Relative Efficacy of Weight Management, Exercise, and Combined Treatment for Muscle Mass and Physical Sarcopenia Indices in Adults with Overweight or Obesity and Osteoarthritis: A Network Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Criteria for Selecting Studies
2.4. Outcome Measures
2.5. Data Extraction
2.6. Assessment of Bias Risks and Methodological Quality of Included Studies
2.7. Data Synthesis and Analysis
3. Results
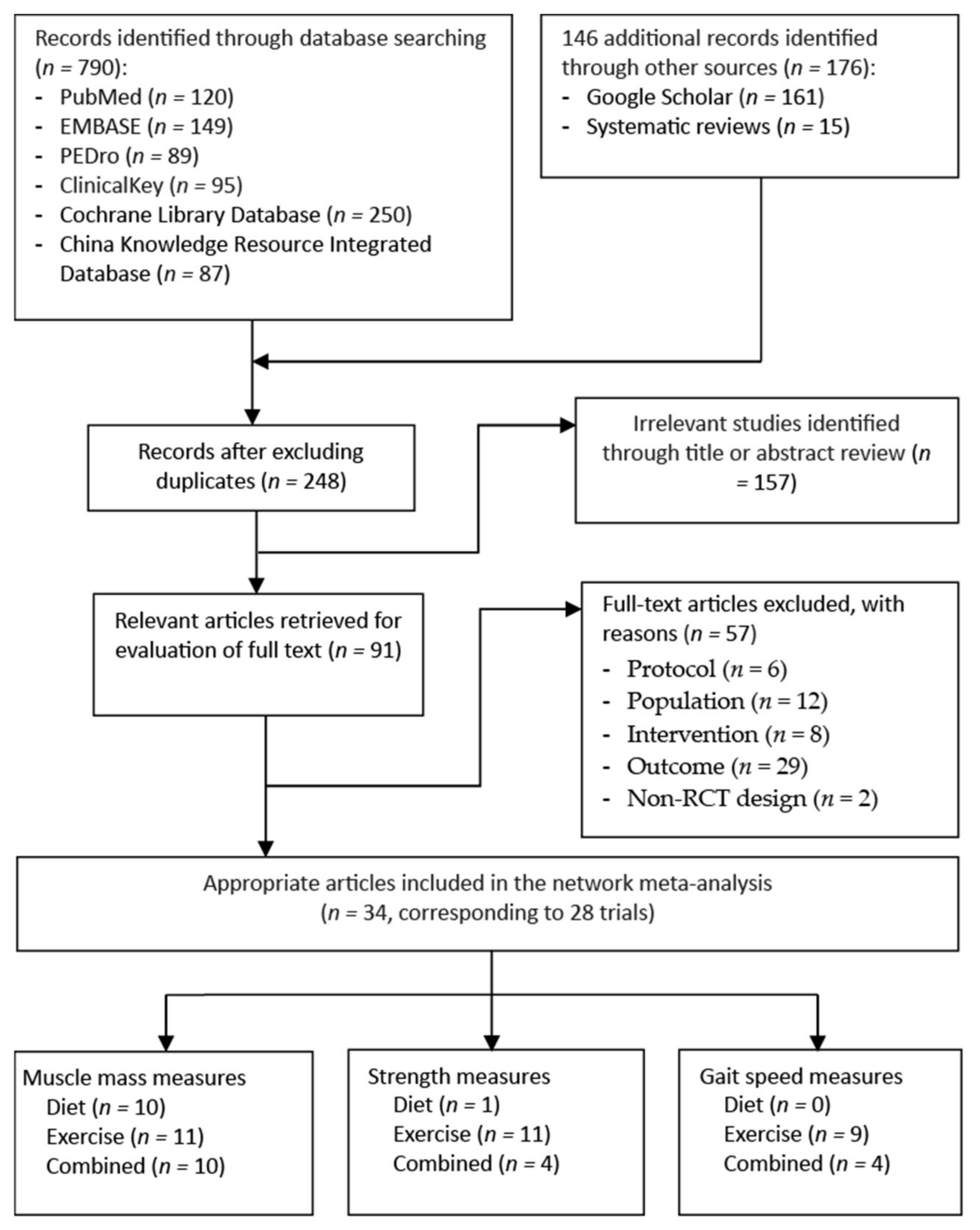
3.1. Trial Selection Flowchart
3.2. Study Characteristics
| Study (Author, y, Ref) | Study Arm 1 | Age (y) 2 | BMI (kg/m2) | Sex (F/M) | N | Involved Joint | Exercise Intervention | Diet Intervention | Measured Time Point (weeks) | Main Outcome Measure | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type (COM%) | Frequency × Duration | Type (COM%) | WL Target (% or kg) 6 | |||||||||
| Diet intervention alone | ||||||||||||
| Christensen, | D | 60.5 ± 11.6 | 36.3 ± 5.6 | 35/5 | 40 | Knee | None | None | MR | None | Baseline | FFM |
| 2005 [61] | UC | 64.6 ± 10.4 | 35.5 ± 4.6 | 36/4 | 40 | (6 meals/d), | Posttest: 8 | |||||
| DIA, CBT | ||||||||||||
| −93.2 | ||||||||||||
| Christensen, | D1, Regular MR | 63.7 ± 6.5 | 32.6 ± 3.7 | 62/15 | 77 | Knee | None | None | MR | None | Baseline | LBM |
| 2017 [60] | D2, Intermittent | 63.9 ± 6.3 | 34.0 ± 5.3 | 65/11 | 76 | (1–3 meals/d), | Midtest: 52 | |||||
| MR | DIA | Posttest: 156 | ||||||||||
| −71.2 | ||||||||||||
| López- | D1, Uni-MR | 60.9 ± 11.2 | 38.9 ± 5.1 | 35/17 | 52 | Hip | None | None | MR (1 or | ↓ 5 kg | Baseline | FFM |
| Gómez, | D2, Multi-MR | 61.4 ± 11.0 | 40.2 ± 5.3 | 46/14 | 60 | Knee | 2 meals/d) | Posttest: 12 | ||||
| 2020 [67] | (NR) | |||||||||||
| Exercise intervention alone | ||||||||||||
| Gill, | Water-based ET | 69.2 ± 10.5 | 41.4 ± 3.9 | 28/14 | 42 | Hip | AQET, | 2 d/wk × 6 wk | None | None | Baseline | GS |
| 2009 [64] | Land-based ET | 71.6 ± 8.9 | 39.8 ± 13.1 | 23/17 | 40 | Knee | RET | (12 sessions) | Posttest: 7 | |||
| (81.7–87.5) | Follow-up: 15 | |||||||||||
| Kuptniratsaikul, | Water-based ET | 62.1 ± 6.4 | 27.9 ± 1.5 | 38/2 | 40 | Knee | AQET | 3 d/wk × 4 wk | None | None | Baseline | Qd strength |
| 2019 [65] | Land-based ET | 61.7 ± 6.9 | 27.6 ± 1.7 | 37/3 | 40 | IMET | (12 sessions) | Posttest: 4 | ||||
| (76–91.7) | ||||||||||||
| Lim, | Water-based ET | 65.7 ± 8.9 | 27.9 ± 1.5 | 23/3 | 26 | Knee | AQET; | 3 d/wk × 8 wk | None | None | Baseline | LBM |
| 2010 [66] | Land-based ET | 67.7 ± 7.7 | 27.6 ± 1.7 | 21/4 | 25 | RET; | (24 sessions) | Posttest: 8 | FFM | |||
| Home-based ET | 63.3 ± 5.3 | 27.7 ± 2.0 | 21/3 | 24 | (NR) | Qd strength | ||||||
| Mahmoud, | ET | 54.6 ± 8.6 | 35.0 ± 4.1 | 0/32 | 32 | Knee | IM-ET | 3 d/wk × 12 wk | None | None | Baseline | MT |
| 2017 [69] | UC 3 | 53.2 ± 9.6 | 34.8 ± 4.2 | 0/12 | 12 | (NR) | (36 sessions) | Posttest: 12 | Qd strength | |||
| Mangani, | AET | 68.7 ± 5.6 5 | 33.3 ± 5.0 5 | 146/51 5 | 57 | Knee | AET | 3 d/wk × 72 wk | None | None | Baseline | GS |
| 2006 [70] | RET | 64 | RET | (216 sessions) | Mid-test: 12, 36 | |||||||
| UC | 76 | (50.5–81.4) | Posttest: 72 | |||||||||
| Matsuse, | NMES + ET | 58.8 ± 11.8 | 37.5 ± 4.5 | 10/0 | 10 | Knee | AET | 2 d/wk × 12 wk | None | None | Baseline | GS |
| 2020 [71] | ET | 59.7 ± 6.1 | 36.1 ± 3.4 | 10/0 | 10 | (NR) | (24 sessions) | Posttest: 12 | Qd strength | |||
| Rabe, | NMES | 67.3 ± 8.5 | 27.5 ± 6.1 | 17/0 | 17 | Knee | RET | 2 d/wk × 12 wk | None | None | Baseline | GS |
| 2018 [77] | ET | 65.9 ± 9.4 | 27.5 ± 4.1 | 18/0 | 18 | (NR) | (24 sessions) | Posttest: 12 | Qd strength | |||
| Exercise intervention alone | ||||||||||||
| Rosemffet, | NMES + ET | 62.4 ± 8.7 4,5 | 31.6 ± 5.3 4 | 20/6 5 | 8 | Knee | MET | 3 d/wk × 8 wk | None | None | Baseline | Qd strength |
| 2004 [79] | NMES | 34.2 ± 6.7 4 | 8 | −70.3 | (24 sessions) | Posttest: 8 | ||||||
| ET | 29.1 ± 3.3 4 | 10 | ||||||||||
| Segal, | BFR-ET | 58.4 ± 8.7 | 31.3 ± 5.3 | 0/19 | 19 | Knee | RET | 3 d/wk × 4 wk | None | None | Baseline | Leg press 1-RM |
| 2015a [80] | ET | 56.1 ± 7.7 | 30.4 ± 4.2 | 0/22 | 22 | −100 | (12 sessions) | Posttest: 4 | ||||
| Segal, | BFR-ET | 56.1 ± 5.9 | 28.7 ± 4.4 | 19/0 | 19 | Knee | RET | 3 d/wk × 4 wk | None | None | Baseline | Qd volume |
| 2015b [81] | ET | 54.6 ± 6.9 | 32.5 ± 5.2 | 21/0 | 21 | −97.2 | (12 sessions) | Posttest: 4 | Leg press 1-RM | |||
| Swank, | ET | 63.1 ± 7.3 | 35.9 ± 8.5 | 24/12 | 36 | Knee | RET | 3 d/wk × 4–8 wk | None | None | Baseline | Qd strength |
| 2011 [84] | UC 3 | 62.6 ± 7.6 | 32.9 ± 5.7 | 22/13 | 35 | −90 | (12–24 sessions) | Posttest: 8 | ||||
| Tak, | ET | 67.4 ± 7.6 | 26.4 ± 3.0 | 29/16 | 45 | Hip | MET | 7 d/wk × 8 wk | None | None | Baseline | GS |
| 2005 [85] | UC 3 | 68.9 ± 7.6 | 26.6 ± 4.3 | 35/14 | 49 | −77 | (56 sessions) | Posttest: 8 | ||||
| Follow-up: 20 | ||||||||||||
| Talbot, | ET | 69.6 ± 6.7 | 31.0 ± 5.9 | 13/4 | 17 | Knee | AET | 3 d/wk × 12 wk | None | None | Baseline | GS |
| 2003a [86] | UC 3 | 70.8 ± 4.7 | 32.6 ± 6.9 | 13/4 | 17 | −76 | (36 sessions) | Posttest: 12 | Qd strength | |||
| Follow-up: 24 | ||||||||||||
| Talbot, | NMES | 70.3 ± 5.6 | 29.5 ± 4.1 | 15/3 | 18 | Knee | IMET | 3 d/wk × 12 wk | None | None | Baseline | GS |
| 2003b [87] | UC 3 | 70.8 ± 4.9 | 31.6 ± 5.9 | 4/12 | 16 | −85 | (36 sessions) | Posttest: 12 | Qd strength | |||
| Follow-up: 24 | ||||||||||||
| Wallis, | ET | 68.0 ± 8.0 | 34.0 ± 5.2 | 9/14 | 23 | Knee | AET | 7 d/wk × 12 wk | None | None | Baseline | GS |
| 2017 [90] | UC 3 | 67.0 ± 7.0 | 34.0 ± 7.4 | 11/12 | 23 | −70 | (84 sessions) | Posttest: 13 | ||||
| Combined treatments | ||||||||||||
| Beavers, | D + ET | 65.5 ± 6.0 | 33.5 ± 3.7 | 108/43 | 151 | Knee | MET | 3 d/wk × 72 wk | MR | ↓ ≥10% | Baseline | FFM 4 |
| 2015 [58] | ET | 65.5 ± 6.4 | 33.5 ± 3.7 | 108/42 | 150 | (58–70) | (216 sessions) | (2 meals/d), | Midtest: 24 | |||
| D | 65.8 ± 6.2 | 33.7 ± 3.8 | 105/44 | 149 | DIA, CBT | Posttest: 72 | ||||||
| −63 | ||||||||||||
| Christensen, | D + ET | 62.9 ± 5.8 | 36.5 ± 4.4 | 52/12 | 64 | MET | 3 d/wk × 52 wk | MR | ↓ ≥10% | Baseline | LBM; | |
| 2013 [59]; | D | 63.0 ± 6.5 | 37.9 ± 5.3 | 52/12 | 64 | −59.1 | (156 sessions) | (1 meal/d), | Posttest: 52 | |||
| 2015 [62] | UC | 61.7 ± 6.8 | 37.6 ± 4.5 | 51/13 | 64 | DIA, CBT | ||||||
| −61.5 | ||||||||||||
| Combined treatments | ||||||||||||
| Ghroubi, | D + ET | 41.4 ± 3.9 | 37.5 ± 3.7 | NR | 12 | Knee | MET | 3 d/wk × 8 wk | MR | NR | Baseline | LBM |
| 2008 [63] | ET | 43.8 ± 13.1 | 37.1 ± 5.7 | 10 | (NR) | (24 sessions) | (3 meals/d), | Posttest: 8 | ||||
| D | 41.5 ± 11.7 | 38.7 ± 6.1 | 12 | (NR) | ||||||||
| UC 3 | 42.4 ± 9.8 | 39.2 ± 3.7 | 11 | |||||||||
| Magrans- | D + ET | 54.0 ± 9.0 5 | 33.3 ± 5.0 5 | 14/0 | 14 | Knee | RET | 3 d/wk × 14 wk | DIA | ↓ 3–5 kg | Baseline | FFM |
| Courtney, | ET | 16/0 | 16 | (NR) | (42 sessions) | (NR) | Midtest: 10 | Bench- | ||||
| 2011 [68] | Posttest: 14 | press 1-RM | ||||||||||
| McLeod, | D + ET | 66.5 ± 4.8 | 33.7 ± 7.6 | 64/8 | 72 | Hip | MET | 3 d/wk × 8 wk | DIA, CBT | ↓ 5% | Baseline | LBM |
| 2020 [72] | ET | 67.2 ± 5.7 | 33.9 ± 7.3 | 73/10 | 83 | Knee | (NR) | (24 sessions) | (NR) | Posttest: 8 | FFM 4 | |
| Messier, | D + ET | 67.0 ± 4.0 | 35.0 ± 5.0 | 10/3 | 13 | Knee | MET | 3 d/wk × 24 wk | DIA, CBT | ↓ ≥6.8 kg | Baseline | GS |
| 2000 [73] | ET | 69.0 ± 5.0 | 38.0 ± 6.0 | 7/4 | 11 | −94.7 | (72 sessions) | −82.6 | Midtest: 12 | Qd strength | ||
| Posttest: 24 | ||||||||||||
| Messier, | D + ET | 65.0 ± 6.0 | 33.6 ± 3.7 | 109/43 | 152 | Knee | MET | 3 d/wk × 72 wk | MR | ↓ 10–15% | Baseline | LBM |
| 2013 [74] | ET | 66.0 ± 6.0 | 33.5 ± 3.7 | 108/42 | 150 | (54–70) | (216 sessions) | (2 meals/d), | Midtest: 24 | |||
| D | 66.0 ± 6.0 | 33.7 ± 3.8 | 108/44 | 152 | DIA, CBT | Posttest: 72 | ||||||
| (61.0–63.0) | ||||||||||||
| Miller, | D + ET | 69.8 ± 8.2 | 34.9 ± 6.5 | 43/24 | 67 | Knee | MET | 3 d/wk × 24 wk | MR, | ↓ 10% | Baseline | FFM |
| 2006 [76] | UC 3 | 69.5 ± 8.2 | 34.4 ± 5.7 | 38/29 | 67 | (72–83) | (72 sessions) | (2 meals/d) | Posttest: 24 | |||
| DIA, CBT | ||||||||||||
| −75 | ||||||||||||
| Miller, | D + ET | 69.3 ± 6.6 | 35.7 ± 6.6 | 14/12 | 26 | Knee | MET | 3 d/wk × 24 wk | MR | ↓ 10% | Baseline | FFM |
| 2012 [75] | UC 3 | 69.3 ± 6.5 | 34.9 ± 4.0 | 13/12 | 25 | −76.3 | (72 sessions) | (2 meals/d), | Posttest: 24 | |||
| DIA, CBT | ||||||||||||
| −74 | ||||||||||||
| Robbins, | D + ET | 62.5 ± 7.4 | 34.6 ± 6.9 4 | 57/30 | 87 | Knee | MET | 3 d/wk × 18 wk | MR | NR | Baseline | GS |
| 2020 [78] | UC 3 | 63.8 ± 7.3 | 36.3 ± 7.5 4 | 52/32 | 84 | (89/73) | (54 sessions) | (2 meals/d), | Midtest: 20 | Qd strength | ||
| −94 | Posttest: 32 | |||||||||||
| Skou, | D + ET | 64.8 ± 8.7 | 30.6 ± 5.6 | 26/24 | 50 | Knee | MET | 2 d/wk × 12 wk | DIA | ↓ ≥5% | Baseline | GS |
| 2015 [82] | UC 3 | 67.1 ± 9.1 | 29.4 ± 5.2 | 25/25 | 50 | −65.8 | (24 sessions) | −67.5 | Posttest: 12 | |||
| Follow-up: 24, 52 | ||||||||||||
| Combined treatments | ||||||||||||
| Skou, | D + ET | 65.9 ± 8.7 | 31.3 ± 5.7 | 56/44 | 100 | Knee | MET | 2 d/wk × 12 wk | DIA | ↓ ≥5% | Baseline | GS |
| 2018 [83] | UC 3 | 67.1 ± 9.1 | 29.4 ± 5.2 | 25/25 | 50 | (NR) | (24 sessions) | (NR) | Posttest: 12 | |||
| Follow-up: 24, 104 | ||||||||||||
| Toda, | D + ET | 56.5 ± 11.1 | 28.1 ± 1.1 | 11/0 | 11 | Knee | AET | 7 d/wk × 8 wk | MR | NR | Baseline | LBM |
| 2000 [89] | UC 3 | 61.9 ± 5.5 | 28.8 ± 3.3 | 31/0 | 31 | RET | (56 sessions) | (2 meals/d), | Posttest: 8 | |||
| (NR) | (NR) | |||||||||||
| Toda, | D + ET | 63.2 ± 7.9 | 27.4 ± 3.1 4 | 63/0 | 63 | Knee | AET | 7 d/wk × 8 wk | MR | NR | Baseline | LLM |
| 2001 [88] | ET | 61.0 ± 11.7 | 26.6 ± 4.0 4 | 84/0 | 84 | RET | (56 sessions) | (2 meals/d), | Posttest: 8 | |||
| D | 60.1 ± 13.5 | 27.9 ± 4.7 4 | 29/0 | 29 | (NR) | (NR) | ||||||
| UC 3 | 63.1 ± 9.3 | 26.4 ± 4.1 4 | 52/0 | 52 | ||||||||
| Wang, | D + ET | 69.9 ± 5.7 | 35.0 ± 5.8 | 25/15 | 40 | Knee | MET | 3 d/wk × 24 wk | MR | ↓ 10% | Baseline | LBM |
| 2007 [91] | UC 3 | 68.8 ± 5.7 | 34.7 ± 4.3 | 21/12 | 33 | −77.5 | (72 sessions) | (2 meals/d), | Posttest: 24 | Qd strength | ||
| DIA, CBT | ||||||||||||
| −75 | ||||||||||||
3.3. Dietary Intervention Characteristics
3.4. Exercise Training Protocol
3.5. Risk of Bias in Included Studies
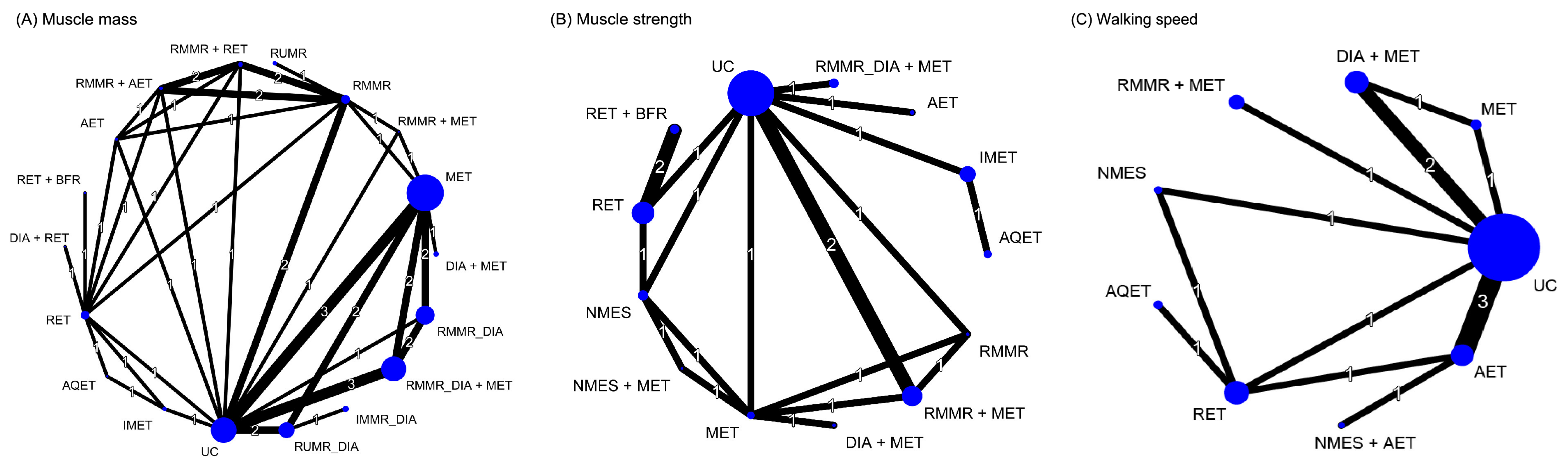
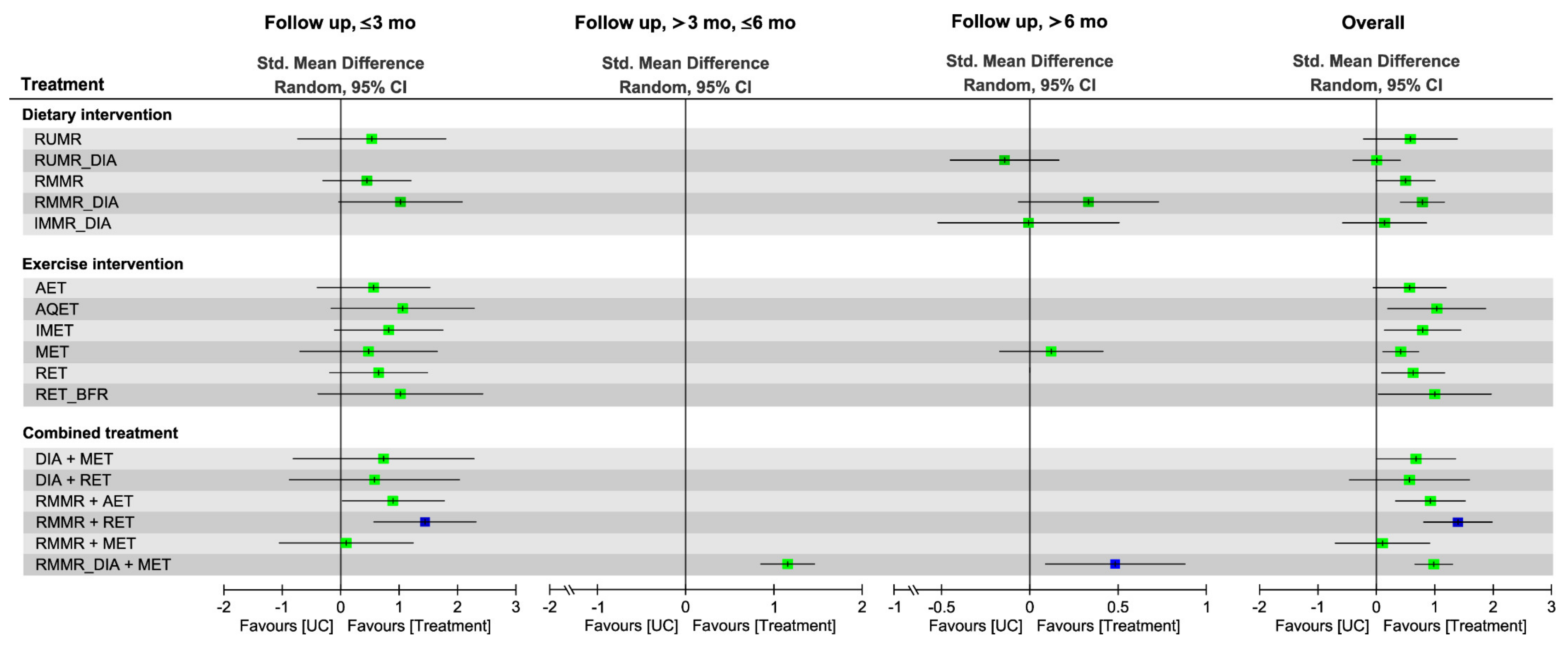
3.6. Effectiveness of Treatment for Muscle Mass Assessed in NMA
3.6.1. Pairwise Meta-Analysis
3.6.2. Global Effects in NMA
3.6.3. Subgroup Analysis of Follow-Up Duration
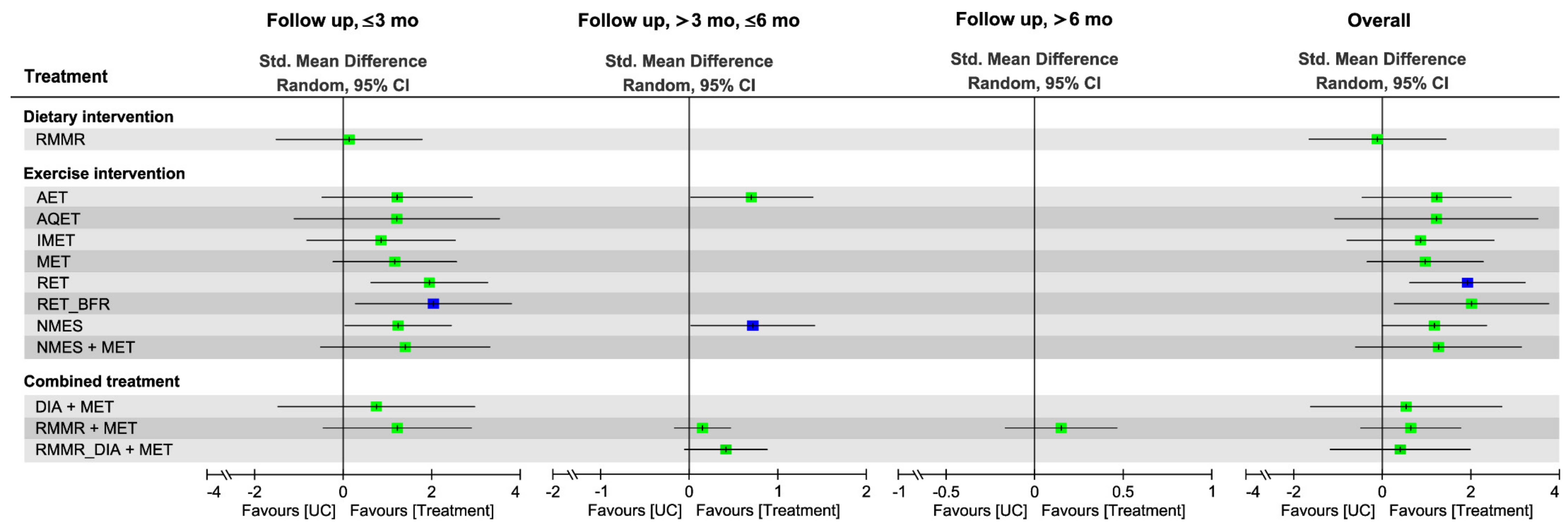
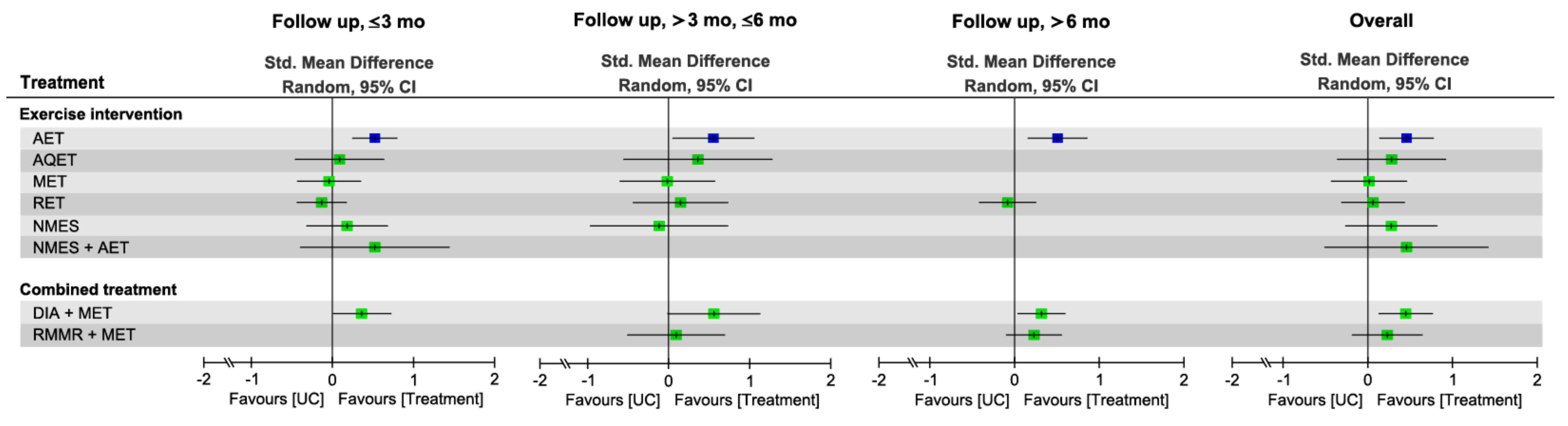
3.7. Effectiveness of Treatment for Muscle Strength
3.7.1. Pairwise Meta-Analysis
3.7.2. Global Effects of NMA
3.7.3. Subgroup Analysis of Follow-Up Duration
3.8. Effectiveness of Treatment for Walking Speed
3.8.1. Pairwise Meta-Analysis
3.8.2. Global Effects of NMA
3.8.3. Subgroup Analysis of Follow-Up Duration
3.9. Network Meta-Regression Results for Moderators of Treatment Efficacy
3.10. Side Effects and Compliance
3.11. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lewis, R.; Gómez Álvarez, C.B.; Rayman, M.; Lanham-New, S.; Woolf, A.; Mobasheri, A. Strategies for optimising musculoskeletal health in the 21(st) century. BMC Musculoskelet. Disord. 2019, 20, 164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunter, D.J.; Bierma-Zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. [Google Scholar] [CrossRef]
- Alshami, A.M.; Alhassany, H.A. Girth, strength, and flexibility of the calf muscle in patients with knee osteoarthritis: A case-control study. J. Taibah Univ. Med. Sci. 2020, 15, 197–202. [Google Scholar] [CrossRef]
- Zacharias, A.; Green, R.A.; Semciw, A.; English, D.J.; Kapakoulakis, T.; Pizzari, T. Atrophy of hip abductor muscles is related to clinical severity in a hip osteoarthritis population. Clin. Anat. 2018, 31, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Loureiro, A.; Constantinou, M.; Diamond, L.E.; Beck, B.; Barrett, R. Individuals with mild-to-moderate hip osteoarthritis have lower limb muscle strength and volume deficits. BMC Musculoskelet Disord. 2018, 19, 303. [Google Scholar] [CrossRef] [PubMed]
- Coriolano, K.; Aiken, A.; Pukall, C.; Harrison, M. Changes in self-reported disability after performance-based tests in obese and non-obese individuals diagnosed with osteoarthritis of the knee. Disabil. Rehabil. 2015, 37, 1152–1161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batsis, J.A.; Zbehlik, A.J.; Barre, L.K.; Bynum, J.P.; Pidgeon, D.; Bartels, S.J. Impact of obesity on disability, function, and physical activity: Data from the Osteoarthritis Initiative. Scand. J. Rheumatol. 2015, 44, 495–502. [Google Scholar] [CrossRef]
- Jeon, H.; Lee, S.U.; Lim, J.Y.; Chung, S.G.; Lee, S.J.; Lee, S.Y. Low skeletal muscle mass and radiographic osteoarthritis in knee, hip, and lumbar spine: A cross-sectional study. Aging Clin. Exp. Res. 2019, 31, 1557–1562. [Google Scholar] [CrossRef]
- Zhang, X.; Pan, X.; Deng, L.; Fu, W. Relationship between Knee Muscle Strength and Fat/Muscle Mass in Elderly Women with Knee Osteoarthritis Based on Dual-Energy X-Ray Absorptiometry. Int. J. Environ. Res. Public Health 2020, 17, 573. [Google Scholar] [CrossRef] [Green Version]
- Park, H.M.; Kim, H.J.; Lee, B.; Kwon, M.; Jung, S.M.; Lee, S.W.; Park, Y.B.; Song, J.J. Decreased muscle mass is independently associated with knee pain in female patients with radiographically mild osteoarthritis: A nationwide cross-sectional study (KNHANES 2010-2011). Clin. Rheumatol. 2018, 37, 1333–1340. [Google Scholar] [CrossRef]
- Cheon, Y.H.; Kim, H.O.; Suh, Y.S.; Kim, M.G.; Yoo, W.H.; Kim, R.B.; Yang, H.S.; Lee, S.I.; Park, K.S. Relationship between decreased lower extremity muscle mass and knee pain severity in both the general population and patients with knee osteoarthritis: Findings from the KNHANES V 1-2. PLoS ONE 2017, 12, e0173036. [Google Scholar] [CrossRef]
- Pickering, M.E.; Chapurlat, R. Where Two Common Conditions of Aging Meet: Osteoarthritis and Sarcopenia. Calcif. Tissue Int. 2020, 107, 203–211. [Google Scholar] [CrossRef]
- Shorter, E.; Sannicandro, A.J.; Poulet, B.; Goljanek-Whysall, K. Skeletal Muscle Wasting and Its Relationship With Osteoarthritis: A Mini-Review of Mechanisms and Current Interventions. Curr. Rheumatol. Rep. 2019, 21, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barazzoni, R.; Bischoff, S.C.; Boirie, Y.; Busetto, L.; Cederholm, T.; Dicker, D.; Toplak, H.; Van Gossum, A.; Yumuk, V.; Vettor, R. Sarcopenic obesity: Time to meet the challenge. Clin. Nutr. 2018, 37, 1787–1793. [Google Scholar] [CrossRef]
- Woo, J. Obesity in older persons. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 5–10. [Google Scholar] [CrossRef]
- Godziuk, K.; Prado, C.M.; Woodhouse, L.J.; Forhan, M. The impact of sarcopenic obesity on knee and hip osteoarthritis: A scoping review. BMC Musculoskelet Disord. 2018, 19, 271. [Google Scholar] [CrossRef]
- Ackerman, I.N.; Osborne, R.H. Obesity and increased burden of hip and knee joint disease in Australia: Results from a national survey. BMC Musculoskelet Disord. 2012, 13, 254. [Google Scholar] [CrossRef] [Green Version]
- Misra, D.; Fielding, R.A.; Felson, D.T.; Niu, J.; Brown, C.; Nevitt, M.; Lewis, C.E.; Torner, J.; Neogi, T. Risk of Knee Osteoarthritis With Obesity, Sarcopenic Obesity, and Sarcopenia. Arthritis Rheumatol. 2019, 71, 232–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ambrose, N.L.; Keogan, F.; O’Callaghan, J.P.; O’Connell, P.G. Obesity and disability in the symptomatic Irish knee osteoarthritis population. Ir. J. Med. Sci. 2010, 179, 265–268. [Google Scholar] [CrossRef]
- Vlietstra, L.; Stebbings, S.; Meredith-Jones, K.; Abbott, J.H.; Treharne, G.J.; Waters, D.L. Sarcopenia in osteoarthritis and rheumatoid arthritis: The association with self-reported fatigue, physical function and obesity. PLoS ONE 2019, 14, e0217462. [Google Scholar] [CrossRef] [Green Version]
- Skou, S.T.; Roos, E.M. Physical therapy for patients with knee and hip osteoarthritis: Supervised, active treatment is current best practice. Clin. Exp. Rheumatol. 2019, 37 (Suppl. 120), 112–117. [Google Scholar]
- Liao, C.D.; Chen, H.C.; Kuo, Y.C.; Tsauo, J.Y.; Huang, S.W.; Liou, T.H. Effects of muscle strength training on muscle mass gain and hypertrophy in older adults with osteoarthritis: A systematic review and meta-analysis. Arthritis Care Res. 2020, 72, 1703–1718. [Google Scholar] [CrossRef]
- Goh, S.L.; Persson, M.S.M.; Stocks, J.; Hou, Y.; Lin, J.; Hall, M.C.; Doherty, M.; Zhang, W. Efficacy and potential determinants of exercise therapy in knee and hip osteoarthritis: A systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2019, 62, 356–365. [Google Scholar] [CrossRef]
- Robson, E.K.; Hodder, R.K.; Kamper, S.J.; O’Brien, K.M.; Williams, A.; Lee, H.; Wolfenden, L.; Yoong, S.; Wiggers, J.; Barnett, C.; et al. Effectiveness of Weight Loss Interventions for Reducing Pain and Disability in People With Common Musculoskeletal Disorders: A Systematic Review With Meta-Analysis. J. Orthop. Sports Phys. Ther. 2020, 50, 319–333. [Google Scholar] [CrossRef]
- Chu, I.J.H.; Lim, A.Y.T.; Ng, C.L.W. Effects of meaningful weight loss beyond symptomatic relief in adults with knee osteoarthritis and obesity: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 1597–1607. [Google Scholar] [CrossRef] [PubMed]
- Christensen, R.; Bartels, E.M.; Astrup, A.; Bliddal, H. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: A systematic review and meta-analysis. Ann. Rheum. Dis. 2007, 66, 433–439. [Google Scholar] [CrossRef]
- Weinheimer, E.M.; Sands, L.P.; Campbell, W.W. A systematic review of the separate and combined effects of energy restriction and exercise on fat-free mass in middle-aged and older adults: Implications for sarcopenic obesity. Nutr. Rev. 2010, 68, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.C.; Koceja, D.M.; Hamilton, E.J. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Int. J. Obes. Relat. Metab. Disord. 1997, 21, 941–947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henriksen, M.; Christensen, R.; Danneskiold-Samsøe, B.; Bliddal, H. Changes in lower extremity muscle mass and muscle strength after weight loss in obese patients with knee osteoarthritis: A prospective cohort study. Arthritis Rheum. 2012, 64, 438–442. [Google Scholar] [CrossRef]
- Ariani, A.; Manara, M.; Fioravanti, A.; Iannone, F.; Salaffi, F.; Ughi, N.; Prevete, I.; Bortoluzzi, A.; Parisi, S.; Scire, C.A. The Italian Society for Rheumatology clinical practice guidelines for the diagnosis and management of knee, hip and hand osteoarthritis. Reumatismo 2019, 71, 5–21. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [Green Version]
- Bennell, K.L.; Wrigley, T.V.; Hunt, M.A.; Lim, B.W.; Hinman, R.S. Update on the role of muscle in the genesis and management of knee osteoarthritis. Rheum. Dis. Clin. N. Am. 2013, 39, 145–176. [Google Scholar] [CrossRef] [PubMed]
- Bierma-Zeinstra, S.; van Middelkoop, M.; Runhaar, J.; Schiphof, D. Nonpharmacological and nonsurgical approaches in OA. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101564. [Google Scholar] [CrossRef]
- Kiadaliri, A.A.; Lohmander, L.S.; Moradi-Lakeh, M.; Petersson, I.F.; Englund, M. High and rising burden of hip and knee osteoarthritis in the Nordic region, 1990–2015. Acta Orthop. 2018, 89, 177–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hall, M.; Castelein, B.; Wittoek, R.; Calders, P.; Van Ginckel, A. Diet-induced weight loss alone or combined with exercise in overweight or obese people with knee osteoarthritis: A systematic review and meta-analysis. Semin. Arthritis Rheum. 2019, 48, 765–777. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [Green Version]
- Hutton, B.; Catalá-López, F.; Moher, D. The PRISMA statement extension for systematic reviews incorporating network meta-analysis: PRISMA-NMA. Med. Clínica 2016, 147, 262–266. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Chapter 3: Defining the criteria for including studies and how they will be grouped for the synthesis. In Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2 (Updated February 2021); Cochrane: London, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 5 June 2021).
- Wu, C.H.; Chen, K.T.; Hou, M.T.; Chang, Y.F.; Chang, C.S.; Liu, P.Y.; Wu, S.J.; Chiu, C.J.; Jou, I.M.; Chen, C.Y. Prevalence and associated factors of sarcopenia and severe sarcopenia in older Taiwanese living in rural community: The Tianliao Old People study 04. Geriatr. Gerontol. Int. 2014, 14 (Suppl. 1), 69–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tooth, L.; Bennett, S.; McCluskey, A.; Hoffmann, T.; McKenna, K.; Lovarini, M. Appraising the quality of randomized controlled trials: Inter-rater reliability for the OTseeker evidence database. J. Eval. Clin. Pract. 2005, 11, 547–555. [Google Scholar] [CrossRef]
- Foley, N.C.; Bhogal, S.K.; Teasell, R.W.; Bureau, Y.; Speechley, M.R. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys. Ther. 2006, 86, 817–824. [Google Scholar] [CrossRef]
- Briani, R.V.; Ferreira, A.S.; Pazzinatto, M.F.; Pappas, E.; De Oliveira Silva, D.; Azevedo, F.M. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br. J. Sports Med. 2018, 52, 1031–1038. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Li, T.; Deeks, J.J. Chapter 6: Choosing effect measures and computing estimates of effect. In Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2 (Updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 5 June 2021).
- Rosenthal, R. Meta-Analytic Procedures for Social Research; Rosenthal, R., Ed.; Sage Publications: Newbury Park, CA, USA, 1993. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NY, USA, 1988. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis in R: A Hands-on Guide; PROTECT Lab: Erlangen, Germany, 2019. [Google Scholar]
- Shim, S.R.; Kim, S.-J.; Lee, J.; Rücker, G. Network meta-analysis: Application and practice using R software. Epidemiol. Health 2019, 41, e201901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Jackson, D.; Barrett, J.K.; Lu, G.; Ades, A.E.; White, I.R. Consistency and inconsistency in network meta-analysis: Concepts and models for multi-arm studies. Res. Synth. Methods 2012, 3, 98–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, D.; Barrett, J.K.; Rice, S.; White, I.R.; Higgins, J.P. A design-by-treatment interaction model for network meta-analysis with random inconsistency effects. Stat. Med. 2014, 33, 3639–3654. [Google Scholar] [CrossRef] [Green Version]
- Rücker, G.; Schwarzer, G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 2015, 15, 58. [Google Scholar] [CrossRef] [Green Version]
- Mbuagbaw, L.; Rochwerg, B.; Jaeschke, R.; Heels-Andsell, D.; Alhazzani, W.; Thabane, L.; Guyatt, G.H. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst. Rev. 2017, 6, 79. [Google Scholar] [CrossRef] [Green Version]
- Beaudreuil, J.; Coudreuse, J.M.; Guyen, N.G.; Deat, P.; Chabaud, A.; Pereira, B.; Lorenzo, A.; Sailhan, F.; Rannou, F.; Coudeyre, E. An algorithm to improve knee orthosis prescription for osteoarthritis patients. Ann. Phys. Rehabil. Med. 2016, 59, e156. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Beavers, K.M.; Beavers, D.P.; Newman, J.J.; Anderson, A.M.; Loeser, R.F., Jr.; Nicklas, B.J.; Lyles, M.F.; Miller, G.D.; Mihalko, S.L.; Messier, S.P. Effects of total and regional fat loss on plasma CRP and IL-6 in overweight and obese, older adults with knee osteoarthritis. Osteoarthr. Cartil. 2015, 23, 249–256. [Google Scholar] [CrossRef] [Green Version]
- Christensen, P.; Frederiksen, R.; Bliddal, H.; Riecke, B.F.; Bartels, E.M.; Henriksen, M.; Juul, S.R.T.; Gudbergsen, H.; Winther, K.; Astrup, A.; et al. Comparison of three weight maintenance programs on cardiovascular risk, bone and vitamins in sedentary older adults. Obesity 2013, 21, 1982–1990. [Google Scholar] [CrossRef]
- Christensen, P.; Henriksen, M.; Bartels, E.M.; Leeds, A.R.; Meinert Larsen, T.; Gudbergsen, H.; Riecke, B.F.; Astrup, A.; Heitmann, B.L.; Boesen, M.; et al. Long-term weight-loss maintenance in obese patients with knee osteoarthritis: A randomized trial. Am. J. Clin. Nutr. 2017, 106, 755–763. [Google Scholar] [CrossRef] [Green Version]
- Christensen, R.; Astrup, A.; Bliddal, H. Weight loss: The treatment of choice for knee osteoarthritis? A randomized trial. Osteoarthr. Cartil. 2005, 13, 20–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, R.; Henriksen, M.; Leeds, A.R.; Gudbergsen, H.; Christensen, P.; Sorensen, T.J.; Bartels, E.M.; Riecke, B.F.; Aaboe, J.; Frederiksen, R.; et al. Effect of weight maintenance on symptoms of knee osteoarthritis in obese patients: A twelve-month randomized controlled trial. Arthritis Care Res. 2015, 67, 640–650. [Google Scholar] [CrossRef]
- Ghroubi, S.; Elleuch, H.; Kaffel, N.; Echikh, T.; Abid, M.; Elleuch, M.H. Contribution of exercise and diet in the management of knee osteoarthritis in the obese. Ann. Readapt. Med. Phys. 2008, 51, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.D.; McBurney, H.; Schulz, D.L. Land-based versus pool-based exercise for people awaiting joint replacement surgery of the hip or knee: Results of a randomized controlled trial. Arch. Phys. Med. Rehabil. 2009, 90, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Kuptniratsaikul, V.; Kittichaikarn, C.; Suntornpiyapan, P.; Kovintaset, K.; Inthibal, S. Is four-week underwater treadmill exercise regimen compared to home exercise efficacious for pain relief and functional improvement in obese patients with knee osteoarthritis? A randomized controlled trial. Clin. Rehabil. 2019, 33, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.Y.; Tchai, E.; Jang, S.N. Effectiveness of aquatic exercise for obese patients with knee osteoarthritis: A randomized controlled trial. Pm&r 2010, 2, 723–731. [Google Scholar]
- López-Gómez, J.J.; Izaola-Jauregui, O.; Primo-Martín, D.; Torres-Torres, B.; Gómez-Hoyos, E.; Ortolá-Buigues, A.; Martín-Ferrero, M.A.; De Luis-Román, D.A. Effect of Two Meal Replacement strategies on Cardiovascular Risk Parameters in Advanced Age Patients with Obesity and Osteoarthritis. Nutrients 2020, 12, 976. [Google Scholar] [CrossRef] [Green Version]
- Magrans-Courtney, T.; Wilborn, C.; Rasmussen, C.; Ferreira, M.; Greenwood, L.; Campbell, B.; Kerksick, C.M.; Nassar, E.; Li, R.; Iosia, M.; et al. Effects of diet type and supplementation of glucosamine, chondroitin, and MSM on body composition, functional status, and markers of health in women with knee osteoarthritis initiating a resistance-based exercise and weight loss program. J. Int. Soc. Sports Nutr. 2011, 8, 8. [Google Scholar] [CrossRef] [Green Version]
- Mahmoud, W.S.; Elnaggar, R.K.; Ahmed, A.S. Influence of Isometric Exercise Training on Quadriceps Muscle Architecture and Strength in Obese Subjects with Knee Osteoarthritis. Int. J. Med. Res. Health Sci. 2017, 6, 1–9. [Google Scholar]
- Mangani, I.; Cesari, M.; Kritchevsky, S.B.; Maraldi, C.; Carter, C.S.; Atkinson, H.H.; Penninx, B.W.; Marchionni, N.; Pahor, M. Physical exercise and comorbidity. Results from the Fitness and Arthritis in Seniors Trial (FAST). Aging Clin. Exp. Res. 2006, 18, 374–380. [Google Scholar] [CrossRef]
- Matsuse, H.; Segal, N.A.; Rabe, K.G.; Shiba, N. The Effect of Neuromuscular Electrical Stimulation During Walking on Muscle Strength and Knee Pain in Obese Women With Knee Pain: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2020, 99, 56–64. [Google Scholar] [CrossRef]
- McLeod, A.; Schiffer, L.; Castellanos, K.; DeMott, A.; Olender, S.; Fitzgibbon, M.; Hughes, S.; Fantuzzi, G.; Tussing-Humphreys, L. Impact of Physical Activity and Weight Loss on Fat Mass, Glucose Metabolism, and Inflammation in Older African Americans with Osteoarthritis. Nutrients 2020, 12, 3299. [Google Scholar] [CrossRef] [PubMed]
- Messier, S.P.; Loeser, R.F.; Mitchell, M.N.; Valle, G.; Morgan, T.P.; Rejeski, W.J.; Ettinger, W.H. Exercise and weight loss in obese older adults with knee osteoarthritis: A preliminary study. J. Am. Geriatr. Soc. 2000, 48, 1062–1072. [Google Scholar] [CrossRef]
- Messier, S.P.; Mihalko, S.L.; Legault, C.; Miller, G.D.; Nicklas, B.J.; DeVita, P.; Beavers, D.P.; Hunter, D.J.; Lyles, M.F.; Eckstein, F.; et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: The IDEA randomized clinical trial. JAMA 2013, 310, 1263–1273. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.D.; Jenks, M.Z.; Vendela, M.; Norris, J.L.; Muday, G.K. Influence of weight loss, body composition, and lifestyle behaviors on plasma adipokines: A randomized weight loss trial in older men and women with symptomatic knee osteoarthritis. J. Obes. 2012, 2012, 708505. [Google Scholar] [CrossRef] [Green Version]
- Miller, G.D.; Nicklas, B.J.; Davis, C.; Loeser, R.F.; Lenchik, L.; Messier, S.P. Intensive weight loss program improves physical function in older obese adults with knee osteoarthritis. Obesity 2006, 14, 1219–1230. [Google Scholar] [CrossRef] [PubMed]
- Rabe, K.G.; Matsuse, H.; Jackson, A.; Segal, N.A. Evaluation of the Combined Application of Neuromuscular Electrical Stimulation and Volitional Contractions on Thigh Muscle Strength, Knee Pain, and Physical Performance in Women at Risk for Knee Osteoarthritis: A Randomized Controlled Trial. Pm&r 2018, 10, 1301–1310. [Google Scholar]
- Robbins, S.R.; Melo, L.R.S.; Urban, H.; Deveza, L.A.; Asher, R.; Johnson, V.L.; Hunter, D.J. Is a stepped-care intervention effective in overweight and obese people with medial tibiofemoral osteoarthritis? The STrEAMline study: A randomised controlled trial. Arthritis Care Res. 2021, 73, 520–530. [Google Scholar] [CrossRef]
- Rosemffet, M.G.; Schneeberger, E.E.; Citera, G.; Sgobba, M.E.; Laiz, C.; Schmulevich, H.; Artçanuturry, P.; Gagliardi, S.; Maldonado Cocco, J.A. Effects of functional electrostimulation on pain, muscular strength, and functional capacity in patients with osteoarthritis of the knee. J. Clin. Rheumatol. 2004, 10, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Segal, N.; Davis, M.D.; Mikesky, A.E. Efficacy of Blood Flow-Restricted Low-Load Resistance Training For Quadriceps Strengthening in Men at Risk of Symptomatic Knee Osteoarthritis. Geriatr. Orthop. Surg. Rehabil. 2015, 6, 160–167. [Google Scholar] [CrossRef] [Green Version]
- Segal, N.A.; Williams, G.N.; Davis, M.C.; Wallace, R.B.; Mikesky, A.E. Efficacy of blood flow-restricted, low-load resistance training in women with risk factors for symptomatic knee osteoarthritis. Pm&r 2015, 7, 376–384. [Google Scholar]
- Skou, S.T.; Rasmussen, S.; Laursen, M.B.; Rathleff, M.S.; Arendt-Nielsen, L.; Simonsen, O.; Roos, E.M. The efficacy of 12 weeks non-surgical treatment for patients not eligible for total knee replacement: A randomized controlled trial with 1-year follow-up. Osteoarthr. Cartil. 2015, 23, 1465–1475. [Google Scholar] [CrossRef] [Green Version]
- Skou, S.T.; Roos, E.M.; Laursen, M.B.; Rathleff, M.S.; Arendt-Nielsen, L.; Rasmussen, S.; Simonsen, O. Total knee replacement and non-surgical treatment of knee osteoarthritis: 2-year outcome from two parallel randomized controlled trials. Osteoarthr. Cartil. 2018, 26, 1170–1180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swank, A.M.; Kachelman, J.B.; Bibeau, W.; Quesada, P.M.; Nyland, J.; Malkani, A.; Topp, R.V. Prehabilitation before total knee arthroplasty increases strength and function in older adults with severe osteoarthritis. J. Strength Cond. Res. 2011, 25, 318–325. [Google Scholar] [CrossRef] [Green Version]
- Tak, E.; Staats, P.; Van Hespen, A.; Hopman-Rock, M. The effects of an exercise program for older adults with osteoarthritis of the hip. J. Rheumatol. 2005, 32, 1106–1113. [Google Scholar]
- Talbot, L.A.; Gaines, J.M.; Huynh, T.N.; Metter, E.J. A home-based pedometer-driven walking program to increase physical activity in older adults with osteoarthritis of the knee: A preliminary study. J. Am. Geriatr. Soc. 2003, 51, 387–392. [Google Scholar] [CrossRef]
- Talbot, L.A.; Gaines, J.M.; Ling, S.M.; Metter, E.J. A home-based protocol of electrical muscle stimulation for quadriceps muscle strength in older adults with osteoarthritis of the knee. J. Rheumatol. 2003, 30, 1571–1578. [Google Scholar] [PubMed]
- Toda, Y. The effect of energy restriction, walking, and exercise on lower extremity lean body mass in obese women with osteoarthritis of the knee. J. Orthop. Sci. 2001, 6, 148–154. [Google Scholar] [CrossRef]
- Toda, Y.; Kobayashi, T. The usefulness of walking for preventing sarcopenia in dieting postmenopausal women complaining of knee pain. Ann. N. Y. Acad. Sci. 2000, 904, 610–613. [Google Scholar] [CrossRef]
- Wallis, J.A.; Webster, K.E.; Levinger, P.; Singh, P.J.; Fong, C.; Taylor, N.F. A walking program for people with severe knee osteoarthritis did not reduce pain but may have benefits for cardiovascular health: A phase II randomised controlled trial. Osteoarthr. Cartil. 2017, 25, 1969–1979. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Miller, G.D.; Messier, S.P.; Nicklas, B.J. Knee strength maintained despite loss of lean body mass during weight loss in older obese adults with knee osteoarthritis. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 866–871. [Google Scholar] [CrossRef] [Green Version]
- Messier, S.P.; Legault, C.; Mihalko, S.; Miller, G.D.; Loeser, R.F.; DeVita, P.; Lyles, M.; Eckstein, F.; Hunter, D.J.; Williamson, J.D.; et al. The Intensive Diet and Exercise for Arthritis (IDEA) trial: Design and rationale. BMC Musculoskelet Disord. 2009, 10, 93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riecke, B.F.; Christensen, R.; Christensen, P.; Leeds, A.R.; Boesen, M.; Lohmander, L.S.; Astrup, A.; Bliddal, H. Comparing two low-energy diets for the treatment of knee osteoarthritis symptoms in obese patients: A pragmatic randomized clinical trial. Osteoarthr. Cartil. 2010, 18, 746–754. [Google Scholar] [CrossRef] [Green Version]
- Skou, S.T.; Roos, E.M.; Laursen, M.B.; Rathleff, M.S.; Arendt-Nielsen, L.; Simonsen, O.; Rasmussen, S. Efficacy of multimodal, systematic non-surgical treatment of knee osteoarthritis for patients not eligible for a total knee replacement: A study protocol of a randomised controlled trial. BMJ Open 2012, 2, e002168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messier, S.P.; Loeser, R.F.; Miller, G.D.; Morgan, T.M.; Rejeski, W.J.; Sevick, M.A.; Ettinger, W.H., Jr.; Pahor, M.; Williamson, J.D. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: The Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004, 50, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Schlenk, E.A.; Lias, J.L.; Sereika, S.M.; Dunbar-Jacob, J.; Kwoh, C.K. Improving physical activity and function in overweight and obese older adults with osteoarthritis of the knee: A feasibility study. Rehabil. Nurs. 2011, 36, 32–42. [Google Scholar] [CrossRef] [Green Version]
- Caldwell, D.M.; Welton, N.J.; Ades, A.E. Mixed treatment comparison analysis provides internally coherent treatment effect estimates based on overviews of reviews and can reveal inconsistency. J. Clin. Epidemiol. 2010, 63, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Reken, S.; Sturtz, S.; Kiefer, C.; Böhler, Y.B.; Wieseler, B. Assumptions of Mixed Treatment Comparisons in Health Technology Assessments—Challenges and Possible Steps for Practical Application. PLoS ONE 2016, 11, e0160712. [Google Scholar] [CrossRef]
- Barajas-Galindo, D.E.; González Arnáiz, E.; Ferrero Vicente, P.; Ballesteros-Pomar, M.D. Effects of physical exercise in sarcopenia. A systematic review. Endocrinol. Diabetes Nutr. 2021, 68, 159–169. [Google Scholar] [CrossRef]
- Beckwée, D.; Delaere, A.; Aelbrecht, S.; Baert, V.; Beaudart, C.; Bruyere, O.; de Saint-Hubert, M.; Bautmans, I. Exercise Interventions for the Prevention and Treatment of Sarcopenia. A Systematic Umbrella Review. J. Nutr. Health Aging 2019, 23, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Morze, J.; Rücker, G.; Danielewicz, A.; Przybyłowicz, K.; Neuenschwander, M.; Schlesinger, S.; Schwingshackl, L. Impact of different training modalities on anthropometric outcomes in patients with obesity: A systematic review and network meta-analysis. Obes. Rev. 2021, 3128, 1–12. [Google Scholar]
- Pazzianotto-Forti, E.M.; Moreno, M.A.; Plater, E.; Baruki, S.B.S.; Rasera-Junior, I.; Reid, W.D. Impact of Physical Training Programs on Physical Fitness in People With Class II and III Obesity: A Systematic Review and Meta-Analysis. Phys. Ther. 2020, 100, 963–978. [Google Scholar] [CrossRef]
- Wada, O.; Kurita, N.; Kamitani, T.; Mizuno, K. Implications of evaluating leg muscle mass and fat mass separately for quadriceps strength in knee osteoarthritis: The SPSS-OK study. Clin. Rheumatol. 2020, 39, 1655–1661. [Google Scholar] [CrossRef]
- Duchowny, K.A.; Peters, K.E.; Cummings, S.R.; Orwoll, E.S.; Hoffman, A.R.; Ensrud, K.E.; Cauley, J.A.; Evans, W.J.; Cawthon, P.M. Association of change in muscle mass assessed by D3 -creatine dilution with changes in grip strength and walking speed. J. Cachexia Sarcopenia Muscle 2020, 11, 55–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osawa, Y.; Chiles Shaffer, N.; Shardell, M.D.; Studenski, S.A.; Ferrucci, L. Changes in knee extension peak torque and body composition and their relationship with change in gait speed. J. Cachexia Sarcopenia Muscle 2019, 10, 1000–1008. [Google Scholar] [CrossRef]
- Liao, C.D.; Chen, H.C.; Huang, S.W.; Liou, T.H. The Role of Muscle Mass Gain Following Protein Supplementation Plus Exercise Therapy in Older Adults with Sarcopenia and Frailty Risks: A Systematic Review and Meta-Regression Analysis of Randomized Trials. Nutrients 2019, 11, 1713. [Google Scholar] [CrossRef] [Green Version]
- Liao, C.D.; Wu, Y.T.; Tsauo, J.Y.; Chen, P.R.; Tu, Y.K.; Chen, H.C.; Liou, T.H. Effects of Protein Supplementation Combined with Exercise Training on Muscle Mass and Function in Older Adults with Lower-Extremity Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Trials. Nutrients 2020, 12, 2422. [Google Scholar] [CrossRef] [PubMed]
- Da Boit, M.; Sibson, R.; Meakin, J.R.; Aspden, R.M.; Thies, F.; Mangoni, A.A.; Gray, S.R. Sex differences in the response to resistance exercise training in older people. Physiol. Rep. 2016, 4, e12834. [Google Scholar] [CrossRef]
- Burd, N.A.; Tang, J.E.; Moore, D.R.; Phillips, S.M. Exercise training and protein metabolism: Influences of contraction, protein intake, and sex-based differences. J. Appl. Physiol. 2009, 106, 1692–1701. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.I.; Villareal, D.T.; Sinacore, D.R.; Shah, K.; Mittendorfer, B. Muscle protein synthesis response to exercise training in obese, older men and women. Med. Sci. Sports Exerc. 2012, 44, 1259–1266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, M.S.; Callahan, D.M.; Tourville, T.W.; Slauterbeck, J.R.; Kaplan, A.; Fiske, B.R.; Savage, P.D.; Ades, P.A.; Beynnon, B.D.; Toth, M.J. Moderate-intensity resistance exercise alters skeletal muscle molecular and cellular structure and function in inactive older adults with knee osteoarthritis. J. Appl. Physiol. 2017, 122, 775–787. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chu, S.-F.; Liou, T.-H.; Chen, H.-C.; Huang, S.-W.; Liao, C.-D. Relative Efficacy of Weight Management, Exercise, and Combined Treatment for Muscle Mass and Physical Sarcopenia Indices in Adults with Overweight or Obesity and Osteoarthritis: A Network Meta-Analysis of Randomized Controlled Trials. Nutrients 2021, 13, 1992. https://doi.org/10.3390/nu13061992
Chu S-F, Liou T-H, Chen H-C, Huang S-W, Liao C-D. Relative Efficacy of Weight Management, Exercise, and Combined Treatment for Muscle Mass and Physical Sarcopenia Indices in Adults with Overweight or Obesity and Osteoarthritis: A Network Meta-Analysis of Randomized Controlled Trials. Nutrients. 2021; 13(6):1992. https://doi.org/10.3390/nu13061992
Chicago/Turabian StyleChu, Shu-Fen, Tsan-Hon Liou, Hung-Chou Chen, Shih-Wei Huang, and Chun-De Liao. 2021. "Relative Efficacy of Weight Management, Exercise, and Combined Treatment for Muscle Mass and Physical Sarcopenia Indices in Adults with Overweight or Obesity and Osteoarthritis: A Network Meta-Analysis of Randomized Controlled Trials" Nutrients 13, no. 6: 1992. https://doi.org/10.3390/nu13061992






