The INTER-ACT E-Health Supported Lifestyle Intervention Improves Postpartum Food Intake and Eating Behavior, but Not Physical Activity and Sedentary Behavior—A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
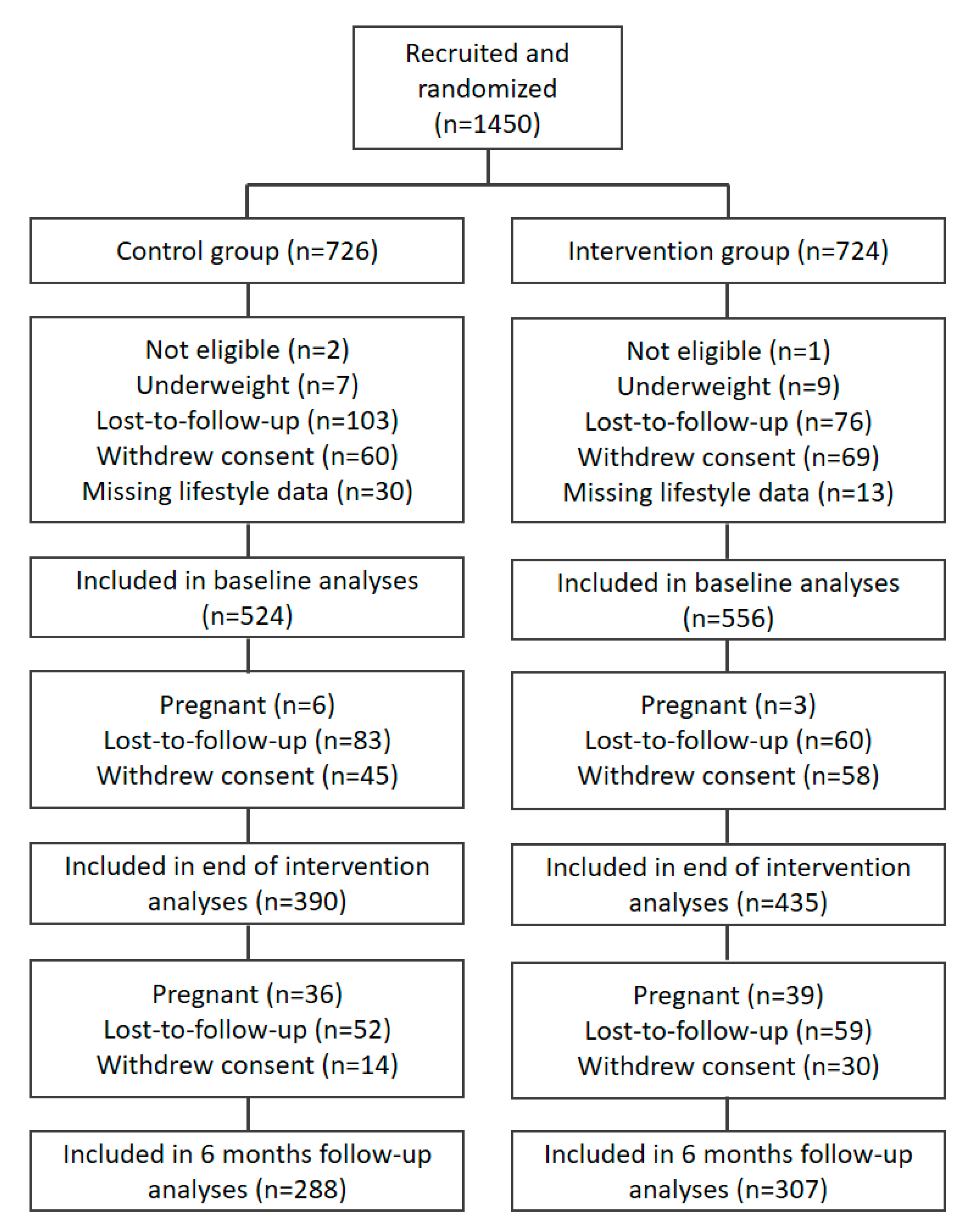
2.1. Participants
2.2. Randomization
2.3. Intervention
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Eating Behavior and Food Intake
3.2. Physical Activity and Sedentary Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- DiPietro, L.; Evenson, K.R.; Bloodgood, B.; Sprow, K.; Troiano, R.P.; Piercy, K.L.; Vaux-Bjerke, A.; Powell, K.E. Benefits of Physical Activity during Pregnancy and Postpartum: An Umbrella Review. Med. Sci. Sports Exerc. 2019, 51, 1292–1302. [Google Scholar] [CrossRef]
- Harrison, C.L.; Brown, W.J.; Hayman, M.; Moran, L.J.; Redman, L.M. The Role of Physical Activity in Preconception, Pregnancy and Postpartum Health. Semin. Reprod. Med. 2016, 34, e28–e37. [Google Scholar] [CrossRef]
- Koletzko, B.; Godfrey, K.M.; Poston, L.; Szajewska, H.; van Goudoever, J.B.; de Waard, M.; Brands, B.; Grivell, R.M.; Deussen, A.R.; Dodd, J.M.; et al. Nutrition During Pregnancy, Lactation and Early Childhood and its Implications for Maternal and Long-Term Child Health: The Early Nutrition Project Recommendations. Ann. Nutr. Metab. 2019, 74, 93–106. [Google Scholar] [CrossRef]
- Stang, J.; Huffman, L.G. Position of the Academy of Nutrition and Dietetics: Obesity, Reproduction, and Pregnancy Outcomes. J. Acad. Nutr. Diet. 2016, 116, 677–691. [Google Scholar] [CrossRef] [PubMed]
- Hoover, E.A.; Louis, J.M. Optimizing Health: Weight, Exercise, and Nutrition in Pregnancy and Beyond. Obstet. Gynecol. Clin. N. Am. 2019, 46, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.A.; Hutchinson, J.; Cade, J.E.; Poston, L.; Barrett, G.; Crozier, S.R.; Barker, M. Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef]
- Teulings, N.E.; Masconi, K.L.; Ozanne, S.E.; Aiken, C.E.; Wood, A.M. Effect of interpregnancy weight change on perinatal outcomes: Systematic review and meta-analysis. BMC Pregnancy Childbirth 2019, 19, 386. [Google Scholar] [CrossRef] [PubMed]
- Poston, L.; Caleyachetty, R.; Cnattingius, S.; Corvalán, C.; Uauy, R.; Herring, S.; Gillman, M.W. Preconceptional and maternal obesity: Epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016, 4, 1025–1036. [Google Scholar] [CrossRef]
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Boyle, J.A.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L. Association of gestational weight gain with maternal and infant outcomes: A systematic review and meta-analysis. JAMA 2017, 317, 2207–2225. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine; National Research Council Committee to Reexamine IOM Pregnancy Weight Guidelines. The National Academies Collection: Reports funded by National Institutes of Health. In Weight Gain During Pregnancy: Reexamining the Guidelines; Rasmussen, K.M., Yaktine, A.L., Eds.; National Academies Press (US): Washington, DC, USA, 2009. [Google Scholar] [CrossRef]
- Bogaerts, A.; Van den Bergh, B.; Nuyts, E.; Martens, E.; Witters, I.; Devlieger, R. Socio-demographic and obstetrical correlates of pre-pregnancy body mass index and gestational weight gain. Clin. Obes. 2012, 2, 150–159. [Google Scholar] [CrossRef]
- Deputy, N.P.; Sharma, A.J.; Kim, S.Y.; Hinkle, S.N. Prevalence and characteristics associated with gestational weight gain adequacy. Obstet. Gynecol. 2015, 125, 773. [Google Scholar] [CrossRef]
- Dalrymple, K.V.; Flynn, A.C.; Relph, S.A.; O’Keeffe, M.; Poston, L. Lifestyle Interventions in Overweight and Obese Pregnant or Postpartum Women for Postpartum Weight Management: A Systematic Review of the Literature. Nutrients 2018, 10, 1704. [Google Scholar] [CrossRef]
- Mertens, L.; Braeken, M.A.; Bogaerts, A. Effect of lifestyle coaching including telemonitoring and telecoaching on gestational weight gain and postnatal weight loss: A systematic review. Telemed. E-Health 2019, 25, 889–901. [Google Scholar] [CrossRef]
- Bogaerts, A.; Ameye, L.; Bijlholt, M.; Amuli, K.; Heynickx, D.; Devlieger, R. INTER-ACT: Prevention of pregnancy complications through an e-health driven interpregnancy lifestyle intervention–study protocol of a multicentre randomised controlled trial. BMC Pregnancy Childbirth 2017, 17, 154. [Google Scholar] [CrossRef] [PubMed]
- Bogaerts, A.; Bijlholt, M.; Mertens, L.; Braeken, M.; Jacobs, B.; Vandenberghe, B.; Ameye, L.; Devlieger, R. Development and Field Evaluation of the INTER-ACT App, a Pregnancy and Interpregnancy Coaching App to Reduce Maternal Overweight and Obesity: Mixed Methods Design. JMIR Form. Res. 2020, 4, e16090. [Google Scholar] [CrossRef]
- Matthys, C.; Meulemans, A.; Van der Schueren, B. Development and validation of general FFQ for use in clinical practice. Ann. Nutr. Metab. 2015, 67, 239. [Google Scholar]
- Karlsson, J.; Persson, L.-O.; Sjöström, L.; Sullivan, M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int. J. Obes. 2000, 24, 1715–1725. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Bijlholt, M.; Van Uytsel, H.; Ameye, L.; Devlieger, R.; Bogaerts, A. Eating behaviors in relation to gestational weight gain and postpartum weight retention: A systematic review. Obes. Rev. 2020, 21, e13047. [Google Scholar] [CrossRef]
- Farpour-Lambert, N.J.; Ells, L.J.; Martinez de Tejada, B.; Scott, C. Obesity and Weight Gain in Pregnancy and Postpartum: An Evidence Review of Lifestyle Interventions to Inform Maternal and Child Health Policies. Front. Endocrinol. 2018, 9, 546. [Google Scholar] [CrossRef]
- Anschutz, D.J.; Van Strien, T.; Van De Ven, M.O.; Engels, R.C. Eating styles and energy intake in young women. Appetite 2009, 53, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Turner-McGrievy, G.; Davidson, C.R.; Billings, D.L. Dietary intake, eating behaviors, and quality of life in women with polycystic ovary syndrome who are trying to conceive. Hum. Fertil. 2015, 18, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Paans, N.P.G.; Gibson-Smith, D.; Bot, M.; van Strien, T.; Brouwer, I.A.; Visser, M.; Penninx, B. Depression and eating styles are independently associated with dietary intake. Appetite 2019, 134, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Schaumberg, K.; Anderson, D.; Anderson, L.; Reilly, E.; Gorrell, S. Dietary restraint: What’s the harm? A review of the relationship between dietary restraint, weight trajectory and the development of eating pathology. Clin. Obes. 2016, 6, 89–100. [Google Scholar] [CrossRef]
- Bashirian, S.; Ouji, Z.; Afshari, M.; Barati, M.; Heydarimoghadam, R.; Soltanian, A. Effect of an Educational Intervention Based on the BASNEF Model on Promoting Physical Activity Among Postpartum Women. Int. Q. Community Health Educ. 2020, 40, 151–158. [Google Scholar] [CrossRef]
- Maturi, M.S.; Afshary, P.; Abedi, P. Effect of physical activity intervention based on a pedometer on physical activity level and anthropometric measures after childbirth: A randomized controlled trial. BMC Pregnancy Childbirth 2011, 11, 103. [Google Scholar] [CrossRef]
- Phelan, S.; Hagobian, T.; Brannen, A.; Hatley, K.E.; Schaffner, A.; Muñoz-Christian, K.; Tate, D.F. Effect of an Internet-Based Program on Weight Loss for Low-Income Postpartum Women: A Randomized Clinical Trial. JAMA 2017, 317, 2381–2391. [Google Scholar] [CrossRef]
- Bogaerts, A.; Van den Bergh, B.R.; Ameye, L.; Witters, I.; Martens, E.; Timmerman, D.; Devlieger, R. Interpregnancy weight change and risk for adverse perinatal outcome. Obstet. Gynecol. 2013, 122, 999–1009. [Google Scholar] [CrossRef]
- Park, Y.; Dodd, K.W.; Kipnis, V.; Thompson, F.E.; Potischman, N.; Schoeller, D.A.; Baer, D.J.; Midthune, D.; Troiano, R.P.; Bowles, H. Comparison of self-reported dietary intakes from the Automated Self-Administered 24-h recall, 4-d food records, and food-frequency questionnaires against recovery biomarkers. Am. J. Clin. Nutr. 2018, 107, 80–93. [Google Scholar] [CrossRef] [PubMed]
| Overall N = 1046 | Control Group N = 504 | Intervention Group N = 542 | |
|---|---|---|---|
| Age, mean (SD) | 31.3 (3.9) | 31.4 (3.8) | 31.2 (3.9) |
| Highest education, n (percent) | |||
| Up to secondary education | 296 (28.4) | 144 (28.8) | 152 (28.1) |
| College | 405 (38.9) | 196 (39.2) | 209 (38.6) |
| University | 340 (32.7) | 160 (32) | 180 (33.3) |
| Missing | 5 | 4 | 1 |
| Parity, n (percent) | |||
| Primiparous | 577 (55.2) | 286 (56.7) | 291 (53.7) |
| Multiparous | 469 (44.8) | 218 (43.3) | 251 (46.3) |
| Sex of infant, n (percent) | |||
| Boy | 554 (53) | 263 (52.2) | 291 (53.7) |
| Girl | 492 (47) | 241 (47.8) | 251 (46.3) |
| Method of conception, n (percent) a | |||
| Spontaneous | 918 (90.1) | 455 (92.1) | 463 (88.2) |
| Assisted reproductive technology | 101 (9.9) | 39 (7.9) | 62 (11.8) |
| Missing | 27 | 10 | 17 |
| Pre-pregnancy BMI category, n (percent) | |||
| Normal weight | 509 (48.7) | 249 (49.4) | 260 (48) |
| Overweight | 374 (35.8) | 181 (35.9) | 193 (35.6) |
| Obesity | 163 (15.6) | 74 (14.7) | 89 (16.4) |
| Gestational weight gain in kg, median (IQR) | |||
| Among normal weight b | 18.5 (17–20.9) | 19 (17–21) | 18 (17–20) |
| Among overweight | 16 (13.5–19) | 16 (13–18.9) | 16 (14–19) |
| Among obese | 14 (12–17) | 14 (12–17) | 14 (11.3–17) |
| Outcome | Time Point | BMI Group a | Univariate Analyses | Multivariate Analyses | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control Group | Intervention Group | p-Value b | n | p-Value c | ||||||
| n | Mean (SD), Median (Q1–Q3) or n (%) | n | Mean (SD), Median (Q1–Q3) or n (%) | Mean Difference (95% CI) or OR (95% CI) | ||||||
| Restrained eating | Baseline (6 weeks PP) | Overall | 513 | 13.4 (3.4) | 550 | 13.3 (3.3) | ||||
| NW | 252 | 13.6 (3.6) | 259 | 13.5 (3.3) | ||||||
| OW | 188 | 13.3 (3.1) | 200 | 13.1 (3.3) | ||||||
| OB | 73 | 13.3 (3.2) | 91 | 13.3 (3.1) | ||||||
| End of intervention (6 months PP) | Overall | 377 | 14.3 (3.5) | 374 | 15.3 (3.5) | <0.001 | 729 | 1.0 (0.5 to 1.5) | <0.001 | |
| NW | 199 | 14.1 (3.8) | 187 | 15.4 (3.7) | 0.001 | 375 | 1.4 (0.6 to 2.1) | <0.001 | ||
| OW | 125 | 14.7 (3.1) | 137 | 15.2 (3.5) | 0.19 | 253 | 0.5 (−0.3 to 1.3) | 0.23 | ||
| OB | 53 | 14.1 (3.3) | 50 | 15.2 (3.3) | 0.08 | 96 | 0.4 (−0.8 to 1.6) | 0.54 | ||
| 6-month follow-up (12 months PP) | Overall | 285 | 14.5 (3.6) | 276 | 14.8 (3.2) | 0.19 | 558 | 0.5 (−0.1 to 1.1) | 0.10 | |
| NW | 148 | 14.0 (3.7) | 133 | 14.9 (3.2) | 0.04 | 268 | 1.3 (0.5 to 2.1) | 0.001 | ||
| OW | 99 | 14.9 (3.2) | 110 | 14.7 (3.3) | 0.77 | 203 | 0.0 (−0.9 to 0.9) | 0.97 | ||
| OB | 38 | 15.3 (4.1) | 33 | 15.2 (3.3) | 0.85 | 68 | −0.3 (−2.1 to 1.5) | 0.73 | ||
| Uncontrolled eating | Baseline (6 weeks PP) | Overall | 513 | 20.2 (5.5) | 550 | 20.4 (5.5) | ||||
| NW | 252 | 19.5 (5.4) | 259 | 19.1 (5.1) | ||||||
| OW | 188 | 20.3 (5.4) | 200 | 21.6 (5.6) | ||||||
| OB | 73 | 22.5 (5.6) | 91 | 21.7 (5.5) | ||||||
| End of intervention (6 months PP) | Overall | 377 | 20.6 (5.9) | 374 | 19.6 (5.6) | 0.02 | 729 | −1.0 (−1.9 to −0.2) | 0.02 | |
| NW | 199 | 19.8 (5.7) | 187 | 18.1 (5.1) | 0.003 | 375 | −1.6 (−2.7 to −0.5) | 0.004 | ||
| OW | 125 | 20.6 (5.7) | 137 | 20.9 (5.7) | 0.67 | 253 | 0.13 (−1.3 to 1.6) | 0.86 d | ||
| OB | 53 | 23.8 (6.1) | 50 | 21.8 (5.8) | 0.09 | 101 | −1.6 (−4.0 to 0.8) | 0.19 | ||
| 6-month follow-up (12 months PP) | Overall | 286 | 19.7 (5.6) | 276 | 19.7 (5.7) | 0.88 | 559 | 0.0 (−0.9 to 0.9) | 0.85 | |
| NW | 149 | 19.0 (5.2) | 133 | 18.1 (5.2) | 0.18 | 278 | −1.0 (−2.2 to 0.2) | 0.09 | ||
| OW | 99 | 19.4 (5.3) | 110 | 21.3 (6.1) | 0.02 | 194 | 2.2 (0.7 to 3.7) | 0.006d | ||
| OB | 38 | 23.0 (6.6) | 33 | 21.0 (5.3) | 0.18 | 71 | −2.1 (−5.0 to 0.9) | 0.18 | ||
| Emotional eating, continuous | Baseline (6 weeks PP) | Overall | 513 | 6.0 (4.0–8.0) | 550 | 6.0 (4.0–9.0) | ||||
| NW | 252 | 5.0 (3.0–8.0) | 259 | 5.0 (3.0–8.0) | ||||||
| OW | 188 | 6.0 (5.0–9.0) | 200 | 7.0 (5.0–9.0) | ||||||
| OB | 73 | 8.0 (5.5–9.5) | 91 | 8.0 (6.0–10.0) | ||||||
| End of intervention (6 months PP) | Overall | 377 | 6.0 (4.0–9.0) | 374 | 6.0 (4.0–9.0) | 0.88 | ||||
| NW | 199 | 5.0 (3.0–8.0) | 187 | 5.0 (3.0–8.0) | 0.83 | |||||
| OW | 125 | 6.0 (4.5–9.0) | 137 | 7.0 (4.0–9.0) | 0.82 | |||||
| OB | 53 | 9.0 (5.0–10.5) | 50 | 8.0 (6.0–10.0) | 0.93 | |||||
| 6-month follow-up (12 months PP) | Overall | 286 | 6.0 (4.0–8.0) | 276 | 6.0 (4.0–9.0) | 0.26 | ||||
| NW | 149 | 6.0 (4.0–7.0) | 133 | 5.0 (3.0–8.0) | 0.50 | |||||
| OW | 99 | 7.0 (4.0–9.0) | 110 | 7.0 (5.0–10.0) | 0.07 | |||||
| OB | 38 | 8.0 (5.0–11.0) | 33 | 8.0 (5.5–9.5) | 0.90 | |||||
| High emotional eating (score > 6) | Baseline (6 weeks PP) | Overall | 513 | 221 (43.1%) | 550 | 264 (48.0%) | ||||
| NW | 252 | 84 (33.3%) | 259 | 89 (34.4%) | ||||||
| OW | 188 | 90 (47.9%) | 200 | 115 (57.5%) | ||||||
| OB | 73 | 47 (64.4%) | 91 | 60 (65.9%) | ||||||
| End of intervention (6 months PP) | Overall | 377 | 165 (43.8%) | 374 | 169 (45.2%) | 0.70 | 729 | 1.04 (0.78 to 1.40) | 0.78 | |
| NW | 199 | 68 (34.2%) | 187 | 63 (33.7%) | 0.92 | 375 | 0.94 (0.61 to 1.45) | 0.79 | ||
| OW | 125 | 59 (47.2%) | 137 | 73 (53.3%) | 0.33 | 253 | 1.21 (0.73 to 1.99) | 0.46 e | ||
| OB | 53 | 38 (71.7%) | 50 | 33 (66%) | 0.53 | 101 | 0.80 (0.34 to 1.87) | 0.60 | ||
| 6-month follow-up (12 months PP) | Overall | 286 | 128 (44.8%) | 276 | 131 (47.5%) | 0.52 | 559 | 1.12 (0.80 to 1.56) | 0.52 | |
| NW | 149 | 54 (36.2%) | 133 | 46 (34.6%) | 0.77 | 285 | 0.93 (0.56 to 1.52) | 0.76 | ||
| OW | 99 | 50 (50.5%) | 110 | 61 (55.5%) | 0.47 | 203 | 1.18 (0.67 to 2.05) | 0.57 e | ||
| OB | 38 | 24 (63.2%) | 33 | 24 (72.7%) | 0.39 | 71 | 1.44 (0.51 to 4.05) | 0.49 | ||
| Energy intake (kcal) | Baseline (6 weeks PP) | Overall | 517 | 1399 (378) | 553 | 1409 (414) | ||||
| NW | 254 | 1351 (344) | 262 | 1398 (430) | ||||||
| OW | 189 | 1443 (414) | 200 | 1390 (356) | ||||||
| OB | 74 | 1448 (376) | 91 | 1482 (475) | ||||||
| End of intervention (6 months PP) | Overall | 378 | 1277 (375) | 377 | 1204 (364) | 0.006 | 732 | −69 (−123 to −15) | 0.01 | |
| NW | 199 | 1249 (381) | 189 | 1199 (390) | 0.20 | 377 | −43 (−121 to 36) | 0.30 | ||
| OW | 126 | 1277 (361) | 138 | 1201 (325) | 0.07 | 254 | −75 (−161 to 11) | 0.09 | ||
| OB | 53 | 1385 (372) | 50 | 1230 (372) | 0.04 | 94 | −174 (−314 to −35) | 0.01 | ||
| 6-month follow-up (12 months PP) | Overall | 286 | 1174 (339) | 279 | 1172 (333) | 0.95 | 562 | −1 (−62 to 59) | 0.96 | |
| NW | 149 | 1139 (324) | 135 | 1146 (313) | 0.85 | 287 | 15 (−70 to 101) | 0.74 | ||
| OW | 99 | 1208 (361) | 110 | 1224 (343) | 0.75 | 199 | 28 (−68 to 125) | 0.57 | ||
| OB | 38 | 1220 (328) | 34 | 1106 (361) | 0.17 | 69 | −138 (−296 to 20) | 0.09 | ||
| Physical activity (MET-minutes per week) | Baseline (6 weeks PP) | Overall | 487 | 1857 (891–3438) | 533 | 1728 (920–3279) | ||||
| NW | 236 | 1785 (892–3525) | 252 | 1685 (787–3070) | ||||||
| OW | 182 | 1924 (918–3030) | 191 | 1837 (1118–3143) | ||||||
| OB | 69 | 1860 (848–3725) | 90 | 1899 (836–3673) | ||||||
| End of intervention (6 months PP) | Overall | 344 | 2461 (1342–4691) | 340 | 2640 (1372–5397) | 0.40 | 649 | 0.052 (−0.099 to 0.203) f | 0.50 | |
| NW | 182 | 2406 (1372–4595) | 168 | 2634 (1325–5294) | 0.65 | 333 | 0.062 (−0.145 to 0.270) f | 0.56 | ||
| OW | 114 | 2681 (1319–4593) | 131 | 2547 (1299–5876) | 0.98 | 230 | −0.036 (−0.296 to 0.223) f | 0.78 | ||
| OB | 48 | 2491 (1167–5315) | 41 | 3032 (2070–4867) | 0.30 | 75 | 0.104 (−0.292 to 0.501) f | 0.60 | ||
| 6-month follow-up (12 months PP) | Overall | 269 | 2403 (1240–4543) | 261 | 2814 (1501–5312) | 0.11 | 497 | 0.144 (−0.025 to 0.313) f | 0.09 | |
| NW | 143 | 2616 (1107–4650) | 128 | 2519 (1392–4103) | 0.11 | 251 | −0.018 (−0.256 to 0.220) f | 0.88 | ||
| OW | 94 | 2132 (1417–4072) | 101 | 3210 (1530–6293) | 0.70 | 181 | 0.265 (−0.001 to 0.531) f | 0.053 | ||
| OB | 32 | 2255 (860–4576) | 32 | 3236 (1789–5412) | 0.06 | 61 | 0.413 (−0.128 to 0.953) f | 0.14 | ||
| Sedentary time (minutes per day) | Baseline (6 weeks PP) | Overall | 486 | 325 (171) | 532 | 323 (180) | ||||
| NW | 235 | 325 (183) | 252 | 313 (171) | ||||||
| OW | 182 | 324 (151) | 191 | 332 (193) | ||||||
| OB | 69 | 326 (180) | 89 | 330 (178) | ||||||
| End of intervention (6 months PP) | Overall | 343 | 308 (167) | 338 | 293 (162) | 0.21 | 661 | −14 (−39 to 12) | 0.30 | |
| NW | 182 | 319 (161) | 167 | 299 (170) | 0.26 | 339 | −21 (−57 to 15) | 0.26 | ||
| OW | 113 | 310 (179) | 130 | 286 (163) | 0.28 | 232 | −24 (−65 to 18) | 0.29 | ||
| OB | 48 | 266 (160) | 41 | 288 (120) | 0.46 | 81 | 31 (−28 to 90) | 0.30 | ||
| 6-month follow-up (12 months PP) | Overall | 269 | 317 (160) | 261 | 299 (173) | 0.22 | 511 | −17 (−46 to 13) | 0.28 | |
| NW | 143 | 319 (158) | 128 | 287 (155) | 0.09 | 263 | −33 (−72 to 6) | 0.12 | ||
| OW | 94 | 311 (157) | 101 | 302 (182) | 0.74 | 178 | −17 (−61 to 26) | 0.43 | ||
| OB | 32 | 321 (176) | 32 | 334 (213) | 0.79 | 58 | −3 (−90 to 85) | 0.95 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bijlholt, M.; Ameye, L.; Van Uytsel, H.; Devlieger, R.; Bogaerts, A. The INTER-ACT E-Health Supported Lifestyle Intervention Improves Postpartum Food Intake and Eating Behavior, but Not Physical Activity and Sedentary Behavior—A Randomized Controlled Trial. Nutrients 2021, 13, 1287. https://doi.org/10.3390/nu13041287
Bijlholt M, Ameye L, Van Uytsel H, Devlieger R, Bogaerts A. The INTER-ACT E-Health Supported Lifestyle Intervention Improves Postpartum Food Intake and Eating Behavior, but Not Physical Activity and Sedentary Behavior—A Randomized Controlled Trial. Nutrients. 2021; 13(4):1287. https://doi.org/10.3390/nu13041287
Chicago/Turabian StyleBijlholt, Margriet, Lieveke Ameye, Hanne Van Uytsel, Roland Devlieger, and Annick Bogaerts. 2021. "The INTER-ACT E-Health Supported Lifestyle Intervention Improves Postpartum Food Intake and Eating Behavior, but Not Physical Activity and Sedentary Behavior—A Randomized Controlled Trial" Nutrients 13, no. 4: 1287. https://doi.org/10.3390/nu13041287
APA StyleBijlholt, M., Ameye, L., Van Uytsel, H., Devlieger, R., & Bogaerts, A. (2021). The INTER-ACT E-Health Supported Lifestyle Intervention Improves Postpartum Food Intake and Eating Behavior, but Not Physical Activity and Sedentary Behavior—A Randomized Controlled Trial. Nutrients, 13(4), 1287. https://doi.org/10.3390/nu13041287







