How to Reliably Measure Stroke Volume Index in Pulmonary Arterial Hypertension: A Comparison of Thermodilution, Direct and Indirect Fick, and Cardiac MRI
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Right Heart Catheterization
2.3. Cardiac Magnetic Resonance Imaging
2.4. Echocardiography
2.5. Statistics
3. Results
3.1. Clinical Characteristics of the Study Population
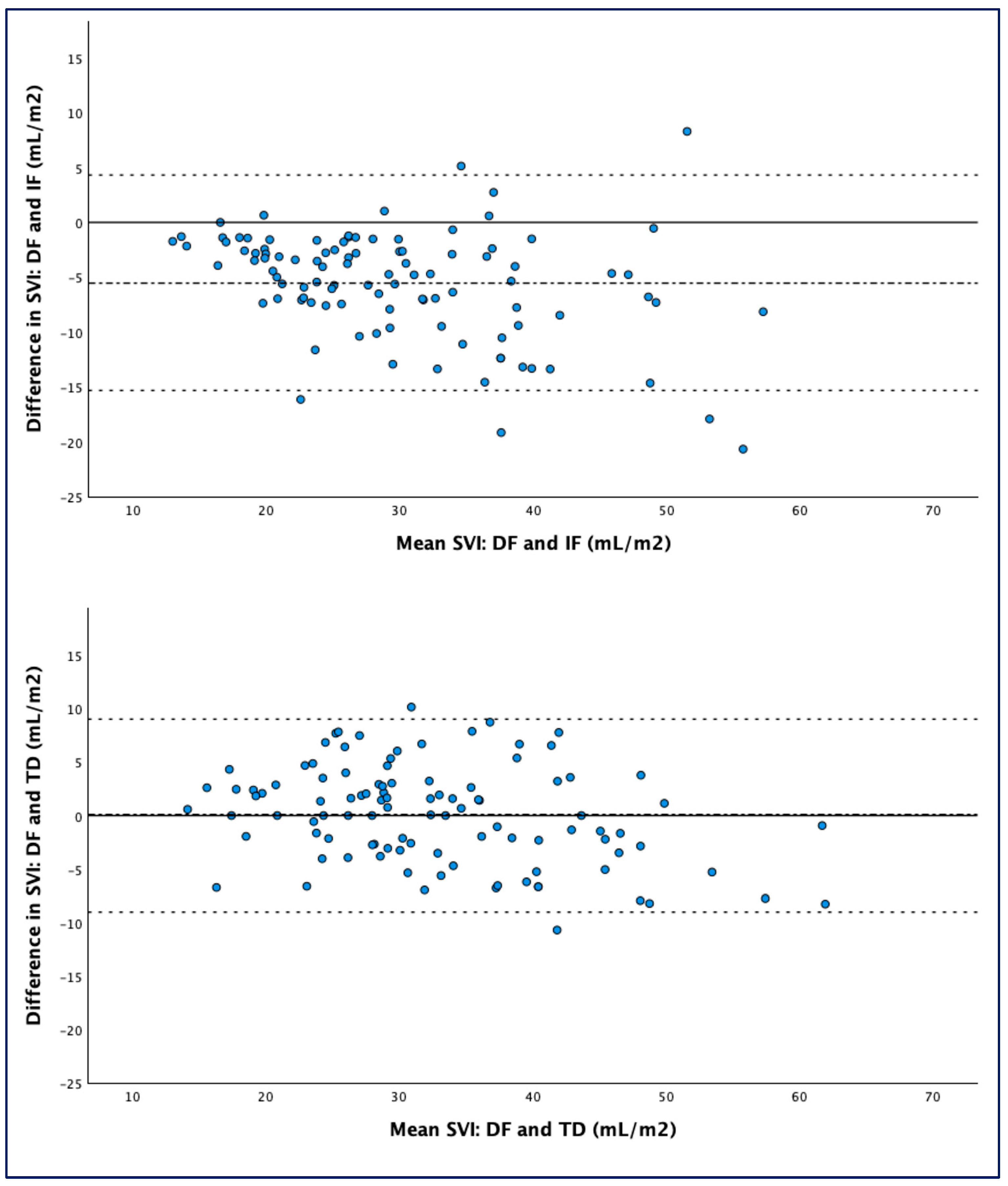
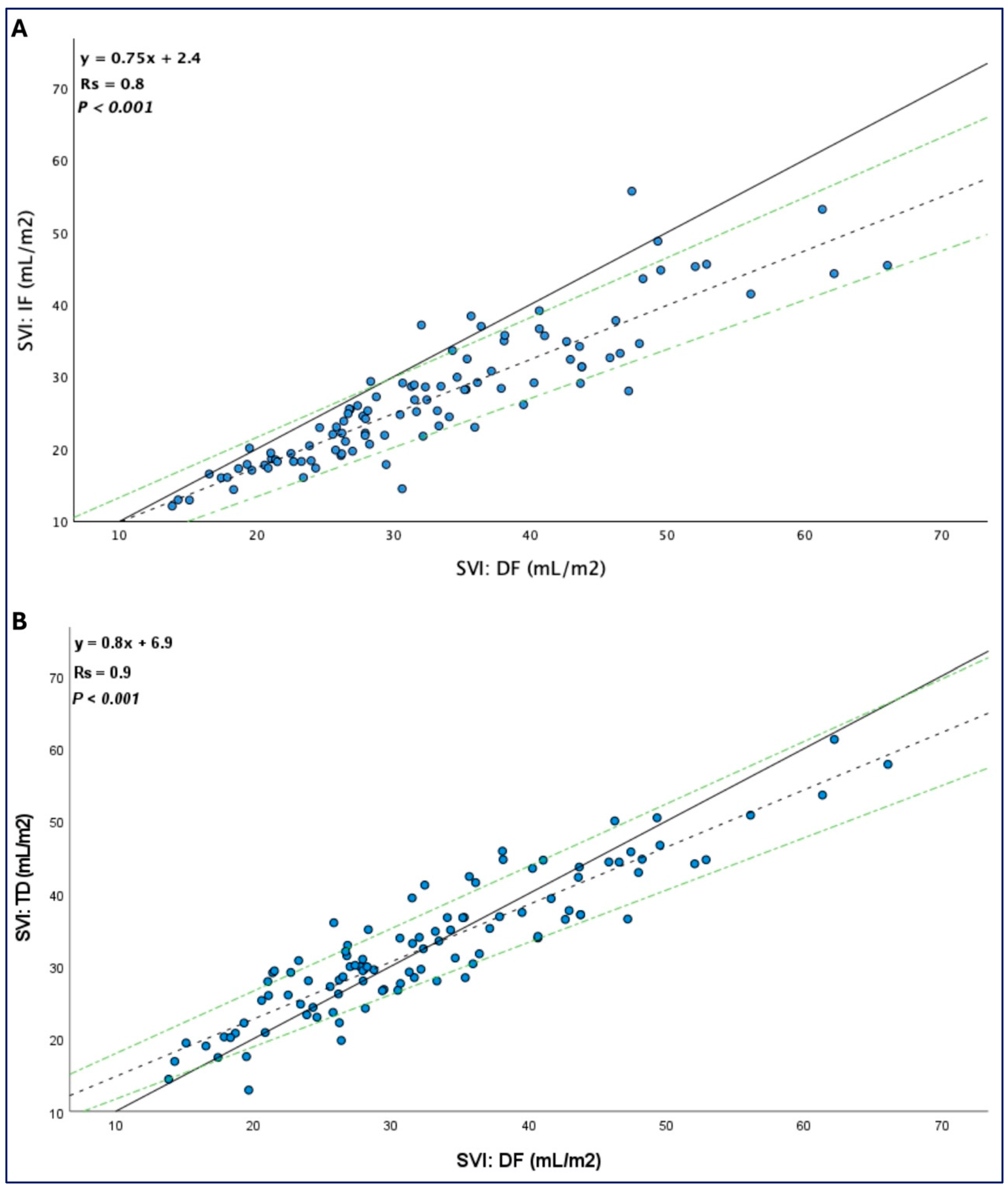
3.2. Thermodilution Shows a Better Agreement with the Gold Standard Direct Fick than Indirect Fick
3.3. Low Cardiac Index and Severe Tricuspid Regurgitation Are Associated with a Greater Bias Between Thermodilution and Direct Fick
3.4. Clinical Implications of the Bias Between Measures
3.5. Cardiac Magnetic Resonance-Derived SVI
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Humbert, M.; Kovacs, G.; Hoeper, M.M.; Badagliacca, R.; Berger, R.M.F.; Brida, M.; Carlsen, J.; Coats, A.J.S.; Escribano-Subias, P.; Ferrari, P.; et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Respir. J. 2023, 61, 2200879. [Google Scholar] [CrossRef] [PubMed]
- Weatherald, J.; Boucly, A.; Chemla, D.; Savale, L.; Peng, M.; Jevnikar, M.; Jaïs, X.; Taniguchi, Y.; O’connell, C.; Parent, F.; et al. Prognostic Value of Follow-Up Hemodynamic Variables After Initial Management in Pulmonary Arterial Hypertension. Circulation 2018, 137, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Boucly, A.; Beurnier, A.; Turquier, S.; Jevnikar, M.; de Groote, P.; Chaouat, A.; Cheron, C.; Jaïs, X.; Picard, F.; Prévot, G.; et al. Risk stratification refinements with inclusion of haemodynamic variables at follow-up in patients with pulmonary arterial hypertension. Eur. Respir. J. 2024, 64, 2400197. [Google Scholar] [CrossRef]
- Dardi, F.; Boucly, A.; Benza, R.; Frantz, R.; Mercurio, V.; Olschewski, H.; Rådegran, G.; Rubin, L.J.; Hoeper, M.M. Risk stratification and treatment goals in pulmonary arterial hypertension. Eur. Respir. J. 2024, 64, 2401323. [Google Scholar] [CrossRef]
- D’alto, M.; Dimopoulos, K.; Coghlan, J.G.; Kovacs, G.; Rosenkranz, S.; Naeije, R. Right Heart Catheterization for the Diagnosis of Pulmonary Hypertension: Controversies and Practical Issues. Heart Fail. Clin. 2018, 14, 467–477. [Google Scholar] [CrossRef]
- Rosenkranz, S.; Preston, I.R. Right heart catheterisation: Best practice and pitfalls in pulmonary hypertension. Eur. Respir. Rev. 2015, 24, 642–652. [Google Scholar] [CrossRef]
- Genecand, L.; Adler, D.; Beghetti, M.; Lador, F. Cardiac Output Determination in Precapillary Pulmonary Hypertension: A Systematic Review. Respiration 2021, 100, 1243–1250. [Google Scholar] [CrossRef]
- Hoeper, M.M.; Maier, R.; Tongers, J.; Niedermeyer, J.; Hohlfeld, J.M.; Hamm, M.; Fabel, H. Determination of Cardiac Output by the Fick Method, Thermodilution, and Acetylene Rebreathing in Pulmonary Hypertension. Am. J. Respir. Crit. Care Med. 1999, 160, 535–541. [Google Scholar] [CrossRef]
- Khirfan, G.; Ahmed, M.K.; Almaaitah, S.; Almoushref, A.; Agmy, G.M.; Dweik, R.A.; Tonelli, A.R. Comparison of Different Methods to Estimate Cardiac Index in Pulmonary Arterial Hypertension. Circulation 2019, 140, 705–707. [Google Scholar] [CrossRef]
- Cigarroa, R.G.; Lange, R.A.; Williams, R.H.; Bedotto, J.B.; Hillis, L.D. Underestimation of cardiac output by thermodilution in patients with tricuspid regurgitation. Am. J. Med. 1989, 86, 417–420. [Google Scholar] [CrossRef]
- van Grondelle, A.; Ditchey, R.V.; Groves, B.M.; Wagner, W.W.; Reeves, J.T. Thermodilution method overestimates low cardiac output in humans. Am. J. Physiol. Circ. Physiol. 1983, 245, H690–H692. [Google Scholar] [CrossRef]
- Mauritz, G.-J.; Marcus, J.T.; Boonstra, A.; Postmus, P.E.; Westerhof, N.; Vonk-Noordegraaf, A. Non-invasive stroke volume assessment in patients with pulmonary arterial hypertension: Left-sided data mandatory. J. Cardiovasc. Magn. Reson. 2008, 10, 51. [Google Scholar] [CrossRef]
- Alabed, S.; Shahin, Y.; Garg, P.; Alandejani, F.; Johns, C.S.; Lewis, R.A.; Condliffe, R.; Wild, J.M.; Kiely, D.G.; Swift, A.J. Cardiac-MRI Predicts Clinical Worsening and Mortality in Pulmonary Arterial Hypertension: A Systematic Review and Meta-Analysis. JACC Cardiovasc. Imaging 2021, 14, 931–942. [Google Scholar] [CrossRef]
- Genecand, L.; Simian, G.; Desponds, R.; Wacker, J.; Ulrich, S.; Lechartier, B.; Fellrath, J.-M.; Sitbon, O.; Beghetti, M.; Lador, F. The Influence of Methods for Cardiac Output Determination on the Diagnosis of Precapillary Pulmonary Hypertension: A Mathematical Model. J. Clin. Med. 2023, 12, 410. [Google Scholar] [CrossRef]
- Narang, N.; Thibodeau, J.T.; Parker, W.F.; Grodin, J.L.; Garg, S.; Tedford, R.J.; Levine, B.D.; McGuire, D.K.; Drazner, M.H. Comparison of Accuracy of Estimation of Cardiac Output by Thermodilution Versus the Fick Method Using Measured Oxygen Uptake. Am. J. Cardiol. 2022, 176, 58–65. [Google Scholar] [CrossRef]
- Desole, S.; Obst, A.; Habedank, D.; Opitz, C.F.; Knaack, C.; Hortien, F.; Heine, A.; Stubbe, B.; Ewert, R. Comparison between thermodilution and Fick methods for resting and exercise-induced cardiac output measurement in patients with chronic dyspnea. Pulm. Circ. 2022, 12, e12128. [Google Scholar] [CrossRef]
- Fares, W.H.; Blanchard, S.K.; Stouffer, G.A.; Chang, P.P.; Rosamond, W.D.; Ford, H.J.; Aris, R.M. Thermodilution and fick cardiac outputs differ: Impact on pulmonary hypertension evaluation. Can. Respir. J. 2012, 19, 261–266. [Google Scholar] [CrossRef]
- Alkhodair, A.; Tsang, M.Y.; Cairns, J.A.; Swiston, J.R.; Levy, R.D.; Lee, L.; Huckell, V.F.; Brunner, N.W. Comparison of thermodilution and indirect Fick cardiac outputs in pulmonary hypertension. Int. J. Cardiol. 2018, 258, 228–231. [Google Scholar] [CrossRef]
- Opotowsky, A.R.; Hess, E.; Maron, B.A.; Brittain, E.L.; Barón, A.E.; Maddox, T.M.; Alshawabkeh, L.I.; Wertheim, B.M.; Xu, M.; Assad, T.R.; et al. Thermodilution vs Estimated Fick Cardiac Output Measurement in Clinical Practice: An Analysis of Mortality From the Veterans Affairs Clinical Assessment, Reporting, and Tracking (VA CART) Program and Vanderbilt University. JAMA Cardiol. 2017, 2, 1090–1099. [Google Scholar] [CrossRef]
- Volodarsky, I.; Kerzhner, K.; Haberman, D.; Cuciuc, V.; Poles, L.; Blatt, A.; Kirzhner, E.; George, J.; Gandelman, G. Comparison between Cardiac Output and Pulmonary Vascular Pressure Measured by Indirect Fick and Thermodilution Methods. J. Pers. Med. 2023, 13, 559. [Google Scholar] [CrossRef]
- Nishikawa, T.; Dohi, S. Errors in the measurement of cardiac output by thermodilution. Can. J. Anaesth. 1993, 40, 142–153. [Google Scholar] [CrossRef]
- Augustine, D.X.; Coates-Bradshaw, L.D.; Willis, J.; Harkness, A.; Ring, L.; Grapsa, J.; Coghlan, G.; Kaye, N.; Oxborough, D.; Robinson, S.; et al. Echocardiographic assessment of pulmonary hypertension: A guideline protocol from the British Society of Echocardiography. Echo Res. Pract. 2018, 5, G11–G24. [Google Scholar] [CrossRef]
- Leong, K.; Howard, L.; Giudice, F.L.; Davies, R.; Haji, G.; Gibbs, S.; Gopalan, D. Utility of cardiac magnetic resonance feature tracking strain assessment in chronic thromboembolic pulmonary hypertension for prediction of REVEAL 2.0 high risk status. Pulm. Circ. 2023, 13, e12116. [Google Scholar] [CrossRef] [PubMed]
- Fegler, G. The reliability of the thermodilution method for determination of the cardiac output and the blood flow in central veins. Q. J. Exp. Physiol. Cogn. Med. Sci. 1957, 42, 254–266. [Google Scholar] [CrossRef]
- Konishi, T.; Nakamura, Y.; Morii, I.; Himura, Y.; Kumada, T.; Kawai, C. Comparison of thermodilution and fick methods for measurement of cardiac output in tricuspid regurgitation. Am. J. Cardiol. 1992, 70, 538–539. [Google Scholar] [CrossRef]
- Gonzalez, J.; Delafosse, C.; Fartoukh, M.; Capderou, A.; Straus, C.; Zelter, M.; Derenne, J.-P.; Similowski, T. Comparison of bedside measurement of cardiac output with the thermodilution method and the Fick method in mechanically ventilated patients. Crit. Care 2003, 7, 171–178. [Google Scholar] [CrossRef]
- McLure, L.E.R.; Peacock, A.J. Cardiac magnetic resonance imaging for the assessment of the heart and pulmonary circulation in pulmonary hypertension. Eur. Respir. J. 2009, 33, 1454–1466. [Google Scholar] [CrossRef]
- Hundley, W.G.; Li, H.F.; Hillis, L.D.; Meshack, B.M.; Lange, R.A.; Willard, J.E.; Landau, C.; Peshock, R.M. Quantitation of cardiac output with velocity-encoded, phase-difference magnetic resonance imaging. Am. J. Cardiol. 1995, 75, 1250–1255. [Google Scholar] [CrossRef] [PubMed]
- Po, J.R.; Tong, M.; Meeran, T.; Potluri, A.; Raina, A.; Doyle, M.; Biederman, R. Quantification of Cardiac Output with Phase Contrast Magnetic Resonance Imaging in Patients with Pulmonary Hypertension. J. Clin. Imaging Sci. 2020, 10, 26. [Google Scholar] [CrossRef]
- Crowe, L.A.; Genecand, L.; Hachulla, A.-L.; Noble, S.; Beghetti, M.; Vallée, J.-P.; Lador, F. Non-Invasive Cardiac Output Determination Using Magnetic Resonance Imaging and Thermodilution in Pulmonary Hypertension. J. Clin. Med. 2022, 11, 2717. [Google Scholar] [CrossRef]


| N = 103 | |
|---|---|
| Age, years | 56 (16) |
| Female, n | 58 (56%) |
| BMI, Kg/m2 | 27.1 (6.3) |
| BSA, m2 # | 1.84 (1.69–2.03) |
| PAH diagnosis | |
| IPAH | 58 (56%) |
| CTD-PAH | 32 (31%) |
| HPAH | 7 (7%) |
| HIV-PAH | 5 (5%) |
| PVOD/PCH | 1 (1%) |
| WHO-FC 1/2/3/4 | 4/32/63/4 |
| Comorbidities | |
| Systemic arterial hypertension | 39 (38%) |
| Ischemic heart disease | 12 (12%) |
| Atrial fibrillation | 14 (14%) |
| COPD | 17 (17%) |
| Chronic kidney disease | 10 (10%) |
| Type 2 Diabetes mellitus | 19 (18%) |
| Echocardiography | |
| RA area indexed, cm2/m2 # | 11.9 (9.5–14.8) |
| LVEF, % | 59 (4) |
| TAPSE, mm | 17 (5) |
| TR 0/1/2/3 | 0/47/36/20 |
| MR 0/1/2/3 | 71/27/5/0 |
| PR 0/1/2/3 | 77/23/3/0 |
| AR 0/1/2/3 | 98/4/1/0 |
| Cardiac magnetic resonance imaging (n = 77) | |
| Heart rate, beats/min | 77 (14) |
| RVEF, % | 40 (13) |
| LVSVI, mL/m2 # | 34 (28.5–42.8) |
| Right heart catheterization | |
| Heart rate, beats/min | 79 (14) |
| Mean systemic BP, mmHg | 86 (14) |
| Measured VO2, mL/min | 246 (49) |
| Estimated VO2, mL/min | 205 (43) |
| Mean RAP, mmHg | 7 (4) |
| Mean PAP, mmHg | 40 (14) |
| Mean PAWP, mmHg | 9 (5) |
| SvO2, % | 62 (10) |
| Median (IQR) | Bias | Limits of Agreement | Median Percentage Error (IQR) | Typical Error | p (vs. DF-SVI) | |
|---|---|---|---|---|---|---|
| IF-SVI | 25.4 (19.4–32.5) | −5.53 | −15.3 to 4.3 | 15 (9–25) | 3.5 | <0.001 |
| TD-SVI | 31.1 (26.7–37.7) | 0.09 | −9.01 to 9.01 | 10 (5–16) | 3.3 | 0.861 |
| TD-SVI (Mild/moderate TR) n = 83 | 32.4 (27.9–41.2) | −0.07 | −9.1 to 8.9 | 10 (5–16) | 3.2 | 0.901 |
| TD-SVI (Severe TR) n = 20 | 28 (22.4–35.5) | 0.84 | −8.66 to 10.1 | 14 (7–17) | 3.4 | 0.573 |
| TD-SVI (CI ≥ 2.2 L/min/m2) n = 67 | 36.4 (29.9–43.7) | −0.9 | −10.1 to 8.3 | 9 (5–15) | 3.3 | 0.107 |
| TD-SVI (CI < 2.2 L/min/m2) n = 36 | 26.9 (20.4–29.5) | 1.9 | −5.9 to 9.7 | 14 (6–23) | 2.8 | 0.007 |
| Median (IQR) | Bias | Limits of Agreement | Median Percent Error (IQR) | Typical Error | p (vs. DF-SVI) | |
|---|---|---|---|---|---|---|
| CMR-SVI | 34 (28.5–42.8) | 0.99 | −3.09 to 5.07 | 5 (3–9) | 1.5 | <0.001 |
| CMR-SVI (Mild/moderate TR) n = 62 | 35.1 (30–45.9) | 0.92 | −3.24 to 5.08 | 5 (3–8) | 1.5 | 0.002 |
| CMR-SVI (Severe TR) n = 15 | 27 (23.2–34.1) | 1.13 | −2.55 to 5.21 | 5 (3–10) | 1.4 | 0.011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baccelli, A.; Gopalan, D.; Davies, R.J.; Haji, G.; Gin-Sing, W.; Howard, L.S.; Lo Giudice, F. How to Reliably Measure Stroke Volume Index in Pulmonary Arterial Hypertension: A Comparison of Thermodilution, Direct and Indirect Fick, and Cardiac MRI. Life 2025, 15, 54. https://doi.org/10.3390/life15010054
Baccelli A, Gopalan D, Davies RJ, Haji G, Gin-Sing W, Howard LS, Lo Giudice F. How to Reliably Measure Stroke Volume Index in Pulmonary Arterial Hypertension: A Comparison of Thermodilution, Direct and Indirect Fick, and Cardiac MRI. Life. 2025; 15(1):54. https://doi.org/10.3390/life15010054
Chicago/Turabian StyleBaccelli, Andrea, Deepa Gopalan, Rachel J. Davies, Gulammehdi Haji, Wendy Gin-Sing, Luke S. Howard, and Francesco Lo Giudice. 2025. "How to Reliably Measure Stroke Volume Index in Pulmonary Arterial Hypertension: A Comparison of Thermodilution, Direct and Indirect Fick, and Cardiac MRI" Life 15, no. 1: 54. https://doi.org/10.3390/life15010054
APA StyleBaccelli, A., Gopalan, D., Davies, R. J., Haji, G., Gin-Sing, W., Howard, L. S., & Lo Giudice, F. (2025). How to Reliably Measure Stroke Volume Index in Pulmonary Arterial Hypertension: A Comparison of Thermodilution, Direct and Indirect Fick, and Cardiac MRI. Life, 15(1), 54. https://doi.org/10.3390/life15010054






