Utilization of Hydroxyl-Methyl Butyrate, Leucine, Glutamine and Arginine Supplementation in Nutritional Management of Sarcopenia—Implications and Clinical Considerations for Type 2 Diabetes Mellitus Risk Modulation
Abstract
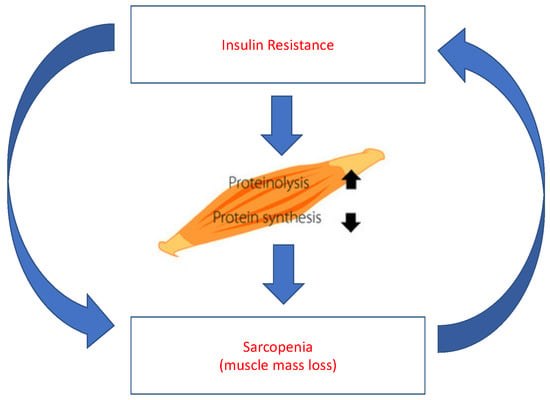
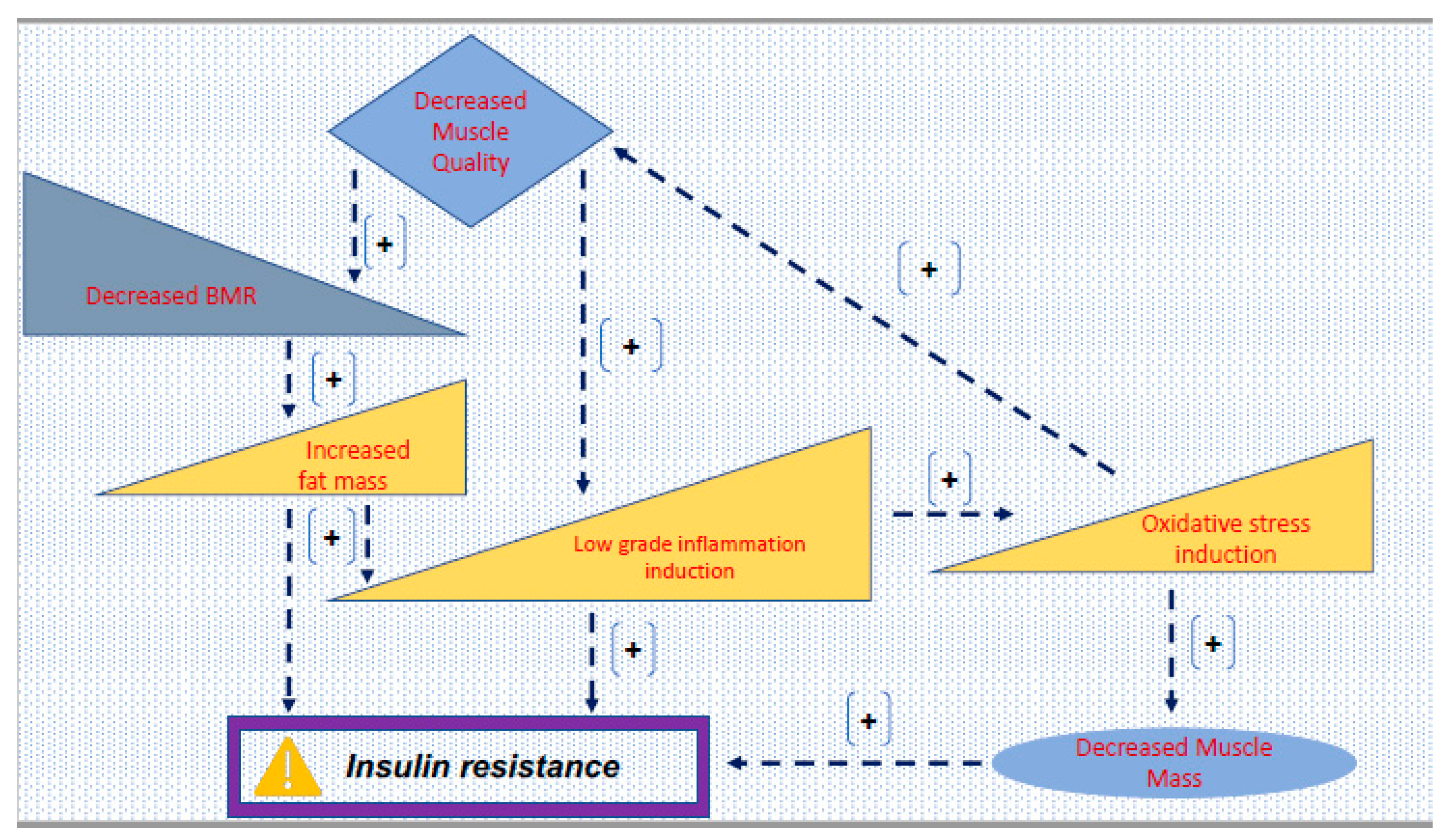
1. Introduction
2. General Considerations for HMB, Gln, Arg, Leu
2.1. Supplementation with HMB
2.2. Supplementation with Leu
2.3. Supplementation with Arg
2.4. Supplementation with Gln
2.5. Supplementation with HMB/Arg/Gln
2.6. Supplementation with Leu/Arg/Gln
3. Discussion
3.1. HMB
3.2. Leu
3.3. HMB and Leu
3.4. Arg—Arg and Gln
3.5. HMB, Gln and Arg
4. Concurrent Therapies for Type 2 Diabetes Mellitus and Sarcopenia
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Tayfur, M. Yaşlı Diyabetik Erkeklerde Sarkopeni; Uzmanlık tezi, İstanbul Üniversitesi Tıp Fakültesi İç Hastalıkları Anabilim Dalı: İstanbul, Türkiye, 2010. [Google Scholar]
- Jong, N. Nutrition and Senescence: Healthy Aging for All in the New Millennium. Nutrition 2000, 16, 537–541. [Google Scholar] [CrossRef]
- Diet, Nutrition and The Prevention of Chronic Diseases; WHO Technical Report Series DSÖ Raporu; Benefits of Physical Activity; Report of a Joint WHO/FAO Expertconsultation: Geneva, Switzerland, 2002; p. 73.
- World Health Organization. Healthy Ageing. In Practical Pointers on Keeping Well; WHO Western Pacific Regional Office: Geneva, Switzerland, 2005. [Google Scholar]
- van Abellan Kan, G. Epidemiology and consequences of sarcopenia. J. Nutr. Health Aging 2009, 13, 708–712. [Google Scholar] [CrossRef]
- Fleg, J.L.; Lakatta, E.G. Role of muscle loss in the age-associated reduction in VO2max. J. Appl. Physiol. 1988, 65, 1147–1151. [Google Scholar] [CrossRef] [PubMed]
- Lindle, R.S.; Metter, E.J.; Lynch, N.A.; Fleg, J.L.; Fozard, J.L.; Tobin, J.; Roy, T.A.; Hurley, B.F. Age and gender comparison of muscle strength in 654 women and men age 20–93 yr. J. Appl. Physiol. 1997, 83, 1581–1587. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, I.H. Sarcopenia: Origins and Clinical Relevance. J. Nutr. 1997, 127, 990S–991S. [Google Scholar] [CrossRef] [PubMed]
- Santilli, V.; Bernetti, A.; Mangone, M.; Paoloni, M. Clinical Definition of Sarcopenia. Clin. Cases Miner. Bone Metab. Off. J. Ital. Soc. Osteoporos. Miner. Metab. Skelet. Dis. 2014, 11, 177–180. [Google Scholar] [CrossRef]
- Sieber, C.C. Malnutrition and sarcopenia. Aging Clin. Exp. Res. 2019, 31, 793–798. [Google Scholar] [CrossRef]
- Marcell, T.J. Sarcopenia: Causes, consequences, and preventions. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, M911–M916. [Google Scholar] [CrossRef]
- Öztürk, Z.A. Tip II Diyabetes Mellituslu Sarkopenik Obez Kişilerde Kan Şekeri Regülasyonunun Sarkopeni Parametreleri Üzerine Etkisi; yan dal uzmanlık tezi, Gaziantep Üniversitesi Tıp Fakültesi İç Hastalıkları Anabiliim Dalı Geriatri Bilim Dalı: Gaziantep, Turkey, 2014. [Google Scholar]
- Boirie, Y. Physiopathological mechanism of sarcopenia. J. Nutr. Heal. Aging 2009, 13, 717–723. [Google Scholar] [CrossRef]
- DeFronzo, R.A.; Devjit, T. Skeletal Muscle Insulin Resistance ıs the Primary Defect in Type 2 Diabetes, Diabetes Care; American Diabetes Association: Arlington, VA, USA, 2009. [Google Scholar]
- Hickson, M. Nutritional interventions in sarcopenia: A critical review. Proc. Nutr. Soc. 2015, 74, 378–386. [Google Scholar] [CrossRef]
- Calvani, R.; Picca, A.; Marini, F.; Biancolillo, A.; Gervasoni, J.; Persichilli, S.; Primiano, A.; Coelho-Junior, H.J.; Bossola, M.; Urbani, A.; et al. A Distinct Pattern of Circulating Amino Acids Characterizes Older Persons with Physical Frailty and Sarcopenia: Results from the BIOSPHERE Study. Nutrients 2018, 10, 1691. [Google Scholar] [CrossRef] [PubMed]
- Candow, D.G.; Forbes, S.C.; Little, J.P.; Cornish, S.M.; Pinkoski, C.; Chilibeck, P.D. Effect of nutritional interventions and resistance exercise on aging muscle mass and strength. Biogerontology 2012, 13, 345–358. [Google Scholar] [CrossRef] [PubMed]
- Wilson, G.J.; Wilson, J.M.; Manninen, A.H. Effects of beta-hydroxy-beta-methylbutyrate (HMB) on exercise performance and body composition across varying levels of age, sex, and training experience: A review. Nutr. Metab. 2008, 5, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Noe, J.E. L-Glutamine use in the treatment and prevention of mucositis and cachexia: A naturopathic perspective. Integr. Cancer Ther. 2009, 8, 409–415. [Google Scholar] [CrossRef]
- Ogawa, M.; Yoshida, N.; Satomi-Kobayashi, S.; Tsuboi, Y.; Komaki, K.; Wakida, K.; Gotake, Y.; Inoue, T.; Tanaka, H.; Yamashita, T.; et al. Efficacy of preoperative amino acid supplements on postoperative physical function and complications in open heart surgery patients: A study protocol for a randomized controlled trial. J. Cardiol. 2019, 74, 360–365. [Google Scholar] [CrossRef]
- Clark, R.H.; Feleke, G.; Din, M.; Yasmin, T.; Singh, G.; Khan, F.A.; Rathmacher, J.A. Nutritional treatment for acquired immunodeficiency virus-associated wasting using β-hyroxy-β-methylbutyrate, glutamine, and arginin: A randomized, double-blind, placebo-controlled study. J. Parenter. Enter. Nutr. 2000, 24, 133–139. [Google Scholar] [CrossRef]
- Hsieh, L.C.; Chow, C.J.; Chang, W.C.; Liu, T.H.; Chang, C.K. Effect of beta hydroxybeta methyl butyrate on protein metabolism in bed ridden elderly receiving tube feeding. Asia Pac. J. Clin. Nutr. 2010, 19, 200–208. [Google Scholar]
- May, P.E.; Barber, A.; D’Olimpio, J.T. Reversal of cancer-related wasting using oral supplementation with a combination of β-hyroxy-β-methylbutyrate, arginine, and glutamine. Am. J. Surg. 2002, 183, 471–479. [Google Scholar] [CrossRef]
- Mero, A. Leucine Supplementation and Intensive Training. Sports Med. 1999, 27, 347–358. [Google Scholar] [CrossRef]
- Berg, J.M.; Tymoczko, J.L.; Stryer, L. Biochemistry, 5th ed.; W H Freeman: New York, NY, USA, 2002; p. 16. [Google Scholar]
- Fukagawa, N.K. Protein and amino acid supplementation in older humans. Amino Acids 2013, 44, 1493–1509. [Google Scholar] [CrossRef]
- Wittmann, F.; Prix, N.; Mayr, S.; Angele, P.; Wichmann, M.W.; van den Engel, N.K.; Hernandez-Richter, T.; Chaudry, I.H.; Jauch, K.W.; Angele, M.K.; et al. l-Arginine Improves Wound Healing after Trauma-Hemorrhage by Increasing Collagen Synthesis. J. Trauma Acute Care Surg. 2005, 59, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.Z.; Abumrad, N.; Barbul, A. Effect of a specialized amino acid mixture on human collagen deposition. Ann. Surg. 2002, 236, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Walrand, S.; Guillet, C.; Salles, J.; Cano, N.; Boirie, Y. Physiopathological mechanism of sarcopenia. Clin. Geriatr. Med. 2011, 27, 365–385. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, L.C.; Chien, S.L.; Huang, S.; Tseng, H.F.; Chang, C.K. Anti-inflammatory and anticatabolic effects of short-term β-hyroxy- β-methylbutyrate supplementation on chronic obstructive pulmonary disease patients in intensive care unit. Asia Pac. J. Clin. Nutr. 2006, 15, 544–550. [Google Scholar] [PubMed]
- Oktaviana, J.; Zanker, J.; Vogrin, S.; Duque, G. The Effect of β-Hydroxy-β-Methylbutyrate (HMB) on Sarcopenia and Functional Frailty in Older Persons: A Systematic Review. J. Nutr. Heal. Aging 2018, 23, 145–150. [Google Scholar] [CrossRef]
- Katsanos, C.S.; Kobayashi, H.; Sheffield-Moore, M.; Aarsland, A.; Wolfe, R.R. A high proportion of Leu is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Am. J. Physiol. Metab. 2006, 291, E381–E387. [Google Scholar]
- Koopman, R.; Verdijk, L.; Manders, R.J.F.; Gijsen, A.P.; Gorselink, M.; Pijpers, E.; Wagenmakers, A.J.; van Loon, L.J.C. Co-ingestion of protein and Leucine stimulates muscle protein synthesis rates to the same extent in young and elderly lean men. Am. J. Clin. Nutr. 2006, 84, 623–632. [Google Scholar] [CrossRef]
- Dardevet, D.; Sornet, C.; Balage, M.; Grizard, J. Stimulation of in vitro rat muscle protein synthesis by Leucine decreases with age. J. Nutr. 2000, 130, 2630–2635. [Google Scholar] [CrossRef]
- Rieu, I.; Sornet, C.; Bayle, G.; Prugnaud, J.; Pouyet, C.; Balage, M.; Papet, I.; Grizard, J.; Dardevet, D. Leucine-supplemented meal feeding for ten days beneficially affects postprandial muscle protein synthesis in old rats. J. Nutr. 2003, 133, 1198–1205. [Google Scholar] [CrossRef]
- Rieu, I.; Balage, M.; Sornet, C.; Giraudet, C.; Pujos, E.; Grizard, J.; Mosoni, L.; Dardevet, D. Leucine supplementation improves muscle protein synthesis in elderly men independently of hyperaminoacidaemia. J. Physiol. 2006, 575, 305–315. [Google Scholar] [CrossRef]
- Debras, E.; Prod’homme, M.; Rieu, I.; Balage, M.; Dardevet, D.; Grizard, J. Postprandial Leucine deficiency failed to alter muscle protein synthesis in growing and adult rats. Nutrition 2007, 23, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Breen, L.; Burd, N.; Hector, A.; Churchward-Venne, T.; Josse, A.; Tarnopolsky, M.A.; Phillips, S. Resistance exercise enhances myofibrillar protein synthesis with graded intakes of whey protein in older men. Nutrition 2007, 23, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Bell, K.E.; Snijders, T.; Zulyniak, M.; Kumbhare, D.; Parise, G.; Chabowski, A.; Phillips, S.M. A whey protein-based multi-ingredient nutritional supplement stimulates gains in lean body mass and strength in healthy older men: A randomized controlled trial. PLOS ONE 2017, 12, e0181387. [Google Scholar] [CrossRef] [PubMed]
- Solerte, S.B.; Gazzaruso, C.; Bonacasa, R.; Rondanelli, M.; Zamboni, M.; Basso, C.; Locatelli, E.; Schifino, N.; Giustina, A.; Fioravanti, M. Nutritional supplements with oral amino acid mixtures increases whole-body lean mass and insulin sensitivity in elderly subjects with sarcopenia. Am. J. Cardiol. 2008, 101, S69–S77. [Google Scholar] [CrossRef] [PubMed]
- Ferrando, A.A.; Paddon-Jones, D.; Hays, N.P.; Kortebein, P.; Ronsen, O.; Williams, R.H.; McComb, A.; Symons, T.B.; Wolfe, R.R.; Evans, W. EAA supplementation to increase nitrogen intake improves muscle function during bed rest in the elderly. Clin. Nutr. 2010, 29, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Rondanelli, M.; Opizzi, A.; Antoniello, N.; Boschi, F.; Iadarola, P.; Pasini, E.; Aquilani, R.; Dioguardi, F.S. Effect of amino acid supplementation on quality of life, amino acid profile and strength in institutionalized elderly patients. Clin. Nutr. 2011, 30, 571–577. [Google Scholar] [CrossRef]
- Xu, Z.E.; Tan, Z.J.; Zhang, Q.; Gui, Q.F.; Yang, Y.M. The effectiveness of Leucine on muscle protein synthesis, lean body mass and leg lean mass accretion in older people: A systematic review and meta-analysis. Br. J. Nutr. 2014, 113, 25–34. [Google Scholar] [CrossRef]
- Murphy, C.H.; Saddler, N.I.; Devries, M.C.; McGlory, C.; Baker, S.K.; Phillips, S.M. Leucine supplementation enhances integrative myofibrillar protein synthesis in free-living older men consuming lower- and higher-protein diets: A parallel-group crossover study. Am. J. Clin. Nutr. 2016, 104, 1594–1606. [Google Scholar] [CrossRef]
- Backx, E.M.P.; Horstman, A.M.H.; Marzuca-Nassr, G.N.; van Kranenburg, J.; Smeets, J.S.; Fuchs, C.J.; Janssen, A.A.W.; de Groot, L.C.P.G.M.; Snijders, T.; Verdijk, L.B.; et al. Leucine Supplementation Does Not Attenuate Skeletal Muscle Loss during Leg Immobilization in Healthy, Young Men. Nutrients 2018, 10, 635. [Google Scholar] [CrossRef]
- Trappe, S.; Creer, A.; Slivka, D.; Minchev, K.; Trappe, T. Single muscle fiber function with concurrent exercise or nutrition countermeasures during 60 days of bed rest in women. J. Appl. Physiol. 2007, 103, 1242–1250. [Google Scholar] [CrossRef]
- Trappe, T.A.; Burd, N.A.; Louis, E.S.; Lee, G.A.; Trappe, S.W. Influence of concurrent exercise or nutrition countermeasures on thigh and calf muscle size and function during 60 days of bed rest in women. Acta Physiol. 2007, 191, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Trappe, S.; Creer, A.; Minchev, K.; Slivka, D.; Louis, E.; Luden, N.; Trappe, T. Human soleus single muscle fiber function with exercise or nutrition countermeasures during 60 days of bed rest. J. Physiol. Integr. Comp. Physiol. 2008, 294, R939–R947. [Google Scholar] [CrossRef] [PubMed]
- Komar, B.; Schwingshackl, L.; Hoffmann, G. Effects of Leucine-rich protein supplements on anthropometric parameter and muscle strength in the elderly: A systematic review and meta-analysis. J. Nutr. Heal. Aging 2014, 19, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Cholewa, J.M.; Dardevet, D.; Lima-Soares, F.; de Araújo Pessôa, K.; Oliveira, P.H.; Dos Santos Pinho, J.R.; Nicastro, H.; Xia, Z.; Cabido, C.E.; Zanchi, N.E. Dietary proteins and amino acids in the control of the muscle mass during immobilization and aging: Role of the MPS response. Amino Acids 2017, 49, 811–820. [Google Scholar] [CrossRef] [PubMed]
- Børsheim, E.; Bui, Q.U.; Tissier, S.; Kobayashi, H.; Ferrando, A.A.; Wolfe, R.R. Effect of amino acid supplementation on muscle mass, strength and physical function in elderly. Clin. Nutr. 2008, 27, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Thalacker-Mercer, A.E.; Drummond, M.J. The importance of dietary protein for muscle health in inactive, hospitalized older adults. Ann. N. Y. Acad. Sci. 2014, 1328, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Souza, M.K.; Moraes, M.R.; Rosa, T.S.; Passos, C.S.; Neves, R.V.P.; Haro, A.S.; Cenedeze, M.A.; Arias, S.C.A.; Fujihara, C.K.; Teixeira, S.A.; et al. l-Arginine Supplementation Blunts Resistance Exercise Improvement in Rats with Chronic Kidney Disease. Life Sci. 2019, 232, 116604. [Google Scholar] [CrossRef]
- Flakoll, P.; Sharp, R.; Baier, S.; Levenhagen, D.; Carr, C.; Nissen, S. Effect of β-hydroxy-β-methylbutyrate, arginine, and lysine supplementation on strength, functionality, body composition, and protein metabolism in elderly women. Nutrition 2004, 20, 445–451. [Google Scholar] [CrossRef]
- Haba, Y.; Fujimura, T.; Oyama, K.; Kinoshita, J.; Miyashita, T.; Fushida, S.; Harada, S.; Ohta, T. Effect of Oral Branched-Chain Amino Acids and Glutamine Supplementation on Skeletal Muscle Atrophy After Total Gastrectomy in Rat Model. J. Surg. Res. 2019, 243, 281–288. [Google Scholar] [CrossRef]
- Mignon, M.; Lêvêque, L.; Bonnel, E.; Meynial-Denis, D. Does Glutamine Supplementation Decrease the Response of Muscle Glutamine Synthesis to Fasting in Muscle in Adult and Very Old Rats? J. Parenter. Enter. Nutr. 2007, 31, 26–31. [Google Scholar] [CrossRef]
- Meynial-Denis, D.; Patureau Mirand, P. Is Glutamine the Cornerstone of Sarcopenia in Very Old Individuals? J. Nutr. Health Aging 2011, 15, 507. [Google Scholar]
- Tatti, P.; Barber, A.E. The use of a specialized nutritional supplement for diabetic foot ulcers reduces the use of antibiotics. J. Endocrinol. Metab. 2012, 2, 26–31. [Google Scholar] [CrossRef][Green Version]
- Baier, S.; Johannsen, D.; Abumrad, N.; Rathmacher, J.A.; Nissen, S.; Flakoll, P. Year-long changes in protein metabolism in elderly men and women supplemented with a nutrition cocktail of betahydroxy-beta-methylbutyrate (HMB), L-arginine, and L-lysine. JPEN 2009, 33, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Olza, J.; Mesa, M.D.; Poyatos, R.M.; Aguilera, C.M.; Moreno-Torres, R.; Perez de la Cruz, A.; Gil, A. A specific protein-enriched enteral formula decreases cortisolemia and improves plasma albumin and amino acid concentrations in elderly patients. Nutr. Metab. 2010, 7, 58. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Nissen, S.; Sharp, R.; Ray, M.; Rathmacher, J.A.; Rice, D.; Fuller, J.C., Jr.; Connelly, A.S.; Abumrad, N. Effect of Leucine metabolite β-hydroxy-β-methylbutyrate on muscle metabolism during resistance-exercise training. J. Appl. Physiol. 1996, 81, 2095–2104. [Google Scholar] [CrossRef]
- Nissen, S.L.; Sharp, R.L. Effect of dietary supplements on lean mass and strength gains with resistance exercise: A meta-analysis. J. Appl. Physiol. 2003, 94, 651–659. [Google Scholar] [CrossRef]
- Marzani, B.; Balage, M.; Vénien, A.; Astruc, T.; Papet, I.; Dardevet, D.; Mosoni, L. Antioxidant supplementation restores defective leucine stimulation of protein synthesis in skeletal muscle from old rats. J. Nutr. 2008, 138, 2205–2211. [Google Scholar] [CrossRef]
- Garlick, P.J.; Grant, I. Amino acid infusion increases the sensitivity of muscle protein synthesis in vivo to insulin. Effect of branched-chain amino acids. Biochem. J. 1988, 254, 579–584. [Google Scholar] [CrossRef]
- Stancliffe, R.A. Role of beta-hydroxy-beta-methylbutyrate (HMB) in Leucine stimulation of mitochondrial biogenesis and fatty acid oxidation. FASEB J. 2012. [Google Scholar] [CrossRef]
- Rathmacher, J.; Nissen, S.; Panton, L.; Clark, R.; May, P.; Barber, A.; D’Olimpio, J.; Abumrad, N. Supplementation with a combination of beta-hydroxy-beta-methylbutyrate (HMB), arginine, and glutamine is safe and could improve hematological parameters. J. Parenter. Enter. Nutr. 2004, 28, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Calvani, R.; Miccheli, A.; Landi, F.; Bossola, M.; Cesari, M.; Leeuwenburgh, C.; Sieber, C.C.; Bernabei, R.; Marzetti, E. Current nutritional recommendations and novel dietary strategies to manage sarcopenia. J. Frailty Aging 2013, 2, 38–53. [Google Scholar] [PubMed]
- Johnson, C.D. Nutrition, Muscle Mass, and Muscular Performance in Middle Age and Beyond. In Proceedings of the The 110th Abbott Nutrition Research Conference, Columbus, OH, USA, 23–25 June 2009. [Google Scholar]
- Sikalidis, A.K.; Maykish, A. The Gut Microbiome and Type 2 Diabetes Mellitus: Discussing a Complex Relationship. Biomedicines 2020, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Betteridge, D.J. What is oxidative stress? Metab. Clin. Exp. 2000, 49 (Suppl. 1), 3–8. [Google Scholar] [CrossRef]
- Hong, S.; Chang, Y.; Jung, H.S.; Yun, K.E.; Shin, H.; Ryu, S. Relative muscle mass and the risk of incident type 2 diabetes: A cohort study. PLOS ONE 2017, 12, e0188650. [Google Scholar] [CrossRef]
- Mesinovic, J.; McMillan, L.B.; Shore-Lorenti, C.; De Courten, B.; Ebeling, P.R.; Scott, D. Metabolic Syndrome and Its Associations with Components of Sarcopenia in Overweight and Obese Older Adults. J. Clin. Med. 2019, 8, 145. [Google Scholar] [CrossRef]
- Clavel, S. Atrophy-related ubiquıtın ligases, Atrogin-1 and MuRF1 are upregulated in aged rat tibialis anterior muscle. Mech. Ageing Dev. 2006, 127, 794–801. [Google Scholar] [CrossRef]
- Scott, D.; de Courten, B.; Ebeling, P.R. Sarcopenia: A potential cause and consequence of type 2 diabetes in Australia’s ageing population? Med. J. Aust. 2016, 205, 329–333. [Google Scholar] [CrossRef]
- Granic, A.; Sayer, A.A.; Robinson, S.M. Dietary Patterns, Skeletal Muscle Health, and Sarcopenia in Older Adults. Nutrients 2019, 11, 745. [Google Scholar] [CrossRef]
- Oh, C.; No, J. Does Protein Intake Affect Metabolic Risk Factors among Older Adults in Korea? J. Obes. Metab. Syndr. 2017, 26, 266–273. [Google Scholar] [CrossRef]
- Sikalidis, A.K.; Stipanuk, M.H. Growing rats respond to a sulfur amino acid-deficient diet by phosphorylation of eIF2α and induction of adaptive components of the integrated stress. J. Nutr. 2010, 140, 1080–1085. [Google Scholar] [CrossRef] [PubMed]
- Sikalidis, A.K.; Mazor, K.M.; Kang, M.; Liu, H.; Stipanuk, M.H. Total 4E-BP1 Is Elevated in Liver of Rats in Response to Low Sulfur Amino Acid Intake. J. Amino Acids 2013, 864757. [Google Scholar] [CrossRef]
| Treatment | Inflammation Prevention | Increased Muscle Protein Synthesis | Reduced Muscle Deterioration | Increased Glucose Tolerance | Other Supplementation Required? | References |
|---|---|---|---|---|---|---|
| HMB | Yes | Yes | Yes | No | Yes | 22, 23, 30, 31 |
| Leu | No | Undetermined | No | Yes | Yes | 32, 33, 34, 35, 36, 37, 38, 45 |
| Gln | No | Yes | Yes | No | Yes | 22, 23, 57 |
| Arg | No | Yes | No | No | Yes | 22, 23, 52, 54 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maykish, A.; Sikalidis, A.K. Utilization of Hydroxyl-Methyl Butyrate, Leucine, Glutamine and Arginine Supplementation in Nutritional Management of Sarcopenia—Implications and Clinical Considerations for Type 2 Diabetes Mellitus Risk Modulation. J. Pers. Med. 2020, 10, 19. https://doi.org/10.3390/jpm10010019
Maykish A, Sikalidis AK. Utilization of Hydroxyl-Methyl Butyrate, Leucine, Glutamine and Arginine Supplementation in Nutritional Management of Sarcopenia—Implications and Clinical Considerations for Type 2 Diabetes Mellitus Risk Modulation. Journal of Personalized Medicine. 2020; 10(1):19. https://doi.org/10.3390/jpm10010019
Chicago/Turabian StyleMaykish, Adeline, and Angelos K. Sikalidis. 2020. "Utilization of Hydroxyl-Methyl Butyrate, Leucine, Glutamine and Arginine Supplementation in Nutritional Management of Sarcopenia—Implications and Clinical Considerations for Type 2 Diabetes Mellitus Risk Modulation" Journal of Personalized Medicine 10, no. 1: 19. https://doi.org/10.3390/jpm10010019
APA StyleMaykish, A., & Sikalidis, A. K. (2020). Utilization of Hydroxyl-Methyl Butyrate, Leucine, Glutamine and Arginine Supplementation in Nutritional Management of Sarcopenia—Implications and Clinical Considerations for Type 2 Diabetes Mellitus Risk Modulation. Journal of Personalized Medicine, 10(1), 19. https://doi.org/10.3390/jpm10010019