Sodium Intake as a Cardiovascular Risk Factor: A Narrative Review
Abstract
:1. Introduction
2. Sodium Intake, Blood Pressure and Cardiovascular Outcomes
2.1. Blood Pressure
2.2. Cardiovascular Outcomes
3. Pathophysiological Considerations
3.1. Basic Principles
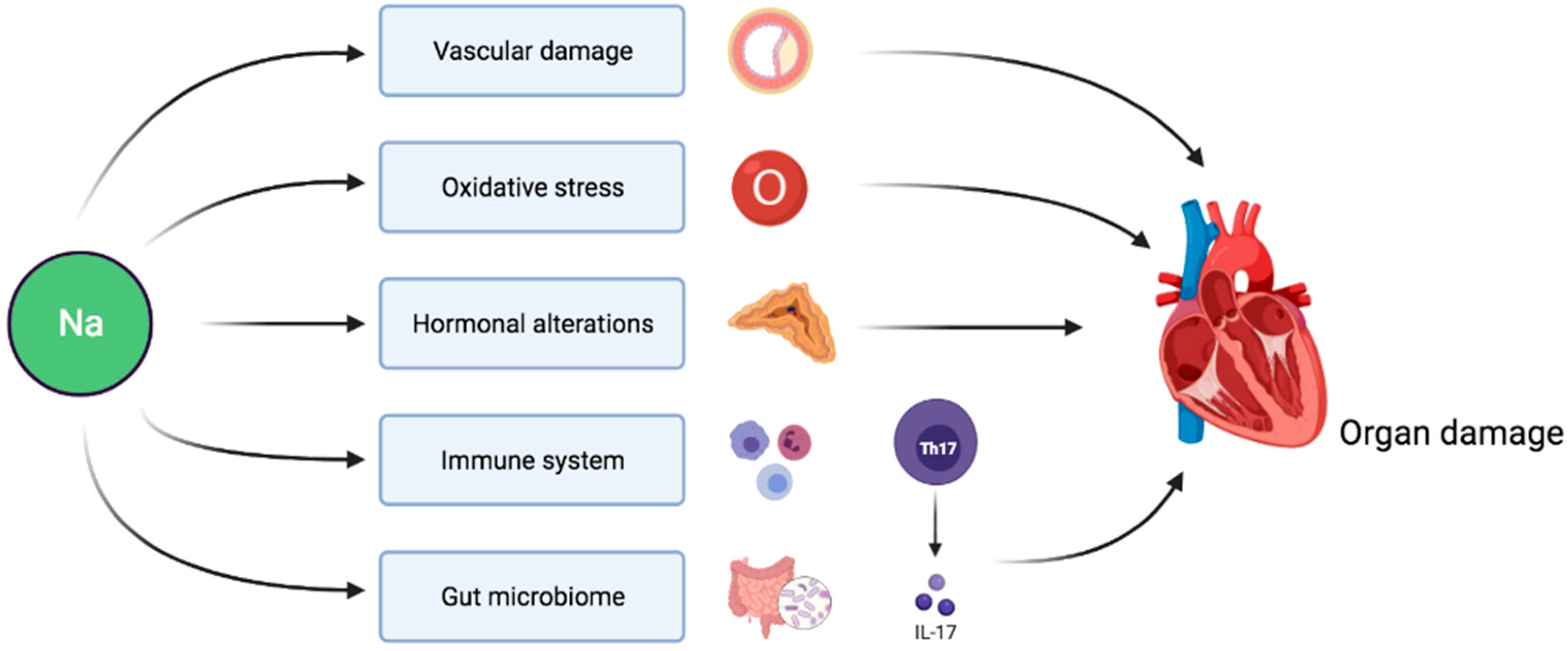
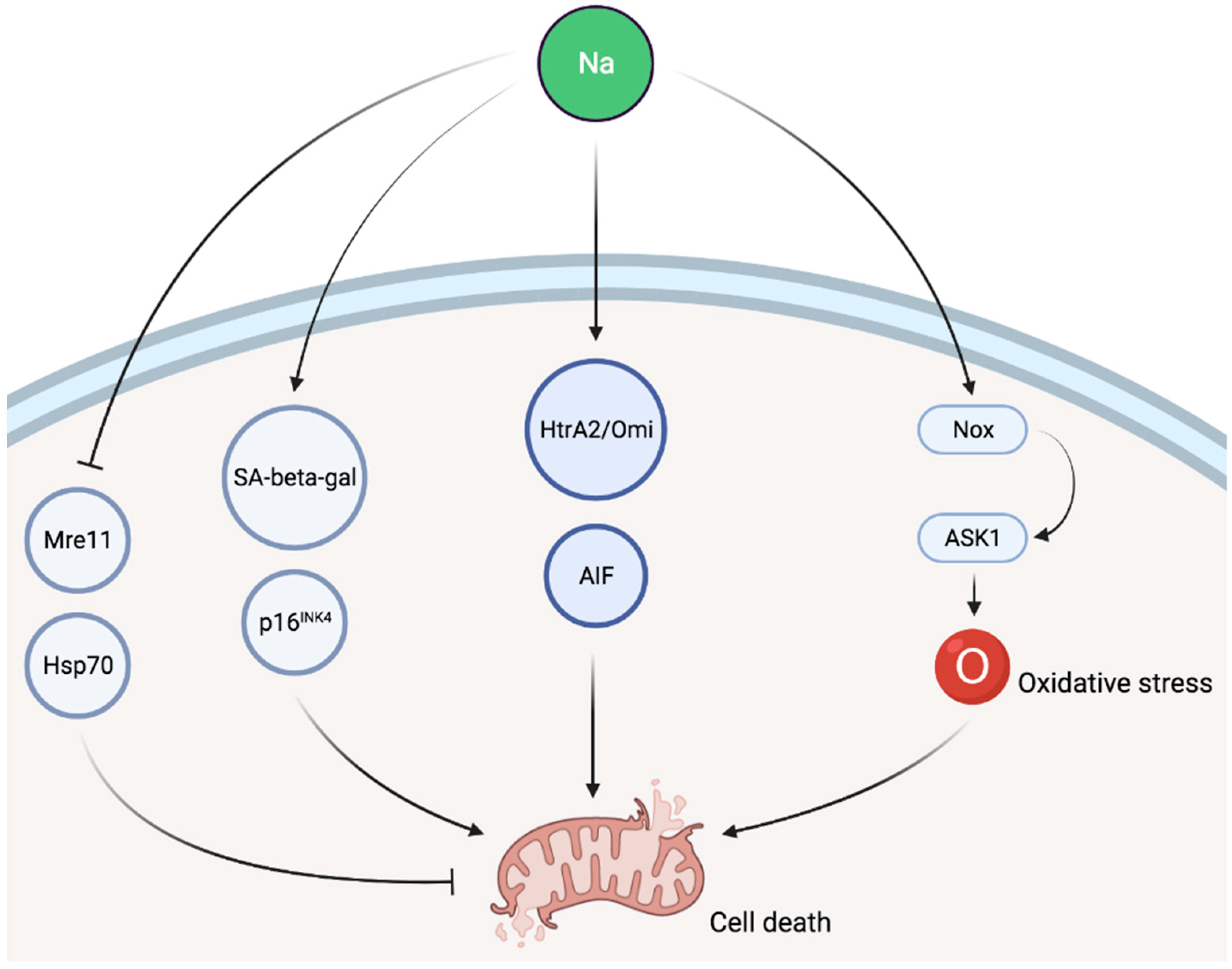
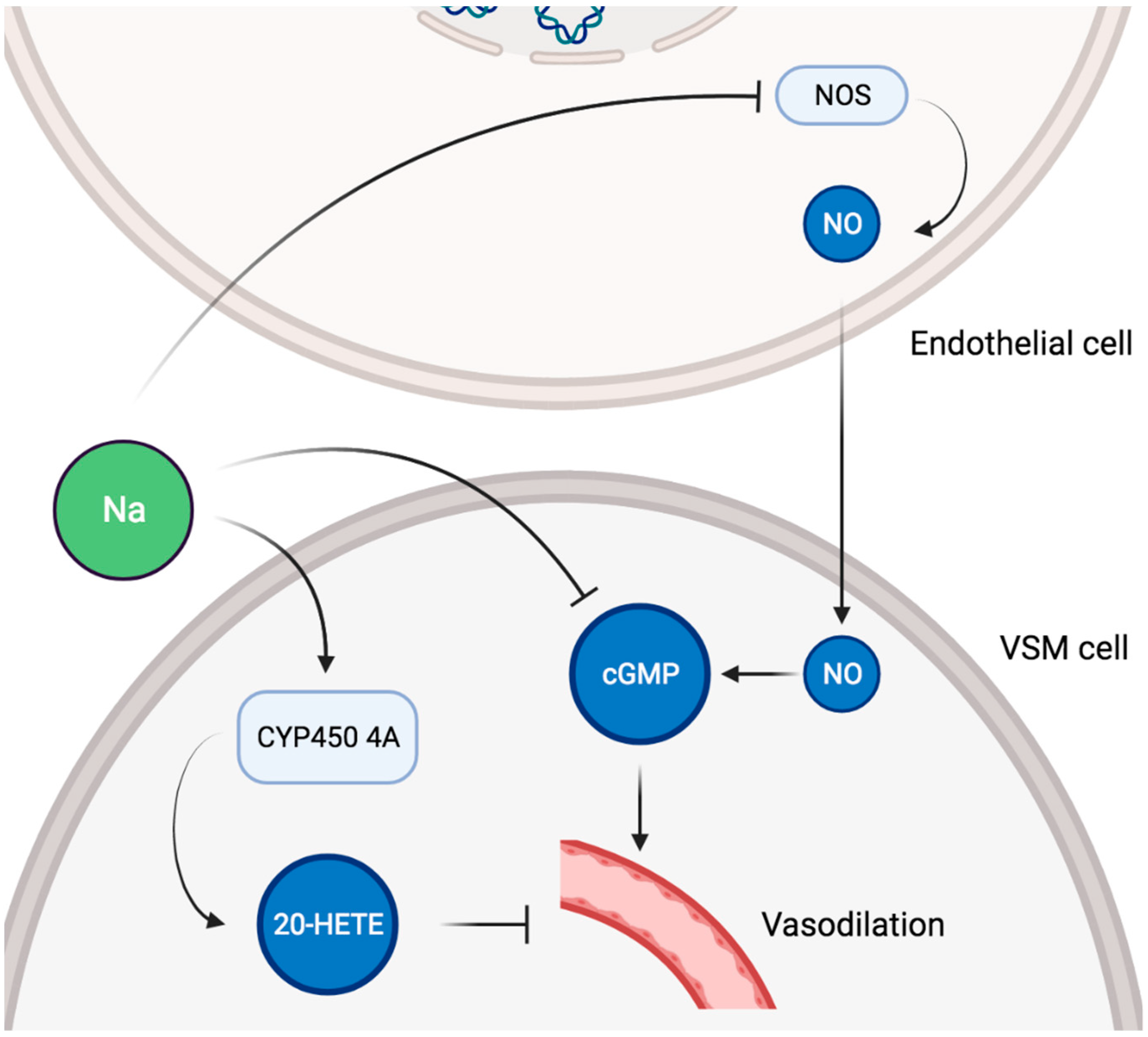
3.2. Organ Damage and Cardiovascular Impact
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- He, F.J.; MacGregor, G.A. Salt, blood pressure and cardiovascular disease. Curr. Opin. Cardiol. 2007, 22, 298–305. [Google Scholar] [CrossRef]
- Thout, S.R.; Santos, J.A.; McKenzie, B.; Trieu, K.; Johnson, C.; McLean, R.; Arcand, J.A.; Campbell, N.R.C.; Webster, J. The Science of Salt: Updating the evidence on global estimates of salt intake. J. Clin. Hypertens. 2019, 21, 710–721. [Google Scholar] [CrossRef] [Green Version]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Lewington, S.; Clarke, R.; Qizilbash, N.; Peto, R.; Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002, 360, 1903–1913. [Google Scholar] [CrossRef]
- O’Donnell, M.; Mente, A.; Alderman, M.H.; Brady, A.J.B.; Diaz, R.; Gupta, R.; López-Jaramillo, P.; Luft, F.C.; Lüscher, T.F.; Mancia, G.; et al. Salt and cardiovascular disease: Insufficient evidence to recommend low sodium intake. Eur. Heart J. 2020, 41, 3363–3373. [Google Scholar] [CrossRef] [PubMed]
- Rose, G.; Stamler, J.; Stamler, R.; Elliott, P.; Marmot, M.; Pyorala, K.; Kesteloot, H.; Joossens, J.; Hansson, L.; Mancia, G.; et al. Intersalt: An international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Br. Med. J. 1988, 297, 319–328. [Google Scholar] [CrossRef] [Green Version]
- Mente, A.; O’Donnell, M.J.; Rangarajan, S.; McQueen, M.J.; Poirier, P.; Wielgosz, A.; Morrison, H.; Li, W.; Wang, X.; Di, C.; et al. Association of Urinary Sodium and Potassium Excretion with Blood Pressure. N. Engl. J. Med. 2014, 371, 601–611. [Google Scholar] [CrossRef] [Green Version]
- Welsh, C.E.; Welsh, P.; Jhund, P.; Delles, C.; Celis-Morales, C.; Lewsey, J.D.; Gray, S.; Lyall, D.; Iliodromiti, S.; Gill, J.M.R.; et al. Urinary Sodium Excretion, Blood Pressure, and Risk of Future Cardiovascular Disease and Mortality in Subjects without Prior Cardiovascular Disease. Hypertension 2019, 73, 1202–1209. [Google Scholar] [CrossRef] [PubMed]
- Stolarz-Skrzypek, K.; Kuznetsova, T.; Thijs, L.; Tikhonoff, V.; Seidlerová, J.; Richart, T.; Jin, Y.; Olszanecka, A.; Malyutina, S.; Casiglia, E.; et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. J. Am. Med. Assoc. 2011, 305, 1777–1785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on Blood Pressure of Reduced Dietary Sodium and the Dietary Approaches to Stop Hypertension (DASH) Diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Cutler, J.A. Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure: The trials of hypertension prevention, phase II. Arch. Intern. Med. 1997, 157, 657–667. [Google Scholar] [CrossRef]
- Whelton, P.K.; Appel, L.J.; Espeland, M.A.; Applegate, W.B.; Ettinger, W.H.; Kostis, J.B.; Kumanyika, S.; Lacy, C.R.; Johnson, K.C.; Folmar, S.; et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: A randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). J. Am. Med. Assoc. 1998, 279, 839–846. [Google Scholar] [CrossRef]
- Aburto, N.J.; Ziolkovska, A.; Hooper, L.; Elliott, P.; Cappuccio, F.P.; Meerpohl, J.J. Effect of lower sodium intake on health: Systematic review and meta-analyses. BMJ 2013, 346, f1326. [Google Scholar] [CrossRef] [Green Version]
- He, F.J.; Li, J.; MacGregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef] [Green Version]
- Graudal, N.A.; Hubeck-Graudal, T.; Jurgens, G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Rhee, O.J.; Rhee, M.Y.; Oh, S.W.; Shin, S.J.; Gu, N.; Nah, D.Y.; Kim, S.W.; Lee, J.H. Effect of sodium intake on renin level: Analysis of general population and meta-analysis of randomized controlled trials. Int. J. Cardiol. 2016, 215, 120–126. [Google Scholar] [CrossRef]
- He, F.J.; MacGregor, G.A. How Far Should Salt Intake Be Reduced? Hypertension 2003, 42, 1093–1099. [Google Scholar] [CrossRef] [Green Version]
- Macgregor, G.A.; Sagnella, G.A.; Markandu, N.D.; Singer, D.R.J.; Cappuccio, F.P. Double-blind study of three sodium intakes and long-term effects of sodium restriction in essential hypertension. Lancet 1989, 334, 1244–1247. [Google Scholar] [CrossRef]
- He, F.J.; Markandu, N.D.; MacGregor, G.A. Importance of the renin system for determining blood pressure fall with acute salt restriction in hypertensive and normotensive whites. Hypertension 2001, 38, 321–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, F.J.; Markandu, N.D.; Sagnella, G.A.; MacGregor, G.A. Importance of the renin system in determining blood pressure fall with salt restriction in black and white hypertensives. Hypertension 1998, 32, 820–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacGregor, G.A.; Markandu, N.D.; Jsinger, D.R.; Cappuccio, F.P.; Shore, A.C.; Sagnella, G.A. Moderate sodium restriction with angiotensin converting enzyme inhibitor in essential hypertension: A double blind study. Br. Med. J. (Clin. Res. Ed.) 1987, 294, 531–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elijovich, F.; Weinberger, M.H.; Anderson, C.A.M.; Appel, L.J.; Bursztyn, M.; Cook, N.R.; Dart, R.A.; Newton-Cheh, C.H.; Sacks, F.M.; Laffer, C.L. Salt sensitivity of blood pressure: A scientific statement from the American Heart Association. Hypertension 2016, 68, e7–e46. [Google Scholar] [CrossRef] [Green Version]
- Weinberger, M.H.; Miller, J.Z.; Luft, F.C.; Grim, C.E.; Fineberg, N.S. Definitions and characteristics of sodium sensitivity and blood pressure resistance. Hypertension 1986, 8, II-127–II-134. [Google Scholar] [CrossRef] [Green Version]
- Balafa, O.; Kalaitzidis, R.G. Salt sensitivity and hypertension. J. Hum. Hypertens. 2021, 35, 184–192. [Google Scholar] [CrossRef]
- Rocchini, A.P. Obesity hypertension, salt sensitivity and insulin resistance. Nutr. Metab. Cardiovasc. Dis. 2000, 10, 287–294. [Google Scholar] [PubMed]
- Weir, M.R.; Chrysant, S.G.; McCarron, D.A.; Canossa-Terris, M.; Cohen, J.D.; Gunter, P.A.; Lewin, A.J.; Mennella, R.F.; Kirkegaard, L.W.; Hamilton, J.H.; et al. Influence of race and dietary salt on the antihypertensive efficacy of an angiotensin-converting enzyme inhibitor or a calcium channel antagonist in salt-sensitive hypertensives. Hypertension 1998, 31, 1088–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, J.; Gu, D.; Chen, J.; Jaquish, C.E.; Rao, D.C.; Hixson, J.E.; Chen, J.C.; Duan, X.; Huang, J.F.; Chen, C.S.; et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J. Hypertens. 2009, 27, 48–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, W.; Dell’Italia, L.J.; Sanders, P.W. Novel paradigms of salt and hypertension. J. Am. Soc. Nephrol. 2017, 28, 1362–1369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Miyaki, K.; Araki, J.; Song, Y.; Kimura, T.; Omae, K.; Muramatsu, M. Interaction of angiotensin I-Converting enzyme insertion-deletion polymorphism and daily salt intake influences hypertension in Japanese men. Hypertens. Res. 2006, 29, 751–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Juraschek, S.P.; Woodward, M.; Sacks, F.M.; Carey, V.J.; Miller, E.R.; Appel, L.J. Time Course of Change in Blood Pressure from Sodium Reduction and the DASH Diet. Hypertension 2017, 70, 923–929. [Google Scholar] [CrossRef]
- Whelton, P.K.; Appel, L.; Charleston, J. The Effects of Nonpharmacologic Interventions on Blood Pressure of Persons With High Normal Levels: Results of the Trials of Hypertension Prevention, Phase I. J. Am. Med. Assoc. 1992, 267, 1213–1220. [Google Scholar] [CrossRef]
- Strazzullo, P.; D’Elia, L.; Kandala, N.B.; Cappuccio, F.P. Salt intake, stroke, and cardiovascular disease: Meta-analysis of prospective studies. BMJ 2009, 339, 1296. [Google Scholar] [CrossRef] [Green Version]
- Poggio, R.; Gutierrez, L.; Matta, M.G.; Elorriaga, N.; Irazola, V.; Rubinstein, A. Daily sodium consumption and CVD mortality in the general population: Systematic review and meta-analysis of prospective studies. Public Health Nutr. 2015, 18, 695–704. [Google Scholar] [CrossRef]
- Graudal, N.; Jürgens, G.; Baslund, B.; Alderman, M.H. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: A meta-analysis. Am. J. Hypertens. 2014, 27, 1129–1137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mente, A.; O’Donnell, M.; Rangarajan, S.; Dagenais, G.; Lear, S.; McQueen, M.; Diaz, R.; Avezum, A.; Lopez-Jaramillo, P.; Lanas, F.; et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: A pooled analysis of data from four studies. Lancet 2016, 388, 465–475. [Google Scholar] [CrossRef]
- O’Donnell, M.J.; Yusuf, S.; Mente, A.; Gao, P.; Mann, J.F.; Teo, K.; McQueen, M.; Sleight, P.; Sharma, A.M.; Dans, A.; et al. Urinary sodium and potassium excretion and risk of cardiovascular events. J. Am. Med. Assoc. 2011, 306, 2229–2238. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, M.; Mente, A.; Rangarajan, S.; McQueen, M.J.; Wang, X.; Liu, L.; Yan, H.; Lee, S.F.; Mony, P.; Devanath, A.; et al. Urinary Sodium and Potassium Excretion, Mortality, and Cardiovascular Events. N. Engl. J. Med. 2014, 371, 612–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawasaki, T.; Itoh, K.; Uezono, K.; Sasaki, H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin. Exp. Pharmacol. Physiol. 1993, 20, 7–14. [Google Scholar] [CrossRef]
- Cook, N.R.; Appel, L.J.; Whelton, P.K. Sodium Intake and All-Cause Mortality Over 20 Years in the Trials of Hypertension Prevention. J. Am. Coll. Cardiol. 2016, 68, 1609–1617. [Google Scholar] [CrossRef] [PubMed]
- Olde Engberink, R.H.G.; Van Den Hoek, T.C.; Van Noordenne, N.D.; Van Den Born, B.J.H.; Peters-Sengers, H.; Vogt, L. Use of a single baseline versus multiyear 24-hour urine collection for estimation of long-term sodium intake and associated cardiovascular and renal risk. Circulation 2017, 136, 917–926. [Google Scholar] [CrossRef]
- Mills, K.T.; Chen, J.; Yang, W.; Appel, L.J.; Kusek, J.W.; Alper, A.; Delafontaine, P.; Keane, M.G.; Mohler, E.; Ojo, A.; et al. Sodium excretion and the risk of cardiovascular disease in patients with chronic kidney disease. J. Am. Med. Assoc. 2016, 315, 2200–2210. [Google Scholar] [CrossRef]
- Cook, N.R.; Appel, L.J.; Whelton, P.K. Lower levels of sodium intake and reduced cardiovascular risk. Circulation 2014, 129, 981–989. [Google Scholar] [CrossRef] [Green Version]
- He, F.J.; Ma, Y.; Campbell, N.R.C.; Macgregor, G.A.; Cogswell, M.E.; Cook, N.R. Formulas to estimate dietary sodium intake from spot urine alter sodium-mortality relationship. Hypertension 2019, 74, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Naser, A.M.; He, F.J.; Rahman, M.; Campbell, N.R.C. Spot Urine Formulas to Estimate 24-Hour Urinary Sodium Excretion Alter the Dietary Sodium and Blood Pressure Relationship. Hypertension 2021, 77, 2127–2137. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.; Garrison, R.J.; Savage, D.D.; Kannel, W.B.; Castelli, W.P. Prognostic Implications of Echocardiographically Determined Left Ventricular Mass in the Framingham Heart Study. N. Engl. J. Med. 1990, 322, 1561–1566. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Kuznetsova, T.; Maillard, M.; Richart, T.; Thijs, L.; Bochud, M.; Herregods, M.C.; Burnier, M.; Fagard, R.; Staessen, J.A. Independent relations of left ventricular structure with the 24-hour urinary excretion of sodium and aldosterone. Hypertension 2009, 54, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Burnier, M.; Phan, O.; Wang, Q. High salt intake: A cause of blood pressure-independent left ventricular hypertrophy? Nephrol. Dial. Transplant. 2007, 22, 2426–2429. [Google Scholar] [CrossRef] [Green Version]
- Messerli, F.H.; Schmieder, R.E.; Weir, M.R. Salt: A perpetrator of hypertensive target organ disease? Arch. Intern. Med. 1997, 157, 2449–2452. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Ogden, L.G.; Bazzano, L.A.; Vupputuri, S.; Loria, C.; Whelton, P.K. Dietary sodium intake and incidence of congestive heart failure in overweight US men and women: First national health and nutrition examination survey epidemiologic follow-up study. Arch. Intern. Med. 2002, 162, 1619–1624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hummel, S.L.; DeFranco, A.C.; Skorcz, S.; Montoye, C.K.; Koelling, T.M. Recommendation of Low-Salt Diet and Short-term Outcomes in Heart Failure with Preserved Systolic Function. Am. J. Med. 2009, 122, 1029–1036. [Google Scholar] [CrossRef] [Green Version]
- Cogswell, M.E.; Mugavero, K.; Bowman, B.A.; Frieden, T.R. Dietary Sodium and Cardiovascular Disease Risk—Measurement Matters. N. Engl. J. Med. 2016, 375, 580–586. [Google Scholar] [CrossRef] [Green Version]
- He, F.J.; Pombo-Rodrigues, S.; MacGregor, G.A. Salt reduction in England from 2003 to 2011: Its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014, 4, 4549. [Google Scholar] [CrossRef] [Green Version]
- Laatikainen, T.; Critchley, J.; Vartiainen, E.; Salomaa, V.; Ketonen, M.; Capewell, S. Explaining the decline in coronary heart disease mortality in Finland between 1982 and 1997. Am. J. Epidemiol. 2005, 162, 764–773. [Google Scholar] [CrossRef]
- Chang, H.Y.; Hu, Y.W.; Yue, C.S.J.; Wen, Y.W.; Yeh, W.T.; Hsu, L.S.; Tsai, S.Y.; Pan, W.H. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am. J. Clin. Nutr. 2006, 83, 1289–1296. [Google Scholar] [CrossRef]
- Taylor, R.S.; Ashton, K.E.; Moxham, T.; Hooper, L.; Ebrahim, S. Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2011, 2011, CD009217. [Google Scholar]
- He, F.J.; MacGregor, G.A. Salt reduction lowers cardiovascular risk: Meta-analysis of outcome trials. Lancet 2011, 378, 380–382. [Google Scholar] [CrossRef]
- Paterna, S.; Gaspare, P.; Fasullo, S.; Sarullo, F.M.; Di Pasquale, P. Normal-sodium diet compared with low-sodium diet in compensated congestive heart failure: Is sodium an old enemy or a new friend? Clin. Sci. 2008, 114, 221–230. [Google Scholar] [CrossRef] [Green Version]
- Sasso, F.C.; De Nicola, L.; Carbonara, O.; Nasti, R.; Minutolo, R.; Salvatore, T.; Conte, G.; Torella, R. Cardiovascular risk factors and disease management in type 2 diabetic patients with diabetic nephropathy. Diabetes Care 2006, 29, 498–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sasso, F.C.; Pafundi, P.C.; Simeon, V.; De Nicola, L.; Chiodini, P.; Galiero, R.; Rinaldi, L.; Nevola, R.; Salvatore, T.; Sardu, C.; et al. Efficacy and durability of multifactorial intervention on mortality and MACEs: A randomized clinical trial in type-2 diabetic kidney disease. Cardiovasc. Diabetol. 2021, 20, 145. [Google Scholar] [CrossRef]
- Dahl, L.; Heine, M.; Thompson, K. Genetic influence of the kidneys on blood pressure. Evidence from chronic renal homografts in rats with opposite predispositions to hypertension. Circ. Res. 1977, 40, 94–101. [Google Scholar] [CrossRef] [Green Version]
- Dahl, L.K.; Heine, M.; Thompson, K. Genetic Influence of Renal Homografts on the Blood Pressure of Rats from Different Strains. Proc. Soc. Exp. Biol. Med. 1972, 140, 852–856. [Google Scholar] [CrossRef] [PubMed]
- Guyton, A.C. Blood pressure control-Special role of the kidneys and body fluids. Science 1991, 252, 1813–1816. [Google Scholar] [CrossRef]
- de Wardener, H.E.; He, F.J.; MacGregor, G.A. Plasma sodium and hypertension. Kidney Int. 2004, 66, 2454–2466. [Google Scholar] [PubMed] [Green Version]
- He, F.J.; Markandu, N.D.; Sagnella, G.A.; De Wardener, H.E.; MacGregor, G.A. Plasma sodium: Ignored and underestimated. Hypertension 2005, 45, 98–102. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Markandu, N.D.; Sagnella, G.A.; MacGregor, G.A. Effect of salt intake on renal excretion of water in humans. Hypertension 2001, 38, 317–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedman, S.M.; McIndoe, R.A.; Tanaka, M. The relation of blood sodium concentration to blood pressure in the rat. J. Hypertens. 1990, 8, 61–66. [Google Scholar] [CrossRef] [PubMed]
- McMaster, W.G.; Kirabo, A.; Madhur, M.S.; Harrison, D.G. Inflammation, Immunity, and Hypertensive End-Organ Damage. Circ. Res. 2015, 116, 1022–1033. [Google Scholar] [CrossRef]
- Edwards, D.G.; Farquhar, W.B. Vascular effects of dietary salt. Curr. Opin. Nephrol. Hypertens. 2015, 24, 8–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Wardener, H.E. The hypothalamus and hypertension. Physiol. Rev. 2001, 81, 1599–1658. [Google Scholar] [CrossRef]
- Nadar, S.; Tayebjee, M.; Messerli, F.; Lip, G. Target Organ Damage in Hypertension: Pathophysiology and Implications for Drug Therapy. Curr. Pharm. Des. 2006, 12, 1581–1592. [Google Scholar] [CrossRef] [PubMed]
- Kwakernaak, A.J.; Waanders, F.; Slagman, M.C.J.; Dokter, M.M.; Laverman, G.D.; De Boer, R.A.; Navis, G. Sodium restriction on top of renin-angiotensin-aldosterone system blockade increases circulating levels of N-acetyl-seryl-aspartyl-lysyl-proline in chronic kidney disease patients. J. Hypertens. 2013, 31, 2425–2432. [Google Scholar] [CrossRef]
- Yu, H.C.M.; Burrell, L.M.; Black, M.J.; Wu, L.L.; Dilley, R.J.; Cooper, M.E.; Johnston, C.I. Salt induces myocardial and renal fibrosis in normotensive and hypertensive rats. Circulation 1998, 98, 2621–2628. [Google Scholar] [CrossRef] [Green Version]
- Ying, W.Z.; Sanders, P.W. Dietary salt modulates renal production of transforming growth factor-β in rats. Am. J. Physiol-Ren. Physiol. 1998, 274, F635–F641. [Google Scholar] [CrossRef] [PubMed]
- Kitiyakara, C.; Chabrashvili, T.; Chen, Y.; Blau, J.; Karber, A.; Aslam, S.; Welch, W.J.; Wilcox, C.S. Salt Intake, Oxidative Stress, and Renal Expression of NADPH Oxidase and Superoxide Dismutase. J. Am. Soc. Nephrol. 2003, 14, 2775–2782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tojo, A.; Kimoto, M.; Wilcox, C.S. Renal expression of constitutive NOS and DDAH: Separate effects of salt intake and angiotensin. Kidney Int. 2000, 58, 2075–2083. [Google Scholar] [CrossRef]
- Jablonski, K.L.; Racine, M.L.; Geolfos, C.J.; Gates, P.E.; Chonchol, M.; McQueen, M.B.; Seals, D.R. Dietary sodium restriction reverses vascular endothelial dysfunction in middle-aged/older adults with moderately elevated systolic blood pressure. J. Am. Coll. Cardiol. 2013, 61, 335–343. [Google Scholar] [CrossRef] [Green Version]
- Dmitrieva, N.I.; Burg, M.B. Living with DNA breaks is an everyday reality for cells adapted to high NaCl. Cell Cycle 2004, 3, 559–561. [Google Scholar] [CrossRef] [Green Version]
- Dmitrieva, N.I.; Bulavin, D.V.; Burg, M.B. High NaCl causes Mre11 to leave the nucleus, disrupting DNA damage signaling and repair. Am. J. Physiol-Ren. Physiol. 2003, 285, F266–F274. [Google Scholar] [CrossRef] [Green Version]
- Dmitrieva, N.I.; Burg, M.B. High NaCl promotes cellular senescence. Cell Cycle 2007, 6, 3108–3113. [Google Scholar] [CrossRef]
- Siu, P.M.; Bae, S.; Bodyak, N.; Rigor, D.L.; Kang, P.M. Response of caspase-independent apoptotic factors to high salt diet-induced heart failure. J. Mol. Cell. Cardiol. 2007, 42, 678–686. [Google Scholar] [CrossRef] [Green Version]
- Kataoka, K.; Tokutomi, Y.; Yamamoto, E.; Nakamura, T.; Fukuda, M.; Dong, Y.F.; Ichijo, H.; Ogawa, H.; Kim-Mitsuyama, S. Apoptosis signal-regulating kinase 1 deficiency eliminates cardiovascular injuries induced by high-salt diet. J. Hypertens. 2011, 29, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Kataoka, K.; Fukuda, M.; Nako, H.; Tokutomi, Y.; Dong, Y.F.; Ichijo, H.; Ogawa, H.; Kim-Mitsuyama, S. Critical role of apoptosis signal-regulating kinase 1 in aldosterone/salt-induced cardiac inflammation and fibrosis. Hypertension 2009, 54, 544–551. [Google Scholar] [CrossRef] [Green Version]
- Dickinson, K.M.; Clifton, P.M.; Burrell, L.M.; Barrett, P.H.R.; Keogh, J.B. Postprandial effects of a high salt meal on serum sodium, arterial stiffness, markers of nitric oxide production and markers of endothelial function. Atherosclerosis 2014, 232, 211–216. [Google Scholar] [CrossRef]
- Dickinson, K.M.; Clifton, P.M.; Keogh, J.B. Endothelial function is impaired after a high-salt meal in healthy subjects. Am. J. Clin. Nutr. 2011, 93, 500–505. [Google Scholar] [CrossRef]
- Dickinson, K.M.; Clifton, P.M.; Keogh, J.B. A reduction of 3 g/day from a usual 9 g/day salt diet improves endothelial function and decreases endothelin-1 in a randomised cross_over study in normotensive overweight and obese subjects. Atherosclerosis 2014, 233, 32–38. [Google Scholar] [CrossRef]
- Matthews, E.L.; Brian, M.S.; Ramick, M.G.; Lennon-Edwards, S.; Edwards, D.G.; Farquhar, W.B. High dietary sodium reduces brachial artery flow-mediated dilation in humans with salt-sensitive and salt-resistant blood pressure. J. Appl. Physiol. 2015, 118, 1510–1515. [Google Scholar] [CrossRef] [Green Version]
- DuPont, J.J.; Greaney, J.L.; Wenner, M.M.; Lennon-Edwards, S.L.; Sanders, P.W.; Farquhar, W.B.; Edwards, D.G. High dietary sodium intake impairs endothelium-dependent dilation in healthy salt-resistant humans. J. Hypertens. 2013, 31, 530–536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greaney, J.L.; Dupont, J.J.; Lennon-Edwards, S.L.; Sanders, P.W.; Edwards, D.G.; Farquhar, W.B. Dietary sodium loading impairs microvascular function independent of blood pressure in humans: Role of oxidative stress. J. Physiol. 2012, 590, 5519–5528. [Google Scholar] [CrossRef]
- Jaques, D.A.; Pruijm, M.; Ackermann, D.; Vogt, B.; Guessous, I.; Burnier, M.; Pechere-Bertschi, A.; Bochud, M.; Ponte, B. Sodium Intake Is Associated with Renal Resistive Index in an Adult Population-Based Study. Hypertension 2020, 76, 1898–1905. [Google Scholar] [CrossRef]
- Doi, Y.; Iwashima, Y.; Yoshihara, F.; Kamide, K.; Hayashi, S.I.; Kubota, Y.; Nakamura, S.; Horio, T.; Kawano, Y. Renal resistive index and cardiovascular and renal outcomes in essential hypertension. Hypertension 2012, 60, 770–777. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamano, K.; Nitta, A.; Ohtake, T.; Kobayashi, S. Associations of renal vascular resistance with albuminuria and other microangiopathy in type 2 diabetic patients. Diabetes Care 2008, 31, 1853–1857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avolio, A.P.; Fa-Quan, D.; Wei-Qiang, L. Effects of aging on arterial distensibility in populations with high and low prevalence of hypertension: Comparison between urban and rural communities in China. Circulation 1985, 71, 202–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avolio, A.P.; Clyde, K.M.; Beard, T.C.; Cooke, H.M.; Ho, K.K.; O’Rourke, M.F. Improved arterial distensibility in normotensive subjects on a low salt diet. Arteriosclerosis 1986, 6, 166–169. [Google Scholar] [CrossRef] [Green Version]
- Widlansky, M.E.; Gokce, N.; Keaney, J.F.; Vita, J.A. The clinical implications of endothelial dysfunction. J. Am. Coll. Cardiol. 2003, 42, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Ying, W.Z.; Sanders, P.W. Increased dietary salt activates rat aortic endothelium. Hypertension 2002, 39, 239–244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; White, J.; Guo, L.; Zhao, X.; Wang, J.; Smart, E.J.; Li, X.A. Salt inactivates endothelial nitric oxide synthase in endothelial cells. J. Nutr. 2009, 139, 447–451. [Google Scholar] [CrossRef]
- Ma, S.; Wang, Q.; Zhang, Y.; Yang, D.; Li, D.; Tang, B.; Yang, Y. Transgenic overexpression of uncoupling protein 2 attenuates salt-induced vascular dysfunction by inhibition of oxidative stress. Am. J. Hypertens. 2014, 27, 345–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, J.; Mori, T.; Huang, T.; Lombard, J.H. Effect of high-salt diet on NO release and superoxide production in rat aorta. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, H575–H583. [Google Scholar] [CrossRef] [PubMed]
- Kagota, S.; Tamashiro, A.; Yamaguchi, Y.; Sugiura, R.; Kuno, T.; Nakamura, K.; Kunitomo, M. Downregulation of vascular soluble guanylate cyclase induced by high salt intake in spontaneously hypertensive rats. Br. J. Pharmacol. 2001, 134, 737–744. [Google Scholar] [CrossRef] [Green Version]
- Kagota, S.; Tamashiro, A.; Yamaguchi, Y.; Nakamura, K.; Kunitomo, M. High salt intake impairs vascular nitric oxide/cyclic guanosine monophosphate system in spontaneously hypertensive rats. J. Pharmacol. Exp. Ther. 2002, 302, 344–351. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Roman, R.J.; Falck, J.R.; De La Cruz, L.; Lombard, J.H. Effects of high-salt diet on CYP450-4A ω-hydroxylase expression and active tone in mesenteric resistance arteries. Am. J. Physiol. Heart Circ. Physiol. 2005, 288, H1557–H1565. [Google Scholar] [CrossRef]
- Pimenta, E.; Gordon, R.D.; Ahmed, A.H.; Cowley, D.; Leano, R.; Marwick, T.H.; Stowasser, M. Cardiac dimensions are largely determined by dietary salt in patients with primary aldosteronism: Results of a case-control study. J. Clin. Endocrinol. Metab. 2011, 96, 2813–2820. [Google Scholar] [CrossRef]
- Catena, C.; Colussi, G.L.; Novello, M.; Verheyen, N.D.; Bertin, N.; Pilz, S.; Tomaschitz, A.; Sechi, L.A. Dietary Salt Intake Is a Determinant of Cardiac Changes After Treatment of Primary Aldosteronism: A Prospective Study. Hypertension 2016, 68, 204–212. [Google Scholar] [CrossRef]
- Catena, C.; Verheyen, N.D.; Url-Michitsch, M.; Kraigher-Krainer, E.; Colussi, G.; Pilz, S.; Tomaschitz, A.; Pieske, B.; Sechi, L.A. Association of Post-Saline Load Plasma Aldosterone Levels with Left Ventricular Hypertrophy in Primary Hypertension. Am. J. Hypertens. 2016, 29, 303–310. [Google Scholar] [CrossRef] [Green Version]
- Du Cailar, G.; Fesler, P.; Ribstein, J.; Mimran, A. Dietary sodium, aldosterone, and left ventricular mass changes during long-term inhibition of the renin-angiotensin system. Hypertension 2010, 56, 865–870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, C.Y.; Kawai, Y.; Inaba, S.; Arakawa, K.; Katsuyama, M.; Kajinami, K.; Yasuda, T.; Yabe-Nishimura, C.; Konoshita, T.; Miyamori, I. Synergy of aldosterone and high salt induces vascular smooth muscle hypertrophy through up-regulation of NOX1. J. Steroid Biochem. Mol. Biol. 2008, 111, 29–36. [Google Scholar] [CrossRef]
- Wu, C.; Yosef, N.; Thalhamer, T.; Zhu, C.; Xiao, S.; Kishi, Y.; Regev, A.; Kuchroo, V.K. Induction of pathogenic TH 17 cells by inducible salt-sensing kinase SGK1. Nature 2013, 496, 513–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattson, D.L. Infiltrating immune cells in the kidney in salt-sensitive hypertension and renal injury. Am. J. Physiol. Ren. Physiol. 2014, 307, F499–F508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, X.; Crowley, S.D. Inflammation in Salt-Sensitive Hypertension and Renal Damage. Curr. Hypertens. Rep. 2018, 20, 103. [Google Scholar] [CrossRef] [PubMed]
- Yi, B.; Titze, J.; Rykova, M.; Feuerecker, M.; Vassilieva, G.; Nichiporuk, I.; Schelling, G.; Morukov, B.; Choukèr, A. Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: A longitudinal study. Transl. Res. 2015, 166, 103–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miranda, P.M.; De Palma, G.; Serkis, V.; Lu, J.; Louis-Auguste, M.P.; McCarville, J.L.; Verdu, E.F.; Collins, S.M.; Bercik, P. High salt diet exacerbates colitis in mice by decreasing Lactobacillus levels and butyrate production. Microbiome 2018, 6, 57. [Google Scholar] [CrossRef]
- Wang, C.; Huang, Z.; Yu, K.; Ding, R.; Ye, K.; Dai, C.; Xu, X.; Zhou, G.; Li, C. High-salt diet has a certain impact on protein digestion and gut microbiota: A sequencing and proteome combined study. Front. Microbiol. 2017, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, J.; Luo, H.; Wang, J.; Tang, W.; Lu, J.; Wu, S.; Xiong, Z.; Yang, G.; Chen, Z.; Lan, T.; et al. Enteric dysbiosis-linked gut barrier disruption triggers early renal injury induced by chronic high salt feeding in mice. Exp. Mol. Med. 2017, 49. [Google Scholar] [CrossRef] [Green Version]
- Faraco, G.; Brea, D.; Garcia-Bonilla, L.; Wang, G.; Racchumi, G.; Chang, H.; Buendia, I.; Santisteban, M.M.; Segarra, S.G.; Koizumi, K.; et al. Dietary salt promotes neurovascular and cognitive dysfunction through a gut-initiated TH17 response. Nat. Neurosci. 2018, 21, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Wilck, N.; Matus, M.G.; Kearney, S.M.; Olesen, S.W.; Forslund, K.; Bartolomaeus, H.; Haase, S.; Mahler, A.; Balogh, A.; Marko, L.; et al. Salt-responsive gut commensal modulates TH17 axis and disease. Nature 2017, 551, 585–589. [Google Scholar] [CrossRef]
- Mell, B.; Jala, V.R.; Mathew, A.V.; Byun, J.; Waghulde, H.; Zhang, Y.; Haribabu, B.; Vijay-Kumar, M.; Pennathur, S.; Joe, B. Evidence for a link between gut microbiota and hypertension in the Dahl rat. Physiol. Genom. 2015, 47, 187–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Study | Population | Intervention | Outcome |
|---|---|---|---|
| Sodium intake and blood pressure | |||
| DASH-sodium n = 412 | Pre-HT; Age 47; Male 41%; White 40% | Sodium intakes of 3.3, 2.4 and 1.5 g/day | SBP reduction of 2.1 mmHg (3.3 vs 2.4 g/day) and 4.6 mmHg (2.4 vs 1.5 g/day) (p < 0.001) |
| TOHP-II n = 2382 | Not HT; Age 43.9; Male 65.7%; White 79.3% | Sodium intake reduction to 80 mmol/day | DBP reduction of 0.7 mmHg (p = 0.10) |
| TONE n = 975 | Treated HT; Age 65.8; Male 53%; White 76% | Sodium intake reduction to 80 mmol/day | SBP reduction of 3.4 mmHg (p < 0.001) |
| Sodium intake and cardiovascular outcomes a | |||
| Morgan et al. n = 77 | Untreated HT; Age 57.1; Male 100%; White NA | Sodium intake reduction to 70–100 mmol/day | Relative risk of CV event: 1.16 (0.39–3.45) |
| TOHP-I n = 744 | Not HT; Age 43.4; Male 71.4%; White 77.2% | Sodium intake reduction to 80 mmol/day | Relative risk of CV event: 0.51 (0.29–0.91) |
| TOHP-II n = 2382 | Not HT; Age 43.9; Male 65.7%; White 79.3% | Sodium intake reduction to 80 mmol/day | Relative risk of CV event: 0.88 (0.65–1.20) |
| TONE n = 975 | Treated HT; Age 65.8; Male 53%; White 76% | Sodium intake reduction to 80 mmol/day | Relative risk of CV event: 0.80 (0.53–1.21) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaques, D.A.; Wuerzner, G.; Ponte, B. Sodium Intake as a Cardiovascular Risk Factor: A Narrative Review. Nutrients 2021, 13, 3177. https://doi.org/10.3390/nu13093177
Jaques DA, Wuerzner G, Ponte B. Sodium Intake as a Cardiovascular Risk Factor: A Narrative Review. Nutrients. 2021; 13(9):3177. https://doi.org/10.3390/nu13093177
Chicago/Turabian StyleJaques, David A., Gregoire Wuerzner, and Belen Ponte. 2021. "Sodium Intake as a Cardiovascular Risk Factor: A Narrative Review" Nutrients 13, no. 9: 3177. https://doi.org/10.3390/nu13093177






