Relationship Between Obesity and Impairment of Cognitive Functions: An Investigation into the Integrated Role of Nutritional Education and Physical Activity in Lower Secondary School
Abstract
1. Introduction
2. Materials and Methods
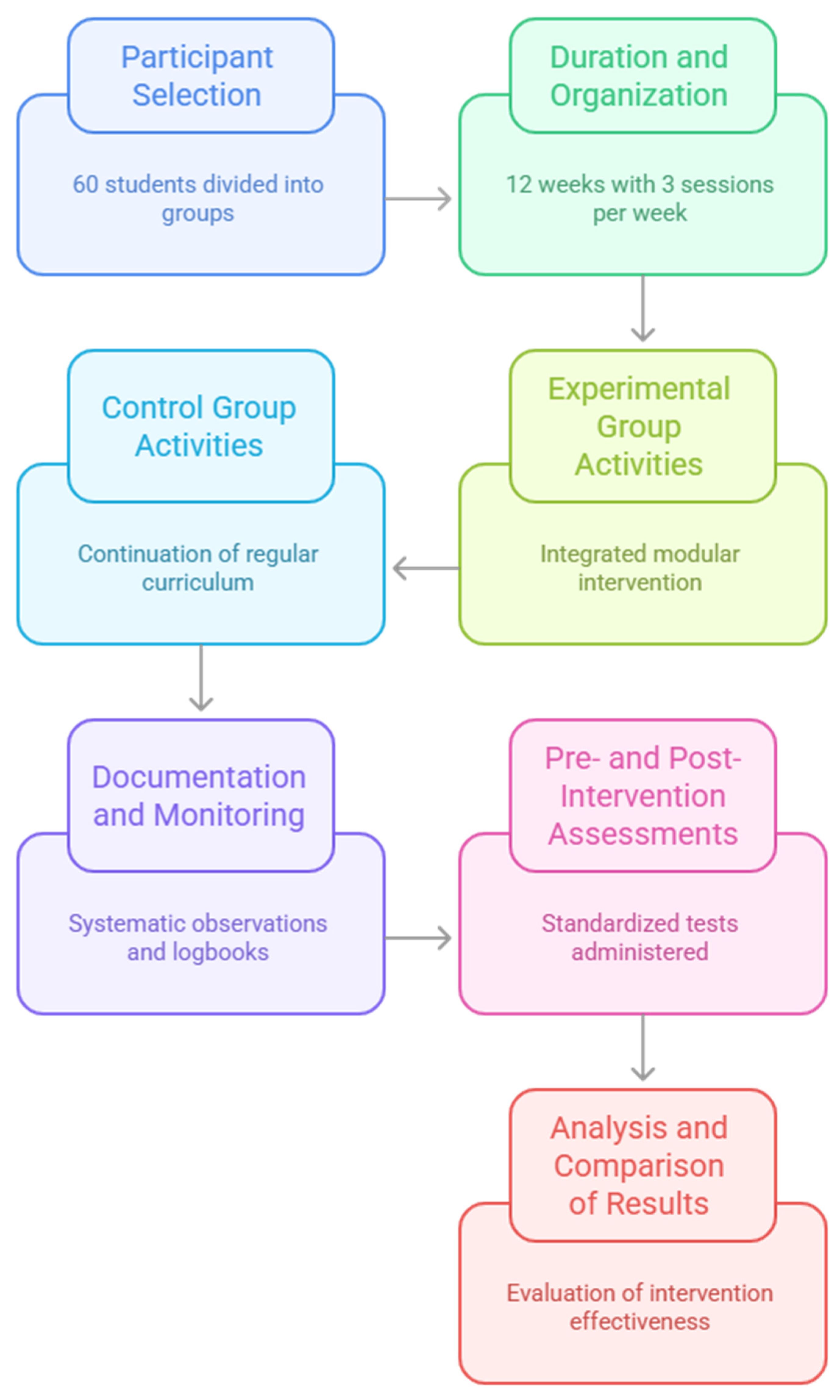
2.1. Study Design
2.2. Participants
2.3. Procedures
2.4. Experimental Intervention
- Nutritional Education Intervention
- Physical Activity Intervention
| Week | Nutritional Education (1 Weekly Session) | Physical Activity (2 Weekly Sessions) |
|---|---|---|
| 1 | Introduction to the relationship between nutrition and the brain: how food influences mental performance | Basic body awareness: posture, breathing, relaxation |
| 2 | Macronutrients and cognitive functions: focus on carbohydrates, proteins, fats | Dynamic postural education and breath control |
| 3 | Glycemic index, attention and memory: effects of glycemic fluctuations | Balance exercises, motor control and spatiotemporal perception |
| 4 | Physiological vs. emotional hunger: self-regulation and bodily signals | Simple coordination paths and progressively challenging games |
| 5 | Nutrition labels: reading and critical interpretation | Rhythmic activities, attention and reaction games, motor memory tasks |
| 6 | Breakfast and school meals: impact on cognitive performance | Dual-task exercises: integration of motor tasks and cognitive challenges |
| 7 | Food and concentration: brain-friendly nutrients | Group motor paths with cooperative and decision-making tasks |
| 8 | Sugary drinks and attention decline | Outdoor activities: paced walking and environmental observation |
| 9 | Inflammation and obesity: effects on the brain and behavior | Spatial orientation games and environmental recognition |
| 10 | Building a balanced meal: nutritional logic and sustainability | Narrative motor activities in outdoor settings: movement and storytelling |
| 11 | Food stereotypes and social influences on eating choices | Multisensory motor experiences: bodily exploration of natural environments |
| 12 | Final reflection and self-assessment: toward conscious food choices | Integrative activities: review of motor and cognitive learning outcomes |
2.5. Measures
- Assessment of cognitive functions
- Digit Span Test—Forward and Backward (Wechsler Intelligence Scale for Children, WISC-IV)
- The Digit Span Test [27] was used to assess working memory and short-term attention. In the Forward version, the student must repeat a sequence of digits in the order presented, while in the Backward version, the student is required to repeat the digits in reverse order. Increasing the length of the sequence allows you to estimate the ability to actively maintain and manipulate information in memory. The Digit Span Test, both Forward and Backward, was used to assess working memory capacity. Previous research has reported acceptable internal consistency, with Cronbach’s alpha values ranging from 0.70 to 0.80 in school-aged children [28].
- Stroop Color and Word Test—Children’s Version
- The Stroop Color and Word Test [29] is a well-established tool for measuring inhibitory control and cognitive flexibility. Participants are asked to name the color of the ink while ignoring the semantic meaning of the written word. The test allows us to highlight the efficiency of the processes of automatic inhibition, switching and selective attention, considered sensitive markers of executive efficiency in developmental age. The Children’s Version of the Stroop Color and Word Test was employed to measure selective attention and cognitive inhibition. The test demonstrates satisfactory reliability, with Cronbach’s alpha values typically reported between 0.75 and 0.85 [30].
- Trail Making Test—Parts A and B (version adapted for school age)
- The Trail Making Test [31] assesses processing speed, the ability to toggle between different cognitive sets (letters and numbers), and the executive organization of behavior. The completion times of the two parts of the test, as well as the errors made, offer useful indicators of the level of cognitive flexibility and visuospatial planning. The adapted school-age version of the Trail Making Test (Parts A and B) was used to evaluate cognitive flexibility and processing speed. Test–retest reliability for children has been reported as good, with ICC values around 0.80 [32].
- Raven’s Progressive Matrices Test—Coloured Progressive Matrices (CPMs)
- Included as a measure of nonverbal logical reasoning and the ability to solve abstract visual problems, the Raven test [33] also allows us to detect any general differences in intellectual functioning between groups, controlling for any pre-existing cognitive biases. Raven’s Coloured Progressive Matrices (CPMs) were administered to assess non-verbal fluid intelligence. The internal consistency of the CPM is high, with Cronbach’s alpha typically above 0.85 [34].
- Assessment of motor and functional condition
- 6-Minute Walk Test (6MWT)
- The 6-Minute Walk Test [35] was used to estimate cardiorespiratory capacity and functional aerobic endurance. The test requires participants to cover the maximum possible distance in six minutes on a straight track. It was chosen for its validity in school contexts and sensitivity to changes related to regular physical activity. The 6-Minute Walk Test (6MWT) was used to evaluate submaximal aerobic capacity and functional endurance. Reliability studies in children report high test–retest reliability with ICC values ranging from 0.90 to 0.95 [36].
- Sit and Reach Test
- The Sit and Reach Test [37] measures the flexibility of the lower back and hamstrings. Although not directly related to cognitive functions, it represents a general index of muscle tone and joint mobility, influenced by the level of sedentary lifestyle. The Sit and Reach Test was administered to assess hamstring and lower back flexibility. It is a widely used field test with good test–retest reliability, with ICC values typically between 0.85 and 0.92 in children [38].
- Assessment of anthropometric parameters
- Body Mass Index (BMI)
- According to the criteria defined by Cole in 2002 [39], the body mass index (BMI) was calculated for each participant using the weight divided by height squared formula, expressed in kilograms per square meter (kg/m2), and interpreted with reference to internationally validated age- and sex-specific cut-offs for the pediatric population. This indicator was used both as a measure of weight status and as a continuous variable in the analysis of pre- and post-intervention variations, with the aim of detecting any changes in the body profile attributable to educational and motor interventions. Body Mass Index (BMI) was calculated using standardized procedures. Anthropometric measurements were conducted by trained personnel, and BMI demonstrates high inter-rater reliability, with ICC values exceeding 0.95 [40].
- Waist Circumference
- Abdominal circumference [41] was measured at the height of the navel with millimeter tape, as an additional indicator of metabolic risk and central fat accumulation, as it is more related to neuroinflammatory risks than BMI alone. Waist circumference was measured using a non-elastic tape at the midpoint between the last rib and the iliac crest. This measure has shown excellent inter-rater reliability in pediatric populations, with ICC values above 0.90 [42].
- Assessment of Nutritional Intervention
- Questionnaire on nutritional knowledge (adapted from Parmenter & Wardle, 1999 [43])
- We used a simplified version of this questionnaire adapted for school age [43], aimed at verifying the understanding of fundamental concepts related to food groups, energy requirements, meal balance and reading nutrition labels. It includes multiple choice and true/false questions, structured in thematic sections. The overall score makes it possible to quantify the effectiveness of the educational path in terms of knowledge acquisition. Nutritional knowledge was assessed using a questionnaire adapted from Parmenter and Wardle [43], which has demonstrated good internal consistency in various populations, with reported Cronbach’s alpha values around 0.78.
2.6. Statistical Analysis
3. Results
3.1. Confirmatory Factor Analysis and Construct Validity of the Measurement Scales
- Overall KMO = 0.81;
- Bartlett’s test: χ2(36) = 228.54, p < 0.001;
- χ2/df = 1.89;
- CFI = 0.95;
- TLI = 0.93;
- RMSEA = 0.064, 90% CI [0.048, 0.078];
- SRMR = 0.051.
3.2. Descriptive Statistics of Pre- and Post-Test Measurements
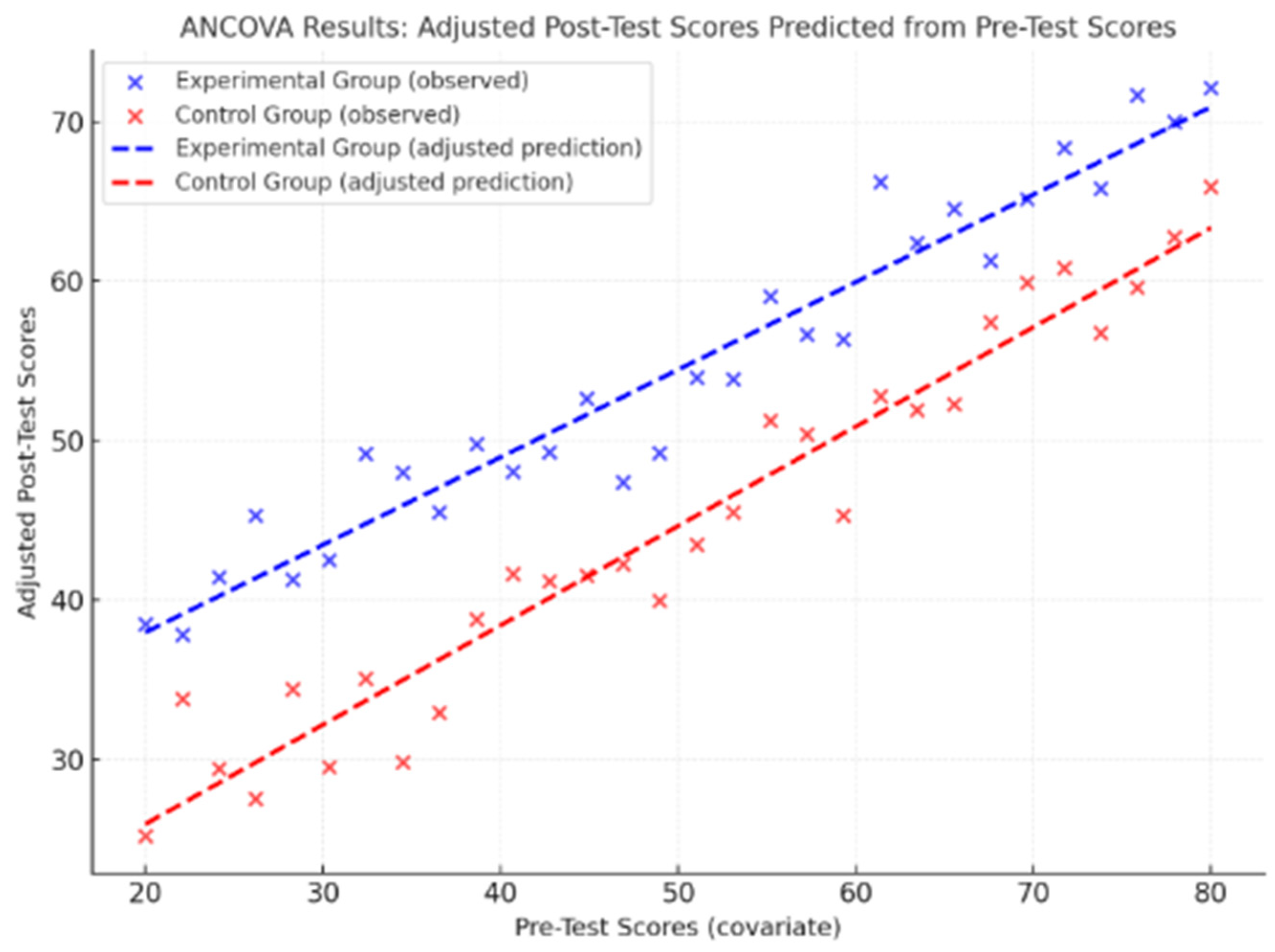
3.3. ANCOVA
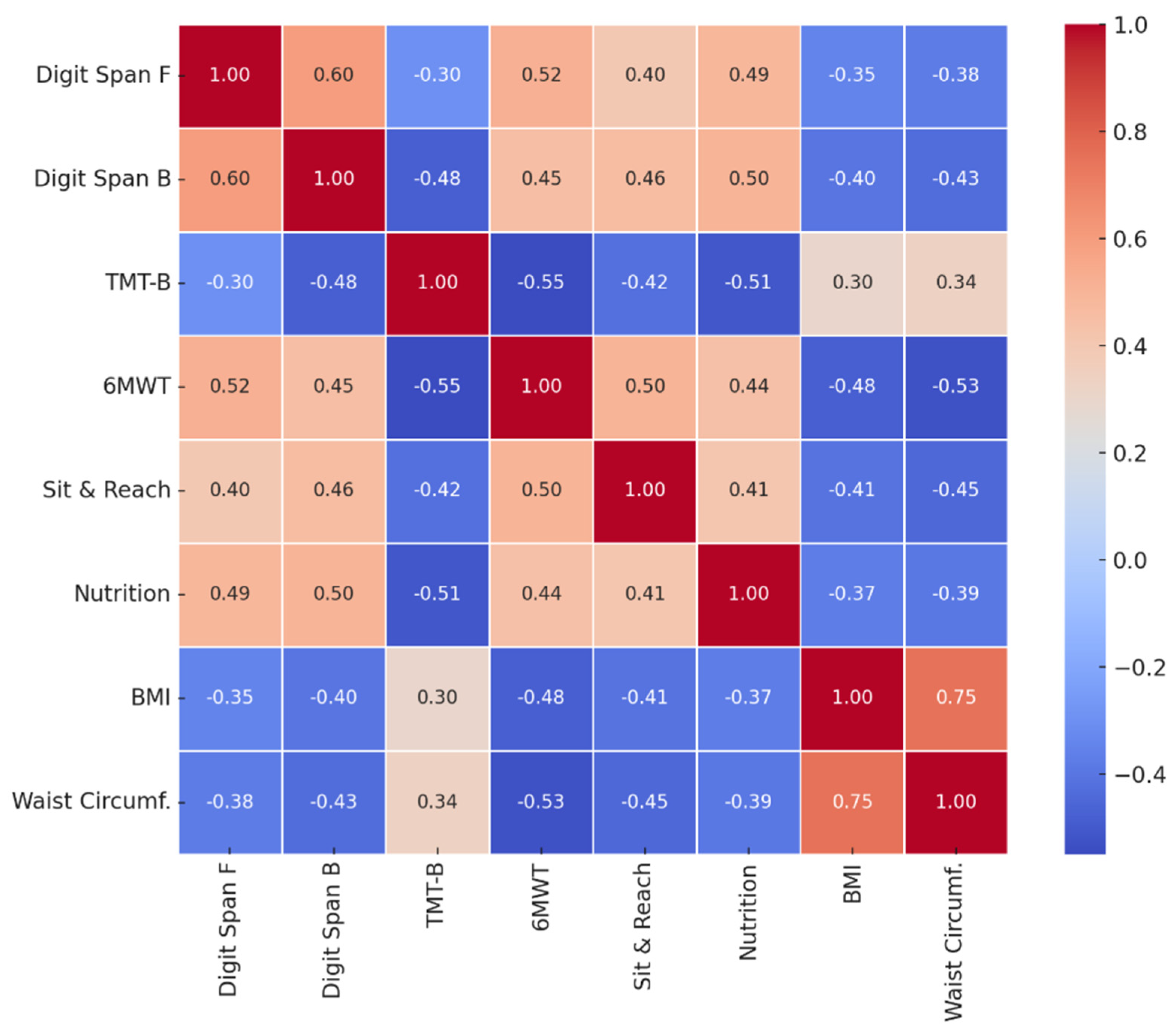
3.4. Pearson Correlation
4. Discussion
5. Conclusions
6. Practical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nogueira-de-Almeida, C.A.; Weffort, V.R.S.; Ued, F.D.V.; Ferraz, I.S.; Contini, A.A.; Martinez, E.Z.; Del Ciampo, L.A. What causes obesity in children and adolescents? J. De Pediatr. 2024, 100, S48–S56. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Overweight and Obesity. 2020. Available online: https://www.oecd.org/en/publications/health-at-a-glance-asia-pacific-2020_26b007cd-en.html (accessed on 2 April 2025).
- Chen, J.; Bai, Y.; Ni, W. Reasons and promotion strategies of physical activity constraints in obese/overweight children and adolescents. Sports Med. Health Sci. 2024, 6, 25–36. [Google Scholar] [CrossRef]
- Valerio, G.; Di Bonito, P.; Calcaterra, V.; Cherubini, V.; Corica, D.; De Sanctis, L.; Di Sessa, A.; Faienza, M.F.; Fornari, E.; Iughetti, L.; et al. Cardiometabolic risk in children and adolescents with obesity: A position paper of the Italian Society for Pediatric Endocrinology and Diabetology. Ital. J. Pediatr. 2024, 50, 205. [Google Scholar] [CrossRef] [PubMed]
- Formisano, A.; Iacomino, G.; Dello Russo, M.; Russo, P.; Siani, A.; Lauria, F. European Nutritional Guidelines for the Management of Childhood Obesity: The Role of Personalised Nutrition. In The Microbiome and Personalized Nutrition; Springer Nature: Cham, Switzerland, 2025; pp. 67–103. [Google Scholar]
- Kang, E.; Hong, Y.H.; Kim, J.; Chung, S.; Kim, K.K.; Haam, J.H.; Kim, B.T.; Kim, E.M.; Park, J.H.; Rhee, S.Y.; et al. Obesity in children and adolescents: 2022 update of clinical practice guidelines for obesity by the Korean Society for the Study of Obesity. J. Obes. Metab. Syndr. 2024, 33, 11. [Google Scholar] [CrossRef]
- Liang, J.; Matheson, B.E.; Kaye, W.H.; Boutelle, K.N. Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int. J. Obes. 2014, 38, 494–506. [Google Scholar] [CrossRef] [PubMed]
- Üney, E.; Baykara, H.B.; Avcil, S. Evaluation of executive functions in children and adolescents with obesity. Appl. Neuropsychol. Child 2025, 14, 368–376. [Google Scholar] [CrossRef]
- Tello, B.; Ocaña, J.; García-Zambrano, P.; Enríque-Moreira, B.; Dueñas-Espín, I. Determinants of overweight and obesity among children between 5 to 11 years in Ecuador: A secondary analysis from the National Health Survey 2018. PLoS ONE 2024, 19, e0296538. [Google Scholar] [CrossRef]
- Giugliano, R.; Carneiro, E.C. Factors associated with obesity in school children. J. Pediatr. 2004, 80, 17–22. [Google Scholar] [CrossRef]
- Dobashi, K. Evaluation of obesity in school-age children. J. Atheroscler. Thromb. 2016, 23, 32–38. [Google Scholar] [CrossRef]
- Li, J.; Hooker, N.H. Childhood obesity and schools: Evidence from the national survey of children’s health. J. Sch. Health 2010, 80, 96–103. [Google Scholar] [CrossRef]
- Sharma, N.; Sanjeevi, R.R.; Balasubramanian, K.; Chahal, A.; Sharma, A.; Sidiq, M. A systematic review on prevalence of overweight and obesity among school children and adolescents in Indian population. Indian J. Endocrinol. Metab. 2024, 28, 104–116. [Google Scholar] [CrossRef] [PubMed]
- Watts, A.W.; Rydell, S.A.; Eisenberg, M.E.; Laska, M.N.; Neumark-Sztainer, D. Yoga’s potential for promoting healthy eating and physical activity behaviors among young adults: A mixed-methods study. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 42. [Google Scholar] [CrossRef] [PubMed]
- De Sá, C.A.; Saretto, C.B.; Cardoso, A.M.; Remor, A.; Breda, C.O.; da Silva Corralo, V. Effects of a physical exercise or motor activity protocol on cognitive function, lipid profile, and BDNF levels in older adults with mild cognitive impairment. Mol. Cell. Biochem. 2024, 479, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Latomme, J.; Calders, P.; Van Waelvelde, H.; Mariën, T.; De Craemer, M. The role of brain-derived neurotrophic factor (BDNF) in the relation between physical activity and executive functioning in children. Children 2022, 9, 596. [Google Scholar] [CrossRef]
- Obita, G.; Alkhatib, A. Effectiveness of lifestyle nutrition and physical activity interventions for childhood obesity and associated comorbidities among children from minority ethnic groups: A systematic review and meta-analysis. Nutrients 2023, 15, 2524. [Google Scholar] [CrossRef]
- Motevalli, M.; Drenowatz, C.; Tanous, D.R.; Khan, N.A.; Wirnitzer, K. Management of childhood obesity—Time to shift from generalized to personalized intervention strategies. Nutrients 2021, 13, 1200. [Google Scholar] [CrossRef]
- Umekar, S.; Joshi, A. Obesity and preventive intervention among children: A narrative review. Cureus 2024, 16, e54520. [Google Scholar] [CrossRef]
- Willeboordse, M.; Bartelink, N.H.M.; van Assema, P.; Kremers, S.P.J.; Savelberg, H.H.C.M.; Hahnraths, M.T.H.; Vonk, L.; Oosterhoff, M.; van Schayck, C.P.; Winkens, B.; et al. Battling the obesity epidemic with a school-based intervention: Long-term effects of a quasi-experimental study. PLoS ONE 2022, 17, e0272291. [Google Scholar] [CrossRef]
- Nally, S.; Carlin, A.; Blackburn, N.E.; Baird, J.S.; Salmon, J.; Murphy, M.H.; Gallagher, A.M. The effectiveness of school-based interventions on obesity-related behaviours in primary school children: A systematic review and meta-analysis of randomised controlled trials. Children 2021, 8, 489. [Google Scholar] [CrossRef]
- Bogataj, Š.; Trajković, N.; Cadenas-Sanchez, C.; Sember, V. Effects of school-based exercise and nutrition intervention on body composition and physical fitness in overweight adolescent girls. Nutrients 2021, 13, 238. [Google Scholar] [CrossRef]
- Jayasinghe, S.; Hills, A.P. Strategies to improve physical activity and nutrition Behaviours in children and adolescents: A review. Nutrients 2023, 15, 3370. [Google Scholar] [CrossRef]
- Sun, X.; Li, Y.; Cai, L.; Wang, Y. Effects of physical activity interventions on cognitive performance of overweight or obese children and adolescents: A systematic review and meta-analysis. Pediatr. Res. 2021, 89, 46–53. [Google Scholar] [CrossRef]
- Maciejewski, M.L. Quasi-experimental design. Biostat. Epidemiol. 2020, 4, 38–47. [Google Scholar] [CrossRef]
- Casadei, K.; Kiel, J. Anthropometric Measurement. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Schroeder, R.W.; Twumasi-Ankrah, P.; Baade, L.E.; Marshall, P.S. Reliable digit span: A systematic review and cross-validation study. Assessment 2012, 19, 21–30. [Google Scholar] [CrossRef]
- Watkins, M.W.; Smith, L.G. Long-term stability of the Wechsler Intelligence Scale for Children—Fourth Edition. Psychol. Assess. 2013, 25, 477. [Google Scholar] [CrossRef]
- Moran, L.; Yeates, K.O. Stroop color and word test, children’s version. In Encyclopedia of Clinical Neuropsychology; Springer: Cham, Switzerland, 2018; pp. 3323–3325. [Google Scholar]
- Strauss, G.P.; Allen, D.N.; Jorgensen, M.L.; Cramer, S.L. Test-retest reliability of standard and emotional stroop tasks: An investigation of color-word and picture-word versions. Assessment 2005, 12, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Espy, K.A.; Cwik, M.F. The development of a trial making test in young children: The TRAILS-P. Clin. Neuropsychol. 2004, 18, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Osuka, Y.; Kojima, N.; Sakurai, R.; Watanabe, Y.; Kim, H. Reliability and construct validity of a novel motor–cognitive dual-task test: A Stepping Trail Making Test. Geriatr. Gerontol. Int. 2020, 20, 291–296. [Google Scholar] [CrossRef]
- Smirni, D. The Raven’s Coloured Progressive Matrices in healthy children: A qualitative approach. Brain Sci. 2020, 10, 877. [Google Scholar] [CrossRef]
- Alhinai, S.S.A.; Al Kharusi, H.A.T.; Ibrahim, M.M. Meta-Analysis Reliability Of Raven’s Progressive Matrices Tests. Perdana Int. J. Acad. Res. 2019, 6, 51–68. [Google Scholar]
- Lammers, A.E.; Hislop, A.A.; Flynn, Y.; Haworth, S.G. The 6-minute walk test: Normal values for children of 4–11 years of age. Arch. Dis. Child. 2008, 93, 464–468. [Google Scholar] [CrossRef]
- Mylius, C.F.; Paap, D.; Takken, T. Reference value for the 6-minute walk test in children and adolescents: A systematic review. Expert Rev. Respir. Med. 2016, 10, 1335–1352. [Google Scholar] [CrossRef]
- Mayorga-Vega, D.; Merino-Marban, R.; Viciana, J. Criterion-related validity of sit-and-reach tests for estimating hamstring and lumbar extensibility: A meta-analysis. J. Sports Sci. Med. 2014, 13, 1–14. [Google Scholar]
- Castro-Piñero, J.; Chillón, P.; Ortega, F.B.; Montesinos, J.L.; Sjöström, M.; Ruiz, J.R. Criterion-related validity of sit-and-reach and modified sit-and-reach test for estimating hamstring flexibility in children and adolescents aged 6–17 years. Int. J. Sports Med. 2009, 30, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J. A chart to link child centiles of body mass index, weight and height. Eur. J. Clin. Nutr. 2002, 56, 1194–1199. [Google Scholar] [CrossRef] [PubMed]
- Marković-Jovanović, S.R.; Stolić, R.V.; Jovanović, A.N. The reliability of body mass index in the diagnosis of obesity and metabolic risk in children. J. Pediatr. Endocrinol. Metab. 2015, 28, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, E.I.D.S.; Sant’Ana, L.F.D.R.; Priore, S.E.; Franceschini, S.D.C.C. Waist circumference, waist/height ratio, and neck circumference as parameters of central obesity assessment in children. Rev. Paul. Pediatr. 2014, 32, 273–281. [Google Scholar]
- Barrios, P.; Martin-Biggers, J.; Quick, V.; Byrd-Bredbenner, C. Reliability and criterion validity of self-measured waist, hip, and neck circumferences. BMC Med. Res. Methodol. 2016, 16, 49. [Google Scholar] [CrossRef]
- Parmenter, K.; Wardle, J. Development of a general nutrition knowledge questionnaire for adults. Eur. J. Clin. Nutr. 1999, 53, 298–308. [Google Scholar] [CrossRef]
- Richardson, J.T. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Renke, M.B.; Marcinkowska, A.B.; Kujach, S.; Winklewski, P.J. A systematic review of the impact of physical exercise-induced increased resting cerebral blood flow on cognitive functions. Front. Aging Neurosci. 2022, 14, 803332. [Google Scholar] [CrossRef]
- Liang, J.; Wang, H.; Zeng, Y.; Qu, Y.; Liu, Q.; Zhao, F.; Duan, J.; Jiang, Y.; Li, S.; Ying, J.; et al. Physical exercise promotes brain remodeling by regulating epigenetics, neuroplasticity and neurotrophins. Rev. Neurosci. 2021, 32, 615–629. [Google Scholar] [CrossRef]
- Dighriri, I.M.; Alsubaie, A.M.; Hakami, F.M.; Hamithi, D.M.; Alshekh, M.M.; Khobrani, F.A.; Dalak, F.E.; Hakami, A.A.; Alsueaadi, E.H.; Alsaawi, L.S.; et al. Effects of omega-3 polyunsaturated fatty acids on brain functions: A systematic review. Cureus 2022, 14, e30091. [Google Scholar] [CrossRef]
- Ortega, F.B.; Mora-Gonzalez, J.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Migueles, J.H.; Solis-Urra, P.; Verdejo-Román, J.; Rodriguez-Ayllon, M.; Molina-Garcia, P.; Ruiz, J.R.; et al. Effects of an exercise program on brain health outcomes for children with overweight or obesity: The ActiveBrains randomized clinical trial. JAMA Netw. Open 2022, 5, e2227893. [Google Scholar] [CrossRef] [PubMed]
- Martí-Nicolovius, M. Effects of overweight and obesity on cognitive functions of children and adolescents. Rev. De Neurol. 2022, 75, 59–65. [Google Scholar]
- Mello, J.B.; Costa, R.R.; da Silva, F.F.; Martins, R.; Cristi-Montero, C. School ACTIVE, brain active: A meta-analysis and meta-regression on chronic school physical activity effects on cognitive performance in children and adolescents. Educ. Res. Rev. 2025, 46, 100658. [Google Scholar] [CrossRef]
- Castelli, D.M. Physical activity, fitness, and cognitive function in children and adolescents. In Sport and Fitness in Children and Adolescents-A Multidimensional View; IntechOpen: London, UK, 2022. [Google Scholar]
- Northey, J.M.; Raine, L.B.; Hillman, C.H. Are there sensitive periods for physical activity to influence the development of executive function in children? J. Sport Health Sci. 2025, 14, 101015. [Google Scholar] [CrossRef]
- Latino, F.; Cataldi, S.; Carvutto, R.; De Candia, M.; D’Elia, F.; Patti, A.; Bonavolontà, V.; Fischetti, F. The importance of lipidomic approach for mapping and exploring the molecular networks underlying physical exercise: A systematic review. Int. J. Mol. Sci. 2021, 22, 8734. [Google Scholar] [CrossRef]
- Morsanuto, S.; Peluso Cassese, F.; Tafuri, F.; Tafuri, D. Outdoor education, integrated soccer activities, and learning in children with autism spectrum disorder: A project aimed at achieving the sustainable development goals of the 2030 agenda. Sustainability 2023, 15, 13456. [Google Scholar] [CrossRef]
- Latino, F.; Fischetti, F.; Cataldi, S.; Monacis, D.; Colella, D. The impact of an 8-weeks at-home physical activity plan on academic achievement at the time of COVID-19 lock-down in Italian school. Sustainability 2021, 13, 5812. [Google Scholar] [CrossRef]
- Farì, G.; Di Paolo, S.; Ungaro, D.; Luperto, G.; Farì, E.; Latino, F. The impact of COVID-19 on sport and daily activities in an Italian cohort of football school children. Int. J. Athl. Ther. Train. 2021, 26, 274–278. [Google Scholar] [CrossRef]
- Lanigan, J. Prevention of overweight and obesity in early life. Proc. Nutr. Soc. 2018, 77, 247–256. [Google Scholar] [CrossRef]
- HEALTHY Study Group. A school-based intervention for diabetes risk reduction. N. Engl. J. Med. 2010, 363, 443–453. [Google Scholar] [CrossRef]
- Caballero, B.; Clay, T.; Davis, S.M.; Ethelbah, B.; Rock, B.H.; Lohman, T.; Norman, J.; Story, M.; Stone, E.J.; Stephenson, L.; et al. Pathways: A school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am. J. Clin. Nutr. 2003, 78, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Asigbee, F.M.; Whitney, S.D.; Peterson, C.E. The link between nutrition and physical activity in increasing academic achievement. J. Sch. Health 2018, 88, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Cataldi, S.; Latino, F.; Greco, G.; Fischetti, F. Multilateral training improves physical fitness and fatigue perception in cancer patients. J. Hum. Sport Exerc. 2019, 14, S910–S920. [Google Scholar] [CrossRef]
- Navidad, L.; Padial-Ruz, R.; Gonzalez, M.C. Nutrition, physical activity, and new technology programs on obesity prevention in primary education: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 10187. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-determination theory. In Encyclopedia of Quality of Life and Well-Being Research; Springer International Publishing: Cham, Switzerland, 2024; pp. 6229–6235. [Google Scholar]
- Pearce, Z.R.; Miller, S.E. Embodied cognition perspectives within early executive function development. Front. Cogn. 2025, 4, 1361748. [Google Scholar] [CrossRef]
- Mesch, A.; Engels, M.; Raghoebar, S.; Winkens, L.H.; Gulikers, J.; Wesselink, R.; Haveman-Nies, A. Determinants, behaviour change techniques and pedagogical approaches used in secondary school-based food and nutrition programmes: A qualitative study of the SWITCH project. BMC Public Health 2025, 25, 1131. [Google Scholar] [CrossRef]
- Mancin, S.; Cangelosi, G.; Sguanci, M.; Matteucci, S.; Morenghi, E.; Lopane, D.; Cattani, D.; Cosmai, S.; Vinciguerra, G.; Parozzi, M.; et al. Integrating Active Learning Methodologies into Clinical Nutrition Education for Nursing Students: A Quasi-Experimental Study. Nurs. Rep. 2025, 15, 77. [Google Scholar] [CrossRef]
- Shao, X.; Tan, L.H.; He, L. Physical activity and exercise alter cognitive abilities, and brain structure and activity in obese children. Front. Neurosci. 2022, 16, 1019129. [Google Scholar] [CrossRef]
| Variable | Experimental Group (n = 30) | Control Group (n = 30) | Total (N = 60) |
|---|---|---|---|
| Mean age (years) | 12.5 (±0.3) | 12.4 (±0.4) | 12.5 (±0.3) |
| Gender (Female/Male) | 15/15 | 14/16 | 29/31 |
| Mean BMI (kg/m2) | 23.4 (±2.8) | 23.1 (±2.6) | 23.3 (±2.7) |
| Overweight percentage (%) | 40% | 37% | 38.5% |
| Obesity percentage (%) | 30% | 27% | 28.5% |
| Students with Law 104/92 certification | 1 | 2 | 3 |
| Regular school attendance (%) | 100% | 100% | 100% |
| Model Domain | χ2 (df) | χ2/df | CFI | TLI | RMSEA (90% CI) | SRMR | KMO | Bartlett’s Test (p) |
|---|---|---|---|---|---|---|---|---|
| Cognitive Function | 52.78 (28) | 1.88 | 0.94 | 0.92 | 0.065 [0.043–0.082] | 0.048 | 0.79 | <0.001 |
| Physical and Anthropometric | 24.66 (14) | 1.76 | 0.96 | 0.94 | 0.059 [0.034–0.088] | 0.041 | 0.75 | <0.001 |
| Nutritional Knowledge | 3.21 (2) | 1.60 | 0.99 | 0.98 | 0.042 [0.000–0.112] | 0.022 | 0.84 | <0.001 |
| Overall 3-Factor Model | 84.65 (45) | 1.88 | 0.95 | 0.93 | 0.064 [0.048–0.078] | 0.051 | 0.81 | <0.001 |
| Variable | Group | Pre-Test M | Pre-Test SD | Post-Test M | Post-Test SD | Δ (Post − Pre) M |
|---|---|---|---|---|---|---|
| Digit Span Forward | Experimental | 5.4 | 0.7 | 6.2 | 0.7 | +0.8 |
| Control | 5.3 | 0.6 | 5.2 | 0.6 | −0.1 | |
| Digit Span Backward | Experimental | 4.1 | 0.7 | 4.75 | 0.7 | +0.65 |
| Control | 4.0 | 0.65 | 3.95 | 0.65 | −0.05 | |
| Stroop Test (s) | Experimental | 55.4 | 5.8 | 49.2 | 5.5 | −6.2 |
| Control | 54.9 | 6.0 | 54.8 | 6.1 | −0.1 | |
| Trail Making Test B (s) | Experimental | 98.0 | 10.2 | 89.5 | 9.8 | −8.5 |
| Control | 97.2 | 9.9 | 96.7 | 9.7 | −0.5 | |
| 6-Minute Walk Test (m) | Experimental | 590.0 | 35.0 | 632.4 | 34.8 | +42.4 |
| Control | 588.5 | 33.5 | 598.7 | 32.8 | +10.2 | |
| Sit and Reach Test (cm) | Experimental | 18.5 | 3.4 | 21.6 | 3.3 | +3.1 |
| Control | 18.2 | 3.6 | 18.9 | 3.5 | +0.7 | |
| Nutrition Knowledge Score | Experimental | 14.8 | 1.7 | 17.4 | 1.6 | +2.6 |
| Control | 14.7 | 1.8 | 14.6 | 1.9 | −0.1 | |
| BMI (kg/m2) | Experimental | 21.1 | 2.2 | 20.3 | 2.0 | −0.8 |
| Control | 21.2 | 2.3 | 21.2 | 2.3 | 0.0 | |
| Weight (kg) | Experimental | 49.4 | 5.15 | 47.5 | 4.68 | −1.9 |
| Control | 49.6 | 5.38 | 49.6 | 5.38 | 0.0 | |
| Waist Circumference (cm) | Experimental | 79.3 | 4.5 | 74.8 | 4.3 | −4.5 |
| Control | 78.7 | 4.8 | 78.2 | 4.7 | −0.5 |
| Variable | F(1,57) | p-Value | Partial η2 |
|---|---|---|---|
| Digit Span Forward | 14.86 | <0.001 | 0.21 |
| Digit Span Backward | 12.45 | 0.001 | 0.18 |
| Stroop Test (s) | 16.92 | <0.001 | 0.23 |
| Trail Making Test B (s) | 11.08 | 0.001 | 0.16 |
| 6-Minute Walk Test (m) | 13.74 | <0.001 | 0.19 |
| Sit and Reach Test (cm) | 10.33 | 0.002 | 0.15 |
| Nutrition Knowledge Score | 18.60 | <0.001 | 0.25 |
| BMI (kg/m2) | 6.40 | 0.05 | 0.10 |
| Waist Circumference (cm) | 8.30 | 0.01 | 0.12 |
| Weight (kg) | 7.10 | 0.01 | 0.11 |
| Variable 1 | Variable 2 | Pearson’s r | p-Value |
|---|---|---|---|
| Digit Span Forward | 6-Minute Walk Test | 0.52 | 0.003 |
| Digit Span Forward | Nutrition Knowledge Score | 0.49 | 0.005 |
| Digit Span Backward | Sit and Reach Test | 0.46 | 0.008 |
| Digit Span Backward | Nutrition Knowledge Score | 0.50 | 0.004 |
| Trail Making Test B | 6-Minute Walk Test | −0.55 | 0.002 |
| Trail Making Test B | Digit Span Backward | −0.48 | 0.006 |
| Nutrition Knowledge | Trail Making Test B | −0.51 | 0.004 |
| BMI (kg/m2) | 6-Minute Walk Test | −0.48 | 0.006 |
| BMI (kg/m2) | Sit and Reach Test | −0.41 | 0.015 |
| BMI (kg/m2) | Nutrition Knowledge Score | −0.37 | 0.028 |
| Waist Circumference | 6-Minute Walk Test | −0.53 | 0.003 |
| Waist Circumference | Sit and Reach Test | −0.45 | 0.009 |
| Waist Circumference | Nutrition Knowledge Score | −0.39 | 0.022 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tafuri, M.G.; Tafuri, D.; Latino, F. Relationship Between Obesity and Impairment of Cognitive Functions: An Investigation into the Integrated Role of Nutritional Education and Physical Activity in Lower Secondary School. Nutrients 2025, 17, 2531. https://doi.org/10.3390/nu17152531
Tafuri MG, Tafuri D, Latino F. Relationship Between Obesity and Impairment of Cognitive Functions: An Investigation into the Integrated Role of Nutritional Education and Physical Activity in Lower Secondary School. Nutrients. 2025; 17(15):2531. https://doi.org/10.3390/nu17152531
Chicago/Turabian StyleTafuri, Maria Giovanna, Domenico Tafuri, and Francesca Latino. 2025. "Relationship Between Obesity and Impairment of Cognitive Functions: An Investigation into the Integrated Role of Nutritional Education and Physical Activity in Lower Secondary School" Nutrients 17, no. 15: 2531. https://doi.org/10.3390/nu17152531
APA StyleTafuri, M. G., Tafuri, D., & Latino, F. (2025). Relationship Between Obesity and Impairment of Cognitive Functions: An Investigation into the Integrated Role of Nutritional Education and Physical Activity in Lower Secondary School. Nutrients, 17(15), 2531. https://doi.org/10.3390/nu17152531







