The Effects of Bariatric Surgery on Vitamin B Status and Mental Health
Abstract
1. Introduction
2. Methodology
3. Role of Vitamin B in Human Health and the Immune System
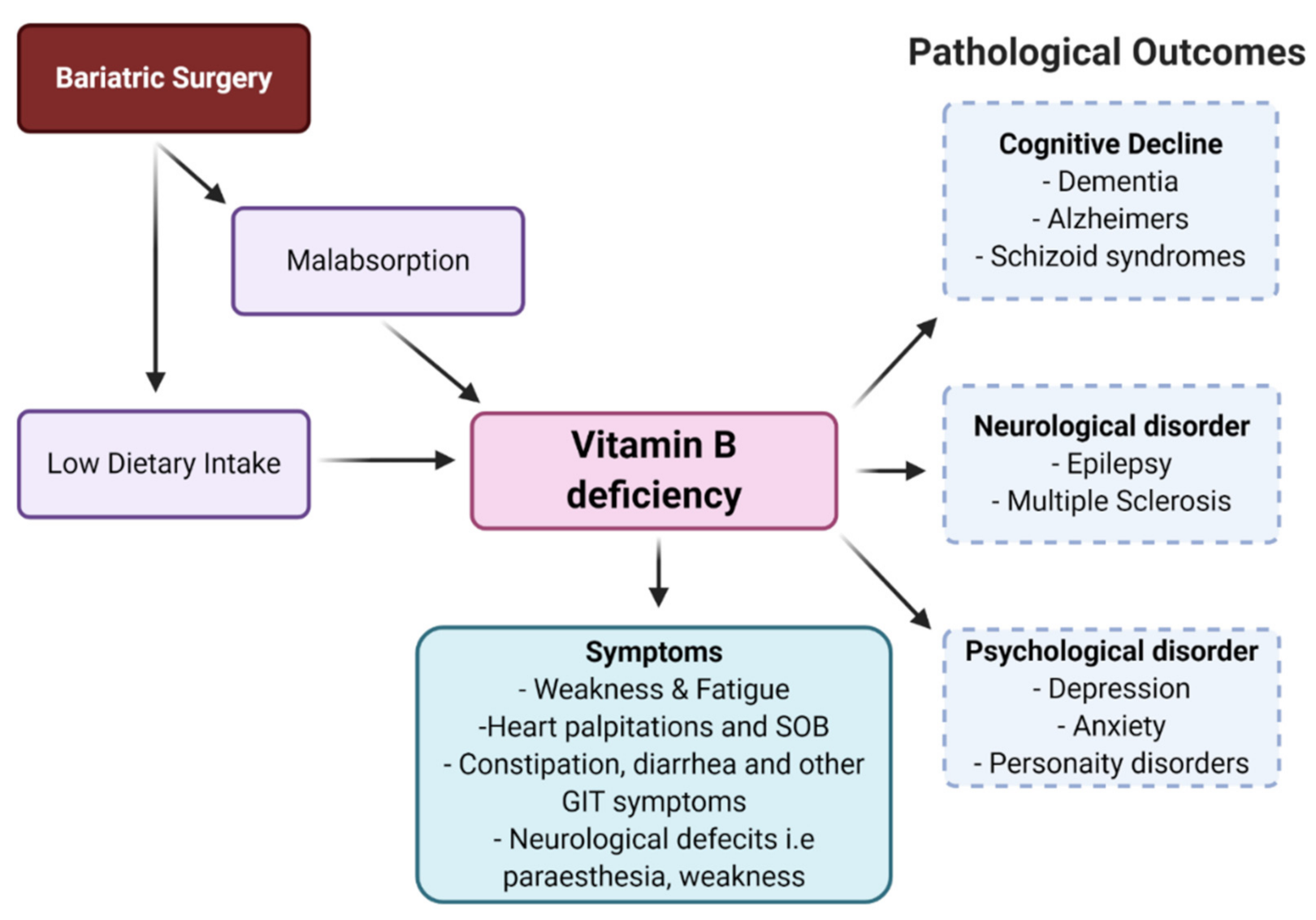
4. Bariatric Surgery and Vitamin B Deficiency
4.1. Bariatric Surgery
| Number of Participants | Duration and Stage | Percentage (%) of Vitamin B Deficiency |
|---|---|---|
| 232 bariatric surgery participants [60] | Post-operative | Folate (3.4%), B12 (18.1%), B3 (5.6%), B6 (2.2%) |
| 169 RYGB patients [61] | Pre-operative, 1,2,3, years’ post-operative | Pre-operative B12 deficient (12.3%), Postoperative B12 after 1, 2, 3 years (19%, 28%, 29%) |
| 149 bariatric surgery participants [62] | Post-operative | B12 (11%) |
| 30 patients underwent laparoscopic RYGB [63] | 6-months preoperative and 3-year post-operative | B12 at 2 years (33.3%) and 3 years (27.2%). No folic acid deficiency |
| 98 participants underwent RYGB and LSG [64] | 1-year pre-operative and 1-year post-operative | B12 deficient one-year post-operative elevated from 6.4–25.5% in the RYGB group |
| 468 patients underwent RYGB and LSG [65] | Pre-operative and post-operative and after one year | Pre-operative B1 deficiency in LSG (8.1%) and RYGB (1.7%) Post-operative B1 deficient in LSG (10.5%) and RYGB (13.7%). One-year B1 deficient in LSG (7.2%) and in RYGB (5.9%). |
| 95 participants underwent RYGB and SG [66] | Post-operative | Low level of vitamin B12 in RYGB (42.1%) and LSG (5%). Folate deficiency in RYGB (20%) and LSG (18.4%). |
| 74 Gastric bypass participants [67] | >1 year | Folate (38%) |
| 253 RYGB and 142 SG participants [68] | 1–2 years post-operative | The serum concentration of vitamin B12 was significantly higher in the group who had undergone SG as compared to RYBG at 2 years |
| 37 patients with severe obesity undergoing bariatric surgery [69] | 3 months and 1 year post-operatively | During the year following operation, vitamin B6 level enhanced |
| 60 bariatric surgery patients (gastric bypass, duodenal switch) All patients received multivitamin, and gastric bypass patients received B12 substitute [70] | 6 months pre-operative, and 1 year post-operative | Duodenal switch patients showed thiamine deficiency after surgery. The level of riboflavin and vitamin B6 did not change after surgery |
| 1160 subject with RYGB, 883 received, and 258 did not receive, specialized multivitamin supplements [71] | 3 years post-operative | Participants who received specialized multivitamin supplements were less deficient in vitamin B12, vitamin D, folic acid, and ferritin as compared to other group receiving no supplements |
| 45 Bariatric patients treated with intramuscular hydroxocobalamin injections, while 45 did not receive [72] | Post-operative | The treated group reported significantly increased vitamin B12 and showed fewer clinical complaints |
| 1538 patients’ micronutrient status assessed prior to bariatric surgery [73] | Pre-operative | Vitamin B12 deficiency was 16%, and various other micronutrient deficiencies pre-exit High level of vitamin B6 by 24% found before surgery |
| 103 morbidly obese women before bariatric surgery [74] | Pre-operative | 10.6% of participants had B12 deficiency, No folic acid deficiency Deficiency of other micronutrients (iron, zinc, calcium, phosphorus) |
| 1732 patients with morbid obesity wishing to undergo bariatric surgery [75] | Pre-operative | 63.2% of participants had a folic acid deficiency and various other micronutrient deficiencies |
| 2008 morbid obese participants wanted bariatric surgery [76] | Pre-operative | Participants deficient in vitamin D, vitamin B12, iron, and hemoglobin by 53.6%, 34.4%, 10.2%, and 16.6%, respectively, prior to bariatric surgery |
| 114 patients assigned for bariatric surgery [77] | Pre-operative | Participants deficient in iron, folic acid, ferritin, vitamin B12, and calcium by 35%, 24%, 24%, 3.6%, and 0.9%, respectively, prior to bariatric surgery |
| 200 patients with SG [78] | Pre- and Post-operative | Participants deficient in B1, B6, B12, folic acid, vitamin D by 5.5%, 3%, 11.5%, 24%, and 81, respectively, prior to surgery and deficient after surgery in B1, B6, B12, and vitamin D by 9%, 4%, 11.5%, and 36%, respectively |
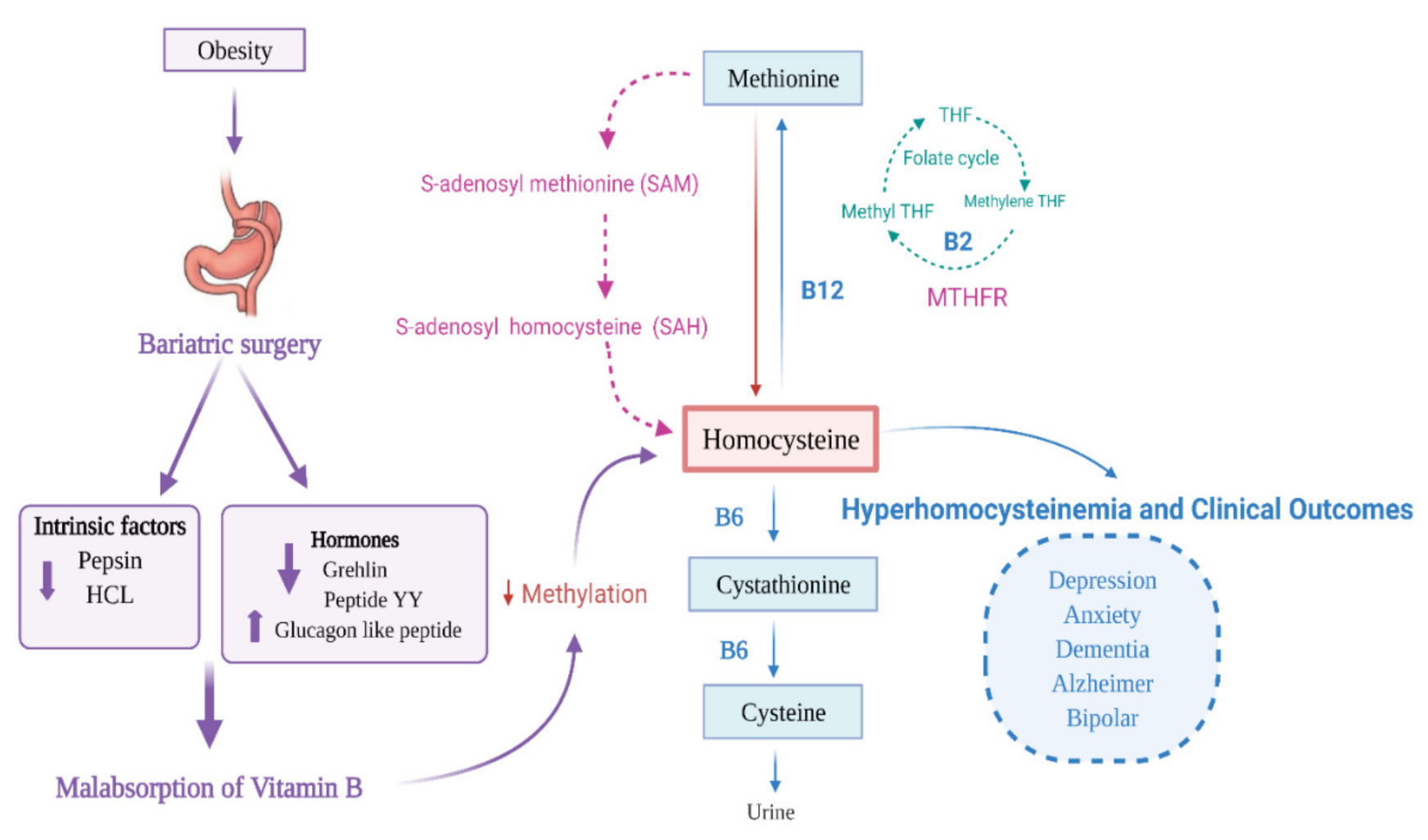
4.2. Mechanisms of Vitamin B Deficiency Following Bariatric Surgery
4.3. Bariatric Surgery and Hyperhomocysteinemia
4.4. Depression and Anxiety in Patients Following Bariatric Surgery
4.5. Neurological Complications in Patients Following Bariatric Surgery
5. Effectiveness of Vitamin B Supplementation in Bariatric Surgery Patients
6. Strategies to Prevent Vitamin B Deficiency in Bariatric Surgery Patients
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Min, J.; Zhao, Y.; Slivka, L.; Wang, Y. Double burden of diseases worldwide: Coexistence of undernutrition and overnutrition-related non-communicable chronic diseases. Obes. Rev. 2018, 19, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention. Micronutrient Malnutrition: Reducing Nutritional Deficiencies Globally; National Center for Chronic Disease Prevention and Health Promotion: Atlanta, GA, USA, 2016. [Google Scholar]
- Aminian, A.; Zelisko, A.; Kirwan, J.P.; Brethauer, S.A.; Schauer, P.R. Exploring the impact of bariatric surgery on high density lipoprotein. Surg. Obes. Relat. Dis. 2015, 11, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Punchai, S.; Hanipah, Z.N.; Meister, K.M.; Schauer, P.R.; Brethauer, S.A.; Aminian, A. Neurologic manifestations of vitamin B deficiency after bariatric surgery. Obes. Surg. 2017, 27, 2079–2082. [Google Scholar] [CrossRef] [PubMed]
- Shankar, P.; Boylan, M.; Sriram, K. Micronutrient deficiencies after bariatric surgery. Nutrition 2010, 26, 1031–1037. [Google Scholar] [CrossRef]
- Parkes, E. Nutritional management of patients after bariatric surgery. Am. J. Med. Sci. 2006, 331, 207–213. [Google Scholar] [CrossRef]
- Szmulewicz, A.; Wanis, K.N.; Gripper, A.; Angriman, F.; Hawel, J.; Elnahas, A.; Alkhamesi, N.A.; Schlachta, C.M. Mental health quality of life after bariatric surgery: A systematic review and meta-analysis of randomized clinical trials. Clin. Obes. 2019, 9, e12290. [Google Scholar] [CrossRef]
- Mattson, M.P.; Shea, T.B. Folate and homocysteine metabolism in neural plasticity and neurodegenerative disorders. Trends Neurosci. 2003, 26, 137–146. [Google Scholar] [CrossRef]
- Mikkelsen, K.; Stojanovska, L.; Prakash, M.; Apostolopoulos, V. The effects of vitamin B on the immune/cytokine network and their involvement in depression. Maturitas 2017, 96, 58–71. [Google Scholar] [CrossRef]
- Hughes, C.F.; Ward, M.; Tracey, F.; Hoey, L.; Molloy, A.M.; Pentieva, K.; McNulty, H. B-vitamin intake and biomarker status in relation to cognitive decline in healthy older adults in a 4-year follow-up study. Nutrients 2017, 9, 53. [Google Scholar] [CrossRef]
- Duthie, S.J.; Whalley, L.J.; Collins, A.R.; Leaper, S.; Berger, K.; Deary, I.J. Homocysteine, B vitamin status, and cognitive function in the elderly. Am. J. Clin. Nutr. 2002, 75, 908–913. [Google Scholar] [CrossRef]
- Kennedy, D.O.; Veasey, R.; Watson, A.; Dodd, F.; Jones, E.; Maggini, S.; Haskell, C.F. Effects of high-dose B vitamin complex with vitamin C and minerals on subjective mood and performance in healthy males. Psychopharmacology 2010, 211, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.E.; Tiozzo, E.; Melillo, A.B.; Leonard, S.; Chen, L.; Mendez, A.; Woolger, J.M.; Konefal, J. The effect of methylated vitamin B complex on depressive and anxiety symptoms and quality of life in adults with depression. Int. Sch. Res. Not. 2013, 2013, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.G.; Mackinnon, A.J.; Batterham, P.; Jorm, A.F.; Hickie, I.; McCarthy, A.; Fenech, M.; Christensen, H. Mental health literacy, folic acid and vitamin B 12, and physical activity for the prevention of depression in older adults: Randomised controlled trial. Br. J. Psychiatry 2010, 197, 45–54. [Google Scholar] [CrossRef]
- Nijst, T.Q.; Wevers, R.A.; Schoonderwaldt, H.C.; Hommes, O.R.; De Haan, A.F. Vitamin B12 and folate concentrations in serum and cerebrospinal fluid of neurological patients with special reference to multiple sclerosis and dementia. J. Neurol. Neurosurg. Psychiatry 1990, 53, 951–954. [Google Scholar] [CrossRef]
- Reynolds, E.H. Schizophrenia-like psychoses of epilepsy and disturbances of folate and vitamin B 12 metabolism induced by anticonvulsant drugs. Br. J. Psychiatry 1967, 113, 911–919. [Google Scholar] [CrossRef]
- Kerns, J.C.; Arundel, C.; Chawla, L.S. Thiamin deficiency in people with obesity. Adv. Nutr. 2015, 6, 147–153. [Google Scholar] [CrossRef]
- Scalabrino, G. Vitamin-regulated cytokines and growth factors in the CNS and elsewhere. J. Neurochem. 2009, 111, 1309–1326. [Google Scholar] [CrossRef]
- Mikkelsen, K.; Prakash, M.D.; Kuol, N.; Nurgali, K.; Stojanovska, L.; Apostolopoulos, V. Anti-Tumor Effects of Vitamin B2, B6 and B9 in Promonocytic Lymphoma Cells. Int. J. Mol. Sci. 2019, 20, 3763. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.M.; Iqbal, S.; Naseem, I. Ameliorative effect of riboflavin on hyperglycemia, oxidative stress and DNA damage in type-2 diabetic mice: Mechanistic and therapeutic strategies. Arch. Biochem. Biophys. 2015, 584, 10–19. [Google Scholar] [CrossRef]
- Kennedy, D.O. B vitamins and the brain: Mechanisms, dose and efficacy—A review. Nutrients 2016, 8, 68. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Saggini, A.; Kritas, S.K.; Cerulli, G.; Caraffa, A.; Antinolfi, P.; Pantalone, A.; Frydas, A.; Tei, M.; Speziali, A. Crosstalk between vitamin B and immunity. J. Biol. Regul. Homeost. Agents 2015, 29, 283–288. [Google Scholar] [PubMed]
- Pitkin, R.M.; Allen, L.H.; Bailey, L.B.; Bernfield, M. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin and Choline; National Academy Press: Washington, DC, USA, 2000. [Google Scholar]
- Ferreira, R.G.; Matsui, T.C.; Gomides, L.F.; Godin, A.M.; Menezes, G.B.; de Matos Coelho, M.; Klein, A. Niacin inhibits carrageenan-induced neutrophil migration in mice. Naunyn Schmiedeberg Arch. Pharmacol. 2013, 386, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Bialonska, D.; Ramnani, P.; Kasimsetty, S.G.; Muntha, K.R.; Gibson, G.R.; Ferreira, D. The influence of pomegranate by-product and punicalagins on selected groups of human intestinal microbiota. Int. J. Food Microbiol. 2010, 140, 175–182. [Google Scholar] [CrossRef]
- Imai, S.-I.; Guarente, L. NAD+ and sirtuins in aging and disease. Trends Cell Biol. 2014, 24, 464–471. [Google Scholar] [CrossRef]
- Johnson, S.; Imai, S. NAD+ biosynthesis, aging, and disease. F1000Research 2018, 7, 132. [Google Scholar] [CrossRef]
- Maqbool, M.A.; Aslam, M.; Akbar, W.; Iqbal, Z. Biological importance of vitamins for human health: A review. J. Agric. Basic Sci. 2018, 2. [Google Scholar]
- Said, H.M.; Mohammed, Z.M. Intestinal absorption of water-soluble vitamins: An update. Curr. Opin. Gastroenterol. 2006, 22, 140–146. [Google Scholar] [CrossRef]
- Said, H.M.; Ortiz, A.; Ma, T.Y. A carrier-mediated mechanism for pyridoxine uptake by human intestinal epithelial Caco-2 cells: Regulation by a PKA-mediated pathway. Am. J. Physiol. Cell Physiol. 2003, 285, C1219–C1225. [Google Scholar] [CrossRef]
- Stover, P.J. Physiology of folate and vitamin B 12 in health and disease. Nutr. Rev. 2004, 62, S3–S12. [Google Scholar] [CrossRef]
- Fang, H.; Kang, J.; Zhang, D. Microbial production of vitamin B 12: A review and future perspectives. Microb. Cell Factories 2017, 16, 15. [Google Scholar] [CrossRef]
- O’Leary, F.; Samman, S. Vitamin B12 in health and disease. Nutrients 2010, 2, 299–316. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, K.; Kobayashi, R.; Sano, H.; Suzuki, D.; Maruoka, H.; Yasuda, K.; Chida, N.; Yamada, M.; Kobayashi, K. Impact of folate therapy on combined immunodeficiency secondary to hereditary folate malabsorption. Clin. Immunol. 2014, 153, 17–22. [Google Scholar] [CrossRef]
- Scalabrino, G.; Veber, D. Cobalamin and normal prions: A new horizon for cobalamin neurotrophism. Biochimie 2013, 95, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Karadag, S.; Gursu, M.; Sakin, A.; Atalay, E.; Basinoglu, F.; Aydin, Z.; Uzun, S.; Sumnu, A.; Cebeci, E.; Koldas, M. The Relationship between Soluble Tumor Necrosis Factor-like Weak Inducer of Apoptosis Levels and Cardiac Functions in Peritoneal Dialysis Patients. Eur. J. Inflamm. 2014, 12, 429–437. [Google Scholar] [CrossRef]
- Kritas, S.K.; Caraffa, A.; Antinolfi, P.; Saggini, A.; Pantalone, A.; Rosati, M.; Tei, M.; Speziali, A.; Saggini, R.; Pandolfi, F. Nerve Growth Factor Interactions with Mast Cells; SAGE Publications Sage UK: London, UK, 2014. [Google Scholar]
- Seemungal, T.A.R.; Lun, J.C.F.; Davis, G.; Neblett, C.; Chinyepi, N.; Dookhan, C.; Drakes, S.; Mandeville, E.; Nana, F.; Setlhake, S. Plasma homocysteine is elevated in COPD patients and is related to COPD severity. Int. J. Chronic Obstr. Pulm. Dis. 2007, 2, 313. [Google Scholar] [CrossRef] [PubMed]
- Tamura, J.; Kubota, K.; Murakami, H.; Sawamura, M.; Matsushima, T.; Tamura, T.; Saitoh, T.; Kurabayshi, H.; Naruse, T. Immunomodulation by vitamin B12: Augmentation of CD8+ T lymphocytes and natural killer (NK) cell activity in vitamin B12-deficient patients by methyl-B12 treatment. Clin. Exp. Immunol. 1999, 116, 28–32. [Google Scholar] [CrossRef]
- Thakur, K.; Tomar, S.K.; Singh, A.K.; Mandal, S.; Arora, S. Riboflavin and health: A review of recent human research. Crit. Rev. Food Sci. Nutr. 2017, 57, 3650–3660. [Google Scholar] [CrossRef]
- Kaneko, S.; Wang, J.; Kaneko, M.; Yiu, G.; Hurrell, J.M.; Chitnis, T.; Khoury, S.J.; He, Z. Protecting axonal degeneration by increasing nicotinamide adenine dinucleotide levels in experimental autoimmune encephalomyelitis models. J. Neurosci. 2006, 26, 9794–9804. [Google Scholar] [CrossRef]
- Chai, J.T.; Digby, J.E.; Ruparelia, N.; Jefferson, A.; Handa, A.; Choudhury, R.P. Nicotinic acid receptor GPR109A is down-regulated in human macrophage-derived foam cells. PLoS ONE 2013, 8, e62934. [Google Scholar] [CrossRef]
- He, W.; Hu, S.; Du, X.; Wen, Q.; Zhong, X.-P.; Zhou, X.; Zhou, C.; Xiong, W.; Gao, Y.; Zhang, S. Vitamin B5 reduces bacterial growth via regulating innate immunity and adaptive immunity in mice infected with Mycobacterium tuberculosis. Front. Immunol. 2018, 9, 365. [Google Scholar] [CrossRef]
- Tolmunen, T.; Voutilainen, S.; Hintikka, J.; Rissanen, T.; Tanskanen, A.; Viinamäki, H.; Kaplan, G.A.; Salonen, J.T. Dietary folate and depressive symptoms are associated in middle-aged Finnish men. J. Nutr. 2003, 133, 3233–3236. [Google Scholar] [CrossRef] [PubMed]
- Kuroishi, T.; Endo, Y.; Muramoto, K.; Sugawara, S. Biotin deficiency up-regulates TNF-α production in murine macrophages. J. Leukoc. Biol. 2008, 83, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Scalabrino, G.; Corsi, M.M.; Veber, D.; Buccellato, F.R.; Pravettoni, G.; Manfridi, A.; Magni, P. Cobalamin (vitamin B12) positively regulates interleukin-6 levels in rat cerebrospinal fluid. J. Neuroimmunol. 2002, 127, 37–43. [Google Scholar] [CrossRef]
- Vogiatzoglou, A.; Refsum, H.; Johnston, C.; Smith, S.M.; Bradley, K.M.; De Jager, C.; Budge, M.M.; Smith, A.D. Vitamin B12 status and rate of brain volume loss in community-dwelling elderly. Neurology 2008, 71, 826–832. [Google Scholar] [CrossRef]
- Switzer, N.J.; Karmali, S.; Gill, R.S.; Sherman, V. Revisional bariatric surgery. Surg. Clin. 2016, 96, 827–842. [Google Scholar] [CrossRef] [PubMed]
- Quercia, I.; Dutia, R.; Laferrere, B.; Kotler, D.P.; Belsley, S. Gastrointestinal changes after bariatric surgery. Diabetes Metab. 2014, 40, 87–94. [Google Scholar] [CrossRef]
- Angrisani, L.; Santonicola, A.; Iovino, P.; Vitiello, A.; Higa, K.; Himpens, J.; Buchwald, H.; Scopinaro, N. IFSO worldwide survey 2016: Primary, endoluminal, and revisional procedures. Obes. Surg. 2018, 28, 3783–3794. [Google Scholar] [CrossRef]
- Strang, B.J.; McGinnis, S.L. Nutritional Concerns in Bariatric Surgery: Thiamin Deficiency after Sleeve Gastrectomy. Support. Line 2016, 38, 9–14. [Google Scholar]
- Goodman, J.C. Neurological complications of bariatric surgery. Curr. Neurol. Neurosci. Rep. 2015, 15, 79. [Google Scholar] [CrossRef]
- Ziegler, O.; Sirveaux, M.A.; Brunaud, L.; Reibel, N.; Quilliot, D. Medical follow up after bariatric surgery: Nutritional and drug issues General recommendations for the prevention and treatment of nutritional deficiencies. Diabetes Metab. 2009, 35, 544–557. [Google Scholar] [CrossRef]
- Gasteyger, C.; Suter, M.; Gaillard, R.C.; Giusti, V. Nutritional deficiencies after Roux-en-Y gastric bypass for morbid obesity often cannot be prevented by standard multivitamin supplementation. Am. J. Clin. Nutr. 2008, 87, 1128–1133. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Halverson, J.D. Metabolic risk of obesity surgery and long-term follow-up. Am. J. Clin. Nutr. 1992, 55, 602S–605S. [Google Scholar] [CrossRef]
- Kwon, Y.; Kim, H.J.; Lo Menzo, E.; Park, S.; Szomstein, S.; Rosenthal, R.J. Anemia, iron and vitamin B12 deficiencies after sleeve gastrectomy compared to Roux-en-Y gastric bypass: A meta-analysis. Surg. Obes. Relat. Dis. 2014, 10, 589–597. [Google Scholar] [CrossRef]
- Moschos, M.; Droutsas, D. A man who lost weight and his sight. Lancet 1998, 351, 1174. [Google Scholar] [CrossRef]
- Eltweri, A.M.; Bowrey, D.J.; Sutton, C.D.; Graham, L.; Williams, R.N. An audit to determine if vitamin b12 supplementation is necessary after sleeve gastrectomy. SpringerPlus 2013, 2, 1–4. [Google Scholar] [CrossRef][Green Version]
- Gagner, M.; Deitel, M.; Erickson, A.L.; Crosby, R.D. Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes. Surg. 2013, 23. [Google Scholar] [CrossRef]
- Ernst, B.; Thurnheer, M.; Schmid, S.M.; Schultes, B. Evidence for the necessity to systematically assess micronutrient status prior to bariatric surgery. Obes. Surg. 2009, 19, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Arias, P.M.; Domeniconi, E.A.; García, M.; Esquivel, C.M.; Martínez Lascano, F.; Foscarini, J.M. Micronutrient Deficiencies After Roux-en-Y Gastric Bypass: Long-Term Results. Obes. Surg. 2020, 30, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Toh, S.Y.; Zarshenas, N.; Jorgensen, J. Prevalence of nutrient deficiencies in bariatric patients. Nutrition 2009, 25, 1150–1156. [Google Scholar] [CrossRef]
- Vargas-Ruiz, A.G.; Hernández-Rivera, G.; Herrera, M.F. Prevalence of iron, folate, and vitamin B12 deficiency anemia after laparoscopic Roux-en-Y gastric bypass. Obes. Surg. 2008, 18, 288–293. [Google Scholar] [CrossRef]
- Antoniewicz, A.; Kalinowski, P.; Kotulecka, K.J.; Kocoń, P.; Paluszkiewicz, R.; Remiszewski, P.; Zieniewicz, K. Nutritional deficiencies in patients after Roux-en-Y gastric bypass and sleeve gastrectomy during 12-month follow-up. Obes. Surg. 2019, 29, 3277–3284. [Google Scholar] [CrossRef]
- Johnson, L.M.; Ikramuddin, S.; Leslie, D.B.; Slusarek, B.; Killeen, A.A. Analysis of vitamin levels and deficiencies in bariatric surgery patients: A single-institutional analysis. Surg. Obes. Relat. Dis. 2019, 15, 1146–1152. [Google Scholar] [CrossRef] [PubMed]
- Brotto, M.; Johnson, M.L. Endocrine crosstalk between muscle and bone. Curr. Osteoporos. Rep. 2014, 12, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Halverson, J.D. Micronutrient deficiencies after gastric bypass for morbid obesity. Am. Surg. 1986, 52, 594–598. [Google Scholar] [PubMed]
- Javanainen, M.; Pekkarinen, T.; Mustonen, H.; Scheinin, T.; Leivonen, M. Two-Year Nutrition Data in Terms of Vitamin D, Vitamin B12, and Albumin After Bariatric Surgery and Long-term Fracture Data Compared with Conservatively Treated Obese Patients: A Retrospective Cohort Study. Obes. Surg. 2018, 28, 2968–2975. [Google Scholar] [CrossRef]
- Christensen, M.H.E.; Fadnes, D.J.; Røst, T.H.; Pedersen, E.R.; Andersen, J.R.; Våge, V.; Ulvik, A.; Midttun, Ø.; Ueland, P.M.; Nygård, O.K. Inflammatory markers, the tryptophan-kynurenine pathway, and vitamin B status after bariatric surgery. PLoS ONE 2018, 13, e0192169. [Google Scholar] [CrossRef]
- Aasheim, E.T.; Björkman, S.; Søvik, T.T.; Engström, M.; Hanvold, S.E.; Mala, T.; Olbers, T.; Bøhmer, T. Vitamin status after bariatric surgery: A randomized study of gastric bypass and duodenal switch. Am. J. Clin. Nutr. 2009, 90, 15–22. [Google Scholar] [CrossRef]
- Schijns, W.; Schuurman, L.T.; Melse-Boonstra, A.; van Laarhoven, C.J.H.M.; Berends, F.J.; Aarts, E.O. Do specialized bariatric multivitamins lower deficiencies after RYGB? Surg. Obes. Relat. Dis. 2018, 14, 1005–1012. [Google Scholar] [CrossRef]
- Smelt, H.J.M.; Smulders, J.F.; Said, M.; Nienhuijs, S.W.; Boer, A.K. Improving Bariatric Patient Aftercare Outcome by Improved Detection of a Functional Vitamin B12 Deficiency. Obes. Surg. 2016, 26, 1500–1504. [Google Scholar] [CrossRef]
- Al-Mutawa, A.; Anderson, A.K.; Alsabah, S.; Al-Mutawa, M. Nutritional Status of Bariatric Surgery Candidates. Nutrients 2018, 10, 67. [Google Scholar] [CrossRef]
- Sánchez, A.; Rojas, P.; Basfi-fer, K.; Carrasco, F.; Inostroza, J.; Codoceo, J.; Valencia, A.; Papapietro, K.; Csendes, A.; Ruz, M. Micronutrient Deficiencies in Morbidly Obese Women Prior to Bariatric Surgery. Obes. Surg. 2016, 26, 361–368. [Google Scholar] [CrossRef]
- Krzizek, E.-C.; Brix, J.M.; Herz, C.T.; Kopp, H.P.; Schernthaner, G.-H.; Schernthaner, G.; Ludvik, B. Prevalence of micronutrient deficiency in patients with morbid obesity before bariatric surgery. Obes. Surg. 2018, 28, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Asghari, G.; Khalaj, A.; Ghadimi, M.; Mahdavi, M.; Farhadnejad, H.; Valizadeh, M.; Azizi, F.; Barzin, M.; Hosseinpanah, F. Prevalence of Micronutrient Deficiencies Prior to Bariatric Surgery: Tehran Obesity Treatment Study (TOTS). Obes. Surg. 2018, 28, 2465–2472. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, C.; Weiss, R.; Berry, E.; Keidar, A. Nutritional deficiencies in bariatric surgery candidates. Obes. Surg. 2010, 20, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Van Rutte, P.W.J.; Aarts, E.O.; Smulders, J.F.; Nienhuijs, S.W. Nutrient Deficiencies Before and After Sleeve Gastrectomy. Obes. Surg. 2014, 24, 1639–1646. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, J.; Müller, A.; Gruner-Labitzke, K.; Lichtinghagen, R.; Hillemacher, T.; Bleich, S.; Frieling, H.; Köhler, H. Homocysteine and Cognition in Bariatric Surgery. Bariatr. Surg. Pract. Patient Care 2017, 12, 190–196. [Google Scholar] [CrossRef]
- Moore, C.E.; Sherman, V. Effectiveness of B Vitamin Supplementation Following Bariatric Surgery: Rapid Increases of Serum Vitamin B 12. Obes. Surg. 2015, 25, 694–699. [Google Scholar] [CrossRef]
- Kornerup, L.S.; Hvas, C.L.; Abild, C.B.; Richelsen, B.; Nexo, E. Early changes in vitamin B12 uptake and biomarker status following Roux-en-Y gastric bypass and sleeve gastrectomy. Clin. Nutr. 2019, 38, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Weng, T.C.; Chang, C.H.; Dong, Y.H.; Chang, Y.C.; Chuang, L.M. Anaemia and related nutrient deficiencies after Roux-en-Y gastric bypass surgery: A systematic review and meta-analysis. BMJ Open 2015, 5, e006964. [Google Scholar] [CrossRef]
- Majumder, S.; Soriano, J.; Louie Cruz, A.; Dasanu, C.A. Vitamin B12 deficiency in patients undergoing bariatric surgery: Preventive strategies and key recommendations. Surg. Obes. Relat. Dis. Off. J. Am. Soc. Bariatr. Surg. 2013, 9, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Marcuard, S.P.; Sinar, D.R.; Swanson, M.S.; Silverman, J.F.; Levine, J.S. Absence of luminal intrinsic factor after gastric bypass surgery for morbid obesity. Dig. Dis. Sci. 1989, 34, 1238–1242. [Google Scholar] [CrossRef] [PubMed]
- Zarshenas, N.; Tapsell, L.C.; Neale, E.P.; Batterham, M.; Talbot, M.L. The relationship between bariatric surgery and diet quality: A systematic review. Obes. Surg. 2020, 30, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Komorniak, N.; Szczuko, M.; Kowalewski, B.; Stachowska, E. Nutritional Deficiencies, Bariatric Surgery, and Serum Homocysteine Level: Review of Current Literature. Obes. Surg. 2019, 29, 3735–3742. [Google Scholar] [CrossRef] [PubMed]
- Algahtani, H.A.; Khan, A.S.; Khan, M.A.; Aldarmahi, A.A.; Lodhi, Y. Neurological complications of bariatric surgery. Neurosciences 2016, 21, 241–245. [Google Scholar] [CrossRef]
- Landais, A. Neurological complications of bariatric surgery. Obes. Surg. 2014, 24, 1800–1807. [Google Scholar] [CrossRef]
- Oudman, E.; Wijnia, J.W.; Van Dam, M.; Biter, L.U.; Postma, A. Preventing Wernicke Encephalopathy After Bariatric Surgery. Obes. Surg. 2018, 1–9. [Google Scholar] [CrossRef]
- Smelt, H.J.M.; Pouwels, S.; Smulders, J.F. Different supplementation regimes to treat perioperative vitamin B12 deficiencies in bariatric surgery: A systematic review. Obes. Surg. 2017, 27, 254–262. [Google Scholar] [CrossRef]
- Ledoux, S.; Msika, S.; Moussa, F.; Larger, E.; Boudou, P.; Salomon, L.; Roy, C.; Clerici, C. Comparison of nutritional consequences of conventional therapy of obesity, adjustable gastric banding, and gastric bypass. Obes. Surg. 2006, 16, 1041–1049. [Google Scholar] [CrossRef]
- Ledoux, S.; Coupaye, M.; Bogard, C.; Clerici, C.; Msika, S. Determinants of hyperhomocysteinemia after gastric bypass surgery in obese subjects. Obes. Surg. 2011, 21, 78–86. [Google Scholar] [CrossRef]
- Smelt, H.J.M.; Pouwels, S.; Smulders, J.F.; Hazebroek, E.J. Patient adherence to multivitamin supplementation after bariatric surgery: A narrative review. J. Nutr. Sci. 2020, 9, 9. [Google Scholar] [CrossRef]
- Homan, J.; Schijns, W.; Janssen, I.M.C.; Berends, F.J.; Aarts, E.O. Adequate multivitamin supplementation after Roux-En-Y gastric bypass results in a decrease of national health care costs: A cost-effectiveness analysis. Obes. Surg. 2019, 29, 1638–1643. [Google Scholar] [CrossRef]
- Dixon, J.B.; Dixon, M.E.; O’Brien, P.E. Elevated homocysteine levels with weight loss after Lap-Band® surgery: Higher folate and vitamin B 12 levels required to maintain homocysteine level. Int. J. Obes. 2001, 25, 219–227. [Google Scholar] [CrossRef] [PubMed]
- De Jager, C.A. Critical levels of brain atrophy associated with homocysteine and cognitive decline. Neurobiol. Aging 2014, 35, S35–S39. [Google Scholar] [CrossRef]
- Mikkelsen, K.; Stojanovska, L.; Tangalakis, K.; Bosevski, M.; Apostolopoulos, V. Cognitive decline: A vitamin B perspective. Maturitas 2016, 93, 108–113. [Google Scholar] [CrossRef]
- Reynolds, E. Vitamin B12, folic acid, and the nervous system. Lancet Neurol. 2006, 5, 949–960. [Google Scholar] [CrossRef]
- Gibson, G.E.; Hirsch, J.A.; Fonzetti, P.; Jordon, B.D.; Cirio, R.T.; Elder, J. Vitamin B1 (thiamine) and dementia. Ann. N. Y. Acad. Sci. 2016, 1367, 21. [Google Scholar] [CrossRef]
- Mitchell, J.E.; King, W.C.; Chen, J.Y.; Devlin, M.J.; Flum, D.; Garcia, L.; Inabet, W.; Pender, J.R.; Kalarchian, M.A.; Khandelwal, S. Course of depressive symptoms and treatment in the longitudinal assessment of bariatric surgery (LABS-2) study. Obesity 2014, 22, 1799–1806. [Google Scholar] [CrossRef] [PubMed]
- Alabi, F.; Guilbert, L.; Villalobos, G.; Mendoza, K.; Hinojosa, R.; Melgarejo, J.C.; Espinosa, O.; Sepúlveda, E.M.; Zerrweck, C. Depression before and after bariatric surgery in low-income patients: The utility of the beck depression inventory. Obes. Surg. 2018, 28, 3492–3498. [Google Scholar] [CrossRef] [PubMed]
- Dawes, A.J.; Maggard-Gibbons, M.; Maher, A.R.; Booth, M.J.; Miake-Lye, I.; Beroes, J.M.; Shekelle, P.G. Mental health conditions among patients seeking and undergoing bariatric surgery: A meta-analysis. JAMA 2016, 315, 150–163. [Google Scholar] [CrossRef]
- Fisher, D.; Coleman, K.J.; Arterburn, D.E.; Fischer, H.; Yamamoto, A.; Young, D.R.; Sherwood, N.E.; Trinacty, C.M.; Lewis, K.H. Mental illness in bariatric surgery: A cohort study from the PORTAL network. Obesity 2017, 25, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Castaneda, D.; Popov, V.B.; Wander, P.; Thompson, C.C. Risk of suicide and self-harm is increased after bariatric surgery—a systematic review and meta-analysis. Obes. Surg. 2019, 29, 322–333. [Google Scholar] [CrossRef]
- Morledge, M.D.; Pories, W.J. Mental Health in Bariatric Surgery: Selection, Access, and Outcomes. Obesity 2020, 28, 689–695. [Google Scholar] [CrossRef]
- Hamad, G.G.; Helsel, J.C.; Kozak, G.M.; McShea, M.C.; Hughes, C.; Confer, A.L.; McCloskey, C.A.; Sit, D.K.; Perel, J.M.; Wisner, K.L.P.U.o.P.P.P.A.U.S. P-35 The effect of gastric bypass on the pharmacokinetics of serotonin reuptake inhibitors. Surg. Obes. Relat. Dis. 2011, 7, 384. [Google Scholar] [CrossRef]
- Spirou, D.R.; Raman, J.; Smith, E. Psychological outcomes following surgical and endoscopic bariatric procedures: A systematic review. Obes. Rev. 2020, 21, e12998. [Google Scholar] [CrossRef]
- Sozer, K.; Gorgulu, Y.; Sonmez, M.B.; Kose Cinar, R. Psychotic depression after obesity surgery and recovery with vitamin B12 replacement. Dusunen Adam J. Psychiatry Neurol. Sci. 2019, 32, 65. [Google Scholar] [CrossRef]
- Ivezaj, V.; Grilo, C.M. When Mood Worsens after Gastric Bypass Surgery: Characterization of Bariatric Patients with Increases in Depressive Symptoms Following Surgery. Obes. Surger 2015, 25, 423–429. [Google Scholar] [CrossRef]
- Lewis, C.-A.; de Jersey, S.; Hopkins, G.; Hickman, I.; Osland, E. Does bariatric surgery cause vitamin A, B1, C or E deficiency? A systematic review. Obes. Surg. 2018, 28, 3640–3657. [Google Scholar] [CrossRef]
- Milone, M.; Di Minno, M.N.D.; Lupoli, R.; Maietta, P.; Bianco, P.; Pisapia, A.; Gaudioso, D.; Taffuri, C.; Milone, F.; Musella, M. Wernicke encephalopathy in subjects undergoing restrictive weight loss surgery: A systematic review of literature data. Eur. Eat. Disord. Rev. 2014, 22, 223–229. [Google Scholar] [CrossRef]
- Philippi, N.; Vinzio, S.; Collongues, N.; Vix, M.; Boehm, N.; Tranchant, C.; Echaniz-Laguna, A. Peripheral neuropathies after bariatric surgery. Rev. Neurol. 2011, 167, 607–614. [Google Scholar] [CrossRef]
- Thaisetthawatkul, P.; Collazo-Clavell, M.L.; Sarr, M.G.; Norell, J.E.; Dyck, P.J.B. A controlled study of peripheral neuropathy after bariatric surgery. Neurology 2004, 63, 1462–1470. [Google Scholar] [CrossRef]
- Mahawar, K.K.; Reid, A.; Graham, Y.; Callejas-Diaz, L.; Parmar, C.; Carr, W.R.J.; Jennings, N.; Singhal, R.; Small, P.K. Oral vitamin B 12 supplementation after Roux-en-Y gastric bypass: A systematic review. Obes. Surg. 2018, 28, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.C.; Vidal-Alaball, J.; Cannings-John, R.; McCaddon, A.; Hood, K.; Papaioannou, A.; McDowell, I.; Goringe, A. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: A systematic review of randomized controlled trials. Fam. Pract. 2006, 23, 279–285. [Google Scholar] [CrossRef]
- Quilliot, D.; Coupaye, M.; Ciangura, C.; Czernichow, S.; Sallé, A.; Gaborit, B.; Alligier, M.; Nguyen-Thi, P.L.; Dargent, J.; Msika, S. Recommendations for nutritional care after bariatric surgery: Recommendations for best practice and SOFFCO-MM/AFERO/SFNCM/expert consensus. J. Visc. Surg. 2021, 158, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.H. How common is vitamin B-12 deficiency? Am. J. Clin. Nutr. 2009, 89, 693S–696S. [Google Scholar] [CrossRef] [PubMed]
- Rhode, B.M.; Arseneau, P.; Cooper, B.A.; Katz, M.; Gilfix, B.M.; MacLean, L.D. Vitamin B-12 deficiency after gastric surgery for obesity. Am. J. Clin. Nutr. 1996, 63, 103–109. [Google Scholar] [CrossRef]
- Provenzale, D.; Reinhold, R.B.; Golner, B.; Irwin, V.; Dallal, G.E.; Papathanasopoulos, N.; Sahyoun, N.; Samloff, I.M.; Russell, R.M. Evidence for diminished B12 absorption after gastric bypass: Oral supplementation does not prevent low plasma B12 levels in bypass patients. J. Am. Coll. Nutr. 1992, 11, 29–35. [Google Scholar] [CrossRef]
- O’Kane, M.; Parretti, H.M.; Pinkney, J.; Welbourn, R.; Hughes, C.A.; Mok, J.; Walker, N.; Thomas, D.; Devin, J.; Coulman, K.D. British Obesity and Metabolic Surgery Society Guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery—2020 update. Obes. Rev. 2020, 21, e13087. [Google Scholar] [CrossRef]
- Nuzzo, A.; Czernichow, S.; Hertig, A.; Ledoux, S.; Poghosyan, T.; Quilliot, D.; Le Gall, M.; Bado, A.; Joly, F. Prevention and treatment of nutritional complications after bariatric surgery. Lancet Gastroenterol. Hepatol. 2021, 6, 238–251. [Google Scholar] [CrossRef]
- Schijns, W.; Homan, J.; van der Meer, L.; Janssen, I.M.; van Laarhoven, C.J.; Berends, F.J.; Aarts, E.O. Efficacy of oral compared with intramuscular vitamin B-12 supplementation after Roux-en-Y gastric bypass: A randomized controlled trial. Am. J. Clin. Nutr. 2018, 108, 6–12. [Google Scholar] [CrossRef]
- Kumari, A.; Nigam, A. Bariatric surgery in women: A boon needs special care during pregnancy. J. Clin. Diagn. Res. JCDR 2015, 9, QE01. [Google Scholar] [CrossRef]
- Wax, J.R.; Pinette, M.G.; Cartin, A.; Blackstone, J. Female reproductive issues following bariatric surgery. Obstet. Gynecol. Surv. 2007, 62, 595–604. [Google Scholar] [CrossRef]
- Kaska, L.; Kobiela, J.; Abacjew-Chmylko, A.; Chmylko, L.; Wojanowska-Pindel, M.; Kobiela, P.; Walerzak, A.; Makarewicz, W.; Proczko-Markuszewska, M.; Stefaniak, T. Nutrition and pregnancy after bariatric surgery. ISRB Obes. 2013, 2013, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Fullmer, M.A.; Abrams, S.H.; Hrovat, K.; Mooney, L.; Scheimann, A.O.; Hillman, J.B.; Suskind, D.L. Nutritional strategy for adolescents undergoing bariatric surgery: Report of a working group of the Nutrition Committee of NASPGHAN/NACHRI. J. Pediatric Gastroenterol. Nutr. 2012, 54, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Kominiarek, M.A. Preparing for and managing a pregnancy after bariatric surgery. Semin. Perinatol. 2011, 35, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.A.; Barger, M.K. Specialized care for women pregnant after bariatric surgery. J. Midwifery Women Health 2010, 55, 529–539. [Google Scholar] [CrossRef]
- Woodard, C.B. Pregnancy following bariatric surgery. J. Perinat. Neonatal Nurs. 2004, 18, 329–340. [Google Scholar] [CrossRef]
- Becker, D.A.B.; Laura, J.; Galetta, S.L. The Neurological Complications of Nutritional Deficiency following Bariatric Surgery. J. Obes. 2012, 2012, 608534. [Google Scholar] [CrossRef]
- Schroder, T.H.; Tan, A.; Mattman, A.; Sinclair, G.; Barr, S.I.; Vallance, H.D.; Lamers, Y. Reference intervals for serum total vitamin B12 and holotranscobalamin concentrations and their change points with methylmalonic acid concentration to assess vitamin B12 status during early and mid-pregnancy. Clin. Chem. Lab. Med. CCLM 2019, 57, 1790–1798. [Google Scholar] [CrossRef]
- Klee, G.G. Cobalamin and folate evaluation: Measurement of methylmalonic acid and homocysteine vs. vitamin B12 and folate. Clin. Chem. 2000, 46, 1277–1283. [Google Scholar] [CrossRef]
- Simoens, C.; Verbiest, A.; Brenninkmeijer, K.; Moyson, C.; Matthys, C.; Meulemans, A.; Lannoo, M.; Van der Schueren, B.; Mertens, A. Nonsurgical complications after bariatric surgery. Proc. Nutr. Soc. 2020, 79. [Google Scholar] [CrossRef]
| B Vitamins | Functions | Absorption Site | Deficiency Related Outcomes |
|---|---|---|---|
| B1 (Thiamine) [9,22] | Acetylcholine production, action potential generation, structure and function of cellular membranes | Duodenum Jejunum | Reduces enzymatic activity and energy production, alters mitochondrial activity |
| B2 (Riboflavin) [40] | Maintains the integrity of mucous membranes, skin, eyes, and the nervous system | Duodenum Jejunum | Mitochondrial dysfunction, effects one-carbon metabolism |
| B3 (Niacin) [41,42] | Acts as an antioxidant, produces energy, protects against axonal damage, neuroprotective role | Duodenum Jejunum | Increases oxidative stress and inflammatory cytokines, mitochondrial dysfunction |
| B5 (Pantothenic acid) [43] | Regulates iron by transporting oxygen to the brain, synthesizes neurotransmitters, helps in the synthesis and regeneration of myelin | Jejunum | Increased cell stress and translocation of NF-κB, altered fatty acid metabolism |
| B6 (Pyridoxine) [22,28] | Assists in the synthesis of hemoglobin, neurotransmitters, DNA methylation, and homocysteine metabolism | Jejunum | Altered tryptophan and one-carbon metabolism |
| B9 (Folate) [44] | Synthesizes norepinephrine, dopamine, and serotonin. Involved in methylation of homocysteine to methionine | Duodenum Jejunum Ileum | Disrupts DNA methylation and alters nitric-oxide balance in the blood |
| B12 (Cobalamin) [45,46,47] | Synthesizes new cells, involved in nerve cells maintenance, assists in breaking fatty acids and amino acids | Ileum (terminal only) | Effects on DNA synthesis, adverse effects on brain function |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Mansoori, A.; Shakoor, H.; Ali, H.I.; Feehan, J.; Al Dhaheri, A.S.; Cheikh Ismail, L.; Bosevski, M.; Apostolopoulos, V.; Stojanovska, L. The Effects of Bariatric Surgery on Vitamin B Status and Mental Health. Nutrients 2021, 13, 1383. https://doi.org/10.3390/nu13041383
Al Mansoori A, Shakoor H, Ali HI, Feehan J, Al Dhaheri AS, Cheikh Ismail L, Bosevski M, Apostolopoulos V, Stojanovska L. The Effects of Bariatric Surgery on Vitamin B Status and Mental Health. Nutrients. 2021; 13(4):1383. https://doi.org/10.3390/nu13041383
Chicago/Turabian StyleAl Mansoori, Amna, Hira Shakoor, Habiba I. Ali, Jack Feehan, Ayesha S. Al Dhaheri, Leila Cheikh Ismail, Marijan Bosevski, Vasso Apostolopoulos, and Lily Stojanovska. 2021. "The Effects of Bariatric Surgery on Vitamin B Status and Mental Health" Nutrients 13, no. 4: 1383. https://doi.org/10.3390/nu13041383
APA StyleAl Mansoori, A., Shakoor, H., Ali, H. I., Feehan, J., Al Dhaheri, A. S., Cheikh Ismail, L., Bosevski, M., Apostolopoulos, V., & Stojanovska, L. (2021). The Effects of Bariatric Surgery on Vitamin B Status and Mental Health. Nutrients, 13(4), 1383. https://doi.org/10.3390/nu13041383












