Dynamics of the Microbiota and Its Relationship with Post-COVID-19 Syndrome
Abstract
:1. Introduction
2. Definition of Prevalence and Symptoms of Long COVID-19
3. General Concepts of the Gut Microbiome and Its Association with the Lungs and Gastrointestinal Tract
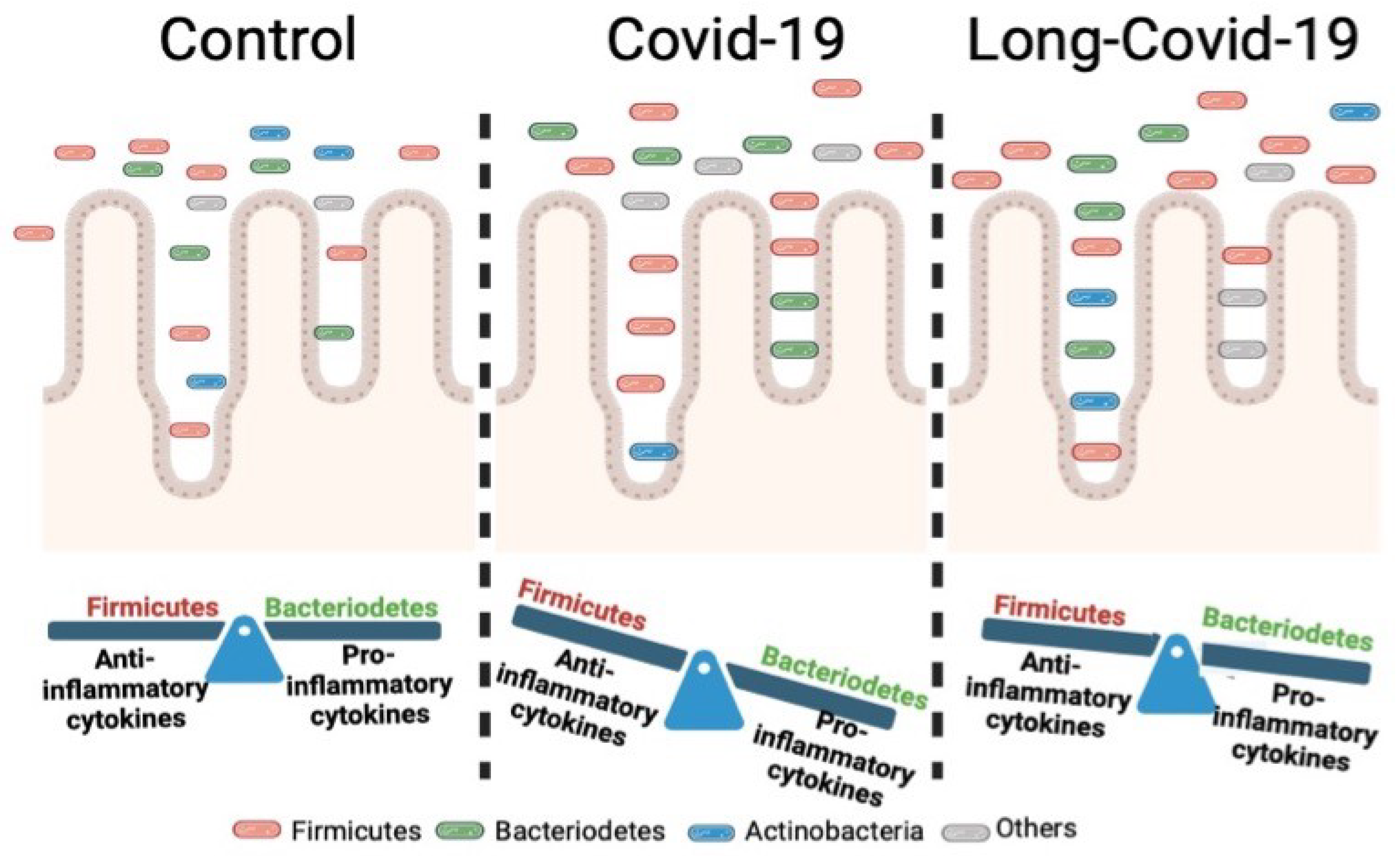
4. Gut Microbiome Association with Clinical Manifestations in Viral Infections
5. Gut Microbiota and Its Dynamics in Typical COVID-19
6. Gut Microbiota and Long COVID-19—Friend or Foe?
| Population | Study Groups | Age | Main Findings | Reference |
|---|---|---|---|---|
| China (Hong Kong) | PACS COVID-19 diagnostic patients (n = 106) non-COVID-19 controls patients (n = 68) | 48.3 (33–62) | Patients without PACS showed recovered gut microbiome profile at 6 months comparable to that of non-COVID-19 controls. Gut microbiome of patients with PACS were characterized by higher levels of Ruminococcus gnavus and Bacteroides vulgatus and lower levels of Faecalibacterium prausnitzii. Persistent respiratory symptoms were correlated with opportunistic gut pathogens, and neuropsychiatric symptoms and fatigue were correlated with nosocomial gut pathogens, including Clostridium innocuum and Actinomyces naeslundii. Butyrate-producing bacteria, including Bifidobacterium pseudocatenulatum and F. prausnitzii, showed the largest inverse correlations with PACS at 6 months. | [57] |
| Italy (Roma) | Post SARS-CoV-2 positive (n = 31) SARS-CoV-2 negative (n = 18). | 66.7 ± 14.4 67.1 ± 17.5 | Bacteroidetes’ relative abundance was higher (≈36.8%) in patients with SARS-CoV-2 and declined to 18.7% when SARS-CoV-2 infection resolved (Six months). Firmicutes were prevalent (≈75%) in controls and in samples collected after SARS-CoV-2 infection resolution. Ruminococcaceae, Lachnospiraceae and Blautia increased after SARS-CoV-2 infection resolution six months after. Lachnospiraceae (Fusicantibacter and Roseburia) and Ruminococcaceae were increased after SARS-CoV-2 infection resolution. | [85] |
| Norway Oslo | Patients with 3 months after hospitalization COVID-19 (PACS) (n = 83) | 59 (50–71) | Three months after hospitalization for COVID-19, patients with respiratory dysfunction showed a lower microbiota diversity and an altered global gut microbiota composition than patients with normal respiratory function. These microbiota alterations included reduced abundance of Erysipelotrichaceae UCG-003 and increased abundance of Veillonella and Flavonifractor. | [61] |
| China (Hong Kong) | Post-acute COVID-19 syndrome (n = 302) Healthy controls (n = 893) | 54.9 | Klebsiella pneumoniae, an opportunistic pathogen, was positively associated with PACS patients. Roseburia intestinalis, a probiotic, was negatively correlated with PACS patients. Subjects with PACS showed a significant increase in abundance of Bacteroides vulgatus and Bacteroides xylanisolvens, compared with healthy controls. | [86] |
| China (Hong Kong) | Patients non-COVID-19 (n = 66) Patients COVID-19 (n = 66) With PACS (n = 48) Without PACS (n = 18) | 47.9 (28–64) 49.2 (33–63) | Post-acute COVID-19-syndrome patients exhibited increased prevalence of Klebsiella sp. | [86] |
| United State of America (New Jersey) | Post-acute COVID-19 syndrome, single patient. | Not specified | ASV002A_Bacteroides was positively correlated with all PACS COVID-19 symptoms and positively correlated with the severity of anxiety. The ASV0AKS_Oscillibacter, ASV009F_Anaerofustis, ASV02YT_Blautia, ASV07LA_Blautia, and ASV0AM6_Eubacterium hallii amplicon sequence variants were potential SCFA-producing bacteria, which were associated with the alleviation of PACS COVID-19 symptoms. | [87] |
| Russia (Moscow) | post-COVID-19 syndrome patients (n = 30) | 62 (53–67) | Excessive bacterial growth (92%) of proinflammatory microorganisms (Bacteroides fragilis group, Candida spp., S. aureus, Proteus spp., Enterococcus spp., Enterobacter spp., and Citrobacter spp.) exceeded the reference values by 1.5–2 times, and low levels of Bacteroides thetaiotimicron and Akkermansia muciniphila compared with the reference values. High ratio of Bacteoides fragilis group/Faecalibacterium prausnitzii associated with inflammatory diseases in post-COVID-19 patients. | [88] |
| China (Hong Kong) | Overall: COVID-19 patients n = 133 Cluster 1: severe and post-acute COVID-19 (n = 63) Cluster 2 non-severe COVID-19 (n = 70) | 42.2 (26–59) | The multi-biome composition of patients in Cluster 1 was characterized by a predominance of bacteria Ruminococcus gnavus, Klebsiella quasipneumoniae, Klebsiella pneumoniae, Klebsiella variicola, Erysipelatoclostridium ramosum, Clostridium bolteae, and Clostridium innocuum, and lower relative abundance of Bifidobacterium adolescentis and Faecalibacterium prausnitzii. | [89] |
| China (Shanghai) | Post severe/critical COVID-19 infection patients (n = 14) Post mild/moderate COVID-19 infection patients (n = 31) Healthy controls (n = 31) | 60.5 (49.5–70.5) 51.0 (42.7–56.2) | The diversity of the gut microbiome was reduced in severe/critical COVID-19 cases compared to mild/moderate cases. The abundance of some gut microbes altered post-SARS-CoV-2 infection and related to disease severity, such as Enterococcus faecium, Coprococcus comes, Roseburia intestinalis, Akkermansia muciniphila, Bacteroides cellulosilyticus, and Blautia obeum. | [90] |
| China (Wuhan) | Asymptomatic group (n = 103) long COVID-19 symptomatic patients (n = 84) | 59 (48–66) 57 (45–67) | Symptomatic recovered patients (long COVID) had gut microbiota dysbiosis, including significantly reduced bacterial diversities and lower relative abundance of SCFAs-producing salutary symbionts, such as Eubacterium hallii group, Subdoligranulum, Ruminococcus, Dorea, Coprococcus, and Eubacterium ventriosum group, compared with healthy controls. The relative abundance of Eubacterium hallii group, Subdoligranulum, and Ruminococcus showed decreasing tendencies in healthy controls, the asymptomatic group, and the symptomatic long COVID group. | [91] |
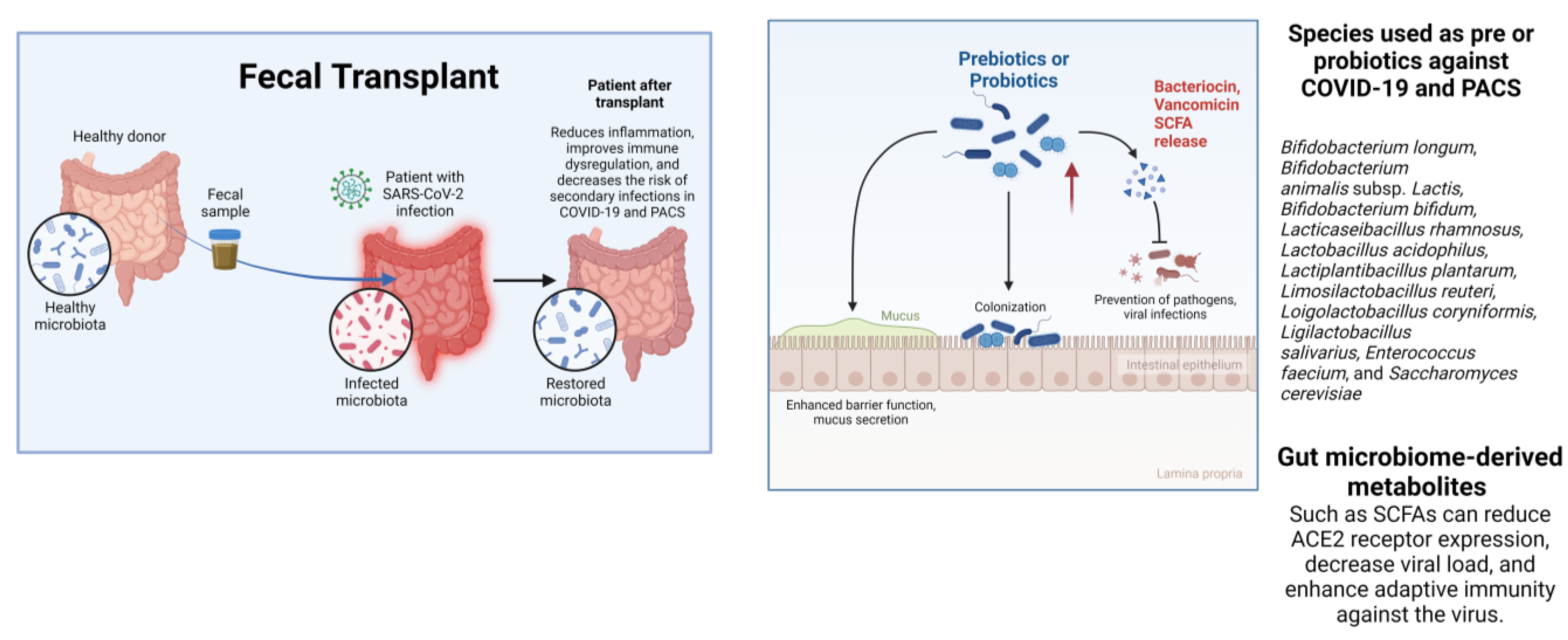
7. Applications and Prospects of Gut Microbiota for the Diagnosis and Treatment of COVID-19 and PACS
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Da Rosa Mesquita, R.; Francelino Silva Junior, L.C.; Santos Santana, F.M.; Farias De Oliveira, T.; Campos Alcântara, R.; Monteiro Arnozo, G.; Rodrigues Da Silva Filho, E.; Galdino Dos Santos, A.G.; Oliveira Da Cunha, E.J.; Salgueiro De Aquino, S.H.; et al. Clinical Manifestations of COVID-19 in the General Population: Systematic Review. Wien. Klin. Wochenschr. 2021, 133, 377–382. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines; National Institutes of Health: Bethesda, MD, USA, 2023.
- Wang, B.; Zhang, L.; Wang, Y.; Dai, T.; Qin, Z.; Zhou, F.; Zhang, L. Alterations in Microbiota of Patients with COVID-19: Potential Mechanisms and Therapeutic Interventions. Signal Transduct. Target. Ther. 2022, 7, 143. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-Acute COVID-19 Syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Pavli, A.; Tsakris, A. Post-COVID Syndrome: An Insight on Its Pathogenesis. Vaccines 2021, 9, 497. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Mak, J.W.Y.; Su, Q.; Yeoh, Y.K.; Lui, G.C.-Y.; Ng, S.S.S.; Zhang, F.; Li, A.Y.L.; Lu, W.; Hui, D.S.-C.; et al. Gut Microbiota Dynamics in a Prospective Cohort of Patients with Post-Acute COVID-19 Syndrome. Gut 2022, 71, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, S.; Mohanty, S.; Sharma, S.; Tripathi, P. Possible Role of Gut Microbes and Host’s Immune Response in Gut–Lung Homeostasis. Front. Immunol. 2022, 13, 954339. [Google Scholar] [CrossRef]
- Xu, R.; Lu, R.; Zhang, T.; Wu, Q.; Cai, W.; Han, X.; Wan, Z.; Jin, X.; Zhang, Z.; Zhang, C. Temporal Association between Human Upper Respiratory and Gut Bacterial Microbiomes during the Course of COVID-19 in Adults. Commun. Biol. 2021, 4, 240. [Google Scholar] [CrossRef]
- Hernández-Terán, A.; Mejía-Nepomuceno, F.; Herrera, M.T.; Barreto, O.; García, E.; Castillejos, M.; Boukadida, C.; Matias-Florentino, M.; Rincón-Rubio, A.; Avila-Rios, S.; et al. Dysbiosis and Structural Disruption of the Respiratory Microbiota in COVID-19 Patients with Severe and Fatal Outcomes. Sci. Rep. 2021, 11, 21297. [Google Scholar] [CrossRef]
- Zuo, T.; Zhang, F.; Lui, G.C.Y.; Yeoh, Y.K.; Li, A.Y.L.; Zhan, H.; Wan, Y.; Chung, A.C.K.; Cheung, C.P.; Chen, N.; et al. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology 2020, 159, 944–955.e8. [Google Scholar] [CrossRef]
- Mizutani, T.; Ishizaka, A.; Koga, M.; Ikeuchi, K.; Saito, M.; Adachi, E.; Yamayoshi, S.; Iwatsuki-Horimoto, K.; Yasuhara, A.; Kiyono, H.; et al. Correlation Analysis between Gut Microbiota Alterations and the Cytokine Response in Patients with Coronavirus Disease during Hospitalization. Microbiol. Spectr. 2022, 10, e01689-21. [Google Scholar] [CrossRef]
- Gang, J.; Wang, H.; Xue, X.; Zhang, S. Microbiota and COVID-19: Long-Term and Complex Influencing Factors. Front. Microbiol. 2022, 13, 963488. [Google Scholar] [CrossRef]
- Schult, D.; Reitmeier, S.; Koyumdzhieva, P.; Lahmer, T.; Middelhoff, M.; Erber, J.; Schneider, J.; Kager, J.; Frolova, M.; Horstmann, J.; et al. Gut Bacterial Dysbiosis and Instability Is Associated with the Onset of Complications and Mortality in COVID-19. Gut Microbes 2022, 14, 2031840. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhang, J.; Zhang, D.; Ma, W.-L.; Wang, X. Linking the Gut Microbiota to Persistent Symptoms in Survivors of COVID-19 after Discharge. J. Microbiol. 2021, 59, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Yeoh, Y.K.; Zuo, T.; Lui, G.C.-Y.; Zhang, F.; Liu, Q.; Li, A.Y.; Chung, A.C.; Cheung, C.P.; Tso, E.Y.; Fung, K.S.; et al. Gut Microbiota Composition Reflects Disease Severity and Dysfunctional Immune Responses in Patients with COVID-19. Gut 2021, 70, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Hazan, S.; Stollman, N.; Bozkurt, H.S.; Dave, S.; Papoutsis, A.J.; Daniels, J.; Barrows, B.D.; Quigley, E.M.; Borody, T.J. Lost Microbes of COVID-19: Bifidobacterium, Faecalibacterium Depletion and Decreased Microbiome Diversity Associated with SARS-CoV-2 Infection Severity. BMJ Open Gastroenterol. 2022, 9, e000871. [Google Scholar] [CrossRef]
- Proal, A.D.; VanElzakker, M.B. Long COVID or Post-Acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms. Front. Microbiol. 2021, 12, 698169. [Google Scholar] [CrossRef]
- Pavli, A.; Theodoridou, M.; Maltezou, H.C. Post-COVID Syndrome: Incidence, Clinical Spectrum, and Challenges for Primary Healthcare Professionals. Arch. Med. Res. 2021, 52, 575–581. [Google Scholar] [CrossRef]
- Post COVID-19 Condition (Long Covid). Available online: Https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-clinical_case_definition-2021.1 (accessed on 11 November 2022).
- Petersen, M.S.; Kristiansen, M.F.; Hanusson, K.D.; Foldbo, B.M.; Danielsen, M.E.; á Steig, B.; Gaini, S.; Strøm, M.; Weihe, P. Prevalence of Long COVID in a National Cohort: Longitudinal Measures from Disease Onset until 8 Months’ Follow-Up. Int. J. Infect. Dis. 2022, 122, 437–441. [Google Scholar] [CrossRef]
- López-Sampalo, A.; Bernal-López, M.R.; Gómez-Huelgas, R. Síndrome de COVID-19 persistente. Una revisión narrativa. Rev. Clínica Esp. 2022, 222, 241–250. [Google Scholar] [CrossRef]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary Manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef]
- Desai, A.D.; Lavelle, M.; Boursiquot, B.C.; Wan, E.Y. Long-Term Complications of COVID-19. Am. J. Physiol.-Cell Physiol. 2022, 322, C1–C11. [Google Scholar] [CrossRef] [PubMed]
- Carod Artal, F.J. Síndrome post-COVID-19: Epidemiología, criterios diagnósticos y mecanismos patogénicos implicados. Rev. Neurol. 2021, 72, 384. [Google Scholar] [CrossRef] [PubMed]
- Brightling, C.E.; Evans, R.A. Long COVID: Which Symptoms Can Be Attributed to SARS-CoV-2 Infection? Lancet 2022, 400, 411–413. [Google Scholar] [CrossRef] [PubMed]
- Han, Q.; Zheng, B.; Daines, L.; Sheikh, A. Long-Term Sequelae of COVID-19: A Systematic Review and Meta-Analysis of One-Year Follow-Up Studies on Post-COVID Symptoms. Pathogens 2022, 11, 269. [Google Scholar] [CrossRef] [PubMed]
- Fumagalli, C.; Zocchi, C.; Tassetti, L.; Silverii, M.V.; Amato, C.; Livi, L.; Giovannoni, L.; Verrillo, F.; Bartoloni, A.; Marcucci, R.; et al. Factors Associated with Persistence of Symptoms 1 Year after COVID-19: A Longitudinal, Prospective Phone-Based Interview Follow-up Cohort Study. Eur. J. Intern. Med. 2022, 97, 36–41. [Google Scholar] [CrossRef]
- Yong, S.J.; Liu, S. Proposed Subtypes of post-COVID-19 Syndrome (or long-COVID) and Their Respective Potential Therapies. Rev. Med. Virol. 2022, 32, e2315. [Google Scholar] [CrossRef]
- Georgiou, K.; Marinov, B.; Farooqi, A.A.; Gazouli, M. Gut Microbiota in Lung Cancer: Where Do We Stand? Int. J. Mol. Sci. 2021, 22, 10429. [Google Scholar] [CrossRef]
- Chunxi, L.; Haiyue, L.; Yanxia, L.; Jianbing, P.; Jin, S. The Gut Microbiota and Respiratory Diseases: New Evidence. J. Immunol. Res. 2020, 2020, 2340670. [Google Scholar] [CrossRef]
- Hou, K.; Wu, Z.-X.; Chen, X.-Y.; Wang, J.-Q.; Zhang, D.; Xiao, C.; Zhu, D.; Koya, J.B.; Wei, L.; Li, J.; et al. Microbiota in Health and Diseases. Signal Transduct. Target. Ther. 2022, 7, 135. [Google Scholar] [CrossRef]
- Invernizzi, R.; Lloyd, C.M.; Molyneaux, P.L. Respiratory Microbiome and Epithelial Interactions Shape Immunity in the Lungs. Immunology 2020, 160, 171–182. [Google Scholar] [CrossRef]
- Sommariva, M.; Le Noci, V.; Bianchi, F.; Camelliti, S.; Balsari, A.; Tagliabue, E.; Sfondrini, L. The Lung Microbiota: Role in Maintaining Pulmonary Immune Homeostasis and Its Implications in Cancer Development and Therapy. Cell. Mol. Life Sci. CMLS 2020, 77, 2739–2749. [Google Scholar] [CrossRef] [PubMed]
- Joseph, S.W.; Carnahan, A.; Rollins, D.; Walker, R.I. Aeromonas and Plesiomonas in the Environment: Value of Differential Biotyping of Aeromonads. J. Diarrhoeal Dis. Res. 1988, 6, 80–87. [Google Scholar] [PubMed]
- Dang, A.T.; Marsland, B.J. Microbes, Metabolites, and the Gut-Lung Axis. Mucosal Immunol. 2019, 12, 843–850. [Google Scholar] [CrossRef]
- McAleer, J.P.; Nguyen, N.L.H.; Chen, K.; Kumar, P.; Ricks, D.M.; Binnie, M.; Armentrout, R.A.; Pociask, D.A.; Hein, A.; Yu, A.; et al. Pulmonary Th17 Antifungal Immunity Is Regulated by the Gut Microbiome. J. Immunol. 2016, 197, 97–107. [Google Scholar] [CrossRef]
- Wang, J.; Tian, Z. How Lung Infection Leads to Gut Injury. Oncotarget 2015, 6, 42394–42395. [Google Scholar] [CrossRef]
- Zhou, A.; Lei, Y.; Tang, L.; Hu, S.; Yang, M.; Wu, L.; Yang, S.; Tang, B. Gut Microbiota: The Emerging Link to Lung Homeostasis and Disease. J. Bacteriol. 2021, 203, e00454-20. [Google Scholar] [CrossRef]
- Wang, H.; Liu, J.-S.; Peng, S.-H.; Deng, X.-Y.; Zhu, D.-M.; Javidiparsijani, S.; Wang, G.-R.; Li, D.-Q.; Li, L.-X.; Wang, Y.-C.; et al. Gut-Lung Crosstalk in Pulmonary Involvement with Inflammatory Bowel Diseases. World, J. Gastroenterol. 2013, 19, 6794–6804. [Google Scholar] [CrossRef]
- Harper, A.; Vijayakumar, V.; Ouwehand, A.C.; ter Haar, J.; Obis, D.; Espadaler, J.; Binda, S.; Desiraju, S.; Day, R. Viral Infections, the Microbiome, and Probiotics. Front. Cell. Infect. Microbiol. 2021, 10, 596166. [Google Scholar] [CrossRef]
- Mizutani, T.; Ishizaka, A.; Koga, M.; Tsutsumi, T.; Yotsuyanagi, H. Role of Microbiota in Viral Infections and Pathological Progression. Viruses 2022, 14, 950. [Google Scholar] [CrossRef]
- Bosch, A.A.T.M.; Biesbroek, G.; Trzcinski, K.; Sanders, E.A.M.; Bogaert, D. Viral and Bacterial Interactions in the Upper Respiratory Tract. PLoS Pathog. 2013, 9, e1003057. [Google Scholar] [CrossRef]
- Man, W.H.; de Steenhuijsen Piters, W.A.A.; Bogaert, D. The Microbiota of the Respiratory Tract: Gatekeeper to Respiratory Health. Nat. Rev. Microbiol. 2017, 15, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Ormerod, K.L.; Wood, D.L.A.; Lachner, N.; Gellatly, S.L.; Daly, J.N.; Parsons, J.D.; Dal’Molin, C.G.O.; Palfreyman, R.W.; Nielsen, L.K.; Cooper, M.A.; et al. Genomic Characterization of the Uncultured Bacteroidales Family S24-7 Inhabiting the Guts of Homeothermic Animals. Microbiome 2016, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- den Besten, G.; van Eunen, K.; Groen, A.K.; Venema, K.; Reijngoud, D.-J.; Bakker, B.M. The Role of Short-Chain Fatty Acids in the Interplay between Diet, Gut Microbiota, and Host Energy Metabolism. J. Lipid Res. 2013, 54, 2325–2340. [Google Scholar] [CrossRef] [PubMed]
- Woods Acevedo, M.A.; Pfeiffer, J.K. Microbiota-Immune System Interactions and Enteric Virus Infection. Curr. Opin. Virol. 2021, 46, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Feng, C.; Jin, C.; Liu, K.; Yang, Z. Microbiota-Derived Short Chain Fatty Acids: Their Role and Mechanisms in Viral Infections. Biomed. Pharmacother. 2023, 160, 114414. [Google Scholar] [CrossRef]
- Antunes, K.H.; Fachi, J.L.; de Paula, R.; da Silva, E.F.; Pral, L.P.; dos Santos, A.Á.; Dias, G.B.M.; Vargas, J.E.; Puga, R.; Mayer, F.Q.; et al. Microbiota-Derived Acetate Protects against Respiratory Syncytial Virus Infection through a GPR43-Type 1 Interferon Response. Nat. Commun. 2019, 10, 3273. [Google Scholar] [CrossRef]
- Erttmann, S.F.; Swacha, P.; Aung, K.M.; Brindefalk, B.; Jiang, H.; Härtlova, A.; Uhlin, B.E.; Wai, S.N.; Gekara, N.O. The Gut Microbiota Prime Systemic Antiviral Immunity via the cGAS-STING-IFN-I Axis. Immunity 2022, 55, 847–861.e10. [Google Scholar] [CrossRef]
- Sencio, V.; Machado, M.G.; Trottein, F. The Lung–Gut Axis during Viral Respiratory Infections: The Impact of Gut Dysbiosis on Secondary Disease Outcomes. Mucosal Immunol. 2021, 14, 296–304. [Google Scholar] [CrossRef]
- Lv, Z.; Xiong, D.; Shi, J.; Long, M.; Chen, Z. The Interaction Between Viruses and Intestinal Microbiota: A Review. Curr. Microbiol. 2021, 78, 3597–3608. [Google Scholar] [CrossRef]
- Van Winkle, J.A.; Peterson, S.T.; Kennedy, E.A.; Wheadon, M.J.; Ingle, H.; Desai, C.; Rodgers, R.; Constant, D.A.; Wright, A.P.; Li, L.; et al. Homeostatic Interferon-Lambda Response to Bacterial Microbiota Stimulates Preemptive Antiviral Defense within Discrete Pockets of Intestinal Epithelium. eLife 2022, 11, e74072. [Google Scholar] [CrossRef]
- Stefan, K.L.; Kim, M.V.; Iwasaki, A.; Kasper, D.L. Commensal Microbiota Modulation of Natural Resistance to Virus Infection. Cell 2020, 183, 1312–1324.e10. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Wang, J.; Li, F.; Shi, Y. Main Clinical Features of COVID-19 and Potential Prognostic and Therapeutic Value of the Microbiota in SARS-CoV-2 Infections. Front. Microbiol. 2020, 11, 1302. [Google Scholar] [CrossRef] [PubMed]
- Aan, F.J.; Glibetic, N.; Montoya-Uribe, V.; Matter, M.L. COVID-19 and the Microbiome: The Gut-Lung Connection. In Comprehensive Gut Microbiota; Elsevier: Amsterdam, The Netherlands, 2022; pp. 442–458. ISBN 978-0-12-822036-8. [Google Scholar]
- Gu, S.; Chen, Y.; Wu, Z.; Chen, Y.; Gao, H.; Lv, L.; Guo, F.; Zhang, X.; Luo, R.; Huang, C.; et al. Alterations of the Gut Microbiota in Patients With Coronavirus Disease 2019 or H1N1 Influenza. Clin. Infect. Dis. 2020, 71, 2669–2678. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Yang, S.; Zhou, Y.; Disoma, C.; Dong, Z.; Du, A.; Zhang, Y.; Chen, Y.; Huang, W.; Chen, J.; et al. Microbiome Profiling Using Shotgun Metagenomic Sequencing Identified Unique Microorganisms in COVID-19 Patients With Altered Gut Microbiota. Front. Microbiol. 2021, 12, 712081. [Google Scholar] [CrossRef]
- Stutz, M.R.; Dylla, N.P.; Pearson, S.D.; Lecompte-Osorio, P.; Nayak, R.; Khalid, M.; Adler, E.; Boissiere, J.; Lin, H.; Leiter, W.; et al. Immunomodulatory Fecal Metabolites Are Associated with Mortality in COVID-19 Patients with Respiratory Failure. Nat. Commun. 2022, 13, 6615. [Google Scholar] [CrossRef]
- Bernard-Raichon, L.; Venzon, M.; Klein, J.; Axelrad, J.E.; Zhang, C.; Sullivan, A.P.; Hussey, G.A.; Casanovas-Massana, A.; Noval, M.G.; Valero-Jimenez, A.M.; et al. Gut Microbiome Dysbiosis in Antibiotic-Treated COVID-19 Patients Is Associated with Microbial Translocation and Bacteremia. Nat. Commun. 2022, 13, 5926. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Wan, Y.; Zuo, T.; Yeoh, Y.K.; Liu, Q.; Zhang, L.; Zhan, H.; Lu, W.; Xu, W.; Lui, G.C.Y.; et al. Prolonged Impairment of Short-Chain Fatty Acid and L-Isoleucine Biosynthesis in Gut Microbiome in Patients With COVID-19. Gastroenterology 2022, 162, 548–561.e4. [Google Scholar] [CrossRef]
- Vestad, B.; Ueland, T.; Lerum, T.V.; Dahl, T.B.; Holm, K.; Barratt-Due, A.; Kåsine, T.; Dyrhol-Riise, A.M.; Stiksrud, B.; Tonby, K.; et al. Respiratory Dysfunction Three Months after Severe COVID-19 Is Associated with Gut Microbiota Alterations. J. Intern. Med. 2022, 291, 801–812. [Google Scholar] [CrossRef]
- Romani, L.; Del Chierico, F.; Macari, G.; Pane, S.; Ristori, M.V.; Guarrasi, V.; Gardini, S.; Pascucci, G.R.; Cotugno, N.; Perno, C.F.; et al. The Relationship Between Pediatric Gut Microbiota and SARS-CoV-2 Infection. Front. Cell. Infect. Microbiol. 2022, 12, 908492. [Google Scholar] [CrossRef]
- Mosca, A.; Leclerc, M.; Hugot, J.P. Gut Microbiota Diversity and Human Diseases: Should We Reintroduce Key Predators in Our Ecosystem? Front. Microbiol. 2016, 7, 455. [Google Scholar] [CrossRef]
- Tang, L.; Gu, S.; Gong, Y.; Li, B.; Lu, H.; Li, Q.; Zhang, R.; Gao, X.; Wu, Z.; Zhang, J.; et al. Clinical Significance of the Correlation between Changes in the Major Intestinal Bacteria Species and COVID-19 Severity. Engineering 2020, 6, 1178–1184. [Google Scholar] [CrossRef]
- Tao, W.; Zhang, G.; Wang, X.; Guo, M.; Zeng, W.; Xu, Z.; Cao, D.; Pan, A.; Wang, Y.; Zhang, K.; et al. Analysis of the Intestinal Microbiota in COVID-19 Patients and Its Correlation with the Inflammatory Factor IL-18. Med. Microecol. 2020, 5, 100023. [Google Scholar] [CrossRef] [PubMed]
- Louis, P.; Flint, H.J. Diversity, Metabolism and Microbial Ecology of Butyrate-Producing Bacteria from the Human Large Intestine. FEMS Microbiol. Lett. 2009, 294, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Andoh, A.; Tsujikawa, T.; Fujiyama, Y. Role of Dietary Fiber and Short-Chain Fatty Acids in the Colon. Curr. Pharm. Des. 2003, 9, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Sokol, H.; Pigneur, B.; Watterlot, L.; Lakhdari, O.; Bermúdez-Humarán, L.G.; Gratadoux, J.-J.; Blugeon, S.; Bridonneau, C.; Furet, J.-P.; Corthier, G.; et al. Faecalibacterium Prausnitzii Is an Anti-Inflammatory Commensal Bacterium Identified by Gut Microbiota Analysis of Crohn Disease Patients. Proc. Natl. Acad. Sci. USA 2008, 105, 16731–16736. [Google Scholar] [CrossRef]
- Larsen, J.M. The Immune Response to Prevotella Bacteria in Chronic Inflammatory Disease. Immunology 2017, 151, 363–374. [Google Scholar] [CrossRef]
- Novick, D.; Kim, S.; Kaplanski, G.; Dinarello, C.A. Interleukin-18, More than a Th1 Cytokine. Semin. Immunol. 2013, 25, 439–448. [Google Scholar] [CrossRef]
- Ceramella, J.; Iacopetta, D.; Sinicropi, M.S.; Andreu, I.; Mariconda, A.; Saturnino, C.; Giuzio, F.; Longo, P.; Aquaro, S.; Catalano, A. Drugs for COVID-19: An Update. Molecules 2022, 27, 8562. [Google Scholar] [CrossRef]
- Granata, G.; Schiavone, F.; Pipitone, G.; Taglietti, F.; Petrosillo, N. Antibiotics Use in COVID-19 Patients: A Systematic Literature Review. J. Clin. Med. 2022, 11, 7207. [Google Scholar] [CrossRef]
- Groves, H.T.; Cuthbertson, L.; James, P.; Moffatt, M.F.; Cox, M.J.; Tregoning, J.S. Respiratory Disease Following Viral Lung Infection Alters the Murine Gut Microbiota. Front. Immunol. 2018, 9, 182. [Google Scholar] [CrossRef]
- Harding, J.N.; Siefker, D.; Vu, L.; You, D.; DeVincenzo, J.; Pierre, J.; Cormier, S.A. Altered Gut Microbiota in Infants Is Associated with Respiratory Syncytial Virus Disease Severity. BMC Microbiol. 2020, 20, 140. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Zhang, C.; Qian, G.; Hu, X.; Zhang, H.; Chen, C.; Liang, W.; Gao, H.; Yang, Y.; Li, L. An Analysis of Microbiota-Targeted Therapies in Patients with Avian Influenza Virus Subtype H7N9 Infection. BMC Infect. Dis. 2014, 14, 359. [Google Scholar] [CrossRef] [PubMed]
- Qin, N.; Zheng, B.; Yao, J.; Guo, L.; Zuo, J.; Wu, L.; Zhou, J.; Liu, L.; Guo, J.; Ni, S.; et al. Influence of H7N9 Virus Infection and Associated Treatment on Human Gut Microbiota. Sci. Rep. 2015, 5, 14771. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef] [PubMed]
- Ou, X.; Liu, Y.; Lei, X.; Li, P.; Mi, D.; Ren, L.; Guo, L.; Guo, R.; Chen, T.; Hu, J.; et al. Characterization of Spike Glycoprotein of SARS-CoV-2 on Virus Entry and Its Immune Cross-Reactivity with SARS-CoV. Nat. Commun. 2020, 11, 1620. [Google Scholar] [CrossRef] [PubMed]
- Geva-Zatorsky, N.; Sefik, E.; Kua, L.; Pasman, L.; Tan, T.G.; Ortiz-Lopez, A.; Yanortsang, T.B.; Yang, L.; Jupp, R.; Mathis, D.; et al. Mining the Human Gut Microbiota for Immunomodulatory Organisms. Cell 2017, 168, 928–943.e11. [Google Scholar] [CrossRef]
- Ahmadi Badi, S.; Malek, A.; Paolini, A.; Rouhollahi Masoumi, M.; Seyedi, S.A.; Amanzadeh, A.; Masotti, A.; Khatami, S.; Siadat, S.D. Downregulation of ACE, AGTR1, and ACE2 Genes Mediating SARS-CoV-2 Pathogenesis by Gut Microbiota Members and Their Postbiotics on Caco-2 Cells. Microb. Pathog. 2022, 173, 105798. [Google Scholar] [CrossRef]
- Guo, Y.; Wang, B.; Gao, H.; Gao, L.; Hua, R.; Xu, J.-D. ACE2 in the Gut: The Center of the 2019-nCoV Infected Pathology. Front. Mol. Biosci. 2021, 8, 708336. [Google Scholar] [CrossRef]
- Cheon, S.Y.; Koo, B.-N. Inflammatory Response in COVID-19 Patients Resulting from the Interaction of the Inflammasome and SARS-CoV-2. Int. J. Mol. Sci. 2021, 22, 7914. [Google Scholar] [CrossRef]
- Yoo, J.; Groer, M.; Dutra, S.; Sarkar, A.; McSkimming, D. Gut Microbiota and Immune System Interactions. Microorganisms 2020, 8, 1587. [Google Scholar] [CrossRef]
- Beyerstedt, S.; Casaro, E.B.; Rangel, É.B. COVID-19: Angiotensin-Converting Enzyme 2 (ACE2) Expression and Tissue Susceptibility to SARS-CoV-2 Infection. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 905–919. [Google Scholar] [CrossRef]
- De Maio, F.; Ianiro, G.; Coppola, G.; Santopaolo, F.; Abbate, V.; Bianco, D.M.; Del Zompo, F.; De Matteis, G.; Leo, M.; Nesci, A.; et al. Improved Gut Microbiota Features after the Resolution of SARS-CoV-2 Infection. Gut Pathog. 2021, 13, 62. [Google Scholar] [CrossRef] [PubMed]
- Su, Q.; Liu, Q.; Lau, R.I.; Zhang, J.; Xu, Z.; Yeoh, Y.K.; Leung, T.W.H.; Tang, W.; Zhang, L.; Liang, J.Q.Y.; et al. Faecal Microbiome-Based Machine Learning for Multi-Class Disease Diagnosis. Nat. Commun. 2022, 13, 6818. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wu, G.; Zhao, L.; Wang, W. Nutritional Modulation of Gut Microbiota Alleviates Severe Gastrointestinal Symptoms in a Patient with Post-Acute COVID-19 Syndrome. mBio 2022, 13, e03801-21. [Google Scholar] [CrossRef] [PubMed]
- Zurabov, F.M.; Chernevskaya, E.A.; Beloborodova, N.V.; Zurabov, A.Y.; Petrova, M.V.; Yadgarov, M.Y.; Popova, V.M.; Fatuev, O.E.; Zakharchenko, V.E.; Gurkova, M.M.; et al. Bacteriophage Cocktails in the Post-COVID Rehabilitation. Viruses 2022, 14, 2614. [Google Scholar] [CrossRef]
- Liu, Q.; Su, Q.; Zhang, F.; Tun, H.M.; Mak, J.W.Y.; Lui, G.C.-Y.; Ng, S.S.S.; Ching, J.Y.L.; Li, A.; Lu, W.; et al. Multi-Kingdom Gut Microbiota Analyses Define COVID-19 Severity and Post-Acute COVID-19 Syndrome. Nat. Commun. 2022, 13, 6806. [Google Scholar] [CrossRef]
- Xu, X.; Zhang, W.; Guo, M.; Xiao, C.; Fu, Z.; Yu, S.; Jiang, L.; Wang, S.; Ling, Y.; Liu, F.; et al. Integrated Analysis of Gut Microbiome and Host Immune Responses in COVID-19. Front. Med. 2022, 16, 263–275. [Google Scholar] [CrossRef]
- Zhang, D.; Zhou, Y.; Ma, Y.; Chen, P.; Tang, J.; Yang, B.; Li, H.; Liang, M.; Xue, Y.; Liu, Y.; et al. Gut Microbiota Dysbiosis Correlates With Long COVID-19 at One-Year After Discharge. J. Korean Med. Sci. 2023, 38, e120. [Google Scholar] [CrossRef]
- Trottein, F.; Sokol, H. Potential Causes and Consequences of Gastrointestinal Disorders during a SARS-CoV-2 Infection. Cell Rep. 2020, 32, 107915. [Google Scholar] [CrossRef]
- Thorson, A.E.; Deen, G.F.; Bernstein, K.T.; Liu, W.J.; Yamba, F.; Habib, N.; Sesay, F.R.; Gaillard, P.; Massaquoi, T.A.; McDonald, S.L.R.; et al. Persistence of Ebola Virus in Semen among Ebola Virus Disease Survivors in Sierra Leone: A Cohort Study of Frequency, Duration, and Risk Factors. PLoS Med. 2021, 18, e1003273. [Google Scholar] [CrossRef]
- Aid, M.; Abbink, P.; Larocca, R.A.; Boyd, M.; Nityanandam, R.; Nanayakkara, O.; Martinot, A.J.; Moseley, E.T.; Blass, E.; Borducchi, E.N.; et al. Zika Virus Persistence in the Central Nervous System and Lymph Nodes of Rhesus Monkeys. Cell 2017, 169, 610–620.e14. [Google Scholar] [CrossRef] [PubMed]
- Walsh, K.A.; Jordan, K.; Clyne, B.; Rohde, D.; Drummond, L.; Byrne, P.; Ahern, S.; Carty, P.G.; O’Brien, K.K.; O’Murchu, E.; et al. SARS-CoV-2 Detection, Viral Load and Infectivity over the Course of an Infection. J. Infect. 2020, 81, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Xu, E.; Xie, Y.; Al-Aly, Z. Long-Term Gastrointestinal Outcomes of COVID-19. Nat. Commun. 2023, 14, 983. [Google Scholar] [CrossRef] [PubMed]
- Filip, R.; Gheorghita Puscaselu, R.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef]
- Farsi, Y.; Tahvildari, A.; Arbabi, M.; Vazife, F.; Sechi, L.A.; Shahidi Bonjar, A.H.; Jamshidi, P.; Nasiri, M.J.; Mirsaeidi, M. Diagnostic, Prognostic, and Therapeutic Roles of Gut Microbiota in COVID-19: A Comprehensive Systematic Review. Front. Cell. Infect. Microbiol. 2022, 12, 804644. [Google Scholar] [CrossRef]
- Zhang, J.; Garrett, S.; Sun, J. Gastrointestinal Symptoms, Pathophysiology, and Treatment in COVID-19. Genes Dis. 2020, 8, 385–400. [Google Scholar] [CrossRef]
- De, R.; Dutta, S. Role of the Microbiome in the Pathogenesis of COVID-19. Front. Cell. Infect. Microbiol. 2022, 12, 736397. [Google Scholar] [CrossRef]
- Papadopoulou, G.; Manoloudi, E.; Repousi, N.; Skoura, L.; Hurst, T.; Karamitros, T. Molecular and Clinical Prognostic Biomarkers of COVID-19 Severity and Persistence. Pathogens 2022, 11, 311. [Google Scholar] [CrossRef]
- Neag, M.A.; Vulturar, D.-M.; Gherman, D.; Burlacu, C.-C.; Todea, D.A.; Buzoianu, A.D. Gastrointestinal Microbiota: A Predictor of COVID-19 Severity? World, J. Gastroenterol. 2022, 28, 6328–6344. [Google Scholar] [CrossRef]
- Mazzarelli, A.; Giancola, M.L.; Fontana, A.; Piselli, P.; Binda, E.; Trivieri, N.; Mencarelli, G.; Marchioni, L.; Vulcano, A.; De Giuli, C.; et al. Gut Microbiota Composition in COVID-19 Hospitalized Patients with Mild or Severe Symptoms. Front. Microbiol. 2022, 13. [Google Scholar] [CrossRef]
- Alsayed, A.R.; Abed, A.; Khader, H.A.; Al-Shdifat, L.M.H.; Hasoun, L.; Al-Rshaidat, M.M.D.; Alkhatib, M.; Zihlif, M. Molecular Accounting and Profiling of Human Respiratory Microbial Communities: Toward Precision Medicine by Targeting the Respiratory Microbiome for Disease Diagnosis and Treatment. Int. J. Mol. Sci. 2023, 24, 4086. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.; Jin, J.; Chen, M.; Chen, Y. The Impact of Infection with COVID-19 on the Respiratory Microbiome: A Narrative Review. Virulence 2022, 13, 1076–1087. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.; Wang, Y.; Zhong, J.; Li, X.; Xiao, Y.; Li, J.; Yang, J.; Fan, G.; Guo, L.; Shen, Z.; et al. Dynamics of the Upper Respiratory Tract Microbiota and Its Association with Mortality in COVID-19. Am. J. Respir. Crit. Care Med. 2021, 204, 1379–1390. [Google Scholar] [CrossRef] [PubMed]
- Durán-Manuel, E.M.; Loyola-Cruz, M.Á.; Cruz-Cruz, C.; Ibáñez-Cervantes, G.; Gaytán-Cervantes, J.; González-Torres, C.; Quiroga-Vargas, E.; Calzada-Mendoza, C.C.; Cureño-Díaz, M.A.; Fernández-Sánchez, V.; et al. Massive Sequencing of the V3-V4 Hypervariable Region of Bronchoalveolar Lavage from Patients with COVID-19 and VAP Reveals the Collapse of the Pulmonary Microbiota. J. Med. Microbiol. 2022, 71. [Google Scholar] [CrossRef]
- Merenstein, C.; Liang, G.; Whiteside, S.A.; Cobián-Güemes, A.G.; Merlino, M.S.; Taylor, L.J.; Glascock, A.; Bittinger, K.; Tanes, C.; Graham-Wooten, J.; et al. Signatures of COVID-19 Severity and Immune Response in the Respiratory Tract Microbiome. mBio 2021, 12, e01777-21. [Google Scholar] [CrossRef]
- Ojala, T.; Kankuri, E.; Kankainen, M. Understanding Human Health through Metatranscriptomics. Trends Mol. Med. 2023, 29, 376–389. [Google Scholar] [CrossRef]
- Athanasopoulou, K.; Adamopoulos, P.G.; Scorilas, A. Unveiling the Human Gastrointestinal Tract Microbiome: The Past, Present, and Future of Metagenomics. Biomedicines 2023, 11, 827. [Google Scholar] [CrossRef]
- Mańkowska-Wierzbicka, D.; Zuraszek, J.; Wierzbicka, A.; Gabryel, M.; Mahadea, D.; Baturo, A.; Zakerska-Banaszak, O.; Slomski, R.; Skrzypczak-Zielinska, M.; Dobrowolska, A. Alterations in Gut Microbiota Composition in Patients with COVID-19: A Pilot Study of Whole Hypervariable 16S rRNA Gene Sequencing. Biomedicines 2023, 11, 367. [Google Scholar] [CrossRef]
- Conti, V.; Corbi, G.; Sabbatino, F.; De Pascale, D.; Sellitto, C.; Stefanelli, B.; Bertini, N.; De Simone, M.; Liguori, L.; Di Paola, I.; et al. Long COVID: Clinical Framing, Biomarkers, and Therapeutic Approaches. J. Pers. Med. 2023, 13, 334. [Google Scholar] [CrossRef]
- Fernández-Lázaro, D.; Sánchez-Serrano, N.; Mielgo-Ayuso, J.; García-Hernández, J.L.; González-Bernal, J.J.; Seco-Calvo, J. Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic? J. Clin. Med. 2021, 10, 5799. [Google Scholar] [CrossRef]
- Scarpellini, E.; Tack, J. Post-COVID-19 Gastro-Intestinal Disturbances. Rev. Recent Clin. Trials 2023, 18, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Xavier-Santos, D.; Padilha, M.; Fabiano, G.A.; Vinderola, G.; Gomes Cruz, A.; Sivieri, K.; Costa Antunes, A.E. Evidences and Perspectives of the Use of Probiotics, Prebiotics, Synbiotics, and Postbiotics as Adjuvants for Prevention and Treatment of COVID-19: A Bibliometric Analysis and Systematic Review. Trends Food Sci. Technol. 2022, 120, 174–192. [Google Scholar] [CrossRef] [PubMed]
- Kazemian, N.; Kao, D.; Pakpour, S. Fecal Microbiota Transplantation during and Post-COVID-19 Pandemic. Int. J. Mol. Sci. 2021, 22, 3004. [Google Scholar] [CrossRef] [PubMed]
- Biliński, J.; Winter, K.; Jasiński, M.; Szczęś, A.; Bilinska, N.; Mullish, B.H.; Małecka-Panas, E.; Basak, G.W. Rapid Resolution of COVID-19 after Faecal Microbiota Transplantation. Gut 2022, 71, 230–232. [Google Scholar] [CrossRef]
- Ianiro, G.; Mullish, B.H.; Kelly, C.R.; Sokol, H.; Kassam, Z.; Ng, S.C.; Fischer, M.; Allegretti, J.R.; Masucci, L.; Zhang, F.; et al. Screening of Faecal Microbiota Transplant Donors during the COVID-19 Outbreak: Suggestions for Urgent Updates from an International Expert Panel. Lancet Gastroenterol. Hepatol. 2020, 5, 430–432. [Google Scholar] [CrossRef]
- Khaled, J.M.A. Probiotics, Prebiotics, and COVID-19 Infection: A Review Article. Saudi, J. Biol. Sci. 2021, 28, 865–869. [Google Scholar] [CrossRef]
- Ray, M.; Manjunath, A.; Halami, P.M. Effect of Probiotics as an Immune Modulator for the Management of COVID-19. Arch. Microbiol. 2023, 205, 182. [Google Scholar] [CrossRef]
- Wang, M.; Zhang, Y.; Li, C.; Chang, W.; Zhang, L. The Relationship between Gut Microbiota and COVID-19 Progression: New Insights into Immunopathogenesis and Treatment. Front. Immunol. 2023, 14. [Google Scholar] [CrossRef]
- Brown, J.A.; Sanidad, K.Z.; Lucotti, S.; Lieber, C.M.; Cox, R.M.; Ananthanarayanan, A.; Basu, S.; Chen, J.; Shan, M.; Amir, M.; et al. Gut Microbiota-Derived Metabolites Confer Protection against SARS-CoV-2 Infection. Gut Microbes 2022, 14, 2105609. [Google Scholar] [CrossRef]
- Ballesteros, R.V.; Gámez, M.A.; Macaya-Ten, F.; Martínez, M.V.; Tejedor, A.V. An Uncommon Cause of Anterior ST-Segment Elevation. Eur. Heart, J. Case Rep. 2023, 7, ytad299. [Google Scholar] [CrossRef]
| Loss of Diversity | Increased Opportunistic Bacteria | Decreased Commensal Bacteria | Decreased SCFA Producing Bacteria | Decreased F. prausnitzii | Detected Specific Bacteria | References | |
|---|---|---|---|---|---|---|---|
| COVID-19 | +++ | + | + | + | + | Streptococcus thermophilus, Bacteroides oleiciplenus, Blautia, Fusobacterium ulcerans, and Prevotella bivia | [6,10,13,15,57,59,60,64,65] |
| RSV | - | - | ND | - | - | Odoribacter, Oribacterium, Clostridiales, and Coriobacteriaceae | [74] |
| Seasonal flu | ++ | - | - | - | - | Oribacterium, Bulleidia, and Aggregatibacter | [60] |
| H1N1 | +++ | + | + | + | Prevotella and Ezakiella | [56,62] | |
| H7N9 | + | + | + | - | + (Only in AB treated patients) | Clostridium sp., Escherichia coli and Enterococcus faecium | [75,76] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Corona, N.C.; López-Ortega, O.; Pérez-Martínez, C.A.; Martínez-Castillo, M.; De Jesús-González, L.A.; León-Reyes, G.; León-Juárez, M. Dynamics of the Microbiota and Its Relationship with Post-COVID-19 Syndrome. Int. J. Mol. Sci. 2023, 24, 14822. https://doi.org/10.3390/ijms241914822
Moreno-Corona NC, López-Ortega O, Pérez-Martínez CA, Martínez-Castillo M, De Jesús-González LA, León-Reyes G, León-Juárez M. Dynamics of the Microbiota and Its Relationship with Post-COVID-19 Syndrome. International Journal of Molecular Sciences. 2023; 24(19):14822. https://doi.org/10.3390/ijms241914822
Chicago/Turabian StyleMoreno-Corona, Nidia Carolina, Orestes López-Ortega, Cesar Augusto Pérez-Martínez, Macario Martínez-Castillo, Luis Adrián De Jesús-González, Guadalupe León-Reyes, and Moisés León-Juárez. 2023. "Dynamics of the Microbiota and Its Relationship with Post-COVID-19 Syndrome" International Journal of Molecular Sciences 24, no. 19: 14822. https://doi.org/10.3390/ijms241914822







