Personalized Dietary Advice to Increase Protein Intake in Older Adults Does Not Affect the Gut Microbiota, Appetite or Central Processing of Food Stimuli in Community-Dwelling Older Adults: A Six-Month Randomized Controlled Trial
Abstract
1. Introduction
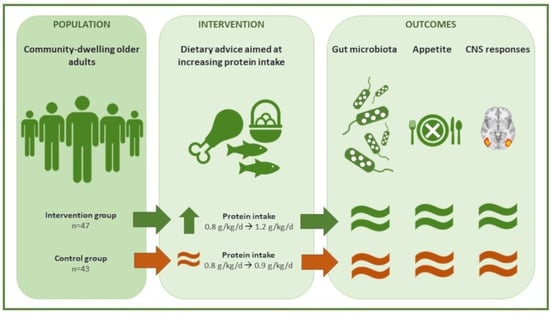
2. Materials and Methods
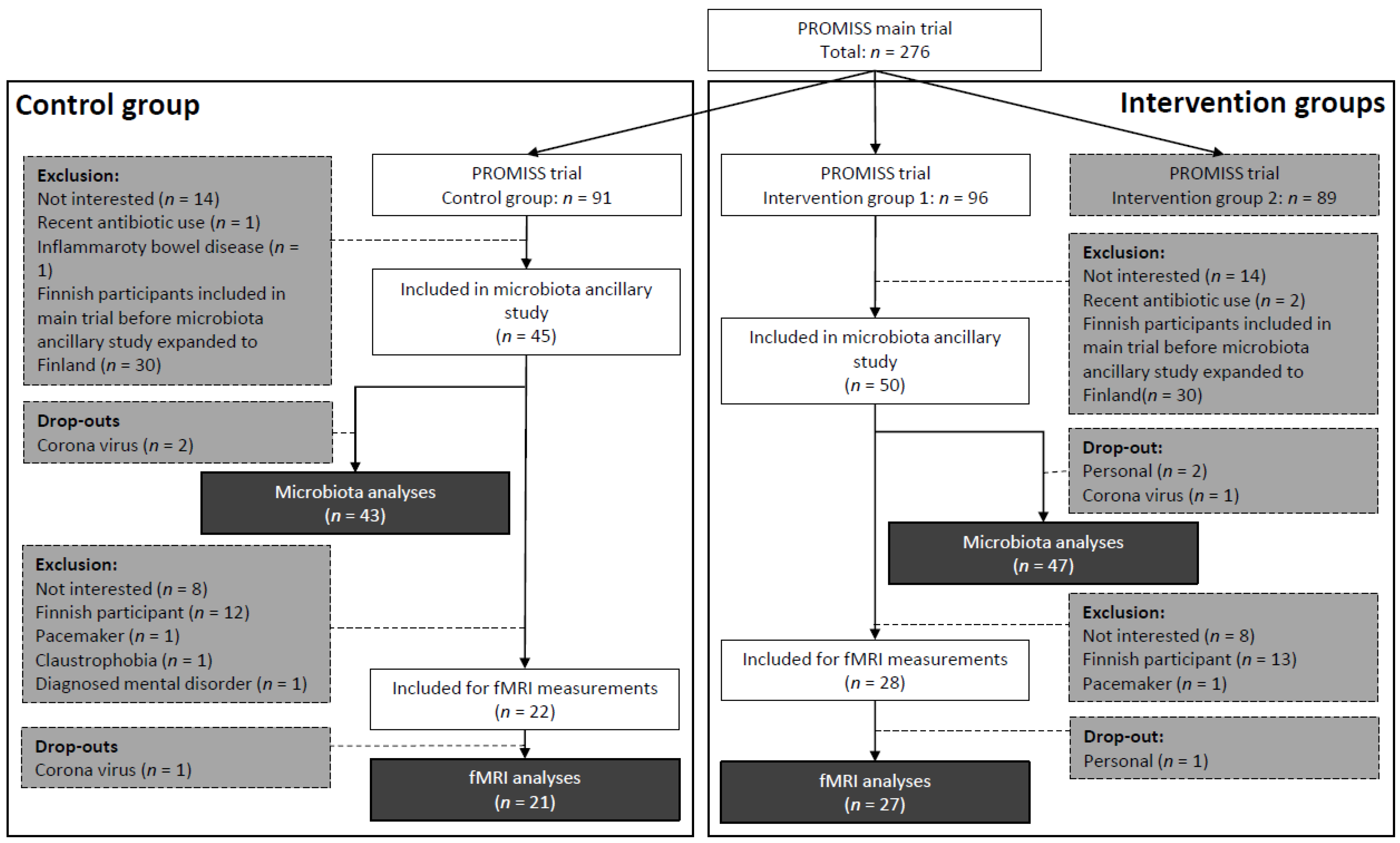
2.1. Participants
2.2. Intervention
2.3. Self-Reported Appetite
2.4. Biosampling and 16S rRNA Sequencing
2.5. MRI Scanning
2.6. Functional MRI Experimental Design
2.7. Statistics
3. Results
3.1. Participants
3.2. Dietary Intake
3.3. Appetite Assessments
3.4. fMRI Assessments
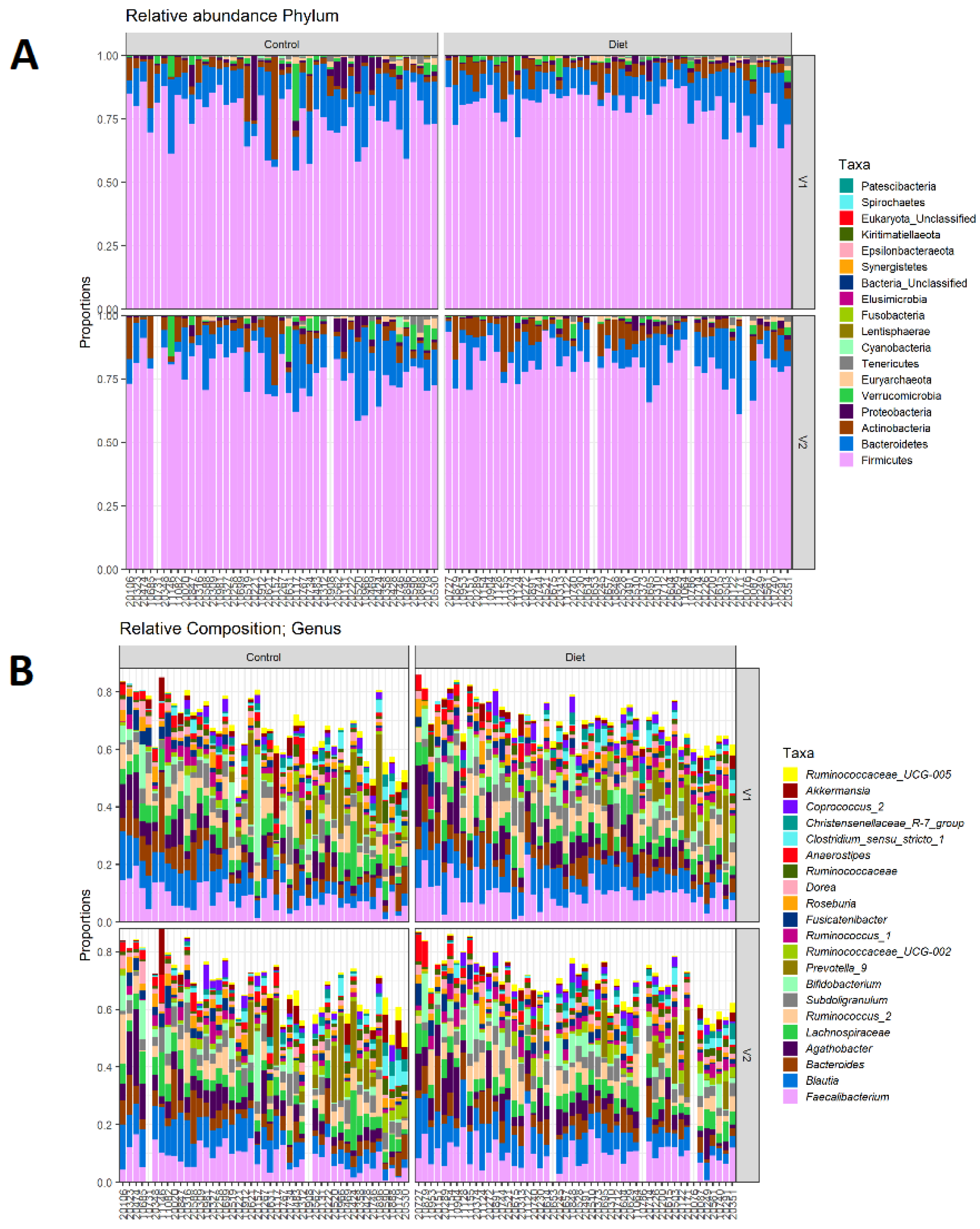
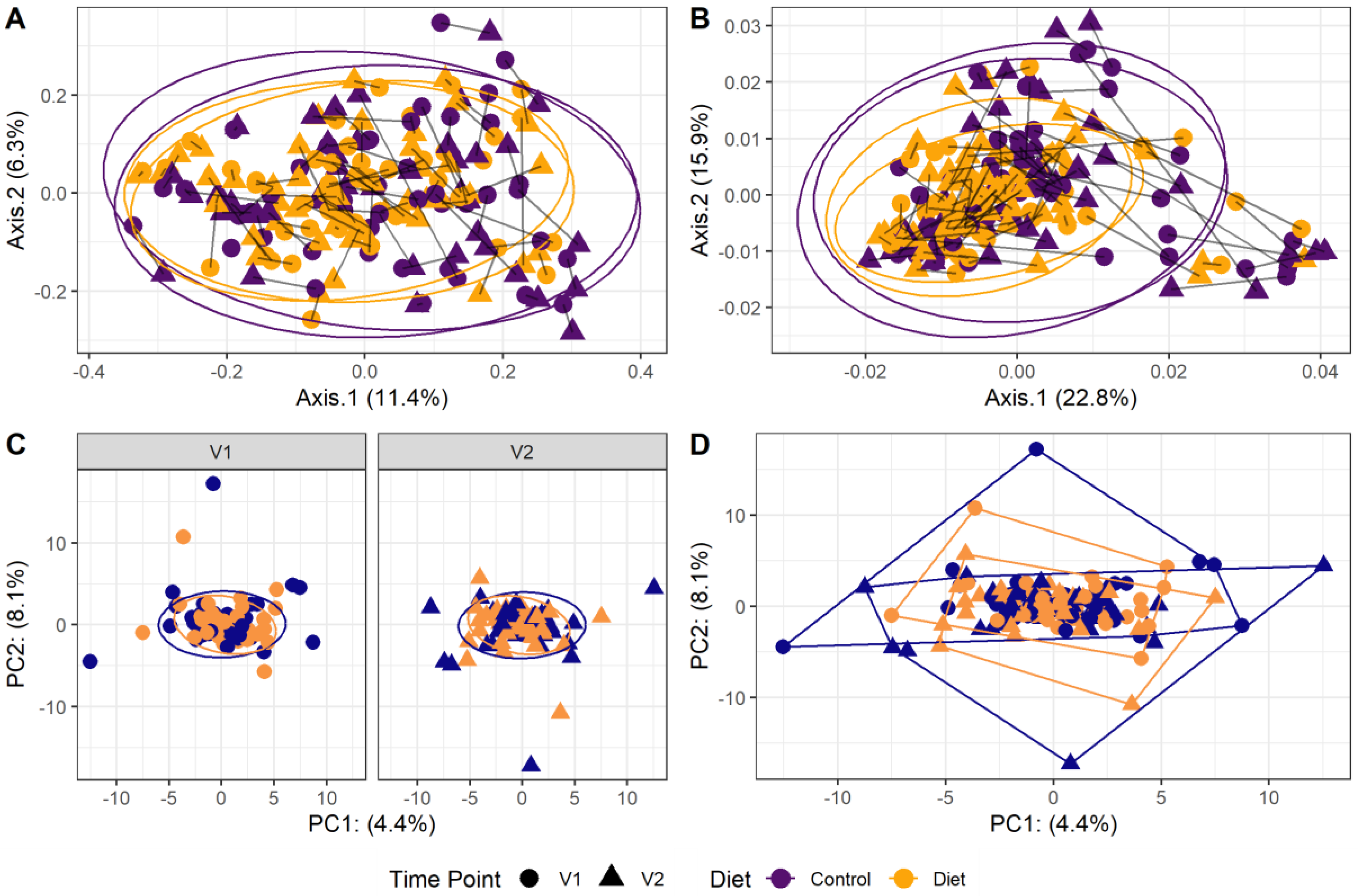
3.5. Gut Microbiota
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eide, H.K.; Benth, J.Š; Sortland, K.; Halvorsen, K.; Almendingen, K. Prevalence of nutritional risk in the non-demented hospitalised elderly: A cross-sectional study from Norway using stratified sampling. J. Nutr. Sci. 2015, 4, e18. [Google Scholar] [CrossRef] [PubMed]
- Almohaisen, N.; Gittins, M.; Todd, C.; Sremanakova, J.; Sowerbutts, A.M.; Aldossari, A.; Almutairi, A.; Jones, D.; Burden, S. Prevalence of Undernutrition, Frailty and Sarcopenia in Community-Dwelling People Aged 50 Years and Above: Systematic Review and Meta-Analysis. Nutrients 2022, 14, 1537. [Google Scholar] [CrossRef] [PubMed]
- Deutz, N.E.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.; Krznariç, Z.; Nair, K.S.; et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Park, Y. Amount of Protein Required to Improve Muscle Mass in Older Adults. Nutrients 2020, 12, 1700. [Google Scholar] [CrossRef]
- EFSA. Scientific Opinion on Dietary Reference Values for protein. EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). EFSA J. 2012, 10, 2257. [Google Scholar] [CrossRef]
- Ouyang, Y.; Huang, F.; Zhang, X.; Li, L.; Zhang, B.; Wang, Z.; Wang, H. Association of Dietary Protein Intake with Muscle Mass in Elderly Chinese: A Cross-Sectional Study. Nutrients 2022, 14, 5130. [Google Scholar] [CrossRef]
- Morgan, P.T.; Harris, D.O.; Marshall, R.N.; Quinlan, J.I.; Edwards, S.J.; Allen, S.L.; Breen, L. Protein Source and Quality for Skeletal Muscle Anabolism in Young and Older Adults: A Systematic Review and Meta-Analysis. J. Nutr. 2021, 151, 1901–1920. [Google Scholar] [CrossRef]
- Lonnie, M.; Hooker, E.; Brunstrom, J.M.; Corfe, B.M.; Green, M.A.; Watson, A.W.; Williams, E.A.; Stevenson, E.J.; Penson, S.; Johnstone, A.M. Protein for Life: Review of Optimal Protein Intake, Sustainable Dietary Sources and the Effect on Appetite in Ageing Adults. Nutrients 2018, 10, 360. [Google Scholar] [CrossRef]
- Paddon-Jones, D.; Westman, E.; Mattes, R.D.; Wolfe, R.R.; Astrup, A.; Westerterp-Plantenga, M. Protein, weight management, and satiety. Am. J. Clin. Nutr. 2008, 87, 1558S–1561S. [Google Scholar] [CrossRef]
- Lejeune, M.P.G.M.; Westerterp, K.R.; Adam, T.C.M.; Luscombe-Marsh, N.; Westerterp-Plantenga, M.S. Ghrelin and glucagon-like peptide 1 concentrations, 24-h satiety, and energy and substrate metabolism during a high-protein diet and measured in a respiration chamber. Am. J. Clin. Nutr. 2006, 83, 89–94. [Google Scholar] [CrossRef]
- Soenen, S.; Giezenaar, C.; Hutchison, A.T.; Horowitz, M.; Chapman, I.; Luscombe-Marsh, N. Effects of intraduodenal protein on appetite, energy intake, and antropyloroduodenal motility in healthy older compared with young men in a randomized trial. Am. J. Clin. Nutr. 2014, 100, 1108–1115. [Google Scholar] [CrossRef]
- van der Pols-Vijlbrief, R.; Wijnhoven, H.A.; Schaap, L.A.; Terwee, C.B.; Visser, M. Determinants of protein-energy malnutrition in community-dwelling older adults: A systematic review of observational studies. Ageing Res. Rev. 2014, 18, 112–131. [Google Scholar] [CrossRef]
- Jahan-Mihan, A.; Luhovyy, B.L.; El Khoury, D.; Anderson, G.H. Dietary Proteins as Determinants of Metabolic and Physiologic Functions of the Gastrointestinal Tract. Nutrients 2011, 3, 574–603. [Google Scholar] [CrossRef] [PubMed]
- Drummen, M.; Dorenbos, E.; Vreugdenhil, A.C.E.; Stratton, G.; Raben, A.; Westerterp-Plantenga, M.S.; Adam, T.C. Associations of Brain Reactivity to Food Cues with Weight Loss, Protein Intake and Dietary Restraint during the PREVIEW Intervention. Nutrients 2018, 10, 1771. [Google Scholar] [CrossRef] [PubMed]
- Leidy, H.J.; Ortinau, L.C.; Douglas, S.M.; Hoertel, H.A. Beneficial effects of a higher-protein breakfast on the appetitive, hormonal, and neural signals controlling energy intake regulation in overweight/obese, “breakfast-skipping,” late-adolescent girls. Am. J. Clin. Nutr. 2013, 97, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Griffioen-Roose, S.; Smeets, P.A.; van den Heuvel, E.; Boesveldt, S.; Finlayson, G.; De Graaf, C. Human protein status modulates brain reward responses to food cues. Am. J. Clin. Nutr. 2014, 100, 113–122. [Google Scholar] [CrossRef]
- Russell, W.R.; Gratz, S.W.; Duncan, S.H.; Holtrop, G.; Ince, J.; Scobbie, L.; Duncan, G.; Johnstone, A.M.; Lobley, G.E.; Wallace, R.J.; et al. High-protein, reduced-carbohydrate weight-loss diets promote metabolite profiles likely to be detrimental to colonic health. Am. J. Clin. Nutr. 2011, 93, 1062–1072. [Google Scholar] [CrossRef]
- Fluitman, K.S.; De Clercq, N.C.; Keijser, B.J.; Visser, M.; Nieuwdorp, M.; Ijzerman, R.G. The intestinal microbiota, energy balance, and malnutrition: Emphasis on the role of short-chain fatty acids. Expert Rev. Endocrinol. Metab. 2017, 12, 215–226. [Google Scholar] [CrossRef]
- Strasser, B.; Wolters, M.; Weyh, C.; Krüger, K.; Ticinesi, A. The Effects of Lifestyle and Diet on Gut Microbiota Composition, Inflammation and Muscle Performance in Our Aging Society. Nutrients 2021, 13, 2045. [Google Scholar] [CrossRef]
- Reinders, I.; Wijnhoven, H.A.H.; Jyväkorpi, S.K.; Suominen, M.H.; Niskanen, R.; Bosmans, J.E.; Brouwer, I.A.; Fluitman, K.S.; Klein, M.C.A.; Kuijper, L.D.; et al. Effectiveness and cost-effectiveness of personalised dietary advice aiming at increasing protein intake on physical functioning in community-dwelling older adults with lower habitual protein intake: Rationale and design of the PROMISS randomised controlled trial. BMJ Open 2020, 10, e040637. [Google Scholar] [CrossRef]
- Reinders, I.; Visser, M.; Jyväkorpi, S.K.; Niskanen, R.T.; Bosmans, J.E.; Ângela, J.B.; Ingeborg, A.B.; Lothar, D.K.; Margreet, R.O.; Kaisu, H.P.; et al. The cost effectiveness of personalized dietary advice to increase protein intake in older adults with lower habitual protein intake: A randomized controlled trial. Eur. J. Nutrition 2022, 61, 505–520. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Grasso, A.C.; Olthof, M.R.; Reinders, I.; Wijnhoven, H.A.H.; Visser, M.; Brouwer, I.A. Effect of personalized dietary advice to increase protein intake on food consumption and the environmental impact of the diet in community-dwelling older adults: Results from the PROMISS trial. Eur. J. Nutrition 2022, 61, 4015–4026. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.-M.G.; Thomas, D.R.; Rubenstein, L.; Chibnall, J.T.; Anderson, S.; Baxi, A.; Diebold, M.R.; Morley, J.E. Appetite assessment: Simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am. J. Clin. Nutr. 2005, 82, 1074–1081. [Google Scholar] [CrossRef]
- Salonen, A.; Nikkilä, J.; Jalanka-Tuovinen, J.; Immonen, O.; Rajilić-Stojanović, M.; Kekkonen, R.A.; Palva, A.; de Vos, W.M. Comparative analysis of fecal DNA extraction methods with phylogenetic microarray: Effective recovery of bacterial and archaeal DNA using mechanical cell lysis. J. Microbiol. Methods 2010, 81, 127–134. [Google Scholar] [CrossRef]
- Kozich, J.J.; Westcott, S.L.; Baxter, N.T.; Highlander, S.K.; Schloss, P.D. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl. Environ. Microbiol. 2013, 79, 5112–5120. [Google Scholar] [CrossRef]
- Edgar, R.C. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 2010, 26, 2460–2461. [Google Scholar] [CrossRef]
- Edgar, R.C. UNOISE2: Improved error-correction for Illumina 16S and ITS amplicon sequencing. BioRxiv. 2016, 081257. [Google Scholar] [CrossRef]
- Wang, Q.; Garrity, G.M.; Tiedje, J.M.; Cole, J.R. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl. Env. Microbiol. 2007, 73, 5261–5267. [Google Scholar] [CrossRef]
- Quast, C.; Pruesse, E.; Yilmaz, P.; Gerken, J.; Schweer, T.; Yarza, P.; Peplies, J.; Glöckner, F.O. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 2013, 41, D590–D596. [Google Scholar] [CrossRef]
- van Bloemendaal, L.; IJzerman, R.G.; Kulve, J.S.T.; Barkhof, F.; Konrad, R.J.; Drent, M.L.; Veltman, D.J.; Diamant, M. GLP-1 receptor activation modulates appetite- and reward-related brain areas in humans. Diabetes 2014, 63, 4186–4196. [Google Scholar] [CrossRef] [PubMed]
- Esteban, O.; Markiewicz, C.J.; Blair, R.W.; Moodie, C.A.; Isik, A.I.; Erramuzpe, A.; Kent, J.D.; Goncalves, M.; DuPre, E.; Snyder, M.; et al. fMRIPrep: A robust preprocessing pipeline for functional MRI. Nat. Methods 2018, 16, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Esteban, O.; Ciric, R.; Finc, K.; Blair, R.W.; Markiewicz, C.J.; Moodie, C.A.; Kent, J.D.; Goncalves, M.; DuPre, E.; Gomez, D.E.P.; et al. Analysis of task-based functional MRI data preprocessed with fMRIPrep. Nat. Protoc. 2020, 15, 2186–2202. [Google Scholar] [CrossRef] [PubMed]
- Fonov, V.; Evans, A.; McKinstry, R.; Almli, C.; Collins, D. Unbiased nonlinear average age-appropriate brain templates from birth to adulthood. Neuroimage 2009, 47, S102. [Google Scholar] [CrossRef]
- Jenkinson, M.; Bannister, P.; Brady, M.; Smith, S. Improved Optimization for the Robust and Accurate Linear Registration and Motion Correction of Brain Images. Neuroimage 2002, 17, 825–841. [Google Scholar] [CrossRef]
- Cox, R.W.; Hyde, J.S. Software tools for analysis and visualization of fMRI data. NMR Biomed. 1997, 10, 171–178. [Google Scholar] [CrossRef]
- Jenkinson, M.; Smith, S. A global optimisation method for robust affine registration of brain images. Med. Image Anal. 2001, 5, 143–156. [Google Scholar] [CrossRef]
- Pruim, R.H.R.; Mennes, M.; van Rooij, D.; Llera, A.; Buitelaar, J.K.; Beckmann, C.F. ICA-AROMA: A robust ICA-based strategy for removing motion artifacts from fMRI data. NeuroImage 2015, 112, 267–277. [Google Scholar] [CrossRef]
- van Bloemendaal, L.; Veltman, D.J.; Kulve, J.S.T.; Groot, P.F.; Ruhe, H.G.; Barkhof, F.; Diamant, M.; Ijzerman, R.G. Brain reward-system activation in response to anticipation and consumption of palatable food is altered by glucagon-like peptide-1 receptor activation in humans. Diabetes Obes. Metab. 2015, 17, 878–886. [Google Scholar] [CrossRef]
- Stice, E.; Spoor, S.; Bohon, C.; Small, D.M. Relation between obesity and blunted striatal response to food is moderated by TaqIA A1 allele. Science 2008, 322, 449–452. [Google Scholar] [CrossRef]
- Moreno-Pérez, D.; Bressa, C.; Bailén, M.; Hamed-Bousdar, S.; Naclerio, F.; Carmona, M.; Pérez, M.; González-Soltero, R.; Montalvo-Lominchar, M.G.; Carabaña, C.; et al. Effect of a Protein Supplement on the Gut Microbiota of Endurance Athletes: A Randomized, Controlled, Double-Blind Pilot Study. Nutrients 2018, 10, 337. [Google Scholar] [CrossRef]
- Schaafsma, A.; Mallee, L.; Belt, M.V.D.; Floris, E.; Kortman, G.; Veldman, J.; Ende, D.V.D.; Kardinaal, A. The Effect of A Whey-Protein and Galacto-Oligosaccharides Based Product on Parameters of Sleep Quality, Stress, and Gut Microbiota in Apparently Healthy Adults with Moderate Sleep Disturbances: A Randomized Controlled Cross-Over Study. Nutrients 2021, 13, 2204. [Google Scholar] [CrossRef] [PubMed]
- Doornweerd, S.; De Geus, E.J.; Barkhof, F.; Van Bloemendaal, L.; Boomsma, D.I.; Van Dongen, J.; Drent, M.L.; Willemsen, G.; Veltman, D.J.; Ijzerman, R.G. Brain reward responses to food stimuli among female monozygotic twins discordant for BMI. Brain Imaging Behav. 2017, 12, 718–727. [Google Scholar] [CrossRef] [PubMed]
- van Ruiten, C.C.; Veltman, D.J.; Wijdeveld, M.; Kulve, J.S.T.; Kramer, M.H.H.; Nieuwdorp, M.; IJzerman, R.G. Combination therapy with exenatide decreases the dapagliflozin-induced changes in brain responses to anticipation and consumption of palatable food in patients with type 2 diabetes: A randomized controlled trial. Diabetes Obes. Metabolism. 2022, 24, 1588–1597. [Google Scholar] [CrossRef] [PubMed]
- Kulve, J.S.T.; Veltman, D.J.; van Bloemendaal, L.; Barkhof, F.; Drent, M.L.; Diamant, M.; IJzerman, R.G. Liraglutide Reduces CNS Activation in Response to Visual Food Cues Only After Short-term Treatment in Patients With Type 2 Diabetes. Diabetes Care. 2016, 39, 214–221. [Google Scholar] [CrossRef]
- Smith, S.M.; Jenkinson, M.; Woolrich, M.W.; Beckmann, C.F.; Behrens, T.E.; Johansen-Berg, H.; Bannister, P.R.; De Luca, M.; Drobnjak, I.; Flitney, D.E.; et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage 2004, 23, S208–S219. [Google Scholar] [CrossRef]
- Born, J.M.; Lemmens, S.G.T.; Rutters, F.; Nieuwenhuizen, A.; Formisano, E.; Goebel, R.; Westerterp-Plantenga, M.S. Acute stress and food-related reward activation in the brain during food choice during eating in the absence of hunger. Int. J. Obes. 2009, 34, 172–181. [Google Scholar] [CrossRef]
- Farr, O.M.; Li, C.-S.R.; Mantzoros, C.S. Central nervous system regulation of eating: Insights from human brain imaging. Metabolism 2016, 65, 699–713. [Google Scholar] [CrossRef]
- Wright, H.; Li, X.; Fallon, N.B.; Crookall, R.; Giesbrecht, T.; Thomas, A.; Halford, J.C.; Harrold, J.; Stancak, A. Differential effects of hunger and satiety on insular cortex and hypothalamic functional connectivity. Eur. J. Neurosci. 2016, 43, 1181–1189. [Google Scholar] [CrossRef]
- Pursey, K.M.; Stanwell, P.; Callister, R.J.; Brain, K.; Collins, C.E.; Burrows, T.L. Neural Responses to Visual Food Cues According to Weight Status: A Systematic Review of Functional Magnetic Resonance Imaging Studies. Front. Nutr. 2014, 1, 7. [Google Scholar] [CrossRef]
- Team, R.C. R: A Language and Environment for Statistical Computing. Vienna, Austria. 2018. Available online: http://www.R-project.org/ (accessed on 28 November 2022).
- McMurdie, P.J.; Holmes, S. phyloseq: An R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE 2013, 8, e61217. [Google Scholar] [CrossRef] [PubMed]
- Oksanen, J.; Blanchet, F.G.; Kindt, R.; Legendre, P.; O’hara, R.B.; Simpson, G.L.; Solymos, P.; Stevens, M.H.H.; Wagner, H. Vegan: Community Ecology Package. Package. R package version. 2018, Volume 2, pp. 5–7. Available online: https://CRAN.R-project.org/package=vegan (accessed on 28 November 2022).
- Wickham, H. Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, G.E.; Schadt, E.E. variancePartition: Interpreting drivers of variation in complex gene expression studies. BMC Bioinform. 2016, 17, 483. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, G.E.; Roussos, P. Dream: Powerful differential expression analysis for repeated measures designs. Bioinformatics 2021, 37, 192–201. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Salem, V.; Dhillo, W.S. IMAGING IN ENDOCRINOLOGY: The use of functional MRI to study the endocrinology of appetite. Eur. J. Endocrinol. 2015, 173, R59–R68. [Google Scholar] [CrossRef]
- Brooks, S.J.; Cedernaes, J.; Schiöth, H.B. Increased Prefrontal and Parahippocampal Activation with Reduced Dorsolateral Prefrontal and Insular Cortex Activation to Food Images in Obesity: A Meta-Analysis of fMRI Studies. PLoS ONE 2013, 8, e60393. [Google Scholar] [CrossRef]
- Boswell, R.G.; Kober, H. Food cue reactivity and craving predict eating and weight gain: A meta-analytic review. Obes. Rev. 2016, 17, 159–177. [Google Scholar] [CrossRef]
- Giezenaar, C.; Trahair, L.G.; Rigda, R.; Hutchison, A.T.; Feinle-Bisset, C.; Luscombe-Marsh, N.D.; Hausken, T.; Jones, K.L.; Horowitz, M.; Chapman, I.; et al. Lesser suppression of energy intake by orally ingested whey protein in healthy older men compared with young controls. Am. J. Physiol. Integr. Comp. Physiol. 2015, 309, R845–R854. [Google Scholar] [CrossRef]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef]
- Ma, N.; Tian, Y.; Wu, Y.; Ma, X. Contributions of the Interaction Between Dietary Protein and Gut Microbiota to Intestinal Health. Curr. Protein Pept. Sci. 2017, 18, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-Based Recommendations for Optimal Dietary Protein Intake in Older People: A Position Paper From the PROT-AGE Study Group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Ben-Harchache, S.; Roche, H.M.; Corish, C.A.; Horner, K.M. The Impact of Protein Supplementation on Appetite and Energy Intake in Healthy Older Adults: A Systematic Review with Meta-Analysis. Adv. Nutr. Int. Rev. J. 2021, 12, 490–502. [Google Scholar] [CrossRef] [PubMed]
- Rogers, H.L.; Fernandez, S.N.; Hernando, S.P.; Sanchez, A.; Martos, C.; Moreno, M.; Grandes, G. “My Patients Asked Me If I Owned a Fruit Stand in Town or Something.” Barriers and Facilitators of Personalized Dietary Advice Implemented in a Primary Care Setting. J. Pers. Medicine 2021, 11, 747. [Google Scholar] [CrossRef] [PubMed]

| Microbiota Sample | fMRI Subsample | |||||
|---|---|---|---|---|---|---|
| Diet Group (n = 47) | Control Group (n = 43) | p-Value | Diet Group (n = 27) | Control Group (n = 21) | p-Value | |
| Demographics | ||||||
| Age (years) | 74.6 ± 4.8 | 74.1 ± 4.7 | 0.572 | 73 (70–80) | 72 (71–75) | 0.445 |
| Sex (male) | 28 (59.6) | 19 (44.2) | 0.205 | 18 (66.7) | 12 (57.1) | 0.558 |
| BMI (kg/m2) | 26.1 ± 2.9 | 26.8 ± 2.9 | 0.227 | 26.6 ± 2.7 | 27.1 ± 2.9 | 0.604 |
| MMSE | 29 (27–30) | 29 (27–30) | 0.573 | 29 (27–29) | 29 (27–30) | 0.734 |
| Education | 0.110 | 0.565 | ||||
| Low | 3 (6.4) | 0 (0.0) | 2 (7.4) | 0 (0.0) | ||
| Middle | 8 (17.0) | 13 (30.2) | 5 (18.5) | 6 (28.6) | ||
| High | 36 (76.6) | 30 (69.8) | 20 (74.1) | 15 (71.4) | ||
| Study site (Amsterdam) | 35 (74.5) | 33 (76.7) | 1.000 | |||
| Appetite | ||||||
| SNAQ appetite score | 14.9 ± 1.7 | 15.0 ± 2.1 | 0.965 | 15.2 ± 1.4 | 15.2 ± 2.4 | 0.978 |
| VAS appetite scores | 4.7 (3.3–5.8) | 5.3 (3.3–6.4) | 0.560 | |||
| Food intake | ||||||
| Energy intake (kcal/day) | 1701.9 ± 427.4 | 1611.0 ± 301.8 | 0.244 | 1740.4 ± 464.5 | 1690.2 ± 311.1 | 0.657 |
| Protein intake (g/kg aBW/day) | 0.8 ± 0.2 | 0.8 ± 0.1 | 0.689 | 0.8 ± 0.2 | 0.8 ± 0.1 | 0.777 |
| Protein intake (g/day) | 62.9 ± 14.0 | 60.9 ± 10.4 | 0.457 | 64.5 ± 14.6 | 62.0 ± 11.2 | 0.526 |
| Carbohydrate intake (g/day) | 181.4 ± 56.4 | 170.9 ± 47.6 | 0.347 | 182.5 ± 63.2 | 182.2 ± 49.3 | 0.986 |
| Fat intake (g/day) | 67.3 ± 20.4 | 66.1 ± 18.3 | 0.771 | 69.2 ± 21.9 | 69.8 ± 20.1 | 0.929 |
| Microbiota Subsample | Diet Group (n = 47) | Control Group (n = 43) | Between-Group Differences | |||
| 3 Months | 6 Months | 3 Months | 6 Months | B (95%-CI) | p-Value | |
| Energy intake (kcal/day) | 1873.9 ± 454.2 | 1836.1 ± 382.9 | 1679.2 ± 429.8 | 1699.2 ± 341.6 | 104.0 (0.4–207.5) | 0.0008 * |
| Protein intake (g/kg aBW/day | 1.3 ± 0.3 | 1.2 ± 0.2 | 0.9 ± 0.2 | 0.9 ± 0.2 | 0.4 (0.3–0.4) | <0.0001 * |
| Protein intake (g/day) | 96.2 ± 26.7 | 94.2 ± 22.2 | 64.1 ± 15.0 | 66.8 ± 15.2 | 27.1 (21.2–33.0) | <0.0001 * |
| Carbohydrate intake (g/day) | 187.7 ± 51.0 | 185.0 ± 48.9 | 177.0 ± 54.6 | 174.2 ± 47.7 | 4.2 (−7.9–16.3) | 0.0367 * |
| Fat intake (g/day) | 72.4 ± 24.4 | 69.9 ± 23.0 | 68.6 ± 24.9 | 71.5 ± 18.3 | 0.2 (−6.3–6.6) | 0.6514 |
| fMRI Subsample | Diet Group (n = 27) | Control Group (n = 21) | Between-Group Differences | |||
| 3 Months | 6 Months | 3 Months | 6 Months | B (95%-CI) | p-Value | |
| Energy intake (kcal/day) | 1893.3 ± 484.3 | 1847.4 ± 402.8 | 1815.0 ± 470.2 | 1764.1 ± 310.7 | 70.4 (−86.3–227.1) | 0.1897 |
| Protein intake (g/kg aBW/day | 1.3 ± 0.3 | 1.3 ± 0.2 | 0.9 ± 0.2 | 0.9 ± 0.2 | 0.4 (0.3–0.5) | <0.0001 * |
| Protein intake (g/day) | 100.8 ± 26.6 | 101.3 ± 19.8 | 66.4 ± 14.4 | 67.9 ± 15.6 | 33.1 (24.5–41.7) | <0.0001 * |
| Carbohydrate intake (g/day) | 187.6 ± 52.5 | 180.9 ± 54.0 | 194.3 ± 61.3 | 183.2 ± 46.6 | −2.5 (−20.8–15.8) | 0.8486 |
| Fat intake (g/day) | 72.7 ± 27.1 | 69.9 ± 25.8 | 74.2 ± 25.1 | 74.3 ± 15.8 | −1.8 (−11.5–8.0) | 0.7255 |
| Diet Group | Control Group | Difference at 6 Months | ||||
|---|---|---|---|---|---|---|
| Baseline | 6 Months | Baseline | 6 Months | B (95%-CI) | p-Value | |
| SNAQ appetite score (n = 90) | 14.9 ± 1.7 | 14.9 ± 2.1 | 15.0 ± 2.1 | 15.3 ± 2.1 | −0.36 (−1.10–0.39) | 0.347 |
| Average VAS appetite score (n = 48) | 4.7 (3.3–5.8) | 4.5 (2.8–6.3) | 5.3 (3.3–6.4) | 5.0 (3.8–6.2) | −0.20 (−1.10–0.70) | 0.657 |
| How hungry are you | 4.0 (2.0–6.0) | 3.0 (1.0–6.0) | 4.1 (1.0–6.0) | 4.5 (1.7–6.0) | −0.62 (−1.80–0.56) | 0.293 |
| How full are you | 2.9 (2.0–5.0) | 2.0 (1.0–3.5) | 2.6 (1.0–5.4) | 3.0 (2.0–5.5) | −1.06 (−2.35–0.23) | 0.104 |
| How eager are you to eat | 5.0 (3.0–7.0) | 5.0 (2.0–6.0) | 6.8 (2.0–7.1) | 5.9 (4.2–7.0) | −0.44 (−1.65–0.77) | 0.469 |
| How much could you eat | 5.0 (3.9–6.9) | 5.0 (3.0–5.5) | 6.0 (4.0–7.0) | 5.5 (4.6–7.0) | −0.77 (−1.80–0.26) | 0.139 |
| How strong is the urge to eat | 4.0 (2.0–6.0) | 4.0 (2.0–6.0) | 5.0 (0.8–7.0) | 5.0 (2.0–6.0) | −0.15 (−1.50–1.20) | 0.825 |
| How strong is the thought of food in your head | 3.0 (1.5–7.0) | 3.0 (1.0–6.0) | 5.0 (1.0–7.0) | 5.0 (2.0–6.0) | −0.48 (−1.93–0.97) | 0.507 |
| Side | MNI | |||||||
|---|---|---|---|---|---|---|---|---|
| Cluster | Voxels | Z-Max | x | y | z | p-Value * | ||
| Food vs. non-food pictures | ||||||||
| Lateral occipital cortex Lateral occipital cortex Superior parietal lobe Cingulate gyrus Superior parietal lobe Lateral occipital cortex | R L R L L L | 6 5 4 3 2 1 | 2751 2418 478 205 201 201 | 7.01 6.52 5.5 4.59 4.19 4.05 | 40 −44 32 −6 −34 −26 | −78 −74 −52 −54 −54 −64 | −10 −4 62 26 66 30 | 2.15 × 10−17 6.3 × 10−16 3.92 × 10−5 0.0096 0.0106 0.0106 |
| High-caloric vs. non-food pictures | ||||||||
| Insula | L | 7 | 218 | 5.73 | −44 | −30 | 34 | 0.00914 |
| Lateral occipital cortex Lateral occipital cortex Lateral occipital cortex Cingulate gyrus Superior parietal lobe Supramarginal gyrus | R L L L L L | 6 5 4 3 2 1 | 4150 3185 295 289 206 156 | 7.08 6.77 4.52 4.72 4.46 4.61 | 46 −44 −20 −6 −32 −44 | −72 −74 −82 −54 −56 −30 | 0 −4 44 26 66 34 | 4.75 × 10−22 2.02 × 10−18 0.00182 0.00205 0.0119 0.0383 |
| Picture Task | Palatable Food Task | |||||||
|---|---|---|---|---|---|---|---|---|
| Food vs. Non-Food | High Caloric vs. Non-Food | Anticipation Chocolate vs. Tasteless Solution | Receipt Chocolate vs. Tasteless Solution | |||||
| B (95%-CI) | p-Value | B (95%-CI) | p-Value | B (95%-CI) | p-Value | B (95%-CI) | p-Value | |
| Putamen right | −0.02 (−0.08–0.03) | 0.385 | −0.04 (−0.11–0.03) | 0.255 | 0.03 (−0.05–0.11) | 0.485 | −0.02 (−0.07–0.03) | 0.495 |
| Insula right | −0.01 (−0.07–0.05) | 0.750 | −0.04 (−0.11–0.03) | 0.272 | 0.07 (0.00–0.13) | 0.045 * | 0.01 (−0.03–0.06) | 0.474 |
| Amygdala right | −0.06 (−0.15–0.03) | 0.178 | −0.07 (−0.19–0.05) | 0.260 | 0.03 (−0.08–0.13) | 0.614 | −0.03 (−0.12–0.06) | 0.475 |
| Caudate nucleus right | −0.02 (−0.07–0.03) | 0.394 | −0.04 (−0.11–0.04) | 0.307 | 0.06 (−0.01–0.14) | 0.091 | −0.03 (−0.09–0.02) | 0.220 |
| Putamen left | −0.04 (−0.09–0.01) | 0.151 | −0.05 (−0.12–0.02) | 0.157 | 0.03 (−0.03–0.10) | 0.334 | −0.04 (−0.10–0.01) | 0.134 |
| Insula left | −0.04 (−0.10–0.03) | 0.256 | −0.05 (−0.12–0.02) | 0.132 | 0.03 (−0.04–0.11) | 0.385 | −0.01 (−0.05–0.04) | 0.759 |
| Amygdala left | −0.04 (−0.13–0.06) | 0.445 | −0.07 (−0.19–0.05) | 0.227 | 0.09 (−0.01–0.19) | 0.063 | −0.05 (−0.14–0.03) | 0.224 |
| Caudate nucleus left | −0.02 (−0.07–0.04) | 0.480 | −0.03 (−0.11–0.04) | 0.359 | 0.04 (−0.04–0.11) | 0.305 | −0.04 (−0.09–0.02) | 0.162 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fluitman, K.S.; Wijdeveld, M.; Davids, M.; van Ruiten, C.C.; Reinders, I.; Wijnhoven, H.A.H.; Keijser, B.J.F.; Visser, M.; Nieuwdorp, M.; IJzerman, R.G. Personalized Dietary Advice to Increase Protein Intake in Older Adults Does Not Affect the Gut Microbiota, Appetite or Central Processing of Food Stimuli in Community-Dwelling Older Adults: A Six-Month Randomized Controlled Trial. Nutrients 2023, 15, 332. https://doi.org/10.3390/nu15020332
Fluitman KS, Wijdeveld M, Davids M, van Ruiten CC, Reinders I, Wijnhoven HAH, Keijser BJF, Visser M, Nieuwdorp M, IJzerman RG. Personalized Dietary Advice to Increase Protein Intake in Older Adults Does Not Affect the Gut Microbiota, Appetite or Central Processing of Food Stimuli in Community-Dwelling Older Adults: A Six-Month Randomized Controlled Trial. Nutrients. 2023; 15(2):332. https://doi.org/10.3390/nu15020332
Chicago/Turabian StyleFluitman, Kristina S., Madelief Wijdeveld, Mark Davids, Charlotte C. van Ruiten, Ilse Reinders, Hanneke A. H. Wijnhoven, Bart J. F. Keijser, Marjolein Visser, Max Nieuwdorp, and Richard G. IJzerman. 2023. "Personalized Dietary Advice to Increase Protein Intake in Older Adults Does Not Affect the Gut Microbiota, Appetite or Central Processing of Food Stimuli in Community-Dwelling Older Adults: A Six-Month Randomized Controlled Trial" Nutrients 15, no. 2: 332. https://doi.org/10.3390/nu15020332
APA StyleFluitman, K. S., Wijdeveld, M., Davids, M., van Ruiten, C. C., Reinders, I., Wijnhoven, H. A. H., Keijser, B. J. F., Visser, M., Nieuwdorp, M., & IJzerman, R. G. (2023). Personalized Dietary Advice to Increase Protein Intake in Older Adults Does Not Affect the Gut Microbiota, Appetite or Central Processing of Food Stimuli in Community-Dwelling Older Adults: A Six-Month Randomized Controlled Trial. Nutrients, 15(2), 332. https://doi.org/10.3390/nu15020332