. [Google Scholar]
- The National Health Service—West Midlands Strategic Health Authority. Risk Indicators for Medicines-Related Problems. 2012. Available online: www.westmidlandsdeanery.nhs.uk/ (accessed on 24 February 2025).
- Nyborg, G.; Straand, J.; Klovning, A.; Brekke, M. The Norwegian General Practice--Nursing Home criteria (NORGEP-NH) for potentially inappropriate medication use: A web-based Delphi study. Scand. J. Prim. Health Care 2015, 33, 134–141. [Google Scholar] [CrossRef]
- Renom-Guiteras, A.; Meyer, G.; Thurmann, P.A. The EU(7)-PIM list: A list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur. J. Clin. Pharmacol. 2015, 71, 861–875. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, D.; O’Sullivan, D.; Byrne, S.; O’Connor, M.N.; Ryan, C.; Gallagher, P. STOPP/START criteria for potentially inappropriate prescribing in older people: Version 2. Age Ageing 2015, 44, 213–218. [Google Scholar] [CrossRef]
- Holt, S.; Schmiedl, S.; Thurmann, P.A. Potentially inappropriate medications in the elderly: The PRISCUS list. Dtsch. Ärzteblatt Int. 2010, 107, 543–551. [Google Scholar]
- Mann, N.-K.; Mathes, T.; Sönnichsen, A.; Pieper, D.; Klager, E.; Moussa, M.; Thürmann, P.A. Potentially Inadequate Medications in the Elderly: PRISCUS 2.0-First Update of the PRISCUS List. Dtsch. Arztebl. Int. 2023, 120, 3–10. [Google Scholar] [CrossRef]
- Tommelein, E.; Mehuys, E.; Petrovic, M.; Somers, A.; Van Damme, C.; Pattyn, E.; Mattelin, K.; Boussery, K. Potentially inappropriate prescribing in nursing home residents detected with the community pharmacist specific GheOP(3)S-tool. Int. J. Clin. Pharm. 2016, 38, 1063–1068. [Google Scholar] [CrossRef]
- Akbarov, A.; Kontopantelis, E.; Sperrin, M.; Stocks, S.J.; Williams, R.; Rodgers, S.; Avery, A.; Buchan, I.; Ashcroft, D.M. Primary Care Medication Safety Surveillance with Integrated Primary and Secondary Care Electronic Health Records: A Cross-Sectional Study. Drug Saf. 2015, 38, 671–682. [Google Scholar] [CrossRef]
- Pazan, F.; Weiss, C.; Wehling, M.; Forta. The FORTA (Fit. fOR The Aged) List 2015: Update of a Validated Clinical Tool for Improved Pharmacotherapy in the Elderly. Drugs Aging 2016, 33, 447–449. [Google Scholar] [CrossRef] [PubMed]
- Tangiisuran, B.; Scutt, G.; Stevenson, J.; Wright, J.; Onder, G.; Petrovic, M.; Van Der Cammen, T.J.; Rajkumar, C.; Davies, G. Development and validation of a risk model for predicting adverse drug reactions in older people during hospital stay: Brighton Adverse Drug Reactions Risk (BADRI) model. PLoS ONE 2014, 9, e111254. [Google Scholar] [CrossRef] [PubMed]
- Karpov, A.; Parcero, C.; Mok, C.P.; Panditha, C.; Yu, E.; Dempster, L.; Hohl, C.M. Performance of trigger tools in identifying adverse drug events in emergency department patients: A validation study. Br. J. Clin. Pharmacol. 2016, 82, 1048–1057. [Google Scholar] [CrossRef] [PubMed]
- Petrovic, M.; Tangiisuran, B.; Rajkumar, C.; van der Cammen, T.; Onder, G. Predicting the Risk of Adverse Drug Reactions in Older Inpatients: External Validation of the GerontoNet ADR Risk Score Using the CRIME Cohort. Drugs Aging 2017, 34, 135–142. [Google Scholar] [CrossRef]
- Donaldson, L.J.; Kelley, E.T.; Dhingra-Kumar, N.; Kieny, M.P.; Sheikh, A. Medication Without Harm: WHO’s Third Global Patient Safety Challenge. Lancet 2017, 389, 1680–1681. [Google Scholar] [CrossRef]
- Campbell, S.M.; Cantrill, J.A. Consensus methods in prescribing research. J. Clin. Pharm. Ther. 2001, 26, 5–14. [Google Scholar] [CrossRef]
- Jones, J.; Hunter, D. Consensus methods for medical and health services research. BMJ 1995, 311, 376–380. [Google Scholar] [CrossRef]
| Characteristic | Round 1 | Round 2 |
|---|---|---|
| Experts, n (%) | 15 (100%) | 15 (100%) |
| Sex | ||
| Female, n (%) | 11 (73%) | 11 (73%) |
| Male, n (%) | 4 (27%) | 4 (27%) |
| Profession | ||
| Physician, n (%) | 5 (33%) | 5 (33%) |
| Pharmacist, n (%) | 5 (33%) | 5 (33%) |
| Nurse, n (%) | 5 (33%) | 5 (33%) |
| Current work setting (multiple options possible) | ||
| Research, n (%) | 6 (40%) | 6 (40%) |
| Inpatient care, n (%) | 9 (60%) | 9 (60%) |
| Home care, n (%) | 4 (27%) | 4 (27%) |
| Long-term care, n (%) | 1 (7%) | 1 (7%) |
| Medical specialisation (multiple options possible) | ||
| Clinical pharmacy, n (%) | 5 (33%) | 5 (33%) |
| Hospital pharmacy, n (%) | 4 (27%) | 4 (27%) |
| General internal medicine, n (%) | 2 (13%) | 2 (13%) |
| Geriatrics, n (%) | 3 (20%) | 3 (20%) |
| Clinical pharmacology, n (%) | 1 (7%) | 1 (7%) |
| Advanced nurse practitioner, n (%) | 5 (33%) | 5 (33%) |
| N | Topic | Risk Factor | MRFR | SD | Med. | IQR | Min. | Max. | N Favourite Nominations |
|---|---|---|---|---|---|---|---|---|---|
| 1 | AG5 | Cognitive deficits | 5.4 | 0.6 | 5 | 1 | 4 | 6 | 9 |
| 2 | P4 | ≥8 medications | 5.4 | 0.9 | 6 | 1 | 3 | 6 | 2 |
| 3 | MM1 | Patient has no current medication list | 5.2 | 0.9 | 5 | 1 | 3 | 6 | 9 |
| 4 | MM5 | Patient has difficulty distinguishing medications or has visual difficulties | 5.1 | 0.8 | 5 | 1.5 | 4 | 6 | 4 |
| 5 | DIA7 | Renal dysfunction (GFR < 30 mL/min) | 5.1 | 0.7 | 5 | 0.75 | 4 | 6 | 4 |
| 6 | M9 | ≥3 psychotropic drugs (centrally acting analgesics, antipsychotics, antidepressants, benzodiazepines) | 5.1 | 0.9 | 5 | 1.5 | 3 | 6 | 4 |
| 7 | H11 | Hospital admission due to MRPs | 5.1 | 1.1 | 5 | 1 | 2 | 6 | 2 |
| 8 | M3 | Medications unsuitable for older adult patients (e.g., PRISCUS® list) | 5.0 | 0.8 | 5 | 2 | 4 | 6 | 5 |
| 9 | MM12 | Patient lacks an understanding of their therapy and/or illness | 5.0 | 0.9 | 5 | 0 | 2 | 6 | 2 |
| 10 | P3 | ≥7 medications | 5.0 | 1.1 | 5 | 2 | 3 | 6 | 0 |
| 11 | S4 | Communication problems and/or foreign language | 4.3 | 0.9 | 4 | 1 | 3 | 6 | 7 |
| 12 | M1 | Medication with narrow therapeutic range | 4.8 | 1.0 | 5 | 1.5 | 2 | 6 | 4 |
| 13 | MM10 | Patient takes medication without their doctor’s knowledge (including over-the-counter drugs) | 4.8 | 1.1 | 5 | 2 | 2 | 6 | 4 |
| 14 | P2 | ≥6 medications | 4.5 | 1.1 | 4 | 1.5 | 2 | 6 | 4 |
| 15 | H4 | Frequently changes physician | 4.2 | 1.5 | 5 | 1.75 | 0 | 6 | 4 |
| N° | Abbr. | Risk Factor | MRFR | SD | Med. | IQR | Min. | Max. | N Favourite Nominations |
|---|---|---|---|---|---|---|---|---|---|
| 1 | P9 | ≥10 medications | 5.5 | 0.6 | 6 | 1 | 4 | 6 | 4 |
| 2 | M23 | Duplicate prescriptions (e.g., generic and original) | 5.3 | 1.2 | 6 | 1 | 1 | 6 | 0 |
| 3 | M24 | High-risk drugs/groups of drugs | 5.2 | 0.6 | 5 | 1 | 4 | 6 | 7 |
| 4 | P10 | Clinically relevant interaction with no possible monitoring | 5.1 | 0.9 | 5 | 1 | 3 | 6 | 1 |
| 5 | MM2 | Poorly comprehensible therapy plan (complex therapy plans) | 5.1 | 0.7 | 5 | 0.5 | 4 | 6 | 3 |
| 6 | H23 | Several medication lists at the same time, especially if there are several prescribers (various specialists involved) | 5.0 | 1.0 | 5 | 0.5 | 2 | 6 | 3 |
| 7 | MM9 | Non-adherence/lack of compliance (e.g., incorrect intake due to not understanding the therapy) | 5.0 | 1.0 | 5 | 1.5 | 3 | 6 | 4 |
| 8 | MM22 | Lack of an up-to-date or correct medication list/no medication list | 5.0 | 0.6 | 5 | 0 | 4 | 6 | 4 |
| 9 | H15 | Changing prescribers (hospital, rehabilitation, general practitioner, specialist) | 4.7 | 1.1 | 5 | 1.5 | 2 | 6 | 6 |
| 10 | D5 | ≥75 years old, multimorbidity and polypharmacy | 4.7 | 1.1 | 5 | 1.5 | 3 | 6 | 6 |
| 11 | S8 | Homebound in combination with cognitive problems or a lack of social support | 4.6 | 1.1 | 5 | 1 | 2 | 6 | 6 |
| 12 | DIA13 | Neurocognitive disorder of any degree of severity | 4.6 | 1.0 | 5 | 1 | 3 | 6 | 7 |
| 13 | MM23 | Inadequate monitoring (irregular follow-up) | 4.5 | 0.8 | 5 | 1 | 3 | 6 | 4 |
| N° | Origin | Risk Factor | Intended Evaluators | |
|---|---|---|---|---|
| Delphi Round One | Delphi Round Two | |||
| 1 | AG5 | S8 DIA13 | Homebound in combination with cognitive problems or a lack of social support | Nurse |
| 2 | H4 (H11) | H15 H23 | Changing prescribers or several prescribers simultaneously (hospital, rehabilitation, general practitioner, specialist) | both |
| 3 | (H11) | new: expert | ≥4 emergency/hospital admissions or >3 rehospitalizations within the last 12 months | Nurse |
| 4 | (H11) | new: expert | Immediate transfer from hospital to home care | Nurse |
| 5 | DIA7 | --- | Renal dysfunction (GFR < 30 mL/min) | Pharmacist |
| 6 | P2 P3 P4 | P9 | ≥7 medications | Pharmacist |
| 7 | --- | D5 | ≥75 years old, multimorbidity and polypharmacy (≥4 medications) | Both |
| 8 | M1 | M24 | High-risk drugs/groups of drugs and/or drugs with a narrow therapeutic range (neuroleptics, especially lithium, digoxin, amiodarone and other antiarrhythmics; antiepileptics, especially phenytoin; phenobarbital; carbamazepine; oral anticoagulants, especially phenprocoumon; direct oral anticoagulants; insulins; methotrexate; theophylline) | Pharmacist |
| 9 | M9 | --- | ≥3 medications with an effect on the central nervous system (centrally acting analgesics; antipsychotics; antidepressants; benzodiazepines) | Pharmacist |
| 10 | M3 | --- | Medications unsuitable for older adult patients (e.g., PRISCUS® list) | Pharmacist |
| 11 | --- | M23 | Duplicate prescriptions (e.g., generic and original) | Pharmacist |
| 12 | MM1 | MM22 | Inadequate medication lists (absence of an up-to-date, understandable or correct medication list or simultaneous existence of several contradictory medication lists) | Both |
| 13 | MM5 | --- | Patient has difficulty distinguishing their tablets from one another, especially due to visual impairment | Nurse |
| 14 | S4 MM12 | MM2 | Patient lacks an understanding of their therapy and/or illness (cognition and/or communication problems, e.g., foreign language, hearing impairment) | Nurse |
| 15 | MM10 | MM9 | Non-adherence/lack of compliance (e.g., incorrect intake due to not understanding the therapy) and/or patient takes medication without the doctor’s knowledge (including self-purchased medication) | Nurse |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meyer-Massetti, C.; Lettieri-Amstutz, S.; Rölli, D.; Meier, C.R. The doMESTIC RISK Tool: Prioritising Home-Care Patients for Clinical Pharmacy Services with the Help of a Delphi Study. Nurs. Rep. 2025, 15, 158. https://doi.org/10.3390/nursrep15050158
Meyer-Massetti C, Lettieri-Amstutz S, Rölli D, Meier CR. The doMESTIC RISK Tool: Prioritising Home-Care Patients for Clinical Pharmacy Services with the Help of a Delphi Study. Nursing Reports. 2025; 15(5):158. https://doi.org/10.3390/nursrep15050158
Chicago/Turabian StyleMeyer-Massetti, Carla, Stefanie Lettieri-Amstutz, Daniela Rölli, and Christoph R. Meier. 2025. "The doMESTIC RISK Tool: Prioritising Home-Care Patients for Clinical Pharmacy Services with the Help of a Delphi Study" Nursing Reports 15, no. 5: 158. https://doi.org/10.3390/nursrep15050158
APA StyleMeyer-Massetti, C., Lettieri-Amstutz, S., Rölli, D., & Meier, C. R. (2025). The doMESTIC RISK Tool: Prioritising Home-Care Patients for Clinical Pharmacy Services with the Help of a Delphi Study. Nursing Reports, 15(5), 158. https://doi.org/10.3390/nursrep15050158






