Evaluating the Educational Video Materials for Radiation Education on Nursing Students and Nurses: A Quasi-Experimental Research
Abstract
1. Introduction
2. Materials and Methods
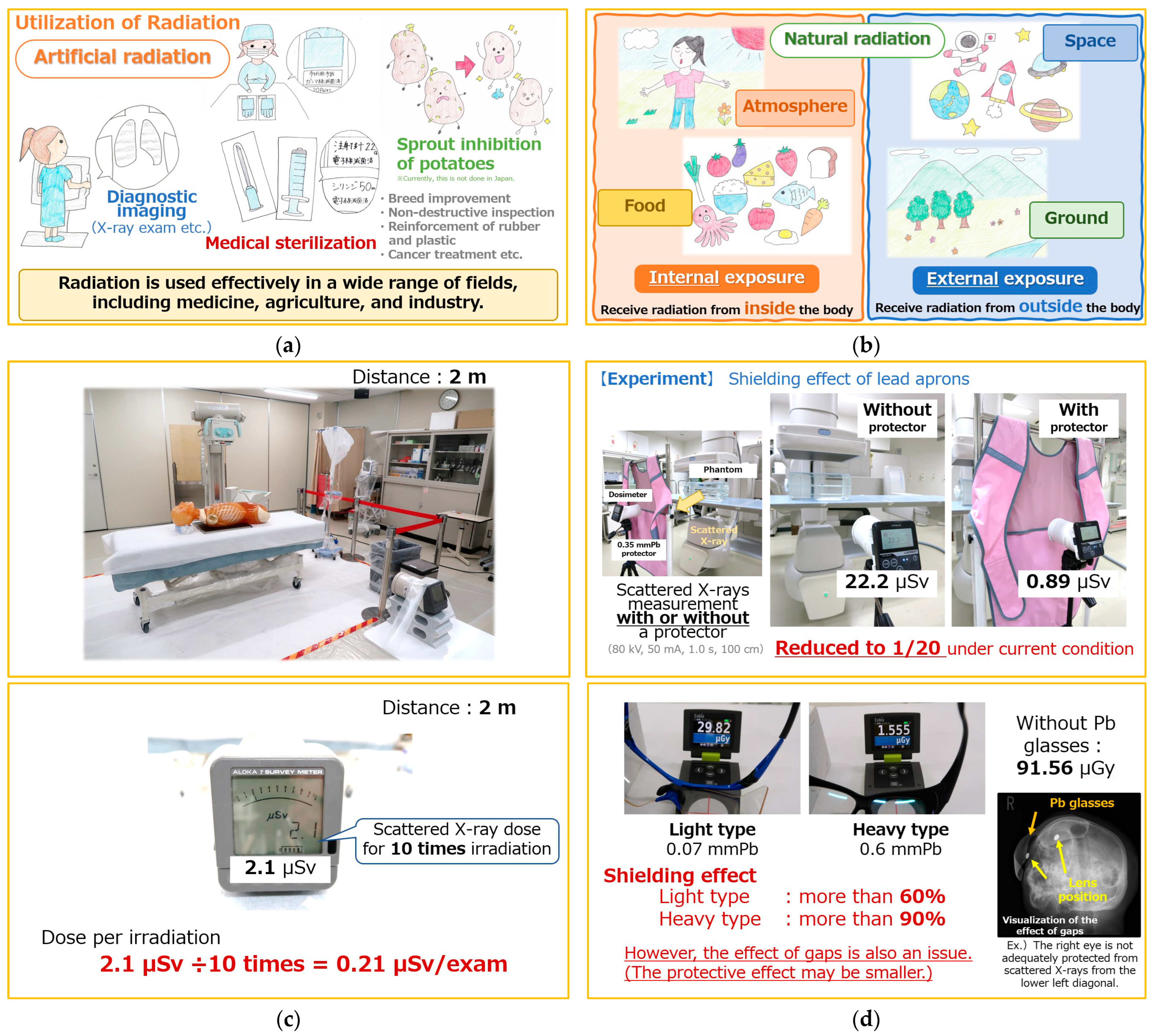
2.1. Development of Video Materials for Radiation Education
2.2. Outcome Measurements
2.2.1. Research Design
2.2.2. Participants
2.2.3. Survey Period
2.2.4. Knowledge of Nursing Students and Nurses Regarding Radiation
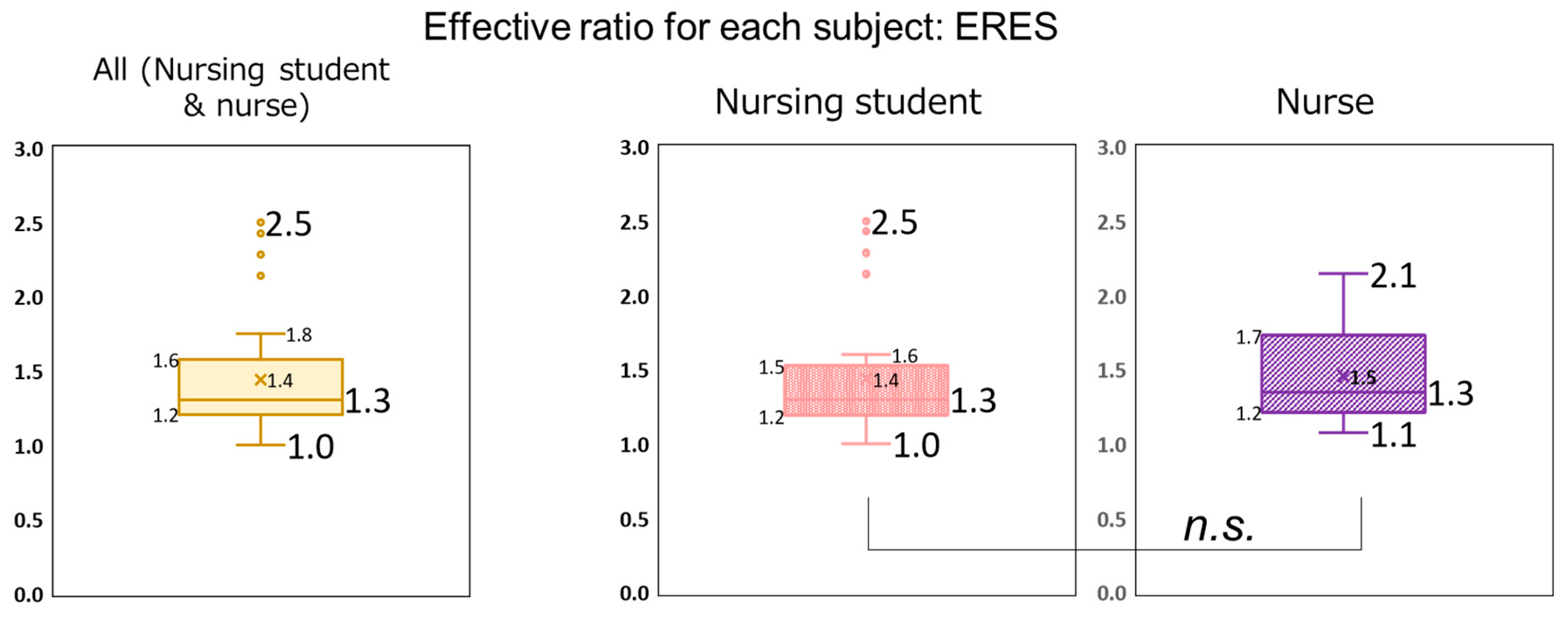
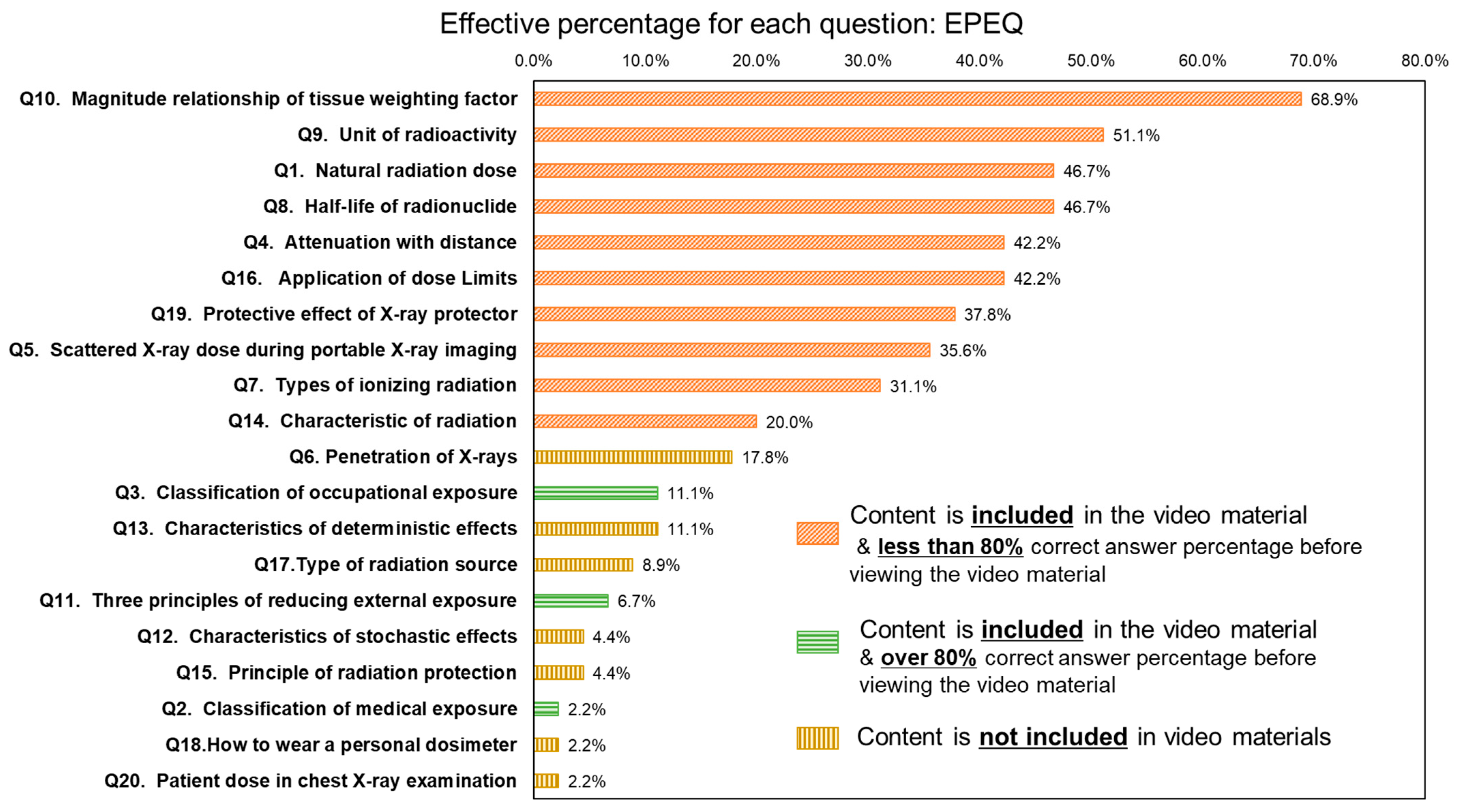
2.2.5. Evaluation of the Usefulness of the Developed Video Materials
2.2.6. Statistical Analysis
| No. | Question | Option | Coverage in the Teaching Materials |
|---|---|---|---|
| 1 | <Natural radiation dose> How much is the annual exposure dose from natural radiation in Japan? | a. 1.1 mSv/y b. 2.1 mSv/y * c. 3.1 mSv/y | Yes |
| 2 | <Classification of medical exposure> Which exposure categories apply to the patient? | a. Medical exposure * b. Occupational exposure c. Public exposure | Yes |
| 3 | <Classification of occupational exposure> Which exposure categories apply to medical staff? | a. Medical exposure b. Occupational exposure * c. Public exposure | Yes |
| 4 | <Attenuation with distance> If the distance from the radiation source is doubled, how small is the exposure dose? | a. One-half b. One-third c. One-fourth * d. One-fifth | Yes |
| 5 | <Scattered X-ray dose during portable X-ray imaging> In portable X-ray examination, what is the minimum distance from the patient at which scattered X-rays pose no problem? | a. 0.5 m b. 1 m c. 2 m * d. 5 m | Yes |
| 6 | <Penetration of X-rays> Which materials are most penetrable by X-rays? | a. Metal b. Fat * c. Water d. Bone | No |
| 7 | <Types of ionizing radiation> Which option is not included in ionizing radiation? | a. X-ray b. Alpha ray c. Ultraviolet * d. Neutron | No |
| 8 | <Half-life of radionuclide> What is the half-life of 131I? | a. 6 h b. 13 h c. 8 days * d. 30 years | Yes |
| 9 | <Unit of radioactivity> What is the unit of radioactivity? | a. Sv b. Gy c. Bq * | Yes |
| 10 | <Magnitude relationship of tissue weighting factor> What is the highest tissue weighting factor in the 2007 recommendations of the ICRP? | a. Lung * b. Gonads c. Esophagus d. Brain | Yes |
| 11 | <Three principles of reducing external exposure> Which is an inappropriate principle among the three for reducing external exposure? | a. Keep distance from the radiation source b. Take time to care for the patient * c. Use shielding | Yes |
| 12 | <Characteristics of stochastic effects> Which answer is false regarding stochastic effects? | a. Threshold exists * b. The frequency of effects increases with increasing dose c. Dose does not affect severity d. Cancer and leukemia exist | No |
| 13 | <Characteristics of deterministic effects> Which answer is false regarding deterministic effects (tissue reaction)? | a. Threshold exists b. Frequency of effects increases with increasing dose c. Cataract appears as a late effect d. Genetic effects exist * | No |
| 14 | <Characteristic of radiation> Which answer is a false characteristic of radiation? | a. Directness b. Penetrating effect c. Not felt by the 5 senses d. Cannot be measured * | Yes |
| 15 | <Principle of radiation protection> Which option is not applicable to the principle of radiation protection? | a. Justification b. Optimization of protection c. Strictness * d. Application of dose limits | No |
| 16 | <Application of dose limits> Which category is not applicable to the concept of dose limits? | a. Medical exposure * b. Occupational exposure c. Public exposure | Yes |
| 17 | <Type of radiation source> Which option is not a source of radiation? | a. natural b. radioisotope c. X-ray tube d. MRI * | No |
| 18 | <How to wear a personal dosimeter> When you perform a radiation procedure while wearing an X-ray protector (i.e., lead apron), where will you wear your personal dosimeter? | a. Inside the protector b. Outside the protector c. Outside and inside the protector * | No |
| 19 | <Protective effect of X-ray protector> By wearing an X-ray protector, how much can you reduce exposure due to scattered X-rays? | a. 30% b. 50% c. 70% d. 90% or more * | Yes |
| 20 | <Patient dose in chest X-ray examination> What is the effective dose to the patient during a chest X-ray examination? | a. 0.06 mSv * b. 0.5 mSv c. 1.0 mSv d. 5.0 mSv | No |
3. Results
3.1. Development of Video Materials for Radiation Education
3.2. Knowledge of Nursing Students and Nurses Regarding Radiation
3.3. Usefulness of the Developed Video Materials
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
Abbreviations
| CT | Computed tomography |
| EPEQ | Effective percentage for each question |
| ERES | Effective ratio for each subject |
| ICRP | International Commission on Radiological Protection |
References
- Rong, J.; Liu, Y. Advances in medical imaging techniques. BMC Methods 2024, 1, 10. [Google Scholar] [CrossRef]
- Brock, K.K.; Chen, S.R.; Sheth, R.A.; Siewerdsen, J.H. Imaging in interventional radiology: 2043 and beyond. Radiology 2023, 308, e230146. [Google Scholar] [CrossRef] [PubMed]
- Chida, K. What are useful methods to reduce occupational radiation exposure among radiological medical workers, especially for interventional radiology personnel? Radiol. Phys. Technol. 2022, 15, 101–115. [Google Scholar] [CrossRef]
- Yamada, A.; Haga, Y.; Sota, M.; Abe, M.; Kaga, Y.; Inaba, Y.; Suzuki, M.; Tada, N.; Zuguchi, M.; Chida, K. Eye lens radiation dose to nurses during cardiac interventional radiology: An initial study. Diagnostics 2023, 13, 3003. [Google Scholar] [CrossRef]
- Noro, T.; Osanai, M.; Hosokawa, S.; Kitajima, M.; Tsushima, M.; Kudo, K. Assessment of air dose distribution in the vertical plane for better occupational exposure management. Radiat. Prot. Dosim. 2024, 200, 1542–1546. [Google Scholar] [CrossRef] [PubMed]
- Osanai, M.; Sato, H.; Sato, K.; Kudo, K.; Hosoda, M.; Hosokawa, S.; Kitajima, M.; Tsushima, M.; Fujita, A.; Hosokawa, Y.; et al. Occupational radiation dose, especially for eye lens: Hp(3), in medical staff members involved in computed tomography examinations. Appl. Sci. 2021, 11, 4448. [Google Scholar] [CrossRef]
- Nagamoto, K.; Moritake, T.; Nakagami, K.; Morota, K.; Matsuzaki, S.; Nihei, S.I.; Kamochi, M.; Kunugita, N. Occupational radiation dose to the lens of the eye of medical staff who assist in diagnostic CT scans. Heliyon 2021, 7, e06063. [Google Scholar] [CrossRef]
- Konishi, E.; Nagai, T.; Kobayashi, M.; Mitsumori, Y.; Ono, W.; Asahara, K.; Porter, S.E. Post-Fukushima radiation education for public health nursing students: A case study. Int. Nurs. Rev. 2016, 63, 292–299. [Google Scholar] [CrossRef]
- Yoshida, K.; Orita, M.; Goto, A.; Kumagai, A.; Yasui, K.; Ohtsuru, A.; Hayashida, N.; Kudo, T.; Yamashita, S.; Takamura, N. Radiation-related anxiety among public health nurses in the Fukushima Prefecture after the accident at the Fukushima Daiichi Nuclear Power Station: A cross-sectional study. BMJ Open 2016, 6, e013564. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection. Publication 103. The 2007 Recommendations of the International Commission on Radiological Protection. Annals of the ICRP; Elsevier Limited: Amsterdam, The Netherlands, 2007. [Google Scholar]
- International Commission on Radiological Protection. Statement on Tissue Reactions; Ref., 4825-3093-1464; ICRP: Ottawa, ON, Canada, 2011. [Google Scholar]
- International Commission on Radiological Protection. Publication 118. ICRP Statement on Tissue Reactions/Early and Late Effects of Radiation in Normal Tissues and Organs-Threshold Doses for Tissue Reactions in a Radiation Protection Context. Annals of the ICRP; Elsevier Limited: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Hamada, N.; Azizova, T.V.; Little, M.P. An update on effects of ionizing radiation exposure on the eye. Br. J. Radiol. 2020, 93, 20190829. [Google Scholar] [CrossRef]
- Barnard, S.G.; Ainsbury, E.A.; Quinlan, R.A.; Bouffler, S.D. Radiation protection of the eye lens in medical workers—Basis and impact of the ICRP recommendations. Br. J. Radiol. 2016, 89, 20151034. [Google Scholar] [CrossRef]
- Morishima, Y.; Chida, K.; Shigeizumi, K.; Katahira, Y.; Seto, H. Importance of radiation education for nurses. Nihon Hoshasen Gijutsu Gakkai Zasshi 2012, 68, 1373–1378. [Google Scholar] [CrossRef] [PubMed]
- Cornacchia, S.; Errico, R.; La Tegola, L.; Maldera, A.; Simeone, G.; Fusco, V.; Niccoli-Asabella, A.; Rubini, G.; Guglielmi, G. The new lens dose limit: Implication for occupational radiation protection. Radiol. Med. 2019, 124, 728–735. [Google Scholar] [CrossRef]
- Fujibuchi, T. Radiation protection education using virtual reality for the visualisation of scattered distributions during radiological examinations. J. Radiol. Prot. 2021, 41, S317–S328. [Google Scholar] [CrossRef]
- Matsuzaki, S.; Moritake, T.; Morota, K.; Nagamoto, K.; Nakagami, K.; Kuriyama, T.; Kunugita, N. Development and assessment of an educational application for the proper use of ceiling-suspended radiation shielding screens in angiography rooms using augmented reality technology. Eur. J. Radiol. 2021, 143, 109925. [Google Scholar] [CrossRef]
- Osanai, M.; Tamura, R.; Tanaka, C.; Mikami, H.; Noro, T.; Kudo, K.; Hosokawa, S.; Tsushima, M.; Yamaguchi, I.; Hosoda, M.; et al. Visualization of scattered X-rays sources using a pinhole camera in general radiography, computed tomography examinations, and interventional radiology. J. Radiol. Nurs. Soc. Jpn. 2024, 12, 44–53. (In Japanese) [Google Scholar]
- Dianati, M.; Zaheri, A.; Talari, H.R.; Deris, F.; Rezaei, S. Intensive care nurses’ knowledge of radiation safety and their behaviors towards portable radiological examinations. Nurs. Midwif. Stud. 2014, 3, e23354. [Google Scholar] [CrossRef]
- Bwanga, O.; Kayembe, R.M. Awareness of nurses to Radiation Protection in Medicine. Int. J. Med. Rev. 2020, 7, 78–84. [Google Scholar]
- The Radiological Nursing Society of Japan. A Model Syllabus for Radiation Nursing (Provisional Translation). 2019. Available online: https://www.rnsj.jp/guidelines-publications/model-core-curriculum/ (accessed on 27 February 2025).
- Sasatake, H.; Kitajima, M.; Urushizaka, M.; Noto, Y. Current status and issues of radiological nursing education of nursing faculty involved in basic nursing education. J. Radiol. Nurs. Soc. Jpn. 2017, 5, 23–30. (In Japanese) [Google Scholar] [CrossRef]
- Aoki, H.; Miyoshi, M.; Monji, M.; Kubota, K.; Aoki, N. Clinical instructors’ difficulties in teaching nursing students how to solve mathematics and physics problems. J. Biomed. Fuzzy Syst. Assoc. 2018, 20, 23–28. (In Japanese) [Google Scholar]
- Goula, A.; Chatzis, A.; Stamouli, M.A.; Kelesi, M.; Kaba, E.; Brilakis, E. Assessment of Health Professionals’ Attitudes on Radiation Protection Measures. Int. J. Environ. Res. Public Health 2021, 18, 13380. [Google Scholar] [CrossRef]
- Nishikawa, A.; Yamaguchi, T.; Yamada, Y.; Urata, H.; Shinkawa, T.; Matsunari, Y. How do disaster relief nurses in Japan perceive and respond to risks? A cross-sectional study. Nurs. Rep. 2023, 13, 1410–1420. [Google Scholar] [CrossRef] [PubMed]
- Oishi, F.; Shiratori, S.; Ito, M.; Yamahata, A. Anxiety in radiology nurses about occupational exposure: A qualitative analysis. J. Radiol. Nurs. Soc. Jpn. 2018, 6, 22–32. (In Japanese) [Google Scholar] [CrossRef]
- Jeyasugiththan, J.; Dissanayake, D.M.T.P.B.; Kohombakadawala, I.M.C.W.B.; Satharasinghe, D.M. Assessment of the awareness of radiation protection and related concepts among nursing staff mainly working in diagnostic imaging units, cath-labs and operation theatres in Sri Lanka: A survey-based study. Radiography 2023, 29, 319–326. [Google Scholar] [CrossRef]
- Shafiq, P.; Mehmood, Y. Awareness of radiation hazards and knowledge about radiation protection among medical students at the Northern Border University, Arar. Cureus 2024, 16, e55484. [Google Scholar] [CrossRef]
- Alyousef, K.; Assiri, A.; Almutairi, S.; Aldalham, T.; Felimban, G. Awareness of radiation protection and common radiation dose levels among healthcare workers. Glob. J. Qual. Saf. Healthc. 2023, 6, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, A.M.; Nurdin, I.; Ismail, S.; Khalil, A. Malaysian nurses’ knowledge of radiation protection: A cross-sectional study. Radiol. Res. Pract. 2021, 2021, 5566654. [Google Scholar] [CrossRef]
- Salih, S.; Nordin, M.N.; Alkatheeri, A.; Nasser, A.; Saif, M.; Abdallah, Z.; Alderei, A.; Faisal, L.A.; Alhasan, M.; Hasaneen, M. Assessment of Nursing Students’ Awareness toward Ionizing Radiation: Cross-Sectional Study. Nurs. Rep. 2023, 13, 855–864. [Google Scholar] [CrossRef]
- Hirvonen, L.; Schroderus-Salo, T.; Henner, A.; Ahonen, S.; Kääriäinen, M.; Miettunen, J.; Mikkonen, K. Nurses’ knowledge of radiation protection: A cross-sectional study. Radiography 2019, 25, e108–e112. [Google Scholar] [CrossRef]
- Kanda, R.; Tsuji, S.; Shirakawa, Y.; Yonehara, H. Preliminary survey for communicating risk in medical exposure--perception of risk among nurses working in radiology. Nihon Hoshasen Gijutsu Gakkai Zasshi 2008, 64, 937–947. [Google Scholar] [CrossRef][Green Version]
- Vorwerk, H.; Engenhart-Cabillic, R. Students’ learning behavior in digital education for radiation oncology. Strahlenther. Onkol. 2022, 198, 12–24. [Google Scholar] [CrossRef] [PubMed]
| Number of Answers | Percentage of Correct Answers | χ2 | p | φ/ Cramer’s V | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| a | b | c | d | Total | ||||||
| Q1 Natural radiation dose | Nursing student | 7 | 20 | 2 | - | 69.0% | 53.3% | 8.12 | 0.017 * | 0.43 |
| Nurse | 10 | 4 | 2 | - | 25.0% | |||||
| Q2 Classification of medical exposure | Nursing student | 28 | 0 | 1 | - | 96.6% | 97.8% | 0.56 | 0.45 | 0.11 |
| Nurse | 16 | 0 | 0 | - | 100.0% | |||||
| Q3 Classification of occupational exposure | Nursing student | 3 | 26 | 0 | - | 89.7% | 88.9% | 0.048 | 0.83 | 0.033 |
| Nurse | 2 | 14 | 0 | - | 87.5% | |||||
| Q4 Attenuation with distance | Nursing student | 9 | 2 | 18 | 0 | 62.1% | 57.8% | 0.735 | 0.69 | 0.13 |
| Nurse | 7 | 1 | 8 | 0 | 50.0% | |||||
| Q5 Scattered X-ray dose during portable X-ray imaging | Nursing student | 0 | 5 | 20 | 4 | 69.0% | 62.2% | 1.67 | 0.43 | 0.19 |
| Nurse | 0 | 5 | 8 | 3 | 50.0% | |||||
| Q6 Penetration of X-rays | Nursing student | 5 | 7 | 11 | 6 | 24.1% | 20.0% | 1.29 | 0.73 | 0.17 |
| Nurse | 2 | 2 | 8 | 4 | 12.5% | |||||
| Q7 Types of ionizing radiation | Nursing student | 1 | 2 | 18 | 8 | 62.1% | 66.7% | 1.15 | 0.77 | 0.16 |
| Nurse | 0 | 1 | 12 | 3 | 75.0% | |||||
| Q8 Half-life of radionuclide | Nursing student | 1 | 5 | 18 | 5 | 62.1% | 46.7% | 9.59 | 0.022 * | 0.46 |
| Nurse | 3 | 7 | 3 | 3 | 18.8% | |||||
| Q9 Unit of radioactivity | Nursing student | 21 | 7 | 1 | - | 3.4% | 13.3% | 8.27 | 0.016 * | 0.43 |
| Nurse | 6 | 5 | 5 | - | 31.3% | |||||
| Q10 Magnitude relationship of tissue weighting factor | Nursing student | 5 | 15 | 3 | 6 | 17.2% | 17.8% | 0.267 | 0.97 | 0.077 |
| Nurse | 3 | 9 | 1 | 3 | 18.8% | |||||
| Q11 Three principles of reducing external exposure | Nursing student | 2 | 25 | 2 | - | 86.2% | 88.9% | 1.18 | 0.56 | 0.16 |
| Nurse | 1 | 15 | 0 | - | 93.8% | |||||
| Q12 Characteristics of stochastic effects | Nursing student | 6 | 8 | 14 | 1 | 20.7% | 17.8% | 5.16 | 0.16 | 0.34 |
| Nurse | 2 | 1 | 13 | 0 | 12.5% | |||||
| Q13 Characteristics of deterministic effects | Nursing student | 1 | 6 | 4 | 18 | 62.1% | 62.2% | 4.26 | 0.23 | 0.31 |
| Nurse | 1 | 0 | 4 | 10 | 62.5% | |||||
| Q14 Characteristic of radiation | Nursing student | 6 | 2 | 6 | 15 | 51.7% | 53.3% | 0.812 | 0.85 | 0.13 |
| Nurse | 3 | 2 | 2 | 9 | 56.3% | |||||
| Q15 Principle of radiation protection | Nursing student | 15 | 0 | 13 | 1 | 44.8% | 35.6% | 3.76 | 0.15 | 0.29 |
| Nurse | 11 | 0 | 3 | 2 | 18.8% | |||||
| Q16 Application of dose Limits | Nursing student | 2 | 4 | 23 | - | 6.9% | 11.1% | 3.52 | 0.17 | 0.28 |
| Nurse | 3 | 0 | 13 | - | 18.8% | |||||
| Q17 Type of radiation source | Nursing student | 5 | 8 | 4 | 12 | 41.4% | 55.6% | 6.76 | 0.080 | 0.39 |
| Nurse | 1 | 1 | 1 | 13 | 81.3% | |||||
| Q18 How to wear a personal dosimeter | Nursing student | 6 | 6 | 16 | - | 55.2% | 57.8% | 0.553 | 0.76 | 0.11 |
| Nurse | 4 | 2 | 10 | - | 62.5% | |||||
| Q19 Protective effect of X-ray protector | Nursing student | 0 | 1 | 11 | 17 | 58.6% | 62.2% | 3.38 | 0.34 | 0.27 |
| Nurse | 1 | 1 | 3 | 11 | 68.8% | |||||
| Q20 Patient dose in chest X-ray examination | Nursing student | 10 | 12 | 5 | 2 | 34.5% | 44.4% | 3.85 | 0.28 | 0.29 |
| Nurse | 10 | 4 | 2 | 0 | 62.5% | |||||
| Nursing Student | Nurse | ||||
|---|---|---|---|---|---|
| Score | Score | ||||
| Subject | Before | After | Subject | Before | After |
| 1 | 12 | 15 | 1 | 8 | 14 |
| 2 | 10 | 13 | 2 | 8 | 14 |
| 3 | 10 | 15 | 3 | 14 | 15 |
| 4 | 12 | 17 | 4 | 10 | 12 |
| 5 | 9 | 11 | 5 | 12 | 13 |
| 6 | 6 | 15 | 6 | 12 | 16 |
| 7 | 13 | 13 | 7 | 10 | 13 |
| 8 | 9 | 13 | 8 | 13 | 15 |
| 9 | 7 | 15 | 9 | 11 | 15 |
| 10 | 13 | 17 | 10 | 8 | 14 |
| 11 | 14 | 16 | 11 | 12 | 15 |
| 12 | 10 | 16 | 12 | 9 | 14 |
| 13 | 7 | 17 | 13 | 7 | 15 |
| 14 | 10 | 11 | 14 | 9 | 12 |
| 15 | 10 | 13 | 15 | 9 | 14 |
| 16 | 14 | 17 | 16 | 9 | 15 |
| 17 | 10 | 13 | |||
| 18 | 11 | 14 | |||
| 19 | 6 | 7 | |||
| 20 | 12 | 14 | |||
| 21 | 7 | 16 | |||
| 22 | 8 | 11 | |||
| 23 | 9 | 13 | |||
| 24 | 11 | 11 | |||
| 25 | 9 | 14 | |||
| 26 | 11 | 14 | |||
| 27 | 13 | 14 | |||
| 28 | 12 | 15 | |||
| 29 | 10 | 16 | |||
| Mean | 10.2 | 14.0 | Mean | 10.1 | 14.1 |
| p-value | <0.001 | p-value | <0.001 | ||
| Comment (Partial Excerpt/Summary) |
|---|
| <Good point> |
| -The video and examples of experiments were very easy to understand. -The scenes of experiments were interesting. -The handwritten illustrations were warm and friendly. -The actual irradiation scene was easy to visualize without portable X-ray equipment. -There were many explanations with diagrams; therefore, concepts were easy to understand visually. |
| <Difficult point to understand> |
| -The amount of information contained in one slide was excessive, and understanding the important points was difficult. -The explanations were too simple, and I could not understand them. |
| <Points to be improved> |
| -I need more detailed explanations in some parts. -I want to see a separate video for each section. -I think that it would be better if there was a quiz in the middle section to prevent sleepiness. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osanai, M.; Nishizawa, Y.; Noto, Y.; Tsuchiya, R. Evaluating the Educational Video Materials for Radiation Education on Nursing Students and Nurses: A Quasi-Experimental Research. Nurs. Rep. 2025, 15, 159. https://doi.org/10.3390/nursrep15050159
Osanai M, Nishizawa Y, Noto Y, Tsuchiya R. Evaluating the Educational Video Materials for Radiation Education on Nursing Students and Nurses: A Quasi-Experimental Research. Nursing Reports. 2025; 15(5):159. https://doi.org/10.3390/nursrep15050159
Chicago/Turabian StyleOsanai, Minoru, Yoshiko Nishizawa, Yuka Noto, and Ryoko Tsuchiya. 2025. "Evaluating the Educational Video Materials for Radiation Education on Nursing Students and Nurses: A Quasi-Experimental Research" Nursing Reports 15, no. 5: 159. https://doi.org/10.3390/nursrep15050159
APA StyleOsanai, M., Nishizawa, Y., Noto, Y., & Tsuchiya, R. (2025). Evaluating the Educational Video Materials for Radiation Education on Nursing Students and Nurses: A Quasi-Experimental Research. Nursing Reports, 15(5), 159. https://doi.org/10.3390/nursrep15050159





