Abstract
Background and objectives: Attention-deficit/hyperactivity disorder (ADHD) is one of the most common psychiatric disorders in children and adolescents. Mind–body therapies (MBTs) seem to be effective for improving health in different populations; however, whether a positive effect occurs in children and adolescents with ADHD is still controversial. The main aim of this systematic review was to analyse the interventions based on MBT aimed to improve the main ADHD symptoms in children and adolescents. Materials and Methods: A systematic review was conducted following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines to identify MBT studies on children and adolescents (4–18 years) with a clinical diagnosis of ADHD. Study quality was evaluated by the NIH quality tool (U.S. National Institute of Health). Results: There were positive results in eleven out of twelve included studies regarding the effect of the MBT interventions on ADHD symptoms. With respect to ADHD symptoms, we observed differences across studies. In relation to the studies’ quality, eleven studies were rated “poor” and one was rated as “fair”. Conclusions: MBTs, such as yoga or mindfulness, could be positive strategies to mitigate ADHD symptoms in children and adolescents. However, further research with high-quality designs, with randomization, greater sample sizes, and more intensive supervised practice programs are needed.
1. Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a common behavioral disorder that affects from 1% to 20% of the children worldwide [1,2], but overall, the pooled prevalence of ADHD is around 5% [3]. ADHD is characterized by pervasive and impairing symptoms of inattention, hyperactivity, and impulsivity according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) [4]. The etiology of ADHD is multifaceted and multidimensional, linking genetic and environmental factors [5]. ADHD has been characterized as a major public health problem due to the broad range of negative effects in diagnosed people and the serious expenses for families and society. According to the American Psychiatric Association in the DSM-V, to be considered ADHD a child must have symptoms before the age of 12 years, for at least six months, and affecting two domains of life [6]. The prevalence of the three subtypes of ADHD are: inattentive (20–30% of diagnosed population), hyperactive-impulsive (less than 15%), and combined subtype (50–75%) [7]. Eleven percent of children ages 4 to 17 in the United States (6.4 million children) have been diagnosed with attention-deficit hyperactivity disorder, according to a survey by the Centers for Disease Control and Prevention [8]. Boys are diagnosed with ADHD three times more frequently than girls. Therefore, evidence corroborates the solid influence of genetic factors on the expression of symptoms; however, psychosocial, environmental, and cultural factors also play an important role in this disorder [9].
To date, ADHD symptoms have been treated with different therapies. A previous systematic review study suggested aerobic exercise had a moderate to large influence on core symptoms of ADHD in children and adolescents [10]. This study indicated that short-term aerobic exercise attenuates ADHD symptoms such as attention, hyperactivity, impulsivity, anxiety, executive functions, and social disorders in diagnosed children. In a study with a sample of 7000 youths with mental health concerns, such as ADHD, depression, and anxiety, complementary alternative medicine therapies had an important role, where mind–body therapies (MBTs) were the most used [11]. Accordingly, MBTs such as yoga, mindfulness, or meditation offered a wide range of positive effects on psychosocial, emotional, and neurobiological functioning in several populations [6]. These non-invasive techniques are based on positive thoughts and emotions to improve emotional and behavioral health. Such techniques consist of deep breathing, meditation, mindfulness, guided imagery, progressive relaxation, and yoga exercises [12]. It has been shown that the practice of these therapies can change brain activation patterns, contribute to improve mood and reduce anxiety, stress, and pain, in addition to developing attention control and inhibitory skills [13]. The neurophysiological mechanisms implicated respond to activation to dopaminergic and noradrenergic systems. The successful pharmacological treatments used from preschooler ages are mainly composed of psychostimulant drugs that increase dopaminergic action [14], however, the MBTs could active the liberation of this hormone without the typical adverse side effect of these chemical medications [15]. In light of these benefits, a few intervention studies have investigated the function of MBTs in controlling ADHD symptoms in young people. However, the potential benefits of MBTs on symptoms of ADHD in youths are still controversial. Thus, the main aim of this systematic review (SR) was to analyse the interventions based on MBT aimed to improve the main ADHD symptoms in children and adolescents.
2. Materials and Methods
We followed the recommendations of preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement [16]. The PRISMA checklist of this SR can be found in Supplementary Table S1.
2.1. Study Eligibility Criteria
Intervention studies focused on MBTs carried out to improve the main symptoms of ADHD in children and adolescents (4–18 years old) were included in the current systematic review. First, the current study included studies enrolling children and adolescents with a clinical diagnosis of ADHD. All ADHD subtypes (i.e., combined type, predominantly inattentive, and predominantly hyperactive/impulsive) were considered as valid studies, following a previous search protocol [10]. Studies including patients with comorbid conditions (such as anxiety, depression, epilepsy, or other medical conditions) were not eligible. Second, the present review considered studies evaluating only MBT-based interventions such as, yoga, meditation, mindfulness, relaxation, or zen therapies or programs. Finally, the main outcomes of the studies included in this SR were the principal ADHD symptoms, such as inattention, hyperactivity, or impulsivity, and related skills, which are attenuated with ADHD diagnostics (e.g., accuracy rate, reaction time, etc.).
Other secondary outcomes related to ADHD, such as anxiety, shyness, social problems, perfectionism, self-reported emotion dysregulation, depressive symptoms, and parent’s emotional regulation and feelings, were included in the description of the intervention studies.
2.2. Search Methods for Identification of Studies
A PICOS approach was used for framing the research question and the evidence search [17]. Participants: Child* OR adolescent* OR young* OR youth. Interventions: Yoga OR yogic OR meditation OR Tai Chi OR mindfulness OR mindful OR mindfulness-based OR mind-body OR relaxation OR zen. Comparisons: Not applicable. Outcomes: Medical condition terms (ADHD OR attention deficit OR attention-deficit OR hyperkinetic syndrome OR hyperkinetic disorder). Study design: intervention OR program OR therapy OR training OR school-based intervention. Additional filters: All database, builder terms: Title/abstract for PubMed, Topic for Web of Science, and abstract for PsycINFO and EBSCOHost, Publication years from 2000 to 2018.
Thus, relevant randomized trials included in systematic reviews were reviewed. A search was performed in the following databases with no language/date/type of document restrictions: Web of Knowledge databases (Web of Science (science citation index expanded), PubMed, PsycINFO, and EBSCOHost, in order to identify additional relevant intervention studies published beyond these reviews [18]. The specific electronic search for each database and terms included are shown in Supplementary File S1.
Additionally, references from the included studies were hand-searched to discover any potential study not detected with the electronic search.
2.3. Screening and Data Extraction
2.3.1. Screening
The eligibility process was conducted in two separate stages:
- The authors (E.V.-G. and B.E.E.) independently screened titles and abstracts of all nonduplicated papers and excluded those with exclusion criteria. A definitive list was established. Discrepancies were resolved by consensus between the authors. When there was no consensus, a third, senior author (Y.B.-R.) acted as mediator. If any doubt about inclusion existed, the article proceeded to the next stage.
- Those articles that passed screening were downloaded (full text) and assessed for eligibility by two authors (E.V.-G. and B.E.E.), independently. Again, discrepancies were resolved by consensus between the authors, and if needed, two seniors author (Y.B.-R. and R.R.-V.) acted as arbitrators. When required, the corresponding authors of screened studies were contacted to inquire about study eligibility (n = 1).
Duplicates, nonintervention studies, non-English language, and studies without analysis of our primary outcomes or main participants were eliminated. Articles included in the review are showed in the PRISMA flow diagram (Figure 1).
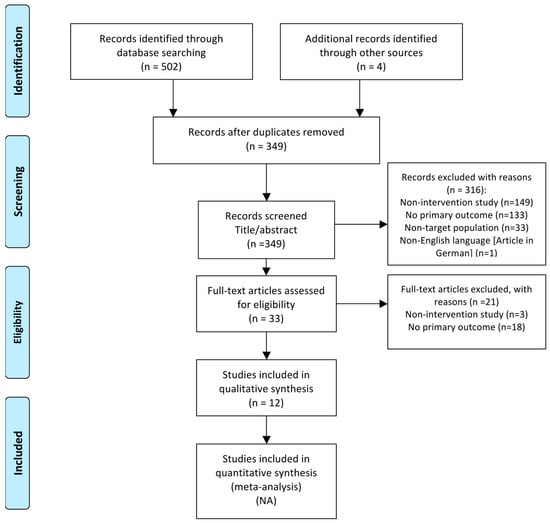
Figure 1.
PRISMA flow diagram of included studies on Mind–Body Therapies for the improvement of attention-deficit/hyperactivity disorder symptoms in children and adolescents.
2.3.2. Data Extraction
Data extraction was independently performed by two researchers (E.V.-G. and Y.B.-R.); discrepancies were resolved by agreement between the two authors. The following data were extracted:
- Publication details: year of publication and country where the study was conducted.
- Study participants’ details: sample and age range.
- Design of the study.
- Intervention characteristic: duration and frequency of the intervention period.
- Outcome: main outcome, secondary outcomes, and assessment test.
- Main study results.
2.4. Study Quality Assessment
Study quality was evaluated using the quality assessment tools from the Risk Assessment Workgroup of the Department of Health and Human Services from the U.S. National Institute of Health [19]. We assessed quality by two different tools: (1) quality assessment of controlled intervention studies (i.e., randomized controlled trials (RCTs) and clinical trials studies), and (2) quality assessment tool for before–after (pre–post) studies with no control group. These instruments were created to evaluate the internal validity of a trial, the extent to which the reported effects can strictly be attributed to the intervention applied, and the potential flaws in methodology or implementation. Each tool contains specific questions to assess bias, confounders, power, and strength of association between intervention and outcomes. The answer to each question could be “yes,” “no,” “cannot determine,” “not reported,” or “not applicable”. A numeric scoring system was not used. The evaluator had to consider the potential risk for bias in the study design whenever a “no” was selected. Overall quality ratings were scored as “good” (low risk of bias, valid results), “fair” (some risk of bias, does not invalidate results), or “poor” (significant risk for bias, may invalidate results). If a study had a “fatal flaw” then risk of bias was significant and the study was of poor quality. Examples of fatal flaws in RCTs include high dropout rates, high differential dropout rates, intention to treat analysis, or other inappropriate statistical analysis. All studies were independently screened by one author (Y.B.-R.), and three additional reviewers (E.V.-G., B.E.E., R.R.-V.) tested a 50% sample (n = 6) to double check for accuracy.
3. Results
3.1. Study Selection
In the first stage of the search strategy, a total of (n = 506) articles were identified. In the second stage, following the removal of duplicates (n = 157), a total of (n = 349) articles were screened by title/abstract. Then, 316 potentially relevant articles were excluded with reasons (details summarized in Figure 1). In the third stage, full-text articles were reviewed in depth and (n = 21) studies were excluded with reasons (details summarized in Figure 1). Finally, only (n = 12) studies based on MBT interventions met the inclusion and exclusion criteria and were included in the final analysis.
3.2. Characteristics of the Included Studies
The characteristics of the included studies are presented in Table 1. The included studies were conducted in different continents, such as “the Americas” [20,21], Europe [22,23], Asia [24,25,26,27,28,29,30], and Australia [31]. All analyzed studies targeted children and adolescents (ranged from 5 to 18 years old). Only one study [20] also included adults, but results from adolescents and adults were displayed separately. Moreover, most of the studies (11/12) [20,21,22,23,24,25,27,28,29,30,31] included parental participation, supporting children to perform the program at home or being involved in the intervention. The number of participants varied across the intervention studies, ranging from eight participants [20] to 100 [28]. Furthermore, the range of parent participation also varied from 11 [29] to 79 [25] families. Regarding the study design, there were five RCT studies [25,27,28,30,31] and a clinical trial [24].

Table 1.
Characteristics of interventions of mind–body therapies for the improvement of ADHD symptoms (n = 12).
3.3. Analysis of the MBT Intervention and its Effects on ADHD Outcomes
3.3.1. MBT Interventions
All interventions consisted of MBTs, including nine studies developing mindfulness treatment [20,21,22,23,25,27,28,29,30] and three studies that conducted yoga [24,26,31]. Five studies [20,24,26,29,31] declared that interventions were guided by a certified instructor in mindfulness or yoga. For instance, in the study of [20] instruction was carried out by an experienced mindfulness instructor. In addition, six studies received the interventions in a homework format, such as an audio CD-ROM and workbooks that guided meditations to support home practice [21], an audio CD-ROM with mindfulness exercises to practice at home [22,23,29,30], and CD-ROMs containing guided sitting meditations [20]. The majority were school-based programs (7/12), whereas one study was carried out in a yoga studio [24]. Regarding the intervention period, most of them lasted eight weeks (8/12), finding that the intervention with the greatest duration lasted 20 weeks [31], whereas the shortest duration was one day (including a 90 min session of mindfulness skills protocol) [25]. Concerning frequency, most studies included at least one session per week (9/12 studies), whereas the duration of the sessions varied across studies, in a range between 40 and 150 min. Finally, four studies [22,24,27,28] included a negative control group (three of these with a wait list control group), and two studies a positive control group, including cooperative activities [32] and pharmacotherapy with risperidone or ritalin [30].
3.3.2. Effects of MBT Interventions on ADHD
Regarding the effect of the interventions on the main ADHD symptoms in children and adolescents, in general, there were significant positive results in eleven out of twelve of the studies (91.6%) [20,21,22,23,24,26,27,28,29,30,31], even though in the study of [25] there were no differences on externalizing symptoms in children after the intervention. With respect to evaluating the main ADHD symptoms, we observed significant improvement across studies on primary outcomes, such as accuracy rate and reaction time [24], hyperactivity and impulsivity [31], as well as on inattention [28].
Secondary outcomes, such as anxiety, shyness, social problems, perfectionism, and impulsivity [31], planning, inhibition, and self-reported emotion dysregulation [27], and depressive symptoms [20] were also significantly improved after MBT interventions. Finally, several specific instruments to measure ADHD symptoms were used (e.g., checklist, questionnaires, visual test, scales, etc.).
3.4. Methodological Quality of the Included Studies
In summary, eleven studies were rated “poor”, and only one was rated as “fair” [25] (see Supplementary Tables S2 and S3).
3.4.1. Quality Assessment of Controlled Intervention Studies
We assessed six studies with this tool (i.e., five RCT studies and a clinical trial). Five [24,27,28,30,31] of the six identified controlled studies included a “fatal flaw”, resulting in a “poor” rating. The randomization process was described in all six controlled studies [24,25,27,28,30,31], and all of them correctly described the randomization sequence. Only one RCT study [25] conducted independent recruitment of participants and blinding. All the controlled intervention studies had similar groups at baseline on important characteristics that could affect the outcome of the study. The overall dropout rates from all the studies at endpoint were lower than 20%, as well as the differential dropout rates between intervention and control group, which were over 15%. Adherence to the intervention program was high in all groups, whereas the application of other interventions was not described in any cases. Furthermore, none of the six controlled intervention studies reported an appropriately sized sample necessary for detecting effects with 80% power. Finally, in all studies, all randomized participants were analyzed in the group to which they were originally assigned (per protocol analysis).
3.4.2. Quality Assessment for Before–After Studies (Pre–Post) Studies with No Control Group
We assessed six studies with this tool (i.e., non-random studies without a control group). The six studies [20,21,22,23,26,29] included at least one “fatal flaw”, resulting in a “poor” rating. All studies included the study question and clearly stated the objective, as well as clearly describing eligibility/selection criteria for the study participants. In the six studies, participants were representative of those who were eligible for the intervention, but they did not include a sample size appropriate to provide assurance in their findings. The outcome assessments were detailed, clearly described, valid, reliable, and assessed consistently across all study participants; however, in none of the studies were the people who assessed the outcomes blinded to the participants’ interventions. In all of the studies, the loss to follow-up after baseline was lower than 20%. Regarding statistical methods, only three studies [20,23,29] examined changes in outcome measures between pre–post intervention, providing the p values. In addition, in three studies [20,21,26], statistical analysis used the individual-level data to determine effects at the group level. Finally, in three studies [21,23,26], the outcome was measured at multiple times along the MBT intervention. Due to heterogeneity in the measurement of mind–body therapies outcomes (i.e., inattention, hyperactivity, or impulsivity, and related skills), type intervention (i.e., yoga, meditation, mindfulness, relaxation, or zen therapies or programs), and on types of comparators (i.e., no treatment as negative control group or traditional intervention as positive control group), doing a meta-analysis was not possible (see Table 1).
4. Discussion
The main findings of this SR were that a significant positive result was found in eleven out of twelve included studies regarding the effect of the MBTs on ADHD symptoms in children and adolescents. In addition, in relation to the quality of the studies, eleven studies were rated “poor” and one was rated as “fair”. A more detailed description of the types of intervention used and the effects produced on the main ADHD symptoms and other related factors are described below.
ADHD persists into adulthood in up to 80% of individuals diagnosed as children [33], so prevention and mitigation of ADHD symptoms are important from an early age. Stimulant medication is the most usual first-line treatment for ADHD for people of all ages. RCTs have proven the effectiveness of stimulants in reducing core symptoms of ADHD in youth [18]. However, a high proportion of young people in these trials were considered nonresponders. Additionally, although stimulant medication is a key component of ADHD treatment, it is necessary to explore the multidimensional effect of other complementary interventions for young people with ADHD, such as nonpharmacological programs, i.e., school-based intervention strategies, psychotherapy, and cognitive–behavioral interventions [34]. Consequently, the positive effects of physical exercise have been described on the same catecholaminergic system targeted by stimulant medications for ADHD [35,36]. Additionally, pharmacotherapy has been related to side effects such as poor tolerance, no response to treatment, and even dependence [10]. Thus, physical exercise could be considered a helper to decrease behavioral problems that influence the learning and academic processes in children with ADHD [10].
As a form of exercise, MBTs, including tai chi, meditation, mindfulness, and yoga, have been put in the crosshairs of the scientific community to analyze in depth the effectiveness of these widely used practices. Accordingly, the National Center for Complementary and Alternative Medicine designates MBTs as a top research priority [6]. According to Morgan et al., MBTs such as tai chi or yoga are multidimensional behavioral therapies that integrate several aspects of physical exercise, such as light to moderate aerobic physical activity, deep breathing, balance, and meditation to encourage stress reduction and relaxation, which could potentially impact ADHD symptoms. Moreover, it has been demonstrated that meditation is a more integrative program for stress reduction, regulating emotional, and affective responses to stress. A recent review [37] with 12 preliminary studies of yoga in schools for children, established that yoga interventions applied positive effects on factors such as emotional balance, attentional control, cognitive efficiency, anxiety, negative thought patterns, emotional and physical arousal, reactivity, and negative behavior. Additional research in children also showed the positive effects of school-based yoga programs on several aspects of mental health, such as concentration, attention, anxiety, stress, mood, resilience, emotional arousal, self-esteem, and coping frequency [38]. However, to date few studies were carried out with MBTs, such as yoga or mindfulness, in children and adolescents with ADHD.
In the current SR, we included twelve studies based on MBTs in children and adolescents with diagnoses of ADHD. Nine developed mindfulness treatments [20,21,22,23,25,27,28,29,30], three conducted yoga programs [24,26,31], and none of these included others such as Zen, tai chi, or specific meditation therapies. Most of the included studies (11/12) displayed significant positive results on ADHD symptoms, where only the study of Gershy et al. [25] did not show significant positive results regarding ADHD symptoms after the intervention. A possible explanation for this lack of effect on ADHD symptoms could be that the intervention period was only one day, including a session of 90 min of mindfulness skills protocol. In this sense, evidence-based interventions often involved 7 to 12 weekly sessions, demonstrating improved child behavior and parent satisfaction [39,40], in addition three to four weeks on stable medication is the minimum length of treatment efficacy in subjects with ADHD [41]. Accordingly, the present SR displayed that most of the included studies (8/12) carried out an intervention for at least eight weeks, including a study with a duration of 20 weeks [31]. So, future intervention studies should include intensive training lasting at least seven to eight weeks of intervention. For example, in two case studies of children with ADHD, a significant decrease in compliance of the child was described after an intensive mindfulness program including 12 sessions (twice weekly) [42]. Future research must establish the optimal frequency, duration, and intensity of intervention programs to lead to effective interventions.
In the study of [25], no differences in child externalizing symptoms were found, which decreased significantly in both groups after intervention. However, mothers’ negative feelings, escalating behaviors, and capacity for emotional regulation improved significantly at the end of the intervention. Moreover, fathers in the mindfulness condition reported greater improvement in the capacity for emotional regulation, reduced negative feelings, and reduced parental submission compared with fathers in the parent training condition. Thus, it is possible that interventions focused only on youth may be more effective than those that include both young people and parents. Contrary to this hypothesis, effective behavioral therapies include parent and youth training, with classroom management, peer interventions, or combinations of these interventions [43]. It seems that parent training improves their understanding of ADHD, behavioral problems, and child development, helping them to use strategies such as praise and rewards for targeted behaviors. Additionally, disruptive child behaviors are decreased. Thereby, MBTs involving both parents and youths seem to have a positive influence on family relationships, further improving ADHD symptoms in children and adolescents, as shown by three of the studies included in the present review [21,22,28]. Additionally, it is important to take into account that ADHD is a neurodevelopmental disorder, which could remit and even transform some symptoms and deficits into adaptive behaviors or even lead a negative trajectory. The patient’s compliance and feeling regarding the medical therapy [44,45,46] and an optimal medical and multicomponent treatment is the key to ensure positive effects.
Concerning study quality, even though we included four RCT studies and a clinical trial, most of the studies (11/12) were rated as “poor” quality, while only the study of [25] was rated as “fair” quality. Again, we hypothesized that the reason for the difference between studies could be the duration of the intervention (i.e., one day of a 90 min session of mindfulness skills protocol), since the short duration (one day) in the intervention could avoid several “fatal flaws” in the design or development of the study (e.g., blinding of participants or providers to the treatment group assignments, etc.).
Another important criteria that could influence the quality assessment differences between the study of Gershy et al. and the rest of the controlled intervention studies could be the dropout rate, since previous literature has shown that there is usually an important prevalence of dropouts in exercise interventions [47]. However, in the current SR, all of controlled intervention studies met both criteria for not having a “fatal flaw”, i.e., overall dropout rate from the study at endpoint (20% or lower) and differential dropout rate (between treatment groups) at endpoint (15% or lower). In this respect, it seems that lower dropout was observed in sports interventions compared with structured aerobic exercise or yoga (p = 0.049), so in order to increase participation, and therefore health benefits, MBT interventions must offer a multidisciplinary approach for children and adolescents with ADHD [47].
In addition to the satisfactory dropout rate across the studies, most of the controlled intervention studies had a high adherence to the intervention programmes (4/6). However, regarding before–after studies with no control group, only the studies of Zylowska et al. [20] and Zhang et al. [29] reported a high rate of adherence, with 78% and 91%, respectively. Regarding adherence correlates, family problems was the main reason for nonadherence among children to yoga practice at home post-discharge [26]. The high percentage of adherence, as well as the low dropout rate could be due to different reasons. First, we hypothesized that there was high satisfaction among the participants who enjoyed MBTs. For instance, Zylowska and colleagues (2008) conducted an open trial of a mindfulness training program where high satisfaction ratings from adolescents were reported. Another possible reason that could explain these two positive aspects in the quality of interventions, i.e., dropout and adherence rates, could be that the sample size was small in all of the studies (12/12), allowing greater control and individual monitoring of the participants. However, an insufficiently large sample size was one of the most usual “fatal flaws” across the studies.
In the controlled intervention studies, none reported a sufficiently large sample size to be able to detect a difference in the main outcome between groups with at least 80% power, as well as in the before–after studies with no control group (6/6), in which the sample size was not sufficiently large to provide confidence in the findings. Thus, small sample sizes in these studies precludes the generalizability of the findings, resulting in a poor quality of the study. Therefore, although most studies reported positive benefits on ADHD symptoms of children and adolescents after completing MBTs, their quality was rated mostly as poor, so future intervention studies should include larger samples as well as randomization and control groups, in order to clarify these findings.
Results of our review study must be viewed in the light of methodological limitations. Overall, the “poor” and “fair” quality ratings for the majority of studies makes it difficult to conclude with consistency regarding future intervention strategies, mainly because risk of bias in the study design critically decreases the confidence in the rationality of the results. Albeit, some aspects must be considered in cases of exercise intervention studies. First, it is possible to find gaps when assessing the quality of the studies using the NIH tools, since these were designed principally for clinical trial studies. For example, the blinding element could be considered inapplicable because it is practically impossible to blind participants who receive MBTs such as yoga or mindfulness. Second, some studies did not specify the intensity/frequency of the intervention, as well as quality criteria such as adherence or in-depth details of the statistical methods. Third, most studies did not report if the participants were involved or stopped some medical or psychological treatment for their ADHD symptoms, or if they performed some additional physical activity, sport, or exercise. Neither were the participants analyzed according to the subtype of ADHD diagnosis. Fourth, the quality of included studies ranked mainly as poor; however, we did not exclude any because of the small number of articles selected. As a strength, a rigorous and strict review process was performed for selecting the studies and extracting the data. Additionally, two valid instruments to evaluate the studies quality were used. Finally, we have not included in this manuscript an SR with a quantitative analysis (meta-analysis) due to the considerable conceptual heterogeneity in the studies (systematic differences in study design, patient populations, interventions or co-interventions, clinical heterogeneity, including duration of the study, the dose of the intervention, and the evaluation of the results). In addition, we observed that the studies were systematically different from each other, so the quantitative synthesis would not be generalizable and applicable to clinical practice. In this context, we recognize and explain the heterogeneity in inclusion studies, particularly from a qualitative perspective, which is a general sense of what all studies say, and is absolutely crucial, especially when analyzing controlled intervention and before–after studies.
5. Conclusions
Most of the intervention studies conducting MBTs in children and adolescents with ADHD indicated positive results for improving ADHD symptoms. The majority of them were eight week school-based programs based on mindfulness treatment, guided by a certified instructor, with a frequency of one session per week, and with duration in a range between 40 and 150 min. However, the studies were identified as being of poor quality. Thus, further studies should be more rigorous to improve the consistency and generalizability of their findings. They must include the use of representative samples with greater statistical power and randomized controlled trial designs. Finally, further research should include behavioral interventions such as MBTs in conjunction with pharmacological treatment.
Supplementary Materials
The following are available online at https://www.mdpi.com/1648-9144/55/7/325/s1, Table S1: PRISMA-P 2015 Checklist, File S1: Electronic search: database and terms included, Table S2: Quality Assessment of Controlled Intervention Studies, Table S3: Quality Assessment for Before-After Studies (Pre-Post) Studies with No Control group).
Author Contributions
Conceptualization, Y.B.-R., B.E.E.; Data curation, Y.B.-R., E.V.-G., and B.E.E.; Formal analysis, Y.B.-R., E.V.-G., and R.R.-V.; Methodology, Y.B.-R., R.R.-V., and E.V.-G.; Project administration, Y.B.-R., and E.V.-G.; Writing—original draft, Y.B.-R., B.E.E., and E.V.-G.; Writing—review & editing, Y.B.-R., R.R.-V., and E.V.-G.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bird, H.R. The Diagnostic Classification, Epidemiology and Crosscultural Validity of Adhd. In Attention Deficit Hyperactivity Disorder: State of the Science: Best Practices; Jensen, P.C.J., Ed.; Civic Research Institute: Kingston, NJ, USA, 2002. [Google Scholar]
- Faraone, S.V.; Sergeant, J.; Gillberg, C.; Biederman, J. The worldwide prevalence of adhd: Is it an american condition? World Psychiatry 2003, 2, 104–113. [Google Scholar] [PubMed]
- Polanczyk, G.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The worldwide prevalence of adhd: A systematic review and metaregression analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. In dsm-5, 5th ed.; American Psychiatric Association: Arlington, TX, USA, 2013. [Google Scholar]
- Faraone, S.V.; Biederman, J.; Spencer, T.; Wilens, T.; Seidman, L.J.; Mick, E.; Doyle, A.E. Attention-deficit/hyperactivity disorder in adults: An overview. Biol. Psychiatry 2000, 48, 9–20. [Google Scholar] [CrossRef]
- Morgan, N.; Irwin, M.R.; Chung, M.; Wang, C. The effects of mind-body therapies on the immune system: Meta-analysis. PLoS ONE 2014, 9, e100903. [Google Scholar] [CrossRef] [PubMed]
- Spencer, T.J.; Biederman, J.; Mick, E. Attention-deficit/hyperactivity disorder: Diagnosis, lifespan, comorbidities, and neurobiology. J. Pediatr. Psychol. 2007, 32, 631–642. [Google Scholar] [CrossRef] [PubMed]
- Visser, S.N.; Bitsko, R.H.; Danielson, M.L.; Perou, R.; Blumberg, S.J. Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children—United States, 2003 and 2007. Morb. Mortal. Wkl. Rep. 2010, 59, 1439–1443. [Google Scholar]
- Swanson, J.M.; Sergeant, J.A.; Taylor, E.; Sonuga-Barke, E.J.; Jensen, P.S.; Cantwell, D.P. Attention-deficit hyperactivity disorder and hyperkinetic disorder. Lancet 1998, 351, 429–433. [Google Scholar] [CrossRef]
- Cerrillo-Urbina, A.J.; Garcia-Hermoso, A.; Sanchez-Lopez, M.; Pardo-Guijarro, M.J.; Santos Gomez, J.L.; Martinez-Vizcaino, V. The effects of physical exercise in children with attention deficit hyperactivity disorder: A systematic review and meta-analysis of randomized control trials. Child Care Health Dev. 2015, 41, 779–788. [Google Scholar] [CrossRef]
- Kemper, K.J.; Gardiner, P.; Birdee, G.S. Use of complementary and alternative medical therapies among youth with mental health concerns. Acad. Pediatr. 2013, 13, 540–545. [Google Scholar] [CrossRef]
- McClafferty, H. Complementary, holistic, and integrative medicine: Mind-body medicine. Pediatr. Rev. 2011, 32, 201–203. [Google Scholar] [CrossRef]
- Edwards, E.; Mischoulon, D.; Rapaport, M.; Stussman, B.; Weber, W. Building an evidence base in complementary and integrative healthcare for child and adolescent psychiatry. Child Adolesc. Psychiatr. Clin. 2013, 22, 509–529. [Google Scholar] [CrossRef] [PubMed]
- Connor, D.F. Preschool attention deficit hyperactivity disorder: A review of prevalence, diagnosis, neurobiology, and stimulant treatment. J. Dev. Behav. Pediatr. 2002, 23, S1–S9. [Google Scholar] [CrossRef] [PubMed]
- Herbert, A.; Esparham, A. Mind-body therapy for children with attention-deficit/hyperactivity disorder. Children 2017, 4, 31. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (pico) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- Catala-Lopez, F.; Hutton, B.; Nunez-Beltran, A.; Mayhew, A.D.; Page, M.J.; Ridao, M.; Tobias, A.; Catala, M.A.; Tabares-Seisdedos, R.; Moher, D. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: Protocol for a systematic review and network meta-analysis of randomized controlled trials. Syst. Rev. 2015, 4, 19. [Google Scholar] [CrossRef] [PubMed]
- Assessing Cardiovascular Risk: Systematic Evidence Review from the Risk Assessment Work Group; National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 2016.
- Zylowska, L.; Ackerman, D.L.; Yang, M.H.; Futrell, J.L.; Horton, N.L.; Hale, T.S.; Pataki, C.; Smalley, S.L. Mindfulness meditation training in adults and adolescents with adhd: A feasibility study. J. Atten. Disord. 2008, 11, 737–746. [Google Scholar] [CrossRef]
- Haydicky, J.; Shecter, C.; Wiener, J.; Ducharme, J.M. Evaluation of mbct for adolescents with adhd and their parents: Impact on individual and family functioning. J. Child Fam. Stud. 2015, 24, 76–94. [Google Scholar] [CrossRef]
- Van der Oord, S.; Bogels, S.M.; Peijnenburg, D. The effectiveness of mindfulness training for children with adhd and mindful parenting for their parents. J. Child Fam. Stud. 2012, 21, 139–147. [Google Scholar] [CrossRef]
- Van de Weijer-Bergsma, E.; Formsma, A.R.; Bruin, E.I.; Bögels, S.M. The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with adhd. J. Child Fam. Stud. 2012, 21, 775–787. [Google Scholar] [CrossRef]
- Chou, C.C.; Huang, C.J. Effects of an 8-week yoga program on sustained attention and discrimination function in children with attention deficit hyperactivity disorder. PeerJ 2017, 5, e2883. [Google Scholar] [CrossRef] [PubMed]
- Gershy, N.; Meehan, K.B.; Omer, H.; Papouchis, N.; Sapir, I.S. Randomized clinical trial of mindfulness skills augmentation in parent training. Child Youth Care Forum 2017, 46, 783–803. [Google Scholar] [CrossRef]
- Hariprasad, V.R.; Arasappa, R.; Varambally, S.; Srinath, S.; Gangadhar, B.N. Feasibility and efficacy of yoga as an add-on intervention in attention deficit-hyperactivity disorder: An exploratory study. Indian J. Psychiatry 2013, 55, S379–S384. [Google Scholar] [CrossRef] [PubMed]
- Kiani, B.; Hadianfard, H.; Mitchell, J.T. The impact of mindfulness meditation training on executive functions and emotion dysregulation in an iranian sample of female adolescents with elevated attention-deficit/hyperactivity disorder symptoms. Aust. J. Psychol. 2017, 69, 273–282. [Google Scholar] [CrossRef]
- Lo, H.H.M.; Wong, S.W.L.; Wong, J.Y.H.; Yeung, J.W.K.; Snel, E.; Wong, S.Y.S. The effects of family-based mindfulness intervention on adhd symptomology in young children and their parents: A randomized control trial. J. Atten. Disord. 2017, 1087054717743330. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Chan, S.K.C.; Lo, H.H.M.; Chan, C.Y.H.; Chan, J.C.Y.; Ting, K.T.; Gao, T.T.; Lai, K.Y.C.; Bögels, S.M.; Wong, S.Y.S. Mindfulness-based intervention for chinese children with adhd and their parents: A pilot mixed-method study. Mindfulness 2017, 8, 859–872. [Google Scholar] [CrossRef]
- Behbahani, M.; Zargar, F.; Assarian, F.; Akbari, H. Effects of mindful parenting training on clinical symptoms in children with attention deficit hyperactivity disorder and parenting stress: Randomized controlled trial. Iran. J. Med. Sci. 2018, 43, 596–604. [Google Scholar] [PubMed]
- Jensen, P.S.; Kenny, D.T. The effects of yoga on the attention and behavior of boys with attention-deficit/ hyperactivity disorder (adhd). J. Atten. Disord. 2004, 7, 205–216. [Google Scholar] [CrossRef]
- Crescentini, C.; Capurso, V.; Furlan, S.; Fabbro, F. Mindfulness-oriented meditation for primary school children: Effects on attention and psychological well-being. Front. Psychol. 2016, 7, 805. [Google Scholar] [CrossRef]
- Barkley, R.A.; Murphy, K.R.; Fischer, M. Adhd in Adults: What the Science Says; Guilford: New York, NY, USA, 2007. [Google Scholar]
- Power, T.J.; Tresco, K.E.; Cassano, M.C. School-based interventions for students with attention-deficit/hyperactivity disorder. Curr. Psychiatry Rep. 2009, 11, 407–414. [Google Scholar] [CrossRef]
- Tomporowski, P.D.; Davis, C.L.; Miller, P.H.; Naglieri, J.A. Exercise and children’s intelligence, cognition, and academic achievement. Educ. Psychol. Rev. 2008, 20, 111–131. [Google Scholar] [CrossRef] [PubMed]
- Wigal, S.B.; Nemet, D.; Swanson, J.M.; Regino, R.; Trampush, J.; Ziegler, M.G.; Cooper, D.M. Catecholamine response to exercise in children with attention deficit hyperactivity disorder. Pediatr. Res. 2003, 53, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Serwacki, M.L.; Cook-Cottone, C. Yoga in the schools: A systematic review of the literature. Int. J. Yoga Therap. 2012, 22, 101–110. [Google Scholar]
- Butzer, B.; LoRusso, A.; Shin, S.H.; Khalsa, S.B. Evaluation of yoga for preventing adolescent substance use risk factors in a middle school setting: A preliminary group-randomized controlled trial. J. Youth Adolesc. 2017, 46, 603–632. [Google Scholar] [CrossRef] [PubMed]
- Pelham, W.E.J.; Fabiano, G.A. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. J. Clin. Child Adolesc. Psychol. 2008, 37, 184–214. [Google Scholar] [CrossRef]
- Evans, S.W.; Owens, J.S.; Bunford, N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. J. Clin. Child Adolesc. Psychol. 2014, 43, 527–551. [Google Scholar] [CrossRef]
- European Medicines Agency. Guideline on the Clinical Investigation of Medicinal Products for the Treatment of Attention Decifit Hyperactivity (ADHD). Emea/chmp/ewp/431734/2008. Available online: https://www.ema.europa.eu/en/clinical-investigation-medicinal-products-treatment-attention-deficit-hyperactivity-disorder-adhd (accessed on 28 June 2019).
- European Medicines Agency. Guideline On the Clinical Investigation of Medicinal Products for the Treatment of Attention Decifit Hyperactivity ADHD). EMEA/CHMP/EWP/431734/2008. European Medicines Agency: London, UK, 2010. Available online: http://www.ema.europa.eu/docs/en_GB/ document_library/Scientific_guideline/2010/08/WC500095686.pdf (accessed on 28 June 2019).
- Singh, N.N.; Singh, A.N.; Lancioni, G.E.; Singh, J.; Winton, A.S.W.; Adkins, A.D. Mindfulness training for parents and their children with adhd increases the children’s compliance. J. Child Fam. Stud. 2010, 19, 157–166. [Google Scholar] [CrossRef]
- Felt, B.T.; Biermann, B.; Christner, J.G.; Kochhar, P.; Van Harrison, R. Diagnosis and management of adhd in children. Am. Fam. Physician 2014, 90, 456–464. [Google Scholar]
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Pagano, S.; Abraha, I.; Montedori, A.; Caruso, S.; Gatto, R.; De Giorgio, S.; Salvato, R. Dental fear/anxiety among children and adolescents. A systematic review. Local messages issues held at the bda library from 2002 onwards, to request this article from the library go to. Eur. J. Paediatr. Dent. 2017, 18, 121–130. [Google Scholar]
- Paglia, L.; Gallus, S.; de Giorgio, S.; Cianetti, S.; Lupatelli, E.; Lombardo, G.; Montedori, A.; Eusebi, P.; Gatto, R.; Caruso, S. Reliability and validity of the italian versions of the children’s fear survey schedule—Dental subscale and the modified child dental anxiety scale. Eur. J. Paediatr. Dent. 2017, 18, 305–312. [Google Scholar] [CrossRef]
- Franke, B.; Michelini, G.; Asherson, P.; Banaschewski, T.; Bilbow, A.; Buitelaar, J.K.; Cormand, B.; Faraone, S.V.; Ginsberg, Y.; Haavik, J. Live fast, die young? A review on the developmental trajectories of adhd across the lifespan. Eur. Neuropsychopharm. 2018, 28, 1059–1088. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).