Systematic Review and Meta-Analysis of the Effectiveness of Calcium-Phosphate Coating on the Osseointegration of Titanium Implants
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Inclusion and Exclusion Criteria
- -
- Preclinical studies in unmodified animals (osteoporotic, diabetic…), using endosseous implants with Ca-P incorporation;
- -
- Studies with at least six animals and 4 weeks of follow-up;
- -
- Studies published in English.
- -
- In vitro studies;
- -
- Narrative and systematic reviews;
- -
- Clinical cases;
- -
- Studies that did not meet the established inclusion criteria.
2.3. Search Strategy
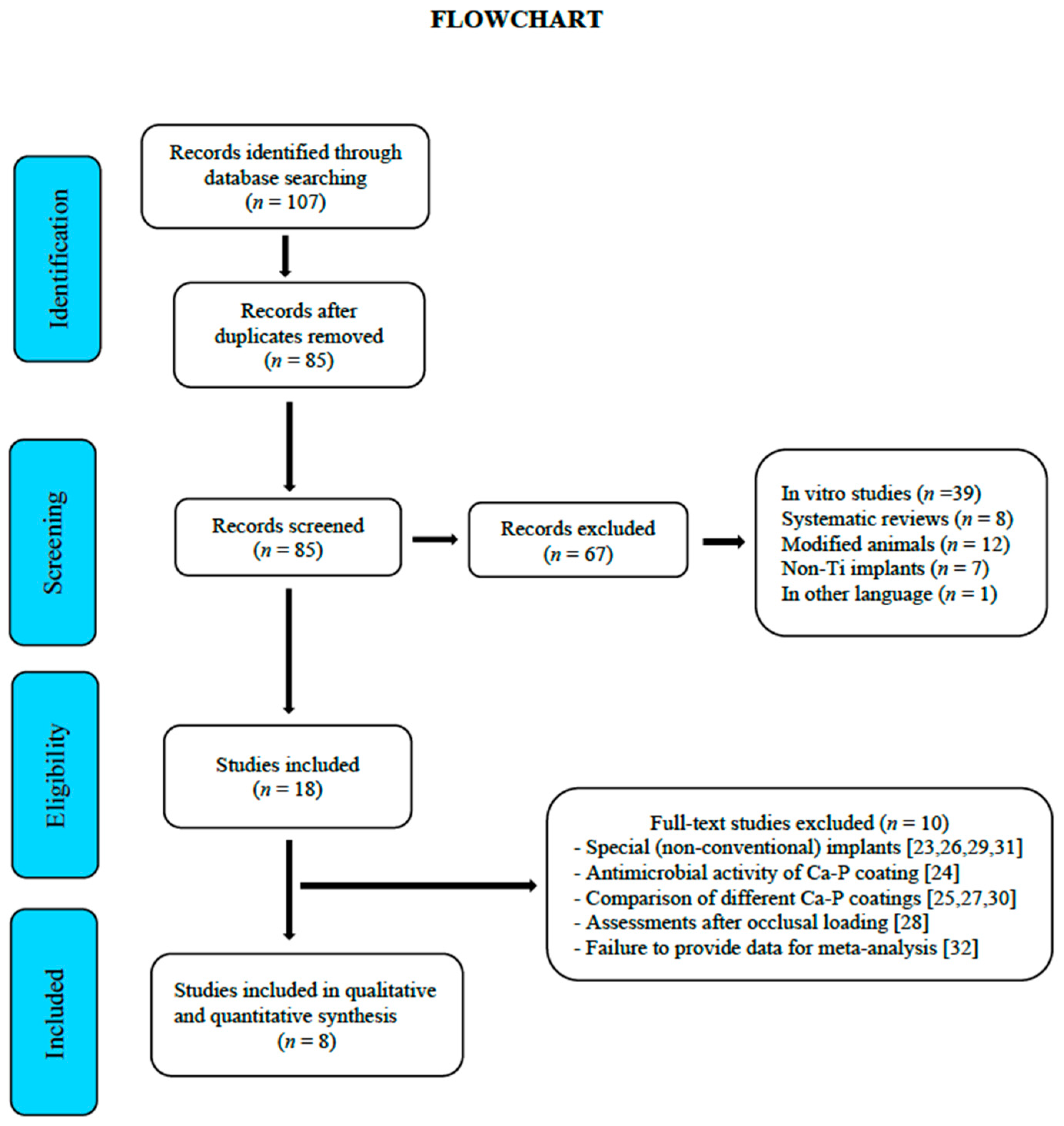
2.4. Selection of Studies
2.5. Risk of Bias
2.6. Quality of the Reports of the Selected Articles
2.7. Statistical Analysis
3. Results
3.1. Selection and Description of Studies
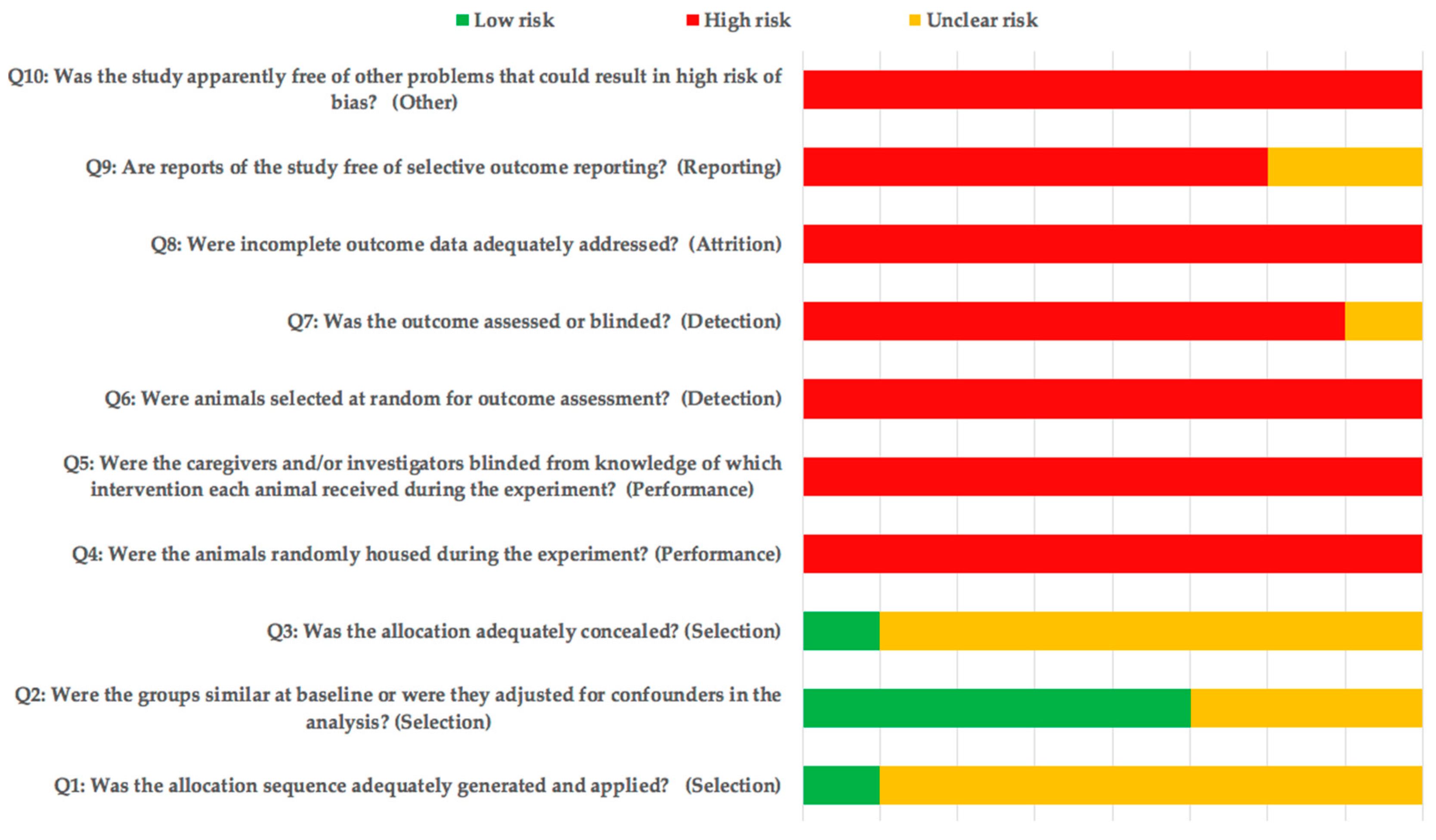
3.2. Risk of Bias Assessment
3.3. Qualitative Synthesis
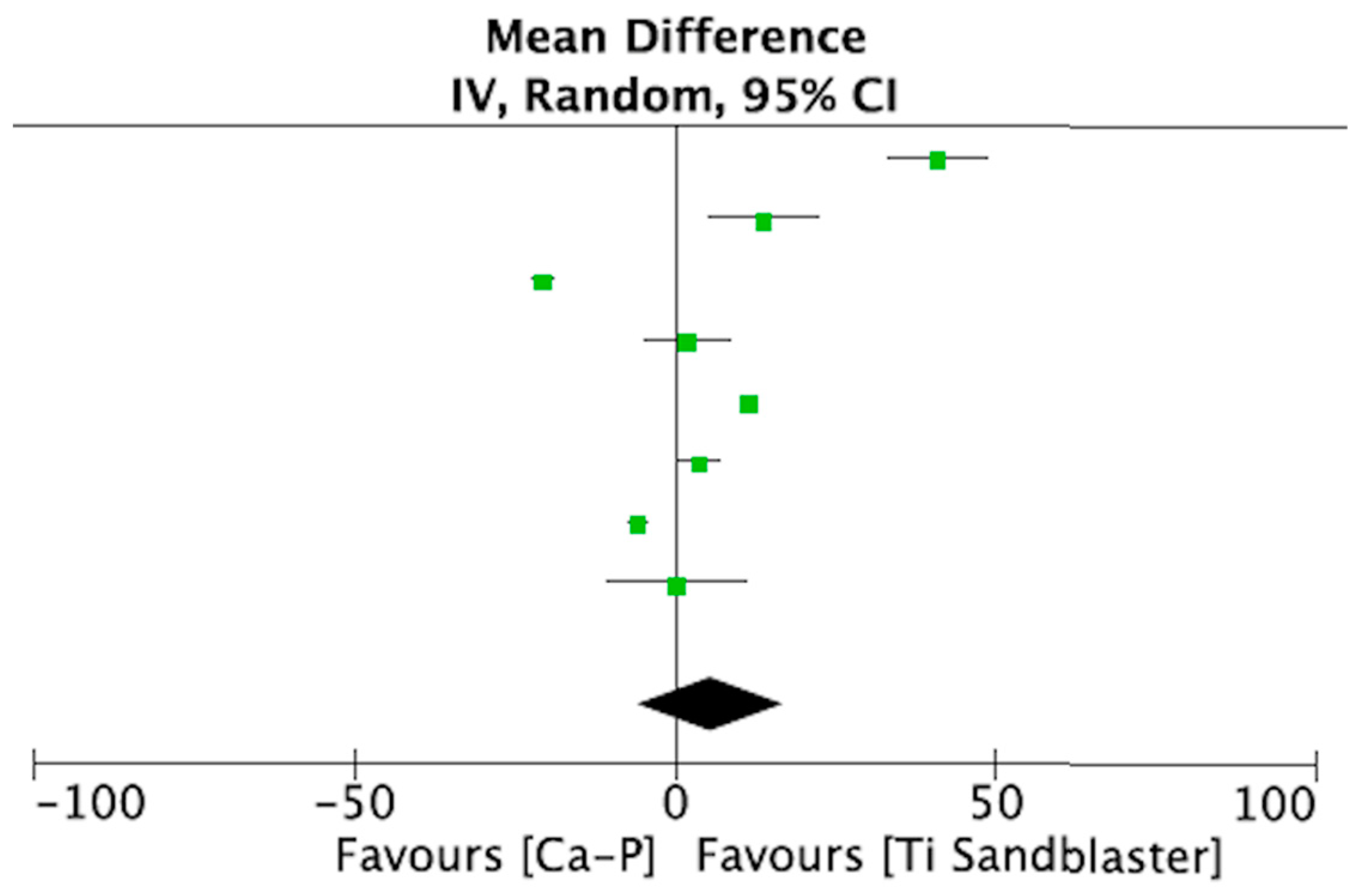
3.4. Quantitative Synthesis (Meta-Analysis)
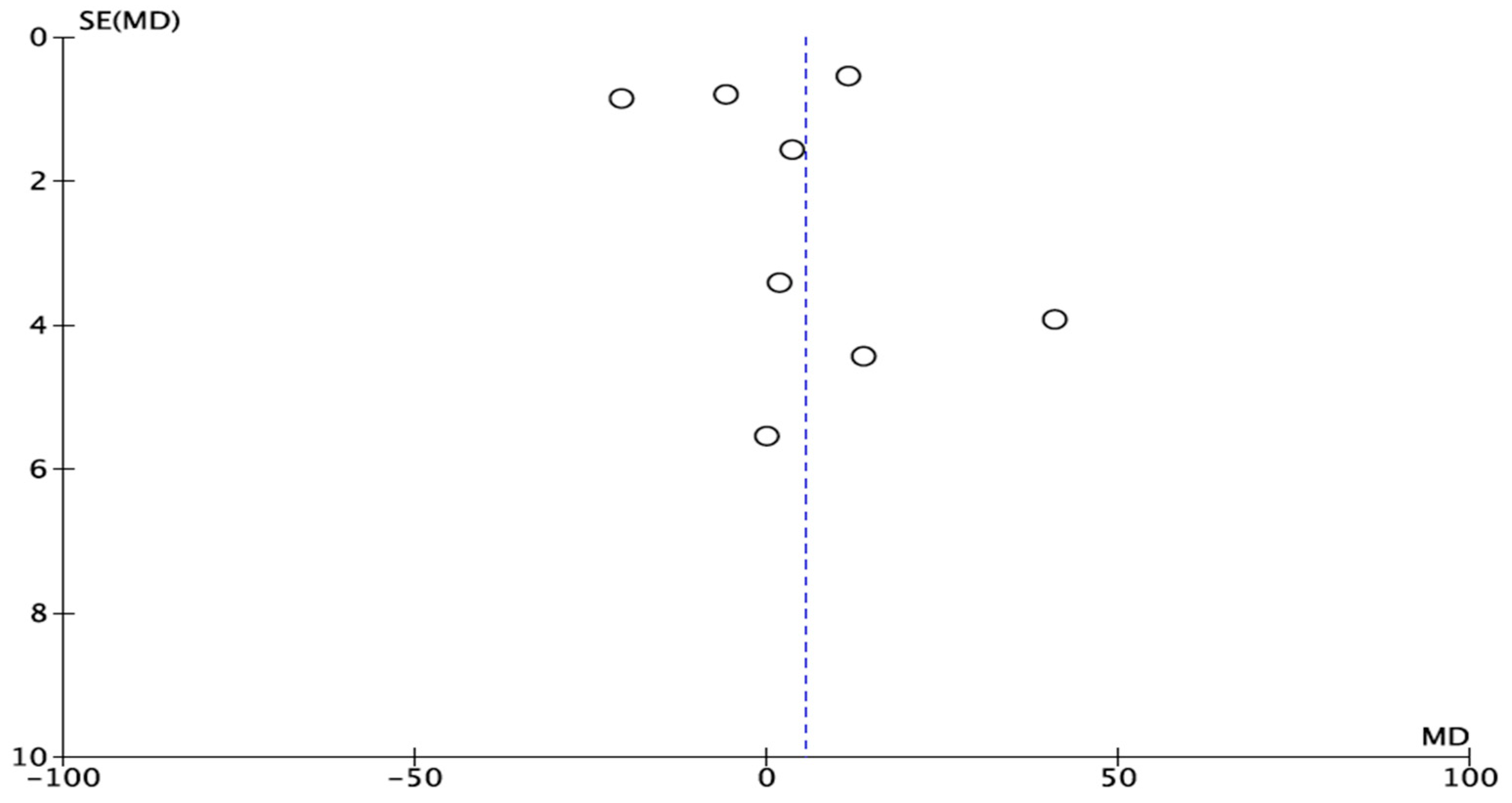
3.5. Publication Bias and Heterogeneity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BA | Bone area |
| BCa-P | Bicalcium phosphate |
| BD | Bone density |
| BIC | Bone-to-implant contact |
| Ca-P | Calcium phosphate |
| CAO | Calcium oxide |
| HA | Hydroxyapatite |
| MeSH | Medical Subject Headings |
| SLA | Sandblasted large grit acid etched |
Appendix A
| Section/Topic | # | Checklist Item | Reported on Page # |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 2 |
| METHODS | |||
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 2 |
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number. | 2 |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | 2 |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 2 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | 2 |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 8 |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 3 |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | 2 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 6 |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | 3 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis. | 7,8 |
References
- Kaur, M.; Singh, K. Review on titanium and titanium-based alloys as biomaterials for orthopaedic applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 102, 844–862. [Google Scholar] [CrossRef] [PubMed]
- Giudice, A.; Bennardo, F.; Antonelli, A.; Barone, S.; Wagner, F.; Fortunato, L.; Traxler, H. Influence of clinician’s skill on primary implant stability with conventional and piezoelectric preparation techniques: An ex-vivo study. J. Biol. Regul. Homeost. Agents 2020, 34, 739–745. [Google Scholar]
- Orsini, G.; Piattelli, M.; Scarano, A.; Petrone, G.; Kenealy, J.; Piattelli, A.; Caputi, S. Randomized, controlledhistologic and histomorphometric evaluation of implants with nanometer-scale calcium phosphate added to the dual acid-etched surface in the human posterior maxilla. J. Periodontol. 2007, 78, 209–218. [Google Scholar] [CrossRef]
- Le Guéhennec, L.; Soueidan, A.; Layrolle, P.; Amouriq, Y. Surface treatments of titanium dental implants for rapid osseointegration. Dent. Mater. 2007, 23, 844–854. [Google Scholar] [CrossRef]
- Winge, M.I.; Reikerås, O.; Røkkum, M. Calcium phosphate bone cement: A possible alternative to autologous bone graft. A radiological and biomechanical comparison in rat tibial bone. Arch. Orthop. Trauma Surg. 2011, 131, 1035–1041. [Google Scholar] [CrossRef]
- Gan, L.; Wang, J.; Tache, A.; Valiquette, N.; Deporter, D.; Pilliar, R. Calcium phosphate sol–gel- derived thin films on porous-surfaced implants for enhanced osteoconductivity Part II: Short-term in vivo studies. Biomaterials 2004, 25, 5313–5321. [Google Scholar] [CrossRef]
- Rey, C. Calcium phosphate biomaterials and bone mineral. Differences in composition, structures and properties. Biomaterials 1990, 11, 13–15. [Google Scholar] [PubMed]
- LeGeros, R.Z. Properties of osteoconductive biomaterials: Calcium phosphates. Clin. Orthop. Relat. Res. 2002, 395, 81–98. [Google Scholar] [CrossRef]
- Wang, D.; Tabassum, A.; Wu, G.; Deng, L.; Wismeijer, D.; Liu, Y. Bone regeneration in critical-sized bone defect enhanced by introducing osteoinductivity to biphasic calcium phosphate granules. Clin. Oral Implant. Res. 2017, 28, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Ambard, A.J.; Mueninghoff, L. Calcium phosphate cement: Review of mechanical and biological properties. J. Prosthodont. 2006, 15, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef]
- Stadlinger, B.; Pourmand, P.; Locher, M.C.; Schulz, M.C. Systematic review of animal models for the study of implant integration, assessing the influence of material, surface and design. J. Clin. Periodontol. 2012, 39, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Koh, J.W.; Kim, Y.S.; Yang, J.H.; Yeo, I.S. Effects of a calcium phosphate-coated and anodized titanium surface on early bone response. Int. J. Oral Maxillofac Implant. 2013, 28, 790–797. [Google Scholar] [CrossRef][Green Version]
- Fontana, F.; Rocchietta, I.; Addis, A.; Schupbach, P.; Zanotti, G.; Simion, M. Effects of a calcium phosphate coating on the osseointegration of endosseous implants in a rabbit model. Clin. Oral Implant. Res. 2011, 22, 760–766. [Google Scholar] [CrossRef] [PubMed]
- Poulos, N.M.; Rodriguez, N.A.; Lee, J.; Rueggeberg, F.A.; Schüpbach, P.; Hall, J.; Susin, C.; Wikesjö, U.M. Evaluation of a novel calcium phosphate-coated titanium porous oxide implant surface: A study in rabbits. Int. J. Oral Maxillofac Implant. 2011, 26, 731–738. [Google Scholar]
- Quaranta, A.; Iezzi, G.; Scarano, A.; Coelho, P.G.; Vozza, I.; Marincola, M.; Piattelli, A. A histomorphometric study of nanothickness and plasma-sprayed calcium-phosphorous-coated implant surfaces in rabbit bone. J. Periodontol. 2010, 81, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Fügl, A.; Ulm, C.; Tangl, S.; Vasak, C.; Gruber, R.; Watzek, G. Long-term effects of magnetron-sputtered calcium phosphate coating on osseointegration of dental implants in non-human primates. Clin. Oral Implant. Res. 2009, 20, 183–188. [Google Scholar]
- Le Guehennec, L.; Goyenvalle, E.; Lopez-Heredia, M.A.; Weiss, P.; Amouriq, Y.; Layrolle, P. Histomorphometric analysis of the osseointegration of four different implant surfaces in the femoral epiphyses of rabbits. Clin. Oral Implant. Res. 2008, 19, 1103–1110. [Google Scholar] [CrossRef]
- Schliephake, H.; Scharnweber, D.; Roesseler, S.; Dard, M.; Sewing, A.; Aref, A. Biomimetic calcium phosphate composite coating of dental implants. Int. J. Oral Maxillofac Implant. 2006, 21, 738–746. [Google Scholar]
- Caulier, H.; van der Waerden, J.P.; Wolke, J.G.; Kalk, W.; Naert, I.; Jansen, J.A. A histological and histomorphometrical evaluation of the application of screw-designed calciumphosphate (Ca-P)-coated implants in the cancellous maxillary bone of the goat. J. Biomed. Mater. Res. 1997, 35, 19–30. [Google Scholar] [CrossRef]
- Alghamdi, H.S.; van Oirschot, B.A.; Bosco, R.; van den Beucken, J.J.; Aldosari, A.A.; Anil, S.; Jansen, J.A. Biological response to titanium implants coated with nanocrystals calcium phosphate or type 1 collagen in a dog model. Clin. Oral Implant. Res. 2013, 24, 475–483. [Google Scholar] [CrossRef]
- Kazemzadeh-Narbat, M.; Noordin, S.; Masri, B.A.; Garbuz, D.S.; Duncan, C.P.; Hancock, R.E.; Wang, R. Drug release and bone growth studies of antimicrobial peptide-loaded calcium phosphate coating on titanium. J. Biomed. Mater. Res. B Appl. Biomater. 2012, 100, 1344–1352. [Google Scholar] [CrossRef] [PubMed]
- Giro, G.; Tovar, N.; Witek, L.; Marin, C.; Silva, N.R.; Bonfante, E.A.; Coelho, P.G. Osseointegration assessment of chairside argon-based nonthermal plasma-treated Ca-P coated dental implants. J. Biomed. Mater. Res. A 2013, 101, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Sun, C.; Wang, Y.; Wang, Y. Early bone apposition and 1-year performance of the electrodeposited calcium phosphate coatings: An experimental study in rabbit femora. Clin. Oral Implant. Res. 2010, 21, 951–960. [Google Scholar] [CrossRef]
- Junker, R.; Manders, P.J.; Wolke, J.; Borisov, Y.; Jansen, J.A. Bone reaction adjacent to microplasma-sprayed CaP-coated oral implants subjected to occlusal load, an experimental study in the dog. Part I: Short-term results. Clin. Oral Implant. Res. 2010, 21, 1251–1263. [Google Scholar] [CrossRef]
- Junker, R.; Manders, P.J.; Wolke, J.; Borisov, Y.; Braceras, I.; Jansen, J.A. Bone reaction adjacent to microplasma-sprayed calcium phosphate-coated oral implants subjected to an occlusal load, an experimental study in the dog. Clin. Oral Implant. Res. 2011, 22, 135–142. [Google Scholar] [CrossRef]
- Schwarz, M.L.; Kowarsch, M.; Rose, S.; Becker, K.; Lenz, T.; Jani, L. Effect of surface roughness, porosity, and a resorbable calcium phosphate coating on osseointegration of titanium in a minipig model. J. Biomed. Mater. Res. A 2009, 89, 667–678. [Google Scholar] [CrossRef] [PubMed]
- Manders, P.J.; Wolke, J.G.; Jansen, J.A. Bone response adjacent to calcium phosphate electrostatic spray deposition coated implants: An experimental study in goats. Clin. Oral Implant. Res. 2006, 17, 548–553. [Google Scholar] [CrossRef]
- Schopper, C.; Moser, D.; Goriwoda, W.; Ziya-Ghazvini, F.; Spassova, E.; Lagogiannis, G.; Auterith, A.; Ewers, R. The effect of three different calcium phosphate implant coatings on bone deposition and coating resorption: A long-term histological study in sheep. Clin. Oral Implant. Res. 2005, 16, 357–368. [Google Scholar] [CrossRef]
- Stewart, M.; Welter, J.F.; Goldberg, V.M. Effect of hydroxyapatite/tricalcium-phosphate coating on osseointegration of plasma-sprayed titanium alloy implants. J. Biomed. Mater. Res. A. 2004, 69, 1–10. [Google Scholar] [CrossRef]
- Yoshinari, M.; Watanabe, Y.; Ohtsuka, Y.; Dérand, T. Solubility control of thin calcium-phosphate coating with rapid heating. J. Dent. Res. 1997, 76, 1485–1494. [Google Scholar] [CrossRef]
- Fuming, H.; Guoli, Y.; Xiaoxiang, W.; Shifang, Z. The removal torque of titanium implant inserted in rabbit femur coated with biomimetic deposited Ca-P coating. J. Oral Rehabil. 2008, 35, 754–765. [Google Scholar] [CrossRef] [PubMed]
- Schouten, C.; Meijer, G.J.; van den Beucken, J.J.; Leeuwenburgh, S.C.; de Jonge, L.T.; Wolke, J.G.; Spauwen, P.H.; Jansen, J.A. In vivo bone response and mechanical evaluation of electrosprayed CaP nanoparticle coatings using the iliac crest of goats as an implantation model. Acta Biomater. 2010, 6, 2227–2236. [Google Scholar] [CrossRef] [PubMed]
- Hayakawa, T.; Yoshinari, M.; Kiba, H.; Yamamoto, H.; Nemoto, K.; Jansen, J.A. Trabecular bone response to surface roughened and calcium phosphate (Ca-P) coated titanium implants. Biomaterials 2002, 23, 1025–1031. [Google Scholar] [CrossRef]
- Vercaigne, S.; Wolke, J.G.C.; Naert, I.; Jansen, J.A. Bone healing capacity of titanium plasma-sprayed and hydroxylapatite-coated oral implants. Clin. Oral Implant. Res. 1998, 9, 261–271. [Google Scholar] [CrossRef]
- Hayakawa, T.; Yoshinari, M.; Nemoto, K.; Wolke, J.G.C.; Jansen, J.A. Effect of surface roughness and calcium phosphate coating on the implant/bone response. Clin. Oral Implant. Res. 2000, 11, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Sergey, V.D. Calcium orthophosphates. J. Mater. Sci. 2007, 42, 1061–1095. [Google Scholar]
- Stellino, G.; Landi, L. A 6-year unloaded hydroxyapatite-coated dental implant placed into an extraction socket in conjunction with nonresorbable hydroxyapatite grafting material: Histologic evaluation. Int. J. Periodontics Restor. Dent. 2002, 22, 575–581. [Google Scholar]
- Yang, Y.L.; Kim, K.H.; Ong, J.L. A review on calcium phosphate coatings produced using a sputtering process an alternative to plasma spraying. Biomaterials 2005, 26, 327–337. [Google Scholar] [CrossRef]
- Lacefield, W.R. Current status of ceramic coatings for dental implants. Implant. Dent. 1998, 7, 315–322. [Google Scholar] [CrossRef]
- Coelho, P.G.; Cardaropoli, G.; Suzuki, M.; Lemons, J.E. Early healing of nanothickness bioceramic coatings on dental implants. An experimental study in dogs. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Abrahamsson, I.; Albouy, J.P.; Lindhe, J. Bone healing at implants with a fluoride-modified surface: An ex- perimental study in dogs. Clin. Oral Implant. Res. 2007, 18, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Mendes, V.C.; Moineddin, R.; Davies, J.E. The effect of discrete calcium phosphate nanocrystals on bone-bonding to titanium surfaces. Biomaterials 2007, 28, 4748–4755. [Google Scholar] [CrossRef] [PubMed]
- Koka, S.; Zarb, G.A. On osseointegration: The healing adaptation principle in the context of osseosufficiency, osseoseparation, and dental implant failure. Int. J. Prosthodont. 2012, 25, 48–52. [Google Scholar] [PubMed]
- Buser, D.; Schenk, R.; Steinemann, S.; Fiorellini, J.; Fox, C.; Stich, H. Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs. J. Biomed. Mater. Res. 1991, 25, 889–902. [Google Scholar] [CrossRef] [PubMed]
- Gotfredsen, K.; Wennerberg, A.; Johansson, C.; Skovgaard, L.T.; Hjorting-Hansen, E. Anchorage of TiO2 -blasted, HA-coated, and machined implants: An experimental study with rabbits. J. Biomed. Mater. Res. 1995, 29, 1223–1231. [Google Scholar] [CrossRef]
- De Bruyn, H.; Christiaens, V.; Doornewaard, R.; Jacobsson, M.; Cosyn, J.; Jacquet, W.; Vervaeke, S. Implant surface roughness and patient factors on long-term peri-implant bone loss. Periodontology 2000 2017, 73, 218–227. [Google Scholar] [CrossRef]
- Daculsi, G.; Laboux, O.; Malard, O.; Weiss, P. Current state of the art of biphasic calcium phosphate bioceramics. J. Mater. Sci. Mater. Med. 2003, 14, 195–200. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Calcium orthophosphate coatings, films and layers. Prog. Biomater. 2012, 26, 1. [Google Scholar] [CrossRef] [PubMed]
- Paital, S.R.; Dahotre, N.B. Wettability and kinetics of hydroxyapatite precipitation on a laser-textured Ca–P bioceramic coating. Acta Biomater. 2009, 5, 2763–2772. [Google Scholar] [CrossRef] [PubMed]
| Population (P) | Unmodified animals (osteoporotic, diabetic…) receiving endosseous titanium implants. |
| Intervention (I) | Ti implants with Ca-P incorporation. |
| Comparison (C) | Ti implants with conventional etched surfaces (SLA type). |
| Outcomes (O) | Bone formation around the implant surface (bone-to-implant contact, BIC). |
| Study design (S) | Preclinical studies with at least six animals and 4 weeks follow-up. |
| Studies | Koh et al. 2013 [15] | Fontana et al. 2011 [16] | Poulos et al. 2011 [17] | Quaranta et al. 2010 [18] | Fügl et al. 2009 [19] | Le Guehennec et al. 2008 [20] | Schliephake et al. 2006 [21] | Caulier et al. 1997 [22] |
|---|---|---|---|---|---|---|---|---|
| 1. Title | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Abstract | ||||||||
| 2. Species | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3. Key finding | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Introduction | ||||||||
| 4. Background | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 5. Reasons for animal models | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 6. Objectives | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Methods | ||||||||
| 7. Ethical statement | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 8. Study design | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 9. Experimental procedures | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 10. Experimental animals | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 11. Accommodation and handling of animals | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 |
| 12. Sample size | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 13. Assignment of animals to experimental groups | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 14. Anesthesia | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 15. Statistical methods | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Results | ||||||||
| 16. Experimental results | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 17. Results and estimation | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Discussion | ||||||||
| 18. Interpretation and scientific implications | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 19. 3Rs reported | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 20. Adverse events | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 21. Study limitations | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 22. Generalization/applicability | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 23. Funding | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 |
| Total score | 17 | 17 | 18 | 17 | 17 | 17 | 18 | 17 |
| Studies | Animal Model | Implants (n) | Follow-Up (Weeks) | Analysis Methods | Conclusions |
|---|---|---|---|---|---|
| Koh et al. 2013 [15] | Rabbit model (6) | 12 | 2 and 4 | Histomorphometry BIC | A Ca-P coating on an anodized surface may induce rapid osseointegration at the bone-implant interface and more bone formation near the implant surface. |
| Fontana et al. 2011 [16] | Rabbit model (36) | 216 | 2, 4, and 9 | Histomorphometry BIC | The results using BIC values suggest that the Ca-P coating had no effect on improving bone apposition. |
| Poulos et al. 2011 [17] | Rabbit model (20) | 40 | 2 and 4 | Histomorphometry BIC | The porous titanium oxide implant coated with calcium phosphate behaved similarly to the porous titanium oxide control. |
| Quaranta et al. 2010 [18] | Rabbit model (12) | 48 | 3, 4, and 8 | Histomorphometry BIC | Ca-P coatings were osteoconductive and promoted early bone response. |
| Fügl et al. 2009 [19] | Non-human primate model (9) | 25 | 80 | Histomorphometry BIC | Ca-P coating of implants enhances osteoconductive properties in the initial phase. |
| Le Guehennec et al. 2008 [20] | Rabbit model (20) | 40 | 2 and 8 | Histomorphometry BIC | Higher BIC for the titanium implant coated with biomimetic Ca-P as compared with the grit-blasted implants. The osseointegration of Ca-P-Ti was similar to that observed for implants with etched surfaces. |
| Schliephake et al. 2006 [21] | Foxhound dog model (10) | 10 | 4 and 12 | Histomorphometry BIC | Coating an implant with Ca-P may have a beneficial effect on peri-implant bone regeneration and could improve BIC in the early stages of healing. |
| Caulier et al. 1997 [22] | Goat model (16) | 64 | 16 | Histomorphometry BIC | No final conclusion can be drawn due to the difference in surface roughness between the coated and noncoated implants. |
| Studies | Implant Dimensions, D(Ø) × L (mm) | Implant Shape | Ca-P Incorporation | Surface Coating |
|---|---|---|---|---|
| Koh et al. 2013 [15] | 3.5 Ø × 8 | Screw | Anodization | Mixed HA and CaO |
| Fontana et al. 2011 [16] | 3.75 Ø × 7 | Screw | Oxidation | Ca-P |
| Poulos et al. 2011 [17] | 3.75 Ø × 7 | Screw | Proprietary method (Nobel Biocare®) | Ca-P |
| Quaranta et al. 2010 [18] | 4.5 Ø × 6 | Screw | Ion beam-assisted deposition | Ca-P |
| Fügl et al. 2009 [19] | 3 Ø × 10 | Screw | Magnetron-sputtered | Ca-P |
| Le Guehennec et al. 2008 [20] | 4.2 Ø × 6 | Screw | Blasting | BCa-P |
| Schliephake et al. 2006 [21] | 4 Ø × NR | Screw | Cathodic polarization | Ca-P |
| Caulier et al. 1997 [22] | 3.75 Ø × 10 | Screw | Plasma-spray | Ca-P |
| Study or Subgroup | Exp. Ca-P | Ti Sandblaster | Mean Difference | Year | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Total | Mean | SD | Total | Weight | IV, Random, 95% CI | ||
| Caulier et al. | 67.4 | 27 | 64 | 26.5 | 16.2 | 64 | 12.2% | 40.90 [33.19, 48.61] | 1997 |
| Schliephake et al. | 45.2 | 9 | 10 | 31.5 | 10.8 | 10 | 12.0% | 13.70 [4.99, 22.41] | 2006 |
| Le Guehennec et al. | 47.3 | 3.9 | 40 | 68 | 3.9 | 40 | 12.9% | −20.70 [−22.41, −18.99] | 2008 |
| Fügl et al. | 74.9 | 0.98 | 25 | 73.2 | 17 | 25 | 12.4% | 1.70 [−4.97, 8.37] | 2009 |
| Quaranta et al. | 43 | 3 | 48 | 31.5 | 2.4 | 48 | 13.0% | 11.50 [10.41, 12.59] | 2010 |
| Fontana et al. | 31.37 | 17.79 | 216 | 27.68 | 14.66 | 216 | 12.9% | 3.69 [0.62, 6.76] | 2011 |
| Poulos et al. | 73.5 | 4.2 | 40 | 79.4 | 2.8 | 40 | 13.0% | −5.90 [−7.46, −4.34] | 2011 |
| Koh et al. | 53.7 | 10.9 | 12 | 53.6 | 15.8 | 12 | 11.6% | 0.10 [−10.76, 10.96] | 2013 |
| Total (95% CI) | 455 | 455 | 100.0% | 5.40 [−5.85, 16.65] | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Valverde, N.; López-Valverde, A.; Aragoneses, J.M.; Macedo de Sousa, B.; Rodrigues, M.J.; Ramírez, J.M. Systematic Review and Meta-Analysis of the Effectiveness of Calcium-Phosphate Coating on the Osseointegration of Titanium Implants. Materials 2021, 14, 3015. https://doi.org/10.3390/ma14113015
López-Valverde N, López-Valverde A, Aragoneses JM, Macedo de Sousa B, Rodrigues MJ, Ramírez JM. Systematic Review and Meta-Analysis of the Effectiveness of Calcium-Phosphate Coating on the Osseointegration of Titanium Implants. Materials. 2021; 14(11):3015. https://doi.org/10.3390/ma14113015
Chicago/Turabian StyleLópez-Valverde, Nansi, Antonio López-Valverde, Juan Manuel Aragoneses, Bruno Macedo de Sousa, María João Rodrigues, and Juan Manuel Ramírez. 2021. "Systematic Review and Meta-Analysis of the Effectiveness of Calcium-Phosphate Coating on the Osseointegration of Titanium Implants" Materials 14, no. 11: 3015. https://doi.org/10.3390/ma14113015
APA StyleLópez-Valverde, N., López-Valverde, A., Aragoneses, J. M., Macedo de Sousa, B., Rodrigues, M. J., & Ramírez, J. M. (2021). Systematic Review and Meta-Analysis of the Effectiveness of Calcium-Phosphate Coating on the Osseointegration of Titanium Implants. Materials, 14(11), 3015. https://doi.org/10.3390/ma14113015








