Clinical Outcome of Multiple Platelet-Rich Plasma Injection and Correlation with PDGF-BB in the Treatment of Knee Osteoarthritis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Randomization
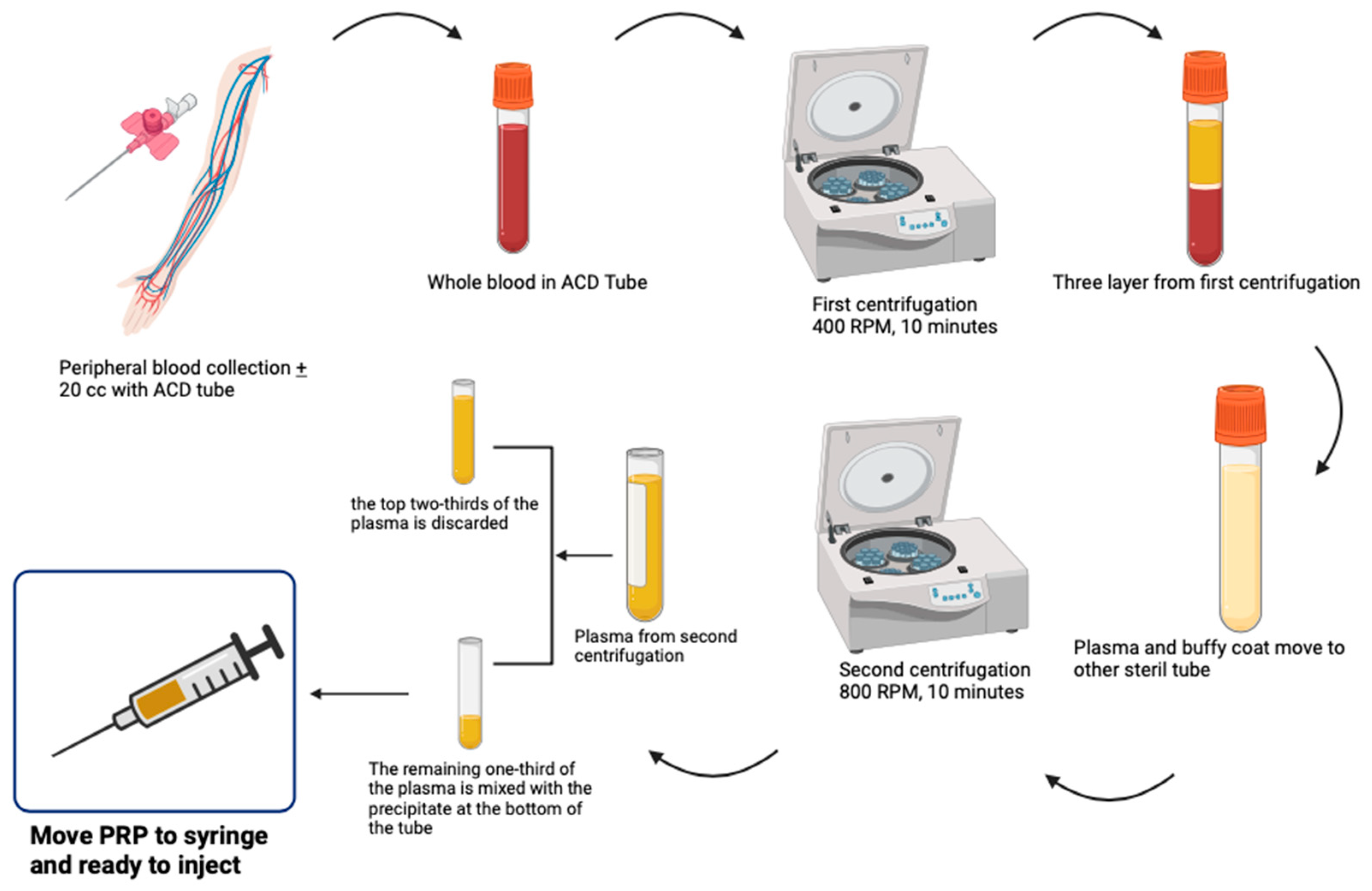
2.2. The Description of PRP
2.3. The Description of HA
2.4. Clinical Outcomes Measures
2.5. Biochemical Assay
2.6. Statistical Analysis
3. Results
3.1. Basic Characteristic
3.2. Clinical Outcomes
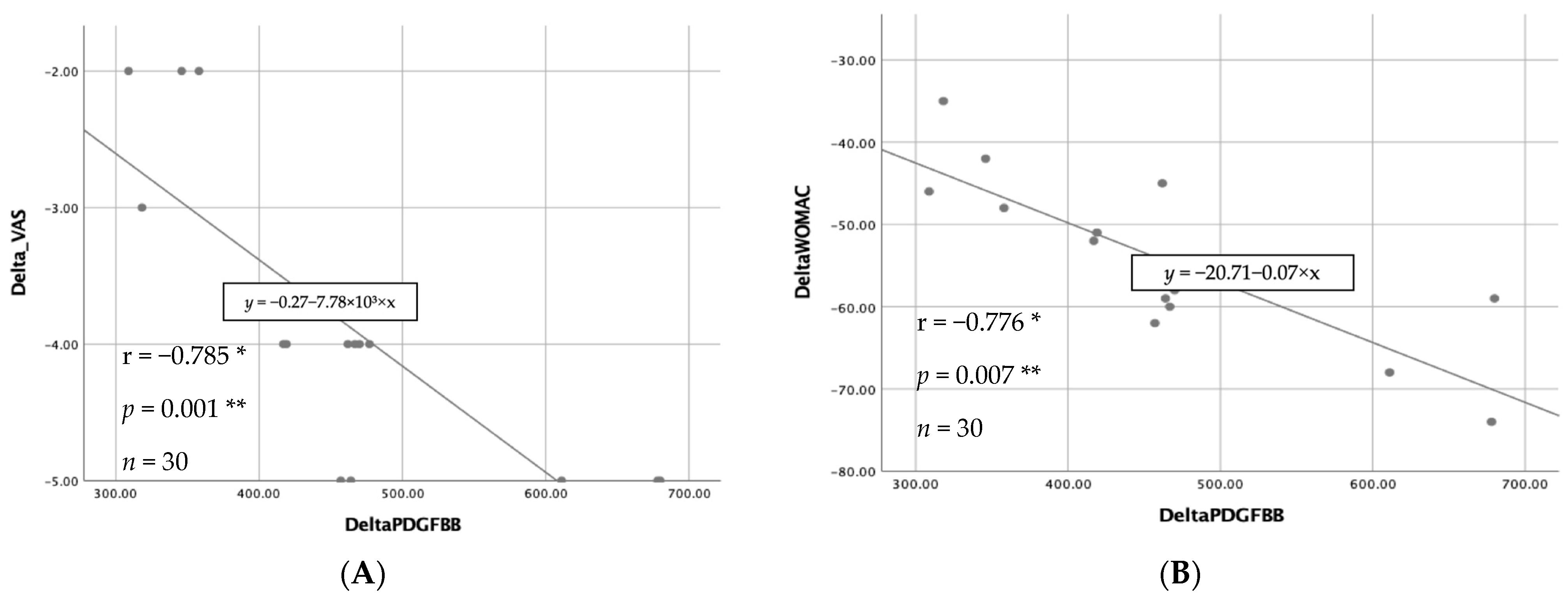
3.3. Biochemical Results
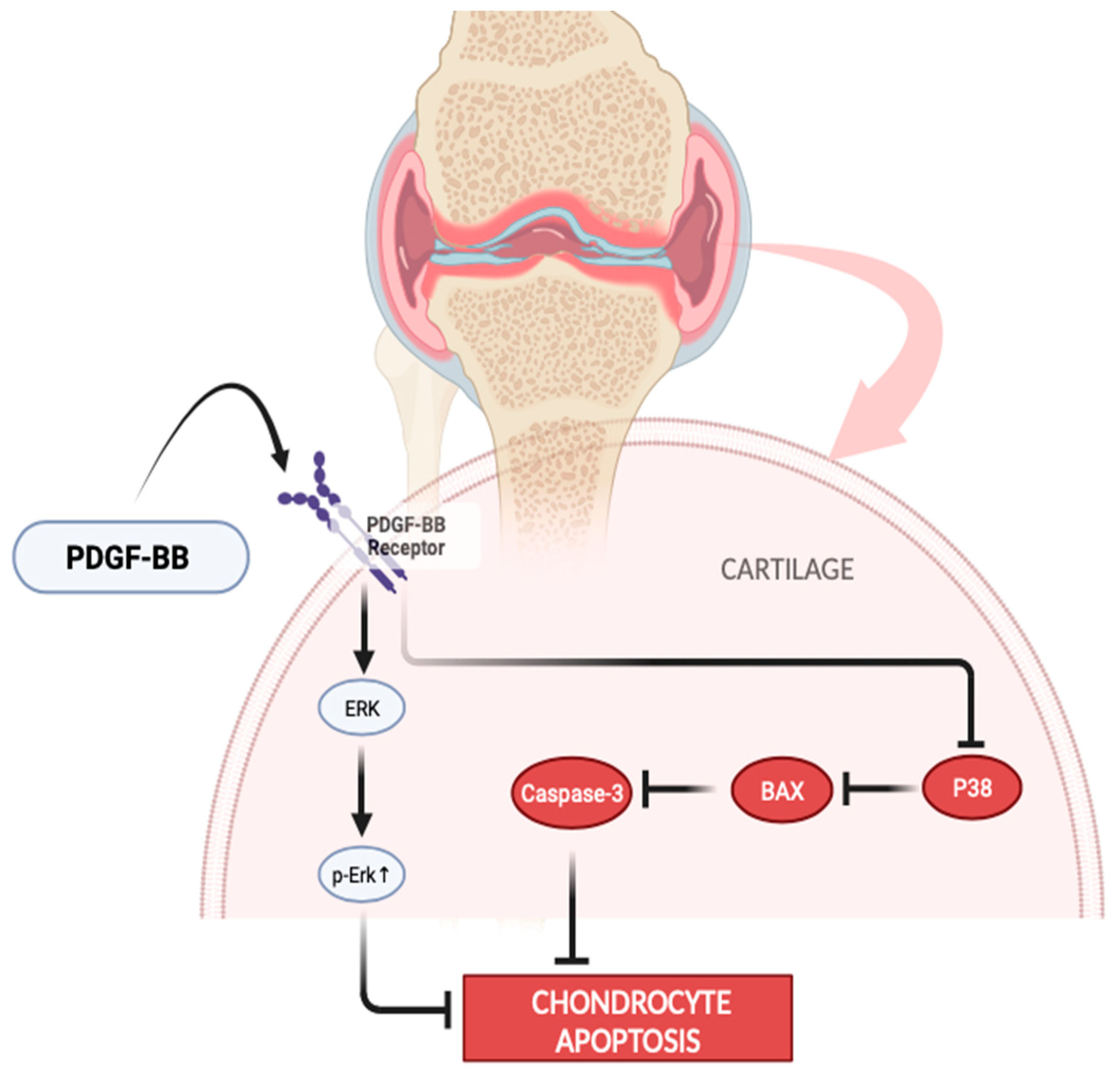
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robinson, W.H.; Lepus, C.M.; Wang, Q.; Raghu, H.; Mao, R.; Lindstrom, T.M.; Sokolove, J. Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat. Rev. Rheumatol. 2016, 12, 580–592. [Google Scholar] [CrossRef]
- Lv, Z.; Yang, Y.X.; Li, J.; Fei, Y.; Guo, H.; Sun, Z.; Lu, J.; Xu, X.; Jiang, Q.; Ikegawa, S.; et al. Molecular Classification of Knee Osteoarthritis. Front. Cell Dev. Biol. 2021, 9, 725568. [Google Scholar] [CrossRef]
- Safiri, S.; Kolahi, A.A.; Smith, E.; Hill, C.; Bettampadi, D.; Mansournia, M.A.; Lu, J.; Xu, X.; Jiang, Q.; Ikegawa, S.; et al. Global, regional and national burden of osteoarthritis 1990–2017: A systematic analysis of the Global Burden of Disease Study 2017. Ann. Rheum. Dis. 2020, 79, 819–828. [Google Scholar] [CrossRef]
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- Di Cesare, P.E.; Haudenschild, D.R.; Samuels, J.; Abramson, S.B. Pathogenesis of Osteoarthritis. In Kelley’s Textbook of Rheumatology, 10th ed.; Firestein, G.S., Budd, R.C., Gabriel, S.E., McInnes, I.B., O’Dell, J.R., Eds.; Elsevier: Philadelphia, PA, USA, 2012; Volume 2, pp. 1617–1635. [Google Scholar] [CrossRef]
- Miller, L.E. Towards reaching consensus on hyaluronic acid efficacy in knee osteoarthritis. Clin. Rheumatol. 2019, 38, 2881–2883. [Google Scholar] [CrossRef]
- Farkas, B.; Kvell, K.; Czömpöly, T.; Illés, T.; Bárdos, T. Increased chondrocyte death after steroid and local anesthetic combination. Clin. Orthop. Relat. Res. 2010, 468, 3112–3120. [Google Scholar] [CrossRef]
- Nakazawa, F.; Matsuno, H.; Yudoh, K.; Watanabe, Y.; Katayama, R.; Kimura, T. Corticosteroid treatment induces chondrocyte apoptosis in an experimental arthritis model in chondrocyte cultures. Clin. Exp. Rheumatol. 2002, 20, 773–781. [Google Scholar]
- Phillips, M.; Bhandari, M.; Grant, J.; Bedi, A.; Trojian, T.; Johnson, A.; Schemitsch, E. A Systematic Review of Current Clinical Practice Guidelines on Intra-articular Hyaluronic Acid, Corticosteroid, and Platelet-Rich Plasma Injection for Knee Osteoarthritis: An International Perspective. Orthop. J. Sport Med. 2021, 9, 23259671211030272. [Google Scholar] [CrossRef] [PubMed]
- Lana, J.F.S.D.; Weglein, A.; Sampson, S.E.; Vicente, E.F.; Huber, S.C.; Souza, C.V.; Ambach, M.A.; Vincent, H.; Urban-Paffaro, A.; Onodera, C.M.K.; et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J. Stem Cells Regen. Med. 2016, 12, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.B.; Kim, J.H.; Ha, C.W.; Lee, D.H. Clinical Efficacy of Platelet-Rich Plasma Injection and Its Association With Growth Factors in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized Double-Blind Controlled Clinical Trial As Compared With Hyaluronic Acid. Am. J. Sports Med. 2021, 49, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Trojian, T.H.; Concoff, A.L.; Joy, S.M.; Hatzenbuehler, J.R.; Saulsberry, W.J.; Coleman, C.I. AMSSM scientific statement concerning viscosupplementation injections for knee osteoarthritis: Importance for individual patient outcomes. Br. J. Sports Med. 2016, 50, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Mazzocca, A.D.; McCarthy, M.B.R.; Chowaniec, D.M.; Dugdale, E.M.; Hansen, D.; Cote, M.P.; Bradley, J.P.; Romeo, A.A.; Arciero, R.A.; Beitzel, K. The positive effects of different platelet-rich plasma methods on human muscle, bone, and tendon cells. Am. J. Sports Med. 2012, 40, 1742–1749. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Zhang, C.; Tuan, R.S. Biology of platelet-rich plasma and its clinical application in cartilage repair. Arthritis Res. Ther. 2014, 16, 204–215. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.J.; Sun, J.B.; Bi, Z.G.; Wang, X.M.; Yang, C.L. Evaluation of platelet-rich plasma and fibrin matrix to assist in healing and repair of rotator cuff injuries: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 158–172. [Google Scholar] [CrossRef] [PubMed]
- Laudy, A.B.M.; Bakker, E.W.P.; Rekers, M.; Moen, M.H. Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 657–672. [Google Scholar] [CrossRef]
- Zhu, P.; Wang, Z.; Sun, Z.; Liao, B.; Cai, Y. Recombinant platelet-derived growth factor-BB alleviates osteoarthritis in a rat model by decreasing chondrocyte apoptosis in vitro and in vivo. J. Cell Mol. Med. 2021, 25, 7472–7484. [Google Scholar] [CrossRef]
- Mochizuki, T.; Ushiki, T.; Watanabe, S.; Omori, G.; Kawase, T. The levels of TGFβ1, VEGF, PDGF-BB, and PF4 in platelet-rich plasma of professional soccer players: A cross-sectional pilot study. J. Orthop. Surg. Res. 2022, 17, 465. [Google Scholar] [CrossRef] [PubMed]
- Fredriksson, L.; Li, H.; Eriksson, U. The PDGF family: Four gene products form five dimeric isoforms. Cytokine Growth Factor Rev. 2004, 15, 197–204. [Google Scholar] [CrossRef]
- Cheng, P.G.; Yang, K.D.; Huang, L.G.; Wang, C.H.; Ko, W.S. Comparisons of Cytokines, Growth Factors and Clinical Efficacy between Platelet-Rich Plasma and Autologous Conditioned Serum for Knee Osteoarthritis Management. Biomolecules 2023, 13, 555. [Google Scholar] [CrossRef]
- Verma, R.; Kandwal, A.; Negi, G.; Chandra, H. Factors affecting the quantity and quality of platelet-rich plasma and platelet-derived growth factor-BB: An observational study. J. Bio-X Res. 2021, 4, 67–70. [Google Scholar] [CrossRef]
- Lansdown, D.A.; Fortier, L.A. Platelet-Rich Plasma: Formulations, Preparations, Constituents, and Their Effects. Oper. Tech. Sports Med. 2017, 25, 7–12. [Google Scholar] [CrossRef]
- Croisé, B.; Paré, A.; Joly, A.; Louisy, A.; Laure, B.; Goga, D. Optimized centrifugation preparation of the platelet rich plasma: Literature review. J. Stomatol. Oral. Maxillofac. Surg. 2020, 121, 150–154. [Google Scholar] [CrossRef]
- Amo CDel Perez-Valle, A.; Atilano, L.; Andia, I. Unraveling the Signaling Secretome of Platelet-Rich Plasma: Towards a Better Understanding of Its Therapeutic Potential in Knee Osteoarthritis. J. Clin. Med. 2022, 11, 473. [Google Scholar] [CrossRef]
- Görmeli, G.; Görmeli, C.A.; Ataoglu, B.; Çolak, C.; Aslantürk, O.; Ertem, K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: A randomized, double-blind, placebo-controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Kon, E.; Mandelbaum, B.; Buda, R.; Filardo, G.; Delcogliano, M.; Timoncini, A.; Fornasari, P.M.; Giannini, S.; Marcacci, M. Platelet-Rich Plasma Intra-Articular Injection Versus Hyaluronic Acid Viscosupplementation as Treatments for Cartilage Pathology: From Early Degeneration to Osteoarthritis. Arthroscopy 2011, 11, 1490–1501. [Google Scholar] [CrossRef] [PubMed]
- Filardo, G.; Di Matteo, B.; Di Martino, A.; Merli, M.L.; Cenacchi, A.; Fornasari, P.; Marcacci, M.; Kon, E. Platelet-rich plasma intra-articular knee injections show no superiority versus viscosupplementation: A randomized controlled trial. Am. J. Sports Med. 2015, 43, 1575–1582. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.Y.; Hsu, C.W.; Lin, G.C.; Lin, H.S.; Chou, Y.J.; Liou, I.H.; Sun, S.-F. Comparing efficacy of a single intraarticular injection of platelet-rich plasma (PRP) combined with different hyaluronans for knee osteoarthritis: A randomized-controlled clinical trial. BMC Musculoskelet. Disord. 2022, 23, 954. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, R.H.; Turk, D.C.; Wyrwich, K.W.; Beaton, D.; Cleeland, C.S.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Kerns, R.D.; Ader, D.N.; et al. Interpreting the Clinical Importance of Treatment Outcomes in Chronic Pain Clinical Trials: IMMPACT Recommendations. J. Pain 2008, 9, 105–121. [Google Scholar] [CrossRef]
- Ngarmukos, S.; Tanavalee, C.; Amarase, C.; Phakham, S.; Mingsiritham, W.; Reantragoon, R.; Leearamwat, N.; Kongkaew, T.; Tharakhet, K.; Honsawek, S.; et al. Two or four injections of platelet-rich plasma for osteoarthritic knee did not change synovial biomarkers but similarly improved clinical outcomes. Sci. Rep. 2021, 11, 23603. [Google Scholar] [CrossRef]
- Li, S.; Xing, F.; Yan, T.; Zhang, S.; Chen, F. Multiple Injections of Platelet-Rich Plasma Versus Hyaluronic Acid for Knee Osteoarthritis: A Systematic Review and Meta-Analysis of Current Evidence in Randomized Controlled Trials. J. Pers. Med. 2023, 13, 429. [Google Scholar] [CrossRef]
- Kabiri, A.; Esfandiari, E.; Esmaeili, A.; Hashemibeni, B.; Pourazar, A.; Mardani, M. Platelet-rich plasma application in chondrogenesis. Adv. Biomed. Res. 2014, 3, 138. [Google Scholar] [CrossRef]
- Lee, H.R.; Park, K.M.; Joung, Y.K.; Park, K.D.; Do, S.H. Platelet-rich plasma loaded hydrogel scaffold enhances chondrogenic differentiation and maturation with up-regulation of CB1 and CB2. J. Control. Release 2012, 159, 332–337. [Google Scholar] [CrossRef]
- Wu, C.C.; Chen, W.H.; Zao, B.; Lai, P.L.; Lin, T.C.; Lo, H.Y.; Shieh, Y.-H.; Wu, C.-H.; Deng, W.-P. Regenerative potentials of platelet-rich plasma enhanced by collagen in retrieving pro-inflammatory cytokine-inhibited chondrogenesis. Biomaterials 2011, 32, 5847–5854. [Google Scholar] [CrossRef]
- Su, C.A.; Jildeh, T.R.; Vopat, M.L.; Waltz, R.A.; Millett, P.J.; Provencher, M.T.; Philippon, M.J.; Huard, J. Current State of Platelet-Rich Plasma and Cell-Based Therapies for the Treatment of Osteoarthritis and Tendon and Ligament Injuries. J. Bone Jt. Surg. 2022, 104, 1406–1414. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.E. Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant. Dent. 2001, 10, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Nugraha, H.K.; Muljanti, M.; Hernaningsih, Y.; Nugraha, J. Platelet Rich Plasma Preparation Protocols: A Preliminary Study. Indones. J. Trop. Infect. Dis. 2016, 3, 104. [Google Scholar] [CrossRef]
- Jain, N.K.; Gulati, M. Platelet-rich plasma: A healing virtuoso. Blood Res. 2016, 51, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Sundman, E.A.; Cole, B.J.; Karas, V.; Della Valle, C.; Tetreault, M.W.; Mohammed, H.O.; Fortier, L.A. The anti-inflammatory and matrix restorative mechanisms of platelet-rich plasma in osteoarthritis. Am. J. Sports Med. 2014, 42, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Sánchez, M.; Nurden, A.T.; Zalduendo, M.M.; De la Fuente, M.; Azofra, J.; Andia, I. Platelet-released growth factors enhance the secretion of hyaluronic acid and induce hepatocyte growth factor production by synovial fibroblasts from arthritic patients. Rheumatology 2007, 46, 1769–1772. [Google Scholar] [CrossRef] [PubMed]
- Szwedowski, D.; Szczepanek, J.; Paczesny, Ł.; Pękała, P.; Zabrzyński, J.; Kruczyński, J. Genetics in cartilage lesions: Basic science and therapy approaches. Int. J. Mol. Sci. 2020, 21, 5430. [Google Scholar] [CrossRef] [PubMed]
- Cook, C.S.; Smith, P.A. Clinical Update: Why PRP Should Be Your First Choice for Injection Therapy in Treating Osteoarthritis of the Knee. Curr. Rev. Musculoskelet. Med. 2018, 11, 583–592. [Google Scholar] [CrossRef]
- Xiong, Y.; Gong, C.; Peng, X.; Liu, X.; Su, X.; Tao, X.; Li, Y.; Wen, Y.; Li, W. Efficacy and safety of platelet-rich plasma injections for the treatment of osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Front. Med. 2023, 10, 1204144. [Google Scholar] [CrossRef]
- Magalon, J.; Bausset, O.; Serratrice, N.; Giraudo, L.; Aboudou, H.; Veran, J.; Magalon, G.; Dignat-Georges, F.; Sabatier, F. Characterization and comparison of 5 platelet-rich plasma preparations in a single-donor model. Arthrosc.-J. Arthrosc. Relat. Surg. 2014, 30, 629–638. [Google Scholar] [CrossRef]
- Gato-Calvo, L.; Magalhaes, J.; Ruiz-Romero, C.; Blanco, F.J.; Burguera, E.F. Platelet-rich plasma in osteoarthritis treatment: Review of current evidence. Ther. Adv. Chronic Dis. 2019, 10, 2040622319825567. [Google Scholar] [CrossRef] [PubMed]
- Etulain, J.; Mena, H.A.; Meiss, R.P.; Frechtel, G.; Gutt, S.; Negrotto, S.; Schattner, M. An optimised protocol for platelet-rich plasma preparation to improve its angiogenic and regenerative properties. Sci. Rep. 2018, 8, 1513. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhu, P.; Liao, B.; You, H.; Cai, Y. Effects and action mechanisms of individual cytokines contained in PRP on osteoarthritis. J. Orthop. Surg. Res. 2023, 18, 713. [Google Scholar] [CrossRef]
- Xia, T.; Gao, R.; Zhou, G.; Liu, J.; Li, J.; Shen, J. Trans-Cinnamaldehyde Inhibits IL-1β-Stimulated Inflammation in Chondrocytes by Suppressing NF-κB and p38-JNK Pathways and Exerts Chondrocyte Protective Effects in a Rat Model of Osteoarthritis. BioMed Research International. BioMed Res. Int. 2019, 2019, 4039472. [Google Scholar] [CrossRef]
- Cai, Y.; Wang, Z.; Liao, B.; Sun, Z.; Zhu, P. Anti-inflammatory and Chondroprotective Effects of Platelet-derived Growth Factor-BB on Osteoarthritis Rat Models. J. Gerontol. A Biol. Sci. Med. Sci. 2023, 78, 51–59. [Google Scholar] [CrossRef]
- Fernandez-Moure, J.S.; Van Eps, J.L.; Cabrera, F.J.; Barbosa, Z.; Medrano del Rosal, G.; Weiner, B.K.; Ellsworth, W.A.; Tasciotti, E. Platelet-rich plasma: A biomimetic approach to enhancement of surgical wound healing. J. Surg. Res. 2017, 207, 33–44. [Google Scholar] [CrossRef]
- Hwang, H.S.; Kim, H.A. Chondrocyte apoptosis in the pathogenesis of osteoarthritis. Int. J. Mol. Sci. 2015, 16, 26035–26054. [Google Scholar] [CrossRef] [PubMed]
- Ji, B.; Ma, Y.; Wang, H.; Fang, X.; Shi, P. Activation of the P38/CREB/MMP13 axis is associated with osteoarthritis. Drug Des. Dev. Ther. 2019, 13, 2195–2204. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.D.; Devji, T.; Bhandari, M.; Fierlinger, A.; Niazi, F.; Christensen, R. Clinical benefit of intra-articular saline as a comparator in clinical trials of knee osteoarthritis treatments: A systematic review and meta-analysis of randomized trials. Semin. Arthritis Rheum. 2016, 46, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020, 72, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Jevsevar, D.S.; Brown, G.A.; Jones, D.L.; Matzkin, E.G.; Manner, P.A.; Mooar, P.; Schousboe, J.T.; Stovitz, S.; Sanders, J.O.; Bozic, K.J.; et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on. J. Bone Jt. Surg. 2013, 95, 1885–1886. [Google Scholar] [CrossRef] [PubMed]


| Variable | Total n = 30 (%) | Intervention Group | |
|---|---|---|---|
| PRP (%) | HA (%) | ||
| Age, y, mean ± SD | 55.5 ± 6.2 | 54.3 ± 9.1 | |
| Symptom duration, mo, mean (range) | 60.4 (7–360) | 64.5 (4–360) | |
| Gender | |||
| Female | 28 (93) | 14 (93) | 14 (93) |
| Male | 2 (7) | 1 (7) | 1 (7) |
| BMI | |||
| Severe Underweight (<17) | |||
| Underweight (17–18.4) | 0 | 0 | 0 |
| Normal (18.5–25) | 3 (20) | 0 | 3 (20) |
| Overweight (25.1–27) | 15 (50) | 9 (60) | 6 (40) |
| Obese (>27) | 12 (30) | 6 (40) | 6 (40) |
| Physical Activity | |||
| Mild | 18 (60) | 12 (80) | 6 (40) |
| Moderate | 12 (40) | 3 (20) | 9 (60) |
| Severe | |||
| Kellgren Lawrence Grade | |||
| Grade 2 | 8 (27) | 3 (20) | 5 (33) |
| Grade 3 | 22 (73) | 12 (80) | 10 (67) |
| Serum 25(OH)D Level | |||
| Normal | |||
| Insufficiency | 10 (33) | 0 | 10 (67) |
| Deficiency | 20 (67) | 15 (100) | 5 (33) |
| Mean Pre-VAS | 15 (50) | 5 | 5 |
| Mean Pre-Womac | 15 (50) | 79 | 55 |
| Mean Post-VAS (12 weeks) | 15 (50) | 1 | 2 |
| Mean Post-Womac (12 weeks) | 15 (50) | 20 | 21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Partan, R.U.; Putra, K.M.; Hafizzanovian, H.; Darma, S.; Reagan, M.; Muthia, P.; Radiandina, A.S.; Rahmawati, E. Clinical Outcome of Multiple Platelet-Rich Plasma Injection and Correlation with PDGF-BB in the Treatment of Knee Osteoarthritis. J. Pers. Med. 2024, 14, 183. https://doi.org/10.3390/jpm14020183
Partan RU, Putra KM, Hafizzanovian H, Darma S, Reagan M, Muthia P, Radiandina AS, Rahmawati E. Clinical Outcome of Multiple Platelet-Rich Plasma Injection and Correlation with PDGF-BB in the Treatment of Knee Osteoarthritis. Journal of Personalized Medicine. 2024; 14(2):183. https://doi.org/10.3390/jpm14020183
Chicago/Turabian StylePartan, Radiyati Umi, Khoirun Mukhsinin Putra, Hafizzanovian Hafizzanovian, Surya Darma, Muhammad Reagan, Putri Muthia, Afifah Salshabila Radiandina, and Eny Rahmawati. 2024. "Clinical Outcome of Multiple Platelet-Rich Plasma Injection and Correlation with PDGF-BB in the Treatment of Knee Osteoarthritis" Journal of Personalized Medicine 14, no. 2: 183. https://doi.org/10.3390/jpm14020183






