Artificial Intelligence and Assistive Robotics in Healthcare Services: Applications in Silver Care
Abstract
1. Introduction
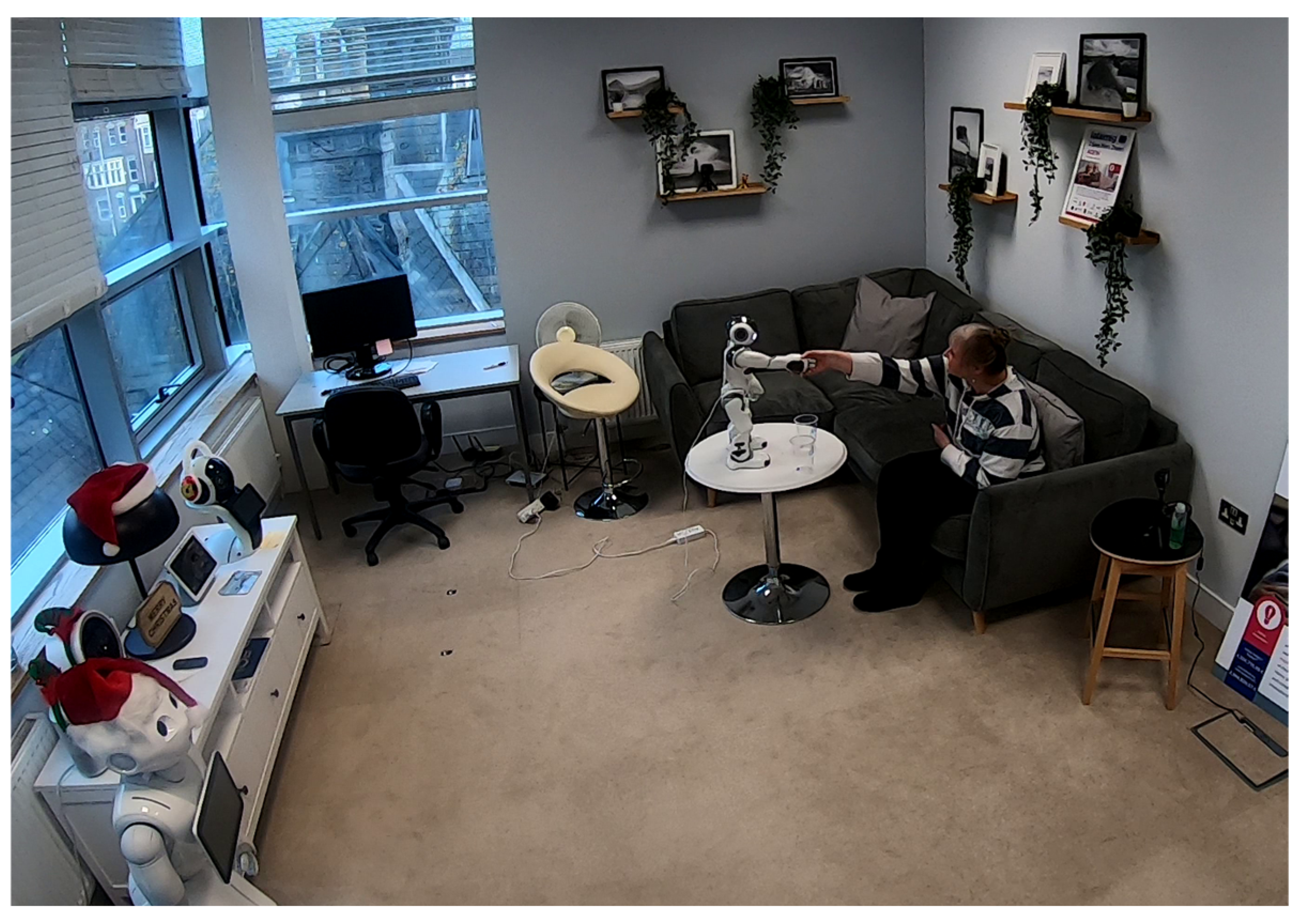
2. The Role of Artificial Intelligence in Healthcare Services
3. Robotics in Elderly Care
4. Trust in Robots for Sensitive Tasks
5. Challenges of Implementing AI and Robotics in Elderly Care
5.1. General Challenges
5.2. Ethical Considerations
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ageing and Health, World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 30 April 2025).
- Mitchell, E.; Walker, R. Global ageing: Successes, challenges and opportunities. Br. J. Hosp. Med. 2020, 81, 1–9. [Google Scholar] [CrossRef]
- Sun, X.; Li, X. Aging and chronic disease: Public health challenge and education reform. Front. Public Health 2023, 11, 1175898. [Google Scholar]
- Henry, J.D.; Coundouris, S.P.; Nangle, M.R. Breaking the links between ageism and health: An integrated perspective. Ageing Res. Rev. 2024, 95, 102212. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zeng, Y.; Wang, L.; Fang, Y. Urban–rural differences in long-term care service status and needs among home-based elderly people in China. Int. J. Environ. Res. Public Health 2020, 17, 1701. [Google Scholar] [CrossRef]
- Lindt, N.; van Berkel, J.; Mulder, B.C. Determinants of overburdening among informal carers: A systematic review. BMC Geriatr. 2020, 20, 304. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Zhang, L. Relationship between aging population, birth rate and disposable income per capita in the context of COVID-19. PLoS ONE 2023, 18, e0289781. [Google Scholar] [CrossRef]
- Padhan, S.; Mohapatra, A.; Ramasamy, S.K.; Agrawal, S.; Ramasamy, S. Artificial intelligence (AI) and robotics in elderly healthcare: Enabling independence and quality of life. Cureus 2023, 15, e42905. [Google Scholar] [CrossRef]
- Powell, A. AI Revolution in Medicine. The Harvard Gazette. 2020. Available online: https://news.harvard.edu/gazette/story/2020/11/risks-and-benefits-of-an-ai-revolution-in-medicine/ (accessed on 30 April 2025).
- Tun, S.Y.Y.; Madanian, S.; Mirza, F. Internet of things (IoT) applications for elderly care: A reflective review. Aging Clin. Exp. Res. 2021, 33, 855–867. [Google Scholar] [CrossRef]
- AI in Healthcare: Navigating the Noise. A Comprehensive Guide Supporting Healthcare Leaders to Make Sense of AI and Explore the Art of the Possible. NHS Confederation. Available online: https://www.nhsconfed.org/publications/ai-healthcare (accessed on 30 April 2025).
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef]
- Moawad, A.W.; Fuentes, D.T.; ElBanan, M.G.; Shalaby, A.S.; Guccione, J.; Kamel, S.; Jensen, C.T.; Elsayes, K.M. Artificial intelligence in diagnostic radiology: Where do we stand, challenges, and opportunities. J. Comput. Assist. Tomogr. 2022, 46, 78–90. [Google Scholar] [CrossRef]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient Intell. Humaniz. Comput. 2023, 14, 8459–8486. [Google Scholar] [CrossRef] [PubMed]
- Ranschaert, E.; Topff, L.; Pianykh, O. Optimization of radiology workflow with artificial intelligence. Radiol. Clin. 2021, 59, 955–966. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, N.; Lacson, R.; Khorasani, R. Workflow applications of artificial intelligence in radiology and an overview of available tools. J. Am. Coll. Radiol. 2020, 17, 1363–1370. [Google Scholar] [CrossRef]
- Hwang, D.K.; Hsu, C.C.; Chang, K.J.; Chao, D.; Sun, C.H.; Jheng, Y.C.; Yarmishyn, A.A.; Wu, J.-C.; Tsai, C.-Y.; Wang, M.-L.; et al. Artificial intelligence-based decision-making for age-related macular degeneration. Theranostics 2019, 9, 232. [Google Scholar] [CrossRef]
- Reddy, A.; Reddy, R.P.; Roghani, A.K.; Garcia, R.I.; Khemka, S.; Pattoor, V.; Jacob, M.; Reddy, P.H.; Sehar, U. Artificial intelligence in Parkinson’s disease: Early detection and diagnostic advancements. Ageing Res. Rev. 2024, 99, 102410. [Google Scholar] [CrossRef] [PubMed]
- Bhandarkar, A.; Naik, P.; Vakkund, K.; Junjappanavar, S.; Bakare, S.; Pattar, S. Deep learning based computer aided diagnosis of Alzheimer’s disease: A snapshot of last 5 years, gaps, and future directions. Artif. Intell. Rev. 2024, 57, 30. [Google Scholar] [CrossRef]
- Javeed, A.; Dallora, A.L.; Berglund, J.S.; Ali, A.; Ali, L.; Anderberg, P. Machine learning for dementia prediction: A systematic review and future research directions. J. Med. Syst. 2023, 47, 17. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.J.; Hsu, C.H.; Chen, L.B. A pose estimation-based fall detection methodology using artificial intelligence edge computing. IEEE Access 2021, 9, 129965–129976. [Google Scholar] [CrossRef]
- Baig, M.M.; Afifi, S.; GholamHosseini, H.; Mirza, F. A systematic review of wearable sensors and IoT-based monitoring applications for older adults–a focus on ageing population and independent living. J. Med. Syst. 2019, 43, 233. [Google Scholar] [CrossRef]
- Macalupu, V.; Miller, E.; Martin, L.; Caldwell, G. Human–robot interactions and experiences of staff and service robots in aged care. Sci. Rep. 2025, 15, 2495. [Google Scholar] [CrossRef]
- Soori, M.; Arezoo, B.; Dastres, R. Artificial intelligence, machine learning and deep learning in advanced robotics, a review. Cogn. Robot. 2023, 3, 54–70. [Google Scholar] [CrossRef]
- Boyd, A.M.; Chaffee, B.W. Critical evaluation of pharmacy automation and robotic systems: A call to action. Hosp. Pharm. 2019, 54, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Automatic Pill Dispenser Evaluations: Hands-On. Tech-Enhanced Life. Available online: https://www.techenhancedlife.com/citizen-research/automatic-pill-dispenser-evaluations (accessed on 30 April 2025).
- Alam, E.; Sufian, A.; Dutta, P.; Leo, M. Vision-based human fall detection systems using deep learning: A review. Comput. Biol. Med. 2022, 146, 105626. [Google Scholar] [CrossRef]
- Zhu, J.; Gienger, M.; Franzese, G.; Kober, J. Do you need a hand?—A bimanual robotic dressing assistance scheme. IEEE Trans. Robot. 2024, 40, 1906–1919. [Google Scholar] [CrossRef]
- Li, J.; Mo, Y.; Jiang, S.; Ma, L.; Zhang, Y.; Wei, S. Bathing assistive devices and robots for the elderly. Biomim. Intell. Robot. 2025, 5, 100218. [Google Scholar] [CrossRef]
- Sharma, A. Robotics in Elderly Care: Current Trends and Opportunities. TechRxiv 2025. submitted. [Google Scholar]
- Ceccarelli, M. Challenges in service robot devices for elderly motion assistance. Robotica 2024, 42, 4186–4199. [Google Scholar] [CrossRef]
- de Paiva, T.S.; Gonçalves, R.S.; Carbone, G.; Ceccarelli, M. Gait devices for stroke rehabilitation: State-of-the-art, challenges, and open issues. In Medical and Healthcare Robotics; Academic Press: Cambridge, MA, USA, 2023; pp. 87–122. [Google Scholar]
- Pang, Z.; Wang, T.; Wang, Z.; Yu, J.; Sun, Z.; Liu, S. Design and analysis of a wearable upper limb rehabilitation robot with characteristics of tension mechanism. Appl. Sci. 2020, 10, 2101. [Google Scholar] [CrossRef]
- Levin, G.; Brezinov, Y.; Brodeur, M.N.; Salvador, S.; Lau, S.; Gotlieb, W. Gynecologic oncology robot-assisted surgery in octogenarians: Impact of age on hospital stay. Int. J. Gynecol. Obstet. 2024, 167, 784–788. [Google Scholar] [CrossRef]
- Bradwell, H.; Edwards, K.J.; Winnington, R.; Thill, S.; Allgar, V.; Jones, R.B. Implementing affordable socially assistive pet robots in care homes before and during the COVID-19 pandemic: Stratified cluster randomized controlled trial and mixed methods study. JMIR Aging 2022, 5, e38864. [Google Scholar] [CrossRef]
- Paro. Available online: http://www.parorobots.com/ (accessed on 9 April 2025).
- JfA. Available online: https://joyforall.com/ (accessed on 9 April 2025).
- AIBO. Available online: https://robotsguide.com/search?q=aibo (accessed on 9 April 2025).
- PLEO. Available online: https://robotsguide.com/robots/pleo/ (accessed on 9 April 2025).
- Takada, M.; Ichino, J.; Hayashi, K. A study of objective evaluation indicator based on robot activity logs for owner attachment to companion robot. Int. J. Soc. Robot. 2024, 16, 125–143. [Google Scholar] [CrossRef]
- Nishio, T.; Yoshikawa, Y.; Sakai, K.; Iio, T.; Chiba, M.; Asami, T.; Isoda, Y.; Ishiguro, H. The effects of physically embodied multiple conversation robots on the elderly. Front. Robot. AI 2021, 8, 633045. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, J.; Uğuralp, A.K.; Uğuralp, Z.; Puntoni, S. AI companions reduce loneliness. arXiv 2024, arXiv:2407.19096. [Google Scholar] [CrossRef]
- Yu, C.; Sommerlad, A.; Sakure, L.; Livingston, G. Socially assistive robots for people with dementia: Systematic review and meta-analysis of feasibility, acceptability and the effect on cognition, neuropsychiatric symptoms and quality of life. Ageing Res. Rev. 2022, 78, 101633. [Google Scholar] [CrossRef]
- Pepper. Available online: https://aldebaran.com/en/pepper/ (accessed on 10 April 2025).
- NAO6. Available online: https://aldebaran.com/en/nao6/ (accessed on 10 April 2025).
- Companion Robot Helping Patients with Alzheimer’s. Available online: https://impact.du.edu/spotlight/designing-developing-knowledge-12/ (accessed on 10 April 2025).
- ElliQ. Your AI Sidekick for Happier, Healthier Aging. Available online: https://elliq.com/pages/features (accessed on 10 April 2025).
- Buddy. The First Affordable Robot Powered by Emotional AI! Available online: https://www.bluefrogrobotics.com/buddy-en (accessed on 10 April 2025).
- iPal. Available online: https://www.ipalrobot.com/ (accessed on 10 April 2025).
- Care-O-Bot 4. Available online: https://www.care-o-bot.de/en/care-o-bot-4.html (accessed on 10 April 2025).
- Figliano, G.; Manzi, F.; Tacci, A.L.; Marchetti, A.; Massaro, D. Ageing society and the challenge for social robotics: A systematic review of socially assistive robotics for mci patients. PLoS ONE 2023, 18, e0293324. [Google Scholar] [CrossRef] [PubMed]
- Niewiadomski, R.; Bruijnes, M.; Huisman, G.; Gallagher, C.P.; Mancini, M. Social robots as eating companions. Front. Comput. Sci. 2022, 4, 909844. [Google Scholar] [CrossRef]
- Arioz, U.; Bratina, B.; Mlakar, I.; Plohl, N.; Uran, S.; Roj, I.R.; Šafarič, R.; Šafran, V. Unlocking the power of socially assistive robotic nurses in hospitals through innovative living lab methodology. Health Inform. J. 2024, 30, 14604582241291380. [Google Scholar] [CrossRef]
- Kok, B.C.; Soh, H. Trust in robots: Challenges and opportunities. Curr. Robot. Rep. 2020, 1, 297–309. [Google Scholar] [CrossRef]
- Giorgi, I.; Tirotto, F.A.; Hagen, O.; Aider, F.; Gianni, M.; Palomino, M.; Masala, G.L. Friendly but faulty: A pilot study on the perceived trust of older adults in a social robot. IEEE Access 2022, 10, 92084–92096. [Google Scholar] [CrossRef]
- Giorgi, I.; Minutolo, A.; Tirotto, F.; Hagen, O.; Esposito, M.; Gianni, M.; Palomino, M.; Masala, G.L. I am robot, your health adviser for older adults: Do you trust my advice? Int. J. Soc. Robot. 2023, 1–20. [Google Scholar] [CrossRef]
- Worth, T. Are Robots the Solution to the Crisis in Older-Person Care? Nature 2024. Available online: https://www.nature.com/articles/d41586-024-01184-4 (accessed on 30 April 2025). [CrossRef] [PubMed]
- Wong, K.L.Y.; Hung, L.; Wong, J.; Park, J.; Alfares, H.; Zhao, Y.; Mousavinejad, A.; Soni, A.; Zhao, H. Adoption of artificial intelligence–enabled robots in long-term care homes by health care providers: Scoping review. JMIR Aging 2024, 7, e55257. [Google Scholar] [CrossRef]
- Chan, H.Y.; Muralidharan, A. Care robots for the elderly: Legal, ethical considerations and regulatory strategies. In Developments in Intellectual Property Strategy: The Impact of Artificial Intelligence, Robotics and New Technologies; Springer International Publishing: Cham, Switzerland, 2024; pp. 129–156. [Google Scholar]
- Yuan, S.; Coghlan, S.; Lederman, R.; Waycott, J. Social robots in aged care: Care staff experiences and perspectives on robot benefits and challenges. Proc. ACM Hum.-Comput. Interact. 2022, 6, 1–23. [Google Scholar] [CrossRef]
- Melkas, H.; Hennala, L.; Pekkarinen, S.; Kyrki, V. Impacts of robot implementation on care personnel and clients in elderly-care institutions. Int. J. Med. Inform. 2020, 134, 104041. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, I.; Koulouglioti, C.; Lazzarino, R.; Ali, S.; Wright, S.; Martín-García, Á.; Oter-Quintana, C.; Kouta, C.; Rousou, E.; Papp, K.; et al. Views about perceived training needs of health care professionals in relation to socially assistive robots: An international online survey. Contemp. Nurse 2023, 59, 344–361. [Google Scholar] [CrossRef]
- Elsheikh, A.; Al-Thani, D.A. Exploring the acceptance and adoption of humanoid robots among older adults: Systematic review. In IFIP Conference on Human-Computer Interaction; Springer Nature: Cham, Switzerland, 2023; pp. 257–266. [Google Scholar]
- Rubeis, G.; Fang, M.L.; Sixsmith, A. Equity in AgeTech for ageing well in technology-driven places: The role of social determinants in designing AI-based assistive technologies. Sci. Eng. Ethics 2022, 28, 49. [Google Scholar] [CrossRef]
- Sahoo, L.; Miazi, N.S.; Shehab, M.; Alt, F.; Abdelrahman, Y. You know too much: Investigating users’ perceptions and privacy concerns towards thermal imaging. In Privacy Symposium: Data Protection Law International Convergence and Compliance with Innovative Technologies; Springer International Publishing: Cham, Switzerland, 2022; pp. 207–229. [Google Scholar]
- Zhang, K.; Meng, X.; Yan, X.; Ji, J.; Liu, J.; Xu, H.; Zhang, H.; Liu, D.; Wang, J.; Wang, X.; et al. Revolutionizing health care: The transformative impact of large language models in medicine. J. Med. Internet Res. 2025, 27, e59069. [Google Scholar] [CrossRef]
- Torresen, J.; Saplacan, D.; Baselizadeh, A.; Mahler, T. Machine excellence tradeoffs to ethical and legal perspectives. In Proceedings of the 2023 IEEE Conference on Artificial Intelligence (CAI), Santa Clara, CA, USA, 5–6 June 2023; pp. 237–240. [Google Scholar]
- van der Gun, L.; Guest, O. Artificial Intelligence: Panacea or Non-Intentional Dehumanisation? J. Hum.-Technol. Relat. 2024, 2. [Google Scholar] [CrossRef]
- Wiczorek, R. Human-Centered Design of AI in Healthcare and the Role of Older Patients. In Advances in Intelligent Healthcare Delivery and Management: Research Papers in Honour of Professor Maria Virvou for Invaluable Contributions; Springer Nature: Cham, Switzerland, 2024; pp. 37–47. [Google Scholar]
- Salles, A.; Evers, K.; Farisco, M. Anthropomorphism in AI. AJOB Neurosci. 2020, 11, 88–95. [Google Scholar] [CrossRef]
- The EU Artificial Intelligence Act. Up-to-Date Developments and Analyses of the EU AI Act. Available online: https://artificialintelligenceact.eu/ (accessed on 30 April 2025).
- AI Act. European Commission. Available online: https://digital-strategy.ec.europa.eu/en/policies/regulatory-framework-ai (accessed on 30 April 2025).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masala, G.L.; Giorgi, I. Artificial Intelligence and Assistive Robotics in Healthcare Services: Applications in Silver Care. Int. J. Environ. Res. Public Health 2025, 22, 781. https://doi.org/10.3390/ijerph22050781
Masala GL, Giorgi I. Artificial Intelligence and Assistive Robotics in Healthcare Services: Applications in Silver Care. International Journal of Environmental Research and Public Health. 2025; 22(5):781. https://doi.org/10.3390/ijerph22050781
Chicago/Turabian StyleMasala, Giovanni Luca, and Ioanna Giorgi. 2025. "Artificial Intelligence and Assistive Robotics in Healthcare Services: Applications in Silver Care" International Journal of Environmental Research and Public Health 22, no. 5: 781. https://doi.org/10.3390/ijerph22050781
APA StyleMasala, G. L., & Giorgi, I. (2025). Artificial Intelligence and Assistive Robotics in Healthcare Services: Applications in Silver Care. International Journal of Environmental Research and Public Health, 22(5), 781. https://doi.org/10.3390/ijerph22050781







