Abstract
The aim was to identify conservative treatments available for acute ankle sprain and to evaluate their effectiveness with respect to pain relief and short-term recovery of functional capacity. A systematic review of the relevant literature was conducted via a data search of the PROSPERO, PubMed, Scopus, CINAHL, PyscINFO and SPORTDiscus databases, from inception until December 2019, focusing on randomised control trial studies. Two of the authors independently assessed the quality of each study located and extracted the relevant data. The quality of each paper was assessed using the Cochrane risk of bias tool included in RevMan 5. In all, 20 studies met the inclusion criteria. In terms of absence of bias, only nine papers were classed as “high quality”. Studies (75%) were of low quality in terms of the blinding of participants and personnel and uncertainty in blinding of outcome assessment and all presented one or more other forms of bias. Despite the generally low quality of the studies considered, it can be concluded that conservative treatment for acute ankle sprain normally achieves pain relief and rapidly improved functionality. Research based on higher-quality study designs and procedures would enable more definitive conclusions to be drawn.
1. Introduction
Ankle sprain is the most prevalent musculoskeletal injury affecting the lower limb in physically active individuals [1]. It consists of the stretching or partial or complete tearing of one or more ligaments in the ankle joint caused by an involuntary twisting movement that exceeds the normal limits of the joint [2].
The most common mechanism of injury in ankle sprain is the combination of inversion and adduction of the foot in conjunction with plantarflexion (supination), which most usually provokes a deterioration of the external lateral ligament and also often impacts on the anterior peroneal tendons [3]. In exceptional circumstances, the anterior ligament may be torn, with associated capsular damage, and rupture of the peroneal tendons. The deltoid ligament may be damaged by traumatic eversion; although this type of sprain occurs only rarely, the possibility of associated injuries such as distal or proximal fracture of the fibula and even of the talus should be considered [4]. Furthermore, hyperdorsiflexion could damage the syndesmotic ligaments [5]. In addition to ligaments, other anatomic structures such as bone, muscles, tendons, nerves and vascular vessels may be affected [2].
The clinical manifestations of ankle sprain include the inability to walk or even move the joint, a searing or tearing sensation, pain that increases with mobility, colour change and rapid bruising. The intensity of these manifestations depends on the severity of the sprain [6]. Treatments to heal the structures and recover functionality after a sprain may be conservative or surgical. Conservative treatment is usually applied for Grade I and II sprains, and Grade III lesions are treated surgically, although for the latter a conservative approach is sometimes considered sufficient [7].
A wide range of conservative treatments are available, including short-term immobilisation [8], complete immobilisation, ice packs [9], local or systemic non-steroidal anti-inflammatory drugs (NSAIDs) [10], physical therapy [11] and electrical stimulation (with or without muscle contraction) [12]. All have been investigated for efficacy in the resolution or improvement of clinical manifestations of ankle sprain, in areas such as the persistence swelling [13] or the patient’s ability to return to work [14] or to playing sport [15]. However, these reviews have considered situations not only of acute sprain [16,17], but also of chronic ankle instability [18] or a combination of conservative and surgical treatments [19,20]. To our knowledge, none have focused specifically on acute ankle sprain.
In view of these considerations, our study aims to identify conservative treatments for acute ankle sprain and to evaluate their effectiveness in terms of pain relief and rapid recovery of functional capacity.
2. Methods
The review protocol was registered at the International Prospective Register of Systematic Reviews (PROSPERO: CRD 42020162500).
2.1. Design
This review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [21].
2.2. Search Strategy
One member of the research team (ABOA) carried out the search to ensure that no previous studies had been conducted with the same study aim as our own. The following databases were searched: PROSPERO, PubMed, Scopus, CINAHL, PyscINFO and SPORTDiscuss, from inception until December 2019 using optimised search strategies (Appendix A). References were exported and duplicate articles removed using reference management software (Mendeley Desktop v 1.19.4).
2.3. Eligibility Criteria
The following eligibility criteria were applied:
- -
- In every case, the study population was diagnosed with acute ankle sprain and given conservative treatment as the first option.
- -
- All studies included in the review were randomised controlled clinical trials (RCTs) in which one or more types of conservative treatment were applied in response to an acute ankle sprain, with a maximum of 7 days after initial injury.
- -
- All the studies included evaluated pain, functionality and/or disability caused by an ankle sprain, using one or more measurement instruments.
- -
- The language of publication was Spanish or English.
Studies of the following types were excluded:
- -
- The study population was diagnosed with chronic or recurrent ankle sprain.
- -
- Those in which both conservative and surgical treatments were applied.
- -
- Those not consisting of an RCT (such as pilot studies, research protocols or quasi-experimental studies).
- -
- Those in which the assessment of risk of bias, using the Cochrane risk of bias tool included in RevMan 5 was high risk (it was not consider random sequence generation, allocation concealment and blinding of participants and personnel).
2.4. Study Selection
In the first stage of the review, a double-blinded assessment of titles and abstracts was carried out by two reviewers (P.C-G and A.M-R), working independently, to determine whether each item met the requirements for inclusion. In case of doubt, the full text of the article was evaluated. Disagreements between the two reviewers were resolved by discussion, or if consensus was not possible, a further opinion was sought. It was also planned, if necessary, to send an email to the original authors to obtain further information regarding the study details, but in no case was this measure necessary.
2.5. Data Extraction
The following data were extracted from each study, using a standardised template: study details (author; year and country of publication), study participant characteristics (number of patients included in the sample, mean age, sex), characteristics of the sprain, study design, type of conservative treatment administered (intervention group and patients included), follow-up period and measurement instrument used.
No meta-analysis was carried out, due to the heterogeneity of the populations, follow-up characteristics and outcomes included in these studies.
2.6. Quality Assessment
Two reviewers (P.C-G and A.M-R), working independently, assessed the risk of bias in the studies considered, using the Cochrane risk of bias tool included in RevMan 5 for this purpose [22]. The following biases were assessed: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, attrition bias, selective reporting and other bias. Each criterion outcome was classed as high risk, low risk or unclear.
3. Results
An initial 10,556 studies were identified, but 9860 were duplicated among the different databases. The remaining 696 were screened against our inclusion/exclusion criteria, using the titles, abstracts and keywords, resulting in 31 studies that met the inclusion criteria. After quality appraisal (Risk of assessment bias), a further 11 were excluded, and so 20 studies remained in the final qualitative analysis. Figure 1 shows the PRISMA flow diagram for the studies included in the review [23].
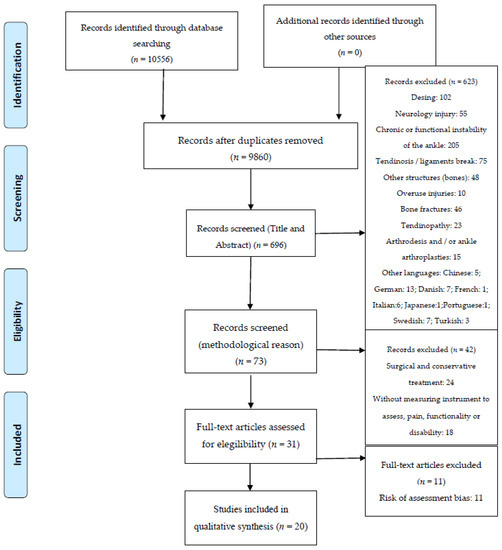
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Flow Diagram.
3.1. Study Characteristics
The studies included a total of 2236 patients with a mean age of 28.86 years. Of these patients, 40.3% were female and 59.7% were male.
The conservative treatment applied was mainly for acute ankle sprains, Grades I, II or III. In many cases, the location of the sprain (right or left ankle) was not specified. The time elapsed from the start of the injury to the start of conservative treatment was recorded. This time was usually less than 48 h except in two studies which described a period of less than 5 days. The minimum follow-up period recorded was four weeks, with an average of 8.5 weeks (162 days).
The most common treatment described was based on manual or physiotherapeutic methods (eight studies), followed by the use of different types of bandage (three studies) (Table 1). The studies using one or more of the following measurement instruments: Visual Analogue Scale, McGill Pain Questionnaire, Numerical Pain Rating Scale, Total Function Score, Lower Extremity Functional Scale, EuroQol-5D (EQ-5D), American Orthopedics Foot and Ankle Score, Lower Limb Task Questionnaire, Motor Activity Scale, Karlsson Score, Adapted Hughston Clinic Subjective Rating Scale for Ankle disorders, Short Form-12 (SF-12) Foot and Ankle Outcome Score, Foot and Ankle Ability Measure. The most used instrument for evaluating the pain of the ankle sprain is the VAS, used in 13 of the found studies. On another hand, the instruments used more for the evaluation of the function are the SF-12, as a general instrument, and the LEFS as a specific instrument, and both are used in 3 different studies.

Table 1.
Characteristics of the studies included in the review.
The measurement instruments used to assess improvement in terms of pain relief and the recovery of functional capacity in patients with an acute ankle sprain after the application of conservative treatment showed that in most cases significant improvement was achieved (p < 0.001) (Table 2). In all the studies is seen an improvement of the pain and the function in the patients. It is seen that this improvement, most of all of the function, is higher in the studies that made the treatments in a bigger period of time.

Table 2.
Reported outcomes for pain relief and recovery of functional capacity.
3.2. Risk of Bias
The risk of bias was evaluated in 20 studies (Figure 2 and Figure 3). Only nine studies presented a low risk of bias. Most studies (75%) were of low quality in terms of the blinding of participants and personnel and uncertainty in blinding of outcome assessment and all presented one or more other forms of bias. The blindness in the evaluation of the results was the bias less specified in the studies, not making it clear if the blindness of the evaluator was made or not.
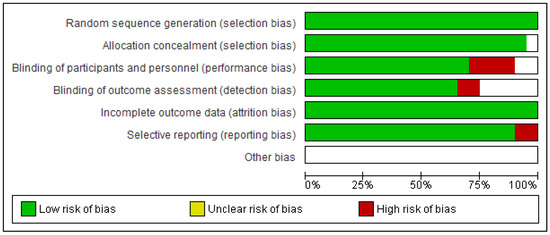
Figure 2.
Risk of bias graph.
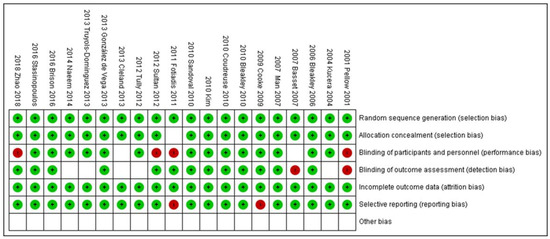
Figure 3.
Risk of bias summary.
4. Discussion
This review has two main aims: to identify conservative treatments for acute ankle sprain level, Grades I, II and III, and to evaluate the effectiveness of these treatments in terms of pain relief and rapid recovery of functional capacity.
Concerning the first of these aims, our analysis was focused on RCTs investigating different types of short-term conservative treatment for patients with an acute ankle sprain. These treatment options included programmes of physical therapy (at home [11] or supervised by a physical therapist [28]), the prescription of NSAIDs such as diclofenac or traumeel [10], the use of a functional brace (for example, a tubular bandage or aircast brace) [2] or neuromuscular electrical stimulation [32]. On many occasions, these treatments are provided in conjunction with cryotherapy (ice packs) [27] and usual care (consisting of ankle protection, rest, the application of a compression bandage, elevation, analgesics as necessary and a gradual return to weight bearing activities) [9]. In all cases, notable pain relief is obtained and functional capacity regained, during the follow-up period considered, i.e., ranging from seven days to nine months (p < 0.001).
Among the studies that focused on identifying treatment effectiveness in terms of pain relief, special attention is paid to the use of cryotherapy, which reduces the sensation of pain when the ice pack is applied intermittently [27], although when it is combined with an exercise intervention programme initiated at an early stage, i.e., after the first week following the occurrence of the sprain, significantly improved results are obtained (p < 0.05) after a 16-week follow-up period [28]. In studies that have analysed the recovery of function following the application of conservative treatment, usual care [9], therapeutic physical intervention at home or supervised by a physical therapist [11,28] or the application of bandages are the methods most commonly employed [2]. The results published show there are no significant differences between the different intervention groups in terms of the improvement obtained, after a maximum follow-up period of nine months.
Regarding the presence of bias in the studies considered, our results show that these RCTs are generally of low quality, with only nine studies characterised as high quality (i.e., presenting a low risk of bias) [9,10,27,28,30,32,33,35,36]. The common weaknesses of the RCTs are “Blinding of participants and personnel” and “Uncertainty in blinding of outcome assessment and other bias”. We emphasise the importance of these deficiencies, as the research findings are inherently less reliable if the participants or the researchers are aware of the intervention that has been assigned. In consequence, the results obtained in terms of pain relief and recovery of functionality must be considered invalid and therefore not transferrable, having been altered by the presence of subjectivity and by the patient’s degree of adherence to treatment. Other types of bias may also be present if the procedure applied is not clearly described.
Recent findings indicate that different types of conservative treatment for patients with acute ankle sprain Grades I, II or III produce significant beneficial effects regarding pain relief and the recovery of functionality. However, very few studies of high methodological quality have focused on this study objective. In addition, a wide variety of treatments, measurement tools and follow-up periods have been reported. Our review findings are in line with those of Kosik et al., 2017 [40], Van Ochten et al., 2014 [41] and Kamper et al., 2012 [7]. These reviews, however, examine not only conservative treatment but also surgical methods and their application to patients with chronic ankle instability. Similarly, while Al bimani et al., 2019 [15] assessed the effectiveness of conservative treatments in enabling the patient to return to playing sports, the review takes into account all types of research design. Another of the reviews considered, by Feger et al., 2015 [42], assessed only electrical stimulation or functional treatment [13]. Moreover, the follow-up period considered is only ten weeks. Overall, nevertheless, these reviews highlight the general improvement achieved by patients from the treatments described, although they emphasise the need for further research with appropriate study methods, a common measurement instrument and sufficiently long-term follow-up.
The present systematic review presents numerous strengths. To our knowledge, it is the first to examine only conservative treatments for patients with acute ankle sprains, Grades I, II or III, and in which all studies included are RCTs (performed up to December 2019). Moreover, we applied specific instruments to analyse the risk of bias, and employed a rigorous methodological process, based on a literature search of six medical databases with no time limitation. On the other hand, certain limitations must be acknowledged. The first is the small number of studies extracted that focus on our study objective. In addition, the non-specificity of the location of the sprain (left or right ankle) is unfortunate, as this information could usefully be taken into account to determine whether there is a direct relationship with the laterality of the patient. Another factor is the heterogeneity of the data presented (several measurement instruments were used), which made it impossible to carry out a meta-analysis and, therefore, prevented us from conducting a joint assessment. Only two languages of publication (Spanish or English) were inclusion criteria, which increases the loss of some randomised control trial studies. Finally, there was a relatively high risk of common bias across the studies reviewed.
The most relevant clinical implications are conservative treatments for acute ankle sprain relieve pain and functional capacity, but the results showed there are no significant differences between the different conservative interventions in terms of the improvement obtained, after a maximum follow-up period of nine months. Clinicians should establish a protocol in terms of prevention and thus avoid recurrences or chronic ankle instability.
5. Conclusions
Despite the generally low quality of the studies considered, it can be concluded that conservative treatments for acute ankle sprain relieve pain and achieve a rapid return to functionality. However, there is no evidence that any one form of conservative treatment is more effective than any other in terms of these parameters, for patients with acute ankle sprain Grades I, II or III, since a wide range of treatments have been studied for this pathology, using diverse measurement instruments. Future research in this field should ensure homogeneity in the size and composition of the study groups, in the follow-up period and in the description of the main outcomes considered, thus limiting the risk of bias. Research based on higher-quality study designs and procedures would enable more definitive conclusions to be drawn.
Author Contributions
Conceptualization, A.B.O.-A.; methodology, G.G.-N. and A.B.O.-A.; formal analysis, P.C.-G., A.M.-R. and E.C.-L.; writing—original draft preparation, C.S., C.J.N.; writing—review and editing, A.B.O.-A., P.C.-G., A.M.-R.; visualization, G.G.-N.; supervision, A.B.O.-A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Searching Strategy.

Table A1.
PubMed. Total articles: 656.
Table A1.
PubMed. Total articles: 656.
| 1 | Ankle |
| 2 | Talocrural |
| 3 | Talo-crural |
| 4 | Talocalcaneal |
| 5 | Talo-calcaneal |
| 6 | Talofibular |
| 7 | Talo-fibular |
| 8 | Ligament |
| 9 | Lateral Ligament ankle |
| 10 | Medial Ligament ankle |
| 11 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 |
| 12 | Sprain |
| 13 | Strain |
| 14 | Ankle injury |
| 15 | Ankle sprain |
| 16 | Inversion sprain |
| 17 | Eversion sprain |
| 18 | 12 OR 13 OR 14 OR 15 OR 16 OR 17 |
| 19 | 11 AND 18 |
| 20 | Conservative treatment |
| 21 | Conservative management |
| 22 | Non-surgical treatment |
| 23 | CAST |
| 24 | Rehabilitation program |
| 25 | Myofascial |
| 26 | Conservative program |
| 27 | Manual Therapy |
| 28 | Physiotherapeutic intervention |
| 29 | Bandage |
| 30 | Plaster |
| 31 | Exercise programme |
| 32 | Home exercise |
| 33 | RICE |
| 34 | Taping |
| 35 | TENSE |
| 36 | Ultrasound |
| 37 | 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 |
| 38 | 19 AND 37 |

Table A2.
CINAHL. Total articles: 2176.
Table A2.
CINAHL. Total articles: 2176.
| 1 | Ankle Sprains |
| 2 | Inversion Sprain |
| 3 | Eversion Sprain |
| 4 | Ankle Injury |
| 5 | 1 OR 2 OR 3 OR 4 |
| 6 | Conservative treatment |
| 7 | Conservative management |
| 8 | Rehabilitation programs |
| 9 | Bandage |
| 10 | Physiotherapeutic |
| 11 | 6 OR 7 OR 8 OR 9 OR 10 |
| 12 | 5 AND 11 |

Table A3.
SCOPUS. Total articles: 597.
Table A3.
SCOPUS. Total articles: 597.
| 1 | TITLE-ABS-KEY (Ankle Sprain) |
| 2 | TITLE-ABS-KEY (Inversion Sprain) |
| 3 | TITLE-ABS-KEY (Eversion Sprain) |
| 4 | TITLE-ABS-KEY (Ankle Injury) |
| 5 | 1 OR 2 OR 3 OR 4 |
| 6 | TITLE-ABS-KEY (Conservative treatment) |
| 7 | TITLE-ABS-KEY (Conservative management) |
| 8 | TITLE-ABS-KEY (TENSE) |
| 9 | TITLE-ABS-KEY (Bandage) |
| 10 | TITLE-ABS-KEY (Rehabilitation program) |
| 11 | TITLE-ABS-KEY (Physiotherapeutic) |
| 12 | 6 OR 7 OR 8 OR 9 OR 10 OR 11 |
| 13 | 5 AND 12 |

Table A4.
SPORTSDiscus via EBSCOHost. Total articles: 5618.
Table A4.
SPORTSDiscus via EBSCOHost. Total articles: 5618.
| 1 | Ankle Sprains |
| 2 | Inversion Sprain |
| 3 | Eversion Sprain |
| 4 | Ankle injury |
| 5 | 1 OR 2 OR 3 OR 4 |
| 6 | Conservative treatment |
| 7 | Conservative management |
| 8 | Rehabilitation program |
| 9 | Physiotherapeutic |
| 10 | 6 OR 7 OR 8 OR 9 OR 10 |
| 11 | 5 AND 10 |

Table A5.
PsycINFO. Total articles: 1371.
Table A5.
PsycINFO. Total articles: 1371.
| 1 | Ankle Sprains |
| 2 | Inversion Ankle sprain |
| 3 | Eversion Ankle sprain |
| 4 | 1 OR 2 OR 3 |
| 5 | Conservative treatment |
| 6 | Conservative management |
| 7 | Rehabilitation program |
| 8 | Physiotherapeutic |
| 9 | 5 OR 6 OR 7 OR 8 |
| 10 | 4 AND 9 |

Table A6.
PROSPERO. Total articles: 38.
Table A6.
PROSPERO. Total articles: 38.
| 1 | Ankle Sprains |
References
- Vuurberg, G.; Hoorntje, A.; Wink, L.M.; Van Der Doelen, B.F.W.; Van Den Bekerom, M.P.; Dekker, R.; Van Dijk, C.N.; Krips, R.; Loogman, M.C.M.; Ridderikhof, M.L.; et al. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br. J. Sports Med. 2018, 52, 956. [Google Scholar] [CrossRef]
- Cooke, M.W.; Marsh, J.L.; Clark, M.; Nakash, R.; Jarvis, R.M.; Hutton, J.L.; Szczepura, A.; Wilson, S.; Lamb, S.E. Treatment of severe ankle sprain: A pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial. Health Technol. Assess. 2009, 13. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar] [PubMed]
- Herzog, M.M.; Kerr, Z.Y.; Marshall, S.W.; Wikstrom, E.A. Epidemiology of ankle sprains and chronic ankle instability. J. Athl. Train. 2019, 54, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Purevsuren, T.; Kim, K.; Batbaatar, M.; Lee, S.K.; Kim, Y.H. Influence of ankle joint plantarflexion and dorsiflexion on lateral ankle sprain: A computational study. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2018, 232, 458–467. [Google Scholar] [CrossRef]
- van Rijn, R.M.; van Os, A.G.; Bernsen, R.M.D.; Luijsterburg, P.A.; Koes, B.W.; Bierma-Zeinstra, S.M.A. What Is the Clinical Course of Acute Ankle Sprains? A Systematic Literature Review. Am. J. Med. 2008, 121, 324–331. [Google Scholar] [CrossRef]
- Kamper, S.J.; Grootjans, S.J.M. Surgical versus conservative treatment for acute ankle sprains. Br. J. Sports Med. 2012, 46, 77–78. [Google Scholar] [CrossRef]
- Lamb, S.E.; Nakash, R.A.; Withers, E.J.; Clark, M.; Marsh, J.L.; Wilson, S.; Hutton, J.L.; Szczepura, A.; Dale, J.R.; Cooke, M.W. Clinical and cost effectiveness of mechanical support for severe ankle sprains: Design of a randomised controlled trial in the emergency department [ISRCTN 37807450]. BMC Musculoskelet. Disord. 2005, 26, 2221–2228. [Google Scholar] [CrossRef]
- Brison, R.J.; Day, A.G.; Pelland, L.; Pickett, W.; Johnson, A.P.; Aiken, A.; Pichora, D.R.; Brouwer, B. Effect of early supervised physiotherapy on recovery from acute ankle sprain: Randomised controlled trial. BMJ 2016, 355, i5650. [Google Scholar] [CrossRef]
- González De Vega, C.; Speed, C.; Wolfarth, B.; González, J. Traumeel vs. diclofenac for reducing pain and improving ankle mobility after acute ankle sprain: A multicentre, randomised, blinded, controlled and non-inferiority trial. Int. J. Clin. Pract. 2013, 67, 979–989. [Google Scholar] [CrossRef]
- Bassett, S.F.; Prapavessis, H. Home-Based Physical Therapy Intervention With Adherence-Enhancing Strategies Versus Clinic-Based Management for Patients With Ankle Sprains. Phys. Ther. 2007, 87, 1132–1143. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, T.W.; Burgess, L.C.; Middleton, R.G. Does Neuromuscular Electrical Stimulation Improve Recovery Following Acute Ankle Sprain? A Pilot Randomised Controlled Trial. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Kemler, E.; Van De Port, I.; Backx, F.; Van Dijk, C.N. A systematic review on the treatment of acute ankle sprain: Brace versus other functional treatment types. Sports Med. 2011, 41, 185–197. [Google Scholar] [CrossRef]
- Kerkhoffs, G.M.M.J.; Rowe, B.H.; Assendelft, W.J.J.; Kelly, K.D.; Struijs, P.A.A.; Van Dijk, C.N. Immobilisation for acute ankle sprain. A systematic review. Arch. Orthop. Trauma Surg. 2001, 121, 462–471. [Google Scholar] [CrossRef]
- Al Bimani, S.A.; Gates, L.S.; Warner, M.; Bowen, C. Factors influencing return to play following conservatively treated ankle sprain: A systematic review. Phys. Sportsmed. 2019, 47, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Ivins, D. Acute Ankle Sprain: An Update. Am. Fam. Physician 2006, 74, 1714–1720. [Google Scholar]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Delahunt, E.; Holden, S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br. J. Sports Med. 2017, 51, 113–125. [Google Scholar] [CrossRef]
- Petersen, W.; Rembitzki, I.V.; Koppenburg, A.G.; Ellermann, A.; Liebau, C.; Brüggemann, G.P.; Best, R. Treatment of acute ankle ligament injuries: A systematic review. Arch. Orthop. Trauma Surg. 2013, 133, 1129–1141. [Google Scholar] [CrossRef]
- Han, L.; Zhang, C.; Liu, B.; Ting, H.; Jihong, W. A Meta-analysis of treatment methods for acute ankle sprain. Pak. J. Med. Sci. 2012, 28, 895–899. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Santesso, N.; Helfand, M.; Vist, G.E.; Kunz, R.; Brozek, J.; Norris, S.; Meerpohl, J.J.; Djulbegovic, B.; et al. The Cochrane Collaboration. Review Manager (RevMan). Pain 2009, 9, 205–213. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. PRISMA 2009 Flow Diagram. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Pellow, J.E.; Brantingham, J.W. The efficacy of adjusting the ankle in the treatment of subacute and chronic grade I and grade II ankle inversion sprains. J. Manip. Physiol. Ther. 2001, 24, 17–24. [Google Scholar] [CrossRef]
- Kučera, M.; Barna, M.; Horáček, O.; Kováriková, J.; Kučera, A. Efficacy and safety of topically applied Symphytum herb extract cream in the treatment of ankle distortion: Results of a randomized controlled clinical double blind study. Wien. Med. Wochenschr. 2004, 154, 498–507. [Google Scholar] [CrossRef]
- Truyols-Domínguez, S.; Salom-Moreno, J.; Abian-Vicen, J.; Cleland, J.A.; Fernández-De-Las-Peñas, C. Efficacy of thrust and nonthrust manipulation and exercise with or without the addition of myofascial therapy for the management of acute inversion ankle sprain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2013, 43, 300–309. [Google Scholar] [CrossRef]
- Bleakley, C.M.; McDonough, S.M.; MacAuley, D.C. Cryotherapy for acute ankle sprains: A randomised controlled study of two different icing protocols. Br. J. Sports Med. 2006, 40, 700–705. [Google Scholar] [CrossRef]
- Bleakley, C.M.; O’Connor, S.R.; Tully, M.A.; Rocke, L.G.; MacAuley, D.C.; Bradbury, I.; Keegan, S.; McDonough, S.M. Effect of accelerated rehabilitation on function after ankle sprain: Randomised controlled trial. BMJ 2010, 340, 1122. [Google Scholar] [CrossRef]
- Cleland, J.A.; Mintken, P.; McDevitt, A.; Bieniek, M.; Carpenter, K.; Kulp, K.; Whitman, J.M. Manual physical therapy and exercise versus supervised home exercise in the management of patients with inversion ankle sprain: A multicenter randomized clinical trial. J. Orthop. Sports Phys. Ther. 2013, 43, 443–455. [Google Scholar] [CrossRef]
- Coudreuse, J.M.; De Vathaire, F. Effect of a plaster containing DHEP and heparin in acute ankle sprains with oedema: A randomized, double-blind, placebo-controlled, clinical study. Curr. Med. Res. Opin. 2010, 26, 2221–2228. [Google Scholar] [CrossRef]
- Fotiadis, E.; Kenanidis, E.; Samoladas, E.; Chytas, A.; Lyrtzis, C.; Koimtzis, M.; Chalidis, B. Are venotonic drugs effective for decreasing acute posttraumatic oedema following ankle sprain? A prospective randomized clinical trial. Arch. Orthop. Trauma Surg. 2011, 131, 389–392. [Google Scholar] [CrossRef] [PubMed]
- Cheung, S.M.; Chen, C.J.; Hsin, Y.J.; Tsai, Y.T.; Leong, C.P. Effect of neuromuscular electrical stimulation in a patient with Sjogren’s syndrome with dysphagia: A real time videofluoroscopic swallowing study. Chang Gung Med. J. 2010, 33, 338–345. [Google Scholar] [PubMed]
- Kim, M.K.; Shin, Y.J. Immediate effects of ankle balance taping with kinesiology tape for amateur soccer players with lateral ankle sprain: A randomized cross-over design. Med. Sci. Monit. 2017, 23, 5534–5541. [Google Scholar] [CrossRef] [PubMed]
- Naeem, M.; Rahimnajjad, M.K.; Rahimnajjad, N.A.; Idrees, Z.; Shah, G.A.; Abbas, G. Assessment of functional treatment versus plaster of Paris in the treatment of grade 1 and 2 lateral ankle sprains. J. Orthop. Traumatol. 2015, 16, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Sandoval, M.C.; Ramirez, C.; Camargo, D.M.; Salvini, T.F. Effect of high-voltage pulsed current plus conventional treatment on acute ankle sprain. Rev. Bras. Fisioter. 2010, 14, 193–199. [Google Scholar] [CrossRef]
- Stasinopoulos, D.; Papadopoulos, C.; Lamnisos, D.; Stasinopoulos, I. The use of Bioptron light (polarized, polychromatic, non-coherent) therapy for the treatment of acute ankle sprains. Disabil. Rehabil. 2017, 39, 450–457. [Google Scholar] [CrossRef]
- Sultan, M.J.; McKeown, A.; McLaughlin, I.; Kurdy, N.; McCollum, C.N. Elastic stockings or Tubigrip for ankle sprain: A randomised clinical trial. Injury 2012, 43, 1079–1083. [Google Scholar] [CrossRef]
- Tully, M.A.; Bleakley, C.M.; O’Connor, S.R.; McDonough, S.M. Functional management of ankle sprains: What volume and intensity of walking is undertaken in the first week postinjury. Br. J. Sports Med. 2012, 46, 877–882. [Google Scholar] [CrossRef]
- Zhao, M.; Gao, W.; Zhang, L.; Huang, W.; Zheng, S.; Wang, G.; Hong, B.Y.; Tang, B. Acupressure Therapy for Acute Ankle Sprains: A Randomized Clinical Trial. PM&R 2018, 10, 36–44. [Google Scholar] [CrossRef]
- Kosik, K.B.; McCann, R.S.; Terada, M.; Gribble, P.A. Therapeutic interventions for improving self-reported function in patients with chronic ankle instability: A systematic review. Br. J. Sports Med. 2017, 51, 105–112. [Google Scholar] [CrossRef]
- Van Ochten, J.M.; Van Middelkoop, M.; Meuffels, D.; Bierma-Zeinstra, S.M.A. Chronic complaints after ankle sprains: A systematic review on effectiveness of treatments. J. Orthop. Sports Phys. Ther. 2014, 44, 862–871. [Google Scholar] [CrossRef] [PubMed]
- Feger, M.A.; Goetschius, J.; Love, H.; Saliba, S.A.; Hertel, J. Electrical stimulation as a treatment intervention to improve function, edema or pain following acute lateral ankle sprains: A systematic review. Phys. Ther. Sport 2015, 16, 361–369. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).