Bisphenol S in Food Causes Hormonal and Obesogenic Effects Comparable to or Worse than Bisphenol A: A Literature Review
Abstract
1. Introduction
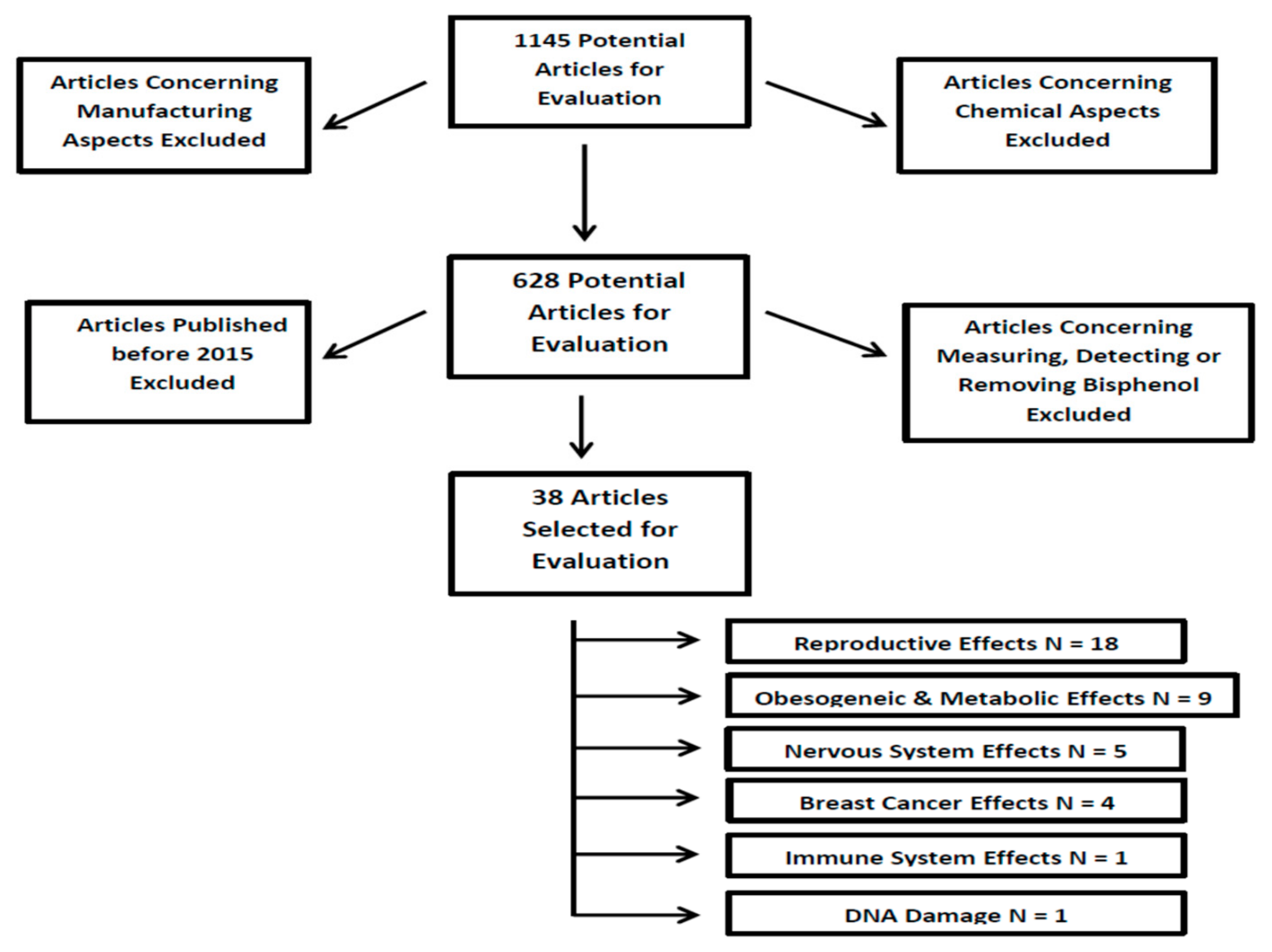
2. Methods and Study Design
3. Results
3.1. Dietary BPS Exposure and Reproduction
3.2. Dietary BPS Exposure and Obesogenic Effects/Metabolic Disorders
3.3. Dietary BPS Exposure and Breast Cancer
3.4. Dietary BPS Exposure and the Nervous System
3.5. Dietary BPS Exposure, DNA Damage, and the Immune System
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| BPA | Bisphenol A |
| BPB | Bisphenol B |
| BPS | Bisphenol S |
| BPF | Bisphenol F |
| BPE | Bisphenol E |
| BPAF | Bisphenol AF |
| BPAP | Bisphenol AP |
| BPP | Bisphenol P |
| BPZ | Bisphenol Z |
| CRH | Corticotropin Releasing Hormone |
| GDM | Gestational Diabetes Mellitus |
| EMT | Epethelial Mesenchymal Transition |
| ERα | Estrogen Receptor alpha |
| LD | Lactation Day |
| PPARG | Peroxisome proliferator-activated receptor gamma |
| VEGF gene | vascular endothelial growth factor gene |
References
- Reif, D.M.; Martin, M.T.; Tan, S.W.; Houck, K.A.; Judson, R.S.; Richard, A.M.; Knudsen, T.B.; Dix, D.J.; Kavlock, R.J. Endocrine profiling and prioritization of environmental chemicals using ToxCast data. Environ. Health Perspect. 2010, 118, 1714–1720. [Google Scholar] [CrossRef] [PubMed]
- Beronius, A.; Ruden, C.; Hakansson, H.; Hanberg, A. Risk to all or none? A comparativeanalysis of controversies in the health risk assessment of Bisphenol A. Reprod. Toxicol. 2010, 29, 132–146. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, L.S.; Bucher, J.R.; Collman, G.W.; Zeldin, D.C.; Johnson, A.F.; Schug, T.T.; Heindel, J.J. Consortium-based science: The NIEHS’s multipronged, collaborative approach to assessing the health effects of bisphenol A. Environ. Health Perspect. 2012, 120, 1640–1644. [Google Scholar] [CrossRef] [PubMed]
- Vandenberg, L.N.; Ehrlich, S.; Belcher, S.M.; Ben-Jonathan, N.; Dolinoy, D.C.; Hugo, E.R.; Hunt, P.A.; Newbold, R.R.; Rubin, B.S.; Saili, K.S.; et al. Low dose effects of bisphenol A. Endocrine Disruptors 2013, 1, e26490. [Google Scholar] [CrossRef]
- MunckafRosenschöld, J.; Honkela, N.; Hukkinen, J.I. Addressing the temporal fit of institutions: The regulation of endocrine-disrupting chemicals in Europe. Ecol. Soc. 2014, 19, 30. [Google Scholar] [CrossRef]
- Wu, L.H.; Zhang, X.M.; Wang, F.; Gao, C.J.; Chen, D.; Palumbo, J.R.; Guo, Y.; Zeng, E.Y. Occurrence of bisphenol S in the environment and implications for human exposure: A short review. Sci. Total Environ. 2017, 615, 87–98. [Google Scholar] [CrossRef]
- Andújar, N.; Gálvez-Ontiveros, Y.; Zafra-Gómez, A.; Rodrigo, L.; Álvarez-Cubero, M.J.; Aguilera, M.; Monteagudo, C.; Rivas, A. Bisphenol A Analogues in Food and Their Hormonal and Obesogenic Effects: A Review. Nutrients 2019, 11, 2136. [Google Scholar] [CrossRef]
- Björnsdotter, M.K.; de Boer, J.; Ballesteros-Gómez, A. Bisphenol A and replacements in thermal paper: A review. Chemosphere 2017, 182, 691–706. [Google Scholar] [CrossRef]
- Kuruto-Niwa, R.; Nozawa, R.; Miyakoshi, T.; Shiozawa, T.; Terao, Y. Estrogenic activity of alkylphenols, bisphenol S, and their chlorinated derivatives using a GFP expression system. Environ. Toxicol. Pharmacol. 2005, 19, 121–130. [Google Scholar] [CrossRef]
- Liao, C.; Liu, F.; Alomirah, H.; Loi, V.D.; Mohd, M.A.; Moon, H.B.; Nakata, H.; Kannan, K. Bisphenol S in urine from the United States and seven Asian countries: Occurrence and human exposures. Environ. Sci. Technol. 2012, 46, 6860–6866. [Google Scholar] [CrossRef]
- Rochester, J.R.; Bolden, A.L. Bisphenol S and F: A Systematic Review and Comparison of the Hormonal Activity of Bisphenol A Substitutes. Environ. Health Perspect. 2015, 123, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Moreman, J.; Lee, O.; Trznadel, M.; David, A.; Kudoh, T.; Tyler, C.R. Acute Toxicity, Teratogenic, and Estrogenic Effects of Bisphenol A and Its Alternative Replacements Bisphenol S, Bisphenol F, and Bisphenol AF in Zebrafish Embryo-Larvae. Environ. Sci. Technol. 2017, 51, 12796–12805. [Google Scholar] [CrossRef] [PubMed]
- Catron, T.R.; Keely, S.P.; Brinkman, N.E.; Zurlinden, T.J.; Wood, C.E.; Wright, J.R.; Phelps, D.; Wheaton, E.; Kvasnicka, A.; Gaballah, S.; et al. Host Developmental Toxicity of BPA and BPA Alternatives Is Inversely Related to Microbiota Disruption in Zebrafish. Toxicol. Sci. 2019, 167, 468–483. [Google Scholar] [CrossRef] [PubMed]
- Qiu, W.; Zhao, Y.; Yang, M.; Farajzadeh, M.; Pan, C.; Wayne, N.L. Actions of Bisphenol A and Bisphenol S on the Reproductive Neuroendocrine System During Early Development in Zebrafish. Endocrinology 2016, 157, 636–647. [Google Scholar] [CrossRef] [PubMed]
- Kinch, C.D.; Ibhazehiebo, K.; Jeong, J.H.; Habibi, H.R.; Kurrasch, D.M. BPA and replacement BPS alters neurogenesis. Proc. Natl. Acad. Sci. USA 2015, 112, 1475–1480. [Google Scholar] [CrossRef] [PubMed]
- Roelofs, M.J.; van den Berg, M.; Bovee, T.F.; Piersma, A.H.; van Duursen, M.B. Structural bisphenol analogues differentially target steroidogenesis in murine MA-10 Leydig cells as well as the glucocorticoid receptor. Toxicology 2015, 329, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.; Yin, L.; Shengyang Yu, K.; Hofmann, M.C.; Yu, X. High-Content Analysis Provides Mechanistic Insights into the Testicular Toxicity of Bisphenol A and Selected Analogues in Mouse Spermatogonial Cells. Toxicol. Sci. 2017, 155, 43–60. [Google Scholar] [CrossRef] [PubMed]
- LaPlante, C.D.; Catanese, M.C.; Bansal, R.; Vandenberg, L.N. Bisphenol S Alters the Lactating Mammary Gland and Nursing Behaviors in Mice Exposed During Pregnancy and Lactation. Endocrinology 2017, 158, 3448–3461. [Google Scholar] [CrossRef]
- Catanese, M.C.; Vandenberg, L.N. Bisphenol S (BPS) Alters Maternal Behavior and Brain in Mice Exposed During Pregnancy/Lactation and Their Daughters. Endocrinology 2017, 158, 516–530. [Google Scholar] [CrossRef]
- Hill, C.E.; Sapouckey, S.A.; Suvorov, A.; Vandenberg, L.N.; Schumacher, U. Developmental exposures to bisphenol S, a BPA replacement, alter estrogen-responsiveness of the female reproductive tract: A pilot study. Cogent Med. 2017, 4. [Google Scholar] [CrossRef]
- Castro, B.; Sanchez, P.; Torres, J.M.; Ortega, E. Bisphenol A, bisphenol F and bisphenol S affect differently 5alpha-reductase expression and dopamine-serotonin systems in the prefrontal cortex of juvenile female rats. Environ. Res. 2015, 142, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Ohtani, N.; Iwano, H.; Suda, K.; Tsuji, E.; Tanemura, K.; Inoue, H.; Yokota, H. Adverse effects of maternal exposure to bisphenol F on the anxiety- and depression like behavior of offspring. J. Veter. Med. Sci. 2017, 79, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Demacopulo, B.; Kreimann, E.L. Bisphenol S increases EZRIN expression and the detrimental effects induced by dehydroepiandrosterone in rat endometrium. Mol. Cell Endocrinol. 2019, 483, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Sekulovski, N.; MacLean, J.A.; Whorton, A.; Hayashi, K. Prenatal Exposure to Bisphenol A Analogues on Female Reproductive Functions in Mice. Toxicol. Sci. 2019, 168, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Sekulovski, N.; MacLean, J.A.; Hayashi, K. Prenatal Exposure to Bisphenol A Analogues on Male Reproductive Functions in Mice. Toxicol. Sci. 2018, 163, 620–631. [Google Scholar] [CrossRef] [PubMed]
- Campen, K.A.; Kucharczyk, K.M.; Bogin, B.; Ehrlich, J.M.; Combelles, C.M.H. Spindle abnormalities and chromosome misalignment in bovine oocytes after exposure to low doses of bisphenol A or bisphenol S. Hum. Reprod. 2018, 33, 895–904. [Google Scholar] [CrossRef] [PubMed]
- Berni, M.; Gigante, P.; Bussolati, S.; Grasselli, F.; Grolli, S.; Ramoni, R.; Basini, G. Bisphenol S, a Bisphenol A alternative, impairs swine ovarian and adipose cell functions. Domest. Anim. Endocrinol. 2019, 66, 48–56. [Google Scholar] [CrossRef]
- Eladak, S.; Grisin, T.; Moison, D.; Guerquin, M.J.; N’Tumba-Byn, T.; Pozzi-Gaudin, S.; Benachi, A.; Livera, G.; Rouiller-Fabre, V.; Habert, R. A new chapter in the bisphenol a story: Bisphenol S and bisphenol F are not safe alternatives to this compound. Fertil. Steril. 2015, 103, 11–21. [Google Scholar] [CrossRef]
- Desdoits-Lethimonier, C.; Lesné, L.; Gaudriault, P.; Zalko, D.; Antignac, J.P.; Deceuninck, Y.; Platel, C.; Dejucq-Rainsford, N.; Mazaud-Guittot, S.; Jégou, B. Parallel assessment of the effects of bisphenol A and several of its analogs on the adult human testis. Hum. Reprod. 2017, 32, 1465–1473. [Google Scholar] [CrossRef]
- Basak, S.; Duttaroy, A.K. Cellular effects of the endocrine disrupters (Bisphenol-S & A): Impact on the growth and development of the first trimester trophoblast cells. Placenta 2017, 57, 253. [Google Scholar] [CrossRef]
- Mustieles, V.; Williams, P.L.; Fernandez, M.F.; Mínguez-Alarcón, L.; Ford, J.B.; Calafat, A.M.; Hauser, R.; Messerlian, C. Environment and Reproductive Health (EARTH) Study Team. Maternal and paternal preconception exposure to bisphenols and size at birth. Hum. Reprod. 2018, 33, 1528–1537. [Google Scholar] [CrossRef] [PubMed]
- Aker, A.M.; Ferguson, K.K.; Rosario, Z.Y.; Mukherjee, B.; Alshawabkeh, A.N.; Calafat, A.M.; Cordero, J.F.; Meeker, J.D. A repeated measures study of phenol, paraben and Triclocarban urinary biomarkers and circulating maternal hormones during gestation in the Puerto Rico PROTECT cohort. Environ. Health 2019, 18, 28. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Colon, E.; Chawla, S.; Vandenberg, L.N.; Suvorov, A. 2015. Endocrine disruptors alter social behaviors and indirectly influence social hierarchies via changes in body weight. Environ. Health Glob. Access Sci. 2015, 14, 64. [Google Scholar] [CrossRef]
- Boucher, J.G.; Ahmed, S.; Atlas, E. Bisphenol S Induces Adipogenesis in Primary Human Preadipocytes From Female Donors. Endocrinology 2016, 157, 1397–1407. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Atlas, E. Bisphenol S- and bisphenol A-induced adipogenesis of murine preadipocytes occurs through direct peroxisome proliferator-activated receptor gamma activation. Int. J. Obes. (Lond.) 2016, 40, 1566–1573. [Google Scholar] [CrossRef]
- Ivry Del Moral, L.; Le Corre, L.; Poirier, H.; Niot, I.; Truntzer, T.; Merlin, J.F.; Rouimi, P.; Besnard, P.; Rahmani, R.; Chagnon, M.C. Obesogen effects after perinatal exposure of 4,4′-sulfonyldiphenol (Bisphenol S) in C57BL/6 mice. Toxicology 2016, 357, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Pu, Y.; Gingrich, J.D.; Steibel, J.P.; Veiga-Lopez, A. Sex-Specific Modulation of Fetal Adipogenesis by Gestational Bisphenol A and Bisphenol S Exposure. Endocrinology 2017, 158, 3844–3858. [Google Scholar] [CrossRef][Green Version]
- Wang, R.Y.; Abbott, R.D.; Zieba, A.; Borowsky, F.E.; Kaplan, D.L. Development of a Three-Dimensional Adipose Tissue Model for Studying Embryonic Exposures to Obesogenic Chemicals. Ann. Biomed. Eng. 2017, 45, 1807–1818. [Google Scholar] [CrossRef]
- Kataria, A.; Levine, D.; Wertenteil, S.; Vento, S.; Xue, J.; Rajendiran, K.; Kannan, K.; Thurman, J.M.; Morrison, D.; Brody, R.; et al. Exposure to bisphenols and phthalates and association with oxidant stress, insulin resistance, and endothelial dysfunction in children. Pediatr. Res. 2017, 81, 857–864. [Google Scholar] [CrossRef]
- Zhang, W.; Xia, W.; Liu, W.; Li, X.; Hu, J.; Zhang, B.; Xu, S.; Zhou, Y.; Li, J.; Cai, Z.; et al. Exposure to Bisphenol a Substitutes and Gestational Diabetes Mellitus: A Prospective Cohort Study in China. Front. Endocrinol. (Lausanne) 2019, 10, 262. [Google Scholar] [CrossRef]
- Mesnage, R.; Phedonos, A.; Arno, M.; Balu, S.; Corton, J.C.; Antoniou, M.N. Editor’s Highlight: Transcriptome Profiling Reveals Bisphenol A Alternatives Activate Estrogen Receptor Alpha in Human Breast Cancer Cells. Toxicol. Sci. 2017, 158, 431–443. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Choi, H.; Lee, H.; Lee, G.; Hwang, K.; Choi, K. Effects of bisphenol compounds on the growth and epithelial mesenchymal transition of MCF-7 CV human breast cancer cells. J. Biomed. Res. 2017, 31, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Gravdal, K.; Halvorsen, O.J.; Haukaas, S.A.; Akslen, L.A. A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin. Cancer Res. 2007, 13, 7003–7011. [Google Scholar] [CrossRef] [PubMed]
- Verbanck, M.; Canouil, M.; Leloire, A.; Dhennin, V.; Coumoul, X.; Yengo, L.; Froguel, P.; Poulain-Godefroy, O. Low-dose exposure to bisphenols A, F and S of human primary adipocyte impacts coding and non-coding RNA profiles. PLoS ONE 2017, 12, e0179583. [Google Scholar] [CrossRef]
- Williams, G.P.; Darbre, P.D. Low-dose environmental endocrine disruptors, increase aromatase activity, estradiol biosynthesis and cell proliferation in human breast cells. Mol. Cell Endocrinol. 2019, 486, 55–64. [Google Scholar] [CrossRef]
- Mersha, M.D.; Patel, B.M.; Patel, D.; Richardson, B.N.; Dhillon, H.S. Effects of BPA and BPS exposure limited to early embryogenesis persist to impair non-associative learning in adults. Behav. Brain Funct. 2015, 11, 27. [Google Scholar] [CrossRef]
- Cano-Nicolau, J.; Vaillant, C.; Pellegrini, E.; Charlier, T.D.; Kah, O.; Coumailleau, P. Estrogenic effects of several BPA analogs in the developing Zebrafish brain. Front. Neurosci. 2016, 10, 112. [Google Scholar] [CrossRef]
- Mokra, K.; Woźniak, K.; Bukowska, B.; Sicińska, P.; Michałowicz, J. Low-concentration exposure to BPA, BPF and BPAF induces oxidative DNA bases lesions in human peripheral blood mononuclear cells. Chemosphere 2018, 201, 119–126. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, H.S.; Guo, T.L. Modulation of cytokine/chemokine production in human macrophages by bisphenol A: A comparison to analogues and interactions with genistein. J. Immunotoxicol. 2018, 15, 96–103. [Google Scholar] [CrossRef]
- Žalmanová, T.; Hošková, K.; Nevoral, J.; Prokešová, Š.; Zámostná, K.; Kott, T.; Petr, J. Bisphenol S instead of bisphenol A: A story of reproductive disruption by regretable substitution—A review. Czech. J. Anim. Sci. 2016, 61, 433–449. [Google Scholar] [CrossRef]
| Specific Effect | Model Used | Results | Reference Number |
|---|---|---|---|
| Reproductive System | Zebrafish | Mixed results with 3 studies claiming BPS was the least toxic to developing zebrafish and one study claiming BPS was the most toxic | Moreman et al. [12] Catron et al. [13] Qiu et al. [14] Kinch et al. [15] |
| Murine | BPS and BPA decreased sperm counts, sperm quality, and spermatogenesis but only BPS decreased sperm motility. In females, BPS decreased lactation, disrupted follicular development, caused an abnormal estrogen response, increased female infertility and altered maternal behavior | Roelofs et al. [16] Liang et al. [17] Shi et al. [25] LaPlante et al. [18] Catanese & Vandenberg [19] Hill et al. [20] Castro et al. [21] Ohtani et al. [22] Demacopulo & Kreimann [23] Shi et al. [24] | |
| Bovine | BPS caused the most abnormal oocyte spindle formation & chromosomal misalignment | Campen et al. [26] | |
| Porcine | BPS inhibited cell proliferation & nonenzymatic scavenging activity causing reproductive toxicity | Berni et al. [27] | |
| human cell lines or explants | BPS more easily decreased spermatogenesis, BPA and BPS both inhibit early placentation | Eladek et al. [28] Desdoits-Lethimonier et al. [29] Basak & Duttaroy [30] | |
| Clinical/Observational Studies | BPS was not correlated with lower birth weight and smaller head circumference, but was correlated with lower Corticotropin-releasing hormone (CRH) levels | Mustieles et al. [31] Aker et al. [32] |
| Specific Effect | Model Used | Results | Reference Number |
|---|---|---|---|
| Obesogenic Effects/Metabolic Disorders | Murine | BPS caused a transient loss in body weight in one behavioral study, but caused increased body weight via the activation of preadipocytes in all other studies | Kim et al. [33] Boucher et al. [34] Achmed & Atlas [35] Ivry Del Moral et al. [36] |
| Sheep | BPS caused adipogenic differentiation in males, while BPA had the same effect in females | Pu et al. [37] | |
| human embryonic stem cells | BPS increased cellular expression of adipogenic genes and caused accumulated triglycerides | Wang et al. [38] | |
| Clinical/Observational | BPS levels correlated with insulin resistance, albuminuria, irregular vascular function and gestational diabetes mellitus (GDM) | Kataria et al. [39] Zhang et al. [40] |
| Specific Effect | Model Used | Results | Reference Number |
|---|---|---|---|
| Human Breast Cancer | MCF-7 human breast cancer cells | BPS had the least effect on estrogen receptors (ERα), but did promote cancer progression | Mesnage et al. [41] Kim et al. [42] Gravdal et al. [43] Williams et al. [45] |
| human primary adipocytes | BPS caused coding changes consistent with cancer progression | Verbanck et al. [44] |
| Specific Effect | Model Used | Results | Reference Number |
|---|---|---|---|
| Nervous System | Zebrafish | Mixed results with four studies reporting opposite findings concerning neural development after BPS exposure | Catron et al. [13] Qiu et al. [14] Kinch et al. [15] Cano-Nicolau et al. [47] |
| C. elegans | BPS significantly impaired neural function | Mersha et al. [46] |
| Specific Effect | Model Used | Results | Reference Number |
|---|---|---|---|
| DNA Damage | peripheral blood cells (PBMCs) | BPS caused the least damage to DNA bases of all tested bisphenols | Mokra et al. [48] |
| Immune System Effects | primary human macrophages | BPS had a very minor effect on cytokine secretion | Chen et al. [49] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thoene, M.; Dzika, E.; Gonkowski, S.; Wojtkiewicz, J. Bisphenol S in Food Causes Hormonal and Obesogenic Effects Comparable to or Worse than Bisphenol A: A Literature Review. Nutrients 2020, 12, 532. https://doi.org/10.3390/nu12020532
Thoene M, Dzika E, Gonkowski S, Wojtkiewicz J. Bisphenol S in Food Causes Hormonal and Obesogenic Effects Comparable to or Worse than Bisphenol A: A Literature Review. Nutrients. 2020; 12(2):532. https://doi.org/10.3390/nu12020532
Chicago/Turabian StyleThoene, Michael, Ewa Dzika, Slawomir Gonkowski, and Joanna Wojtkiewicz. 2020. "Bisphenol S in Food Causes Hormonal and Obesogenic Effects Comparable to or Worse than Bisphenol A: A Literature Review" Nutrients 12, no. 2: 532. https://doi.org/10.3390/nu12020532
APA StyleThoene, M., Dzika, E., Gonkowski, S., & Wojtkiewicz, J. (2020). Bisphenol S in Food Causes Hormonal and Obesogenic Effects Comparable to or Worse than Bisphenol A: A Literature Review. Nutrients, 12(2), 532. https://doi.org/10.3390/nu12020532





