Media Exposure and Substance Use Increase during COVID-19
Abstract
1. Introduction
2. Materials and Methods
2.1. Measures
2.2. Analysis
3. Results
4. Discussion
Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Holland, K.M.; Jones, C.; Vivolo-Kantor, A.M.; Idaikkadar, N.; Zwald, M.; Hoots, B.; Yard, E.; D’Inverno, A.; Swedo, E.; Chen, M.S.; et al. Trends in US Emergency Department Visits for Mental Health, Overdose, and Violence Outcomes Before and During the COVID-19 Pandemic. JAMA Psychiatry 2021, 78, 372–379. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Pan, K.-Y.; Kok, A.A.L.; Eikelenboom, M.; Horsfall, M.; Jörg, F.; Luteijn, R.A.; Rhebergen, D.; van Oppen, P.; Giltay, E.J.; Penninx, B.W.J.H. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 2021, 8, 121–129. [Google Scholar] [CrossRef]
- Riehm, K.E.; Holingue, C.; Kalb, L.G.; Bennett, D.; Kapteyn, A.; Jiang, Q.; Veldhuis, C.B.; Johnson, R.M.; Fallin, M.D.; Kreuter, F.; et al. Associations Between Media Exposure and Mental Distress Among U.S. Adults at the Beginning of the COVID-19 Pandemic. Am. J. Prev. Med. 2020, 59, 630–638. [Google Scholar] [CrossRef]
- Sasaki, N.; Kuroda, R.; Tsuno, K.; Kawakami, N. Exposure to media and fear and worry about COVID -19. Psychiatry Clin. Neurosci. 2020, 74, 501–502. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Holman, E.A.; Garfin, D.R.; Silver, R.C. Media’s role in broadcasting acute stress following the Boston Marathon bombings. Proc. Natl. Acad. Sci. USA 2014, 111, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Primack, B.A.; Kraemer, K.L.; Fine, M.J.; Dalton, M.A. Media Exposure and Marijuana and Alcohol Use Among Adolescents. Subst. Use Misuse 2009, 44, 722–739. [Google Scholar] [CrossRef] [PubMed]
- Chiou, C.-P.; Chung, Y.-C. Effectiveness of multimedia interactive patient education on knowledge, uncertainty and decision-making in patients with end-stage renal disease. J. Clin. Nurs. 2011, 21, 1223–1231. [Google Scholar] [CrossRef] [PubMed]
- Newhagen, J.E. TV news images that induce anger, fear, and disgust: Effects on approach-avoidance and memory. J. Broadcast. Electron. Media 1998, 42, 265–276. [Google Scholar] [CrossRef]
- Sindermann, C.; Elhai, J.D.; Moshagen, M.; Montag, C. Age, gender, personality, ideological attitudes and individual differences in a person’s news spectrum: How many and who might be prone to “filter bubbles” and “echo chambers” online? Heliyon 2020, 6, e03214. [Google Scholar] [CrossRef]
- Ahern, J.; Galea, S.; Resnick, H.; Kilpatrick, D.; Bucuvalas, M.; Gold, J.; Vlahov, D. Television Images and Psychological Symptoms after the September 11 Terrorist Attacks. Psychiatry 2002, 65, 289–300. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; Newman, E.; Nelson, S.D.; Nitiéma, P.; Pfefferbaum, R.L.; Rahman, A. Disaster Media Coverage and Psychological Outcomes: Descriptive Findings in the Extant Research. Curr. Psychiatry Rep. 2014, 16, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ochalek, T.A.; Cumpston, K.L.; Wills, B.K.; Gal, T.S.; Moeller, F.G. Nonfatal Opioid Overdoses at an Urban Emergency Department During the COVID-19 Pandemic. JAMA 2020, 324, 1673. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Prescription Opioid Abuse and Misuse Issues: FDA Briefing for Stakeholders. 2014. Available online: http://www.fda.gov/NewsEvents/Speeches/ucm391767.htm (accessed on 5 November 2016).
- Volkow, N.D.; Frieden, T.; Hyde, P.S.; Cha, S.S. Medication-Assisted Therapies—Tackling the Opioid-Overdose Epidemic. N. Engl. J. Med. 2014, 370, 2063–2066. [Google Scholar] [CrossRef]
- Lee, E.S.; Forthofer, R.N. Analyzing Complex Survey Data, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2006. [Google Scholar]
- United States Census Bureau. State Population Totals and Components of Change: 2010–2019; United States Census Bureau: Houtland, MD, USA, 2019.
- Fiske, A.; Wetherell, J.L.; Gatz, M. Depression in Older Adults. Annu. Rev. Clin. Psychol. 2009, 5, 363–389. [Google Scholar] [CrossRef]
- Mitchell, A.; Jurkowitz, M.; Oliphant, J.; Shearer, E. Americans Who Mainly Get Their News on Social Media are Less Engaged, Less Knowledgeable; Pew Research Center: Washington, DC, USA, 2020. [Google Scholar]
- Ali, S.H.; Foreman, J.; Tozan, Y.; Capasso, A.; Jones, A.M.; DiClemente, R.J. Trends and Predictors of COVID-19 Information Sources and Their Relationship with Knowledge and Beliefs Related to the Pandemic: Nationwide Cross-Sectional Study. JMIR Public Heal Surveill. 2020, 6, e21071. [Google Scholar] [CrossRef]
- Lai, H.M.X.; Cleary, M.; Sitharthan, T.; Hunt, G.E. Prevalence of comorbid substance use, anxiety and mood disorders in epidemi-ological surveys, 1990–2014: A systematic review and meta-analysis. Drug Alcohol Depend. 2015, 154, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, P.A.; Montemitro, C.; Leggio, L. New Challenges in Addiction Medicine: COVID-19 Infection in Patients with Alcohol and Substance Use Disorders—The Perfect Storm. Am. J. Psychiatry 2020, 177, 805–807. [Google Scholar] [CrossRef]
- Koob, G.F.; Schulkin, J. Addiction and stress: An allostatic view. Neurosci. Biobehav. Rev. 2019, 106, 245–262. [Google Scholar] [CrossRef] [PubMed]
- Reece, A.S. Clinical implications of addiction related immunosuppression. J. Infect. 2008, 56, 437–445. [Google Scholar] [CrossRef] [PubMed]
| Please indicate if it is TRUE or FALSE, for each of the following statements about the COVID-19 virus: |
| 1. Antibiotics can be used to treat the COVID-19 virus |
| 2. People of all ages can become infected with COVID-19 |
| 3. People of all racial and ethnic groups can become infected with the COVID-19 |
| 4. Eating garlic can lower your chances of getting infected with the COVID-19 virus. |
| 5. Most people who are infected with the COVID-19 virus die from it. |
| 6. Most people who are infected with the COVID-19 virus recover from it. |
| 7. Older adults or those with compromised immune systems are at a higher risk. |
| Substance Use Increase during COVID-19 | ||||
|---|---|---|---|---|
| Characteristics | N = 1213 (100%) | No Increase = 1016 (83.8%) | Increase = 197 (16.2%) | p Value |
| Age Group | - | |||
| 18–39 | 616 (51.0) | 511 (83) | 105 (17) | <0.001 |
| 40–59 | 360 (29.7) | 283 (78.6) | 77 (21.4) | |
| 60 and over | 234 (19.3) | 219 (93.6) | 15 (6.4) | |
| NA | 3 (0.2) | 3 (0.3) | 0 (0.0) | |
| Gender | ||||
| Female | 604 (49.8) | 520 (86.1) | 84 (13.9) | 0.034 |
| Male | 592 (48.8) | 483 (81.6) | 109 (18.4) | |
| NA | 17 (1.4) | 13 (1.2) | 4 (2.0) | |
| Race | ||||
| White | 772 (63.3) | 654 (84.7) | 118 (15.3) | 0.232 |
| Non-White | 441 (36.4) | 362 (82.1) | 79 (17.9) | |
| NA | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Education Level | ||||
| High School Diploma or less | 265 (21.8) | 227 (85.7) | 38 (14.3) | 0.074 |
| Higher Education | 911 (75.1) | 753 (82.7) | 158 (17.3) | |
| NA | 37 (3.0) | 36 (3.5) | 1 (0.5) | |
| Rurality | ||||
| Urban | 919 (76.3) | 756 (82.3) | 163 (17.7) | 0.052 |
| Large rural | 63 (5.1) | 53 (84.1) | 10 (15.9) | |
| Small rural | 204 (16.5) | 184 (90.2) | 20 (9.8) | |
| Isolated | 23 (1.8) | 19 (82.6) | 4 (17.4) | |
| NA | 4 (0.3) | 4 (0.4) | 0 (0.0) | |
| Income | ||||
| <$49,999 | 300 (24.7) | 254 (84.7) | 46 (15.3) | <0.001 |
| $49,999–$74,999 | 466 (38.4) | 416 (89.3) | 50 (10.7) | |
| >$75,000 | 442 (36.4) | 341 (77.1) | 101 (22.9) | |
| NA | 5 (0.4) | 5 (0.5) | 0 (0.0) | |
| Political Orientation | ||||
| Liberal | 475 (39.2) | 402 (84.6) | 73 (15.4) | 0.012 |
| Moderate | 224 (18.5) | 198 (88.4) | 26 (11.6) | |
| Conservative | 435 (35.9) | 347 (79.8) | 88 (20.2) | |
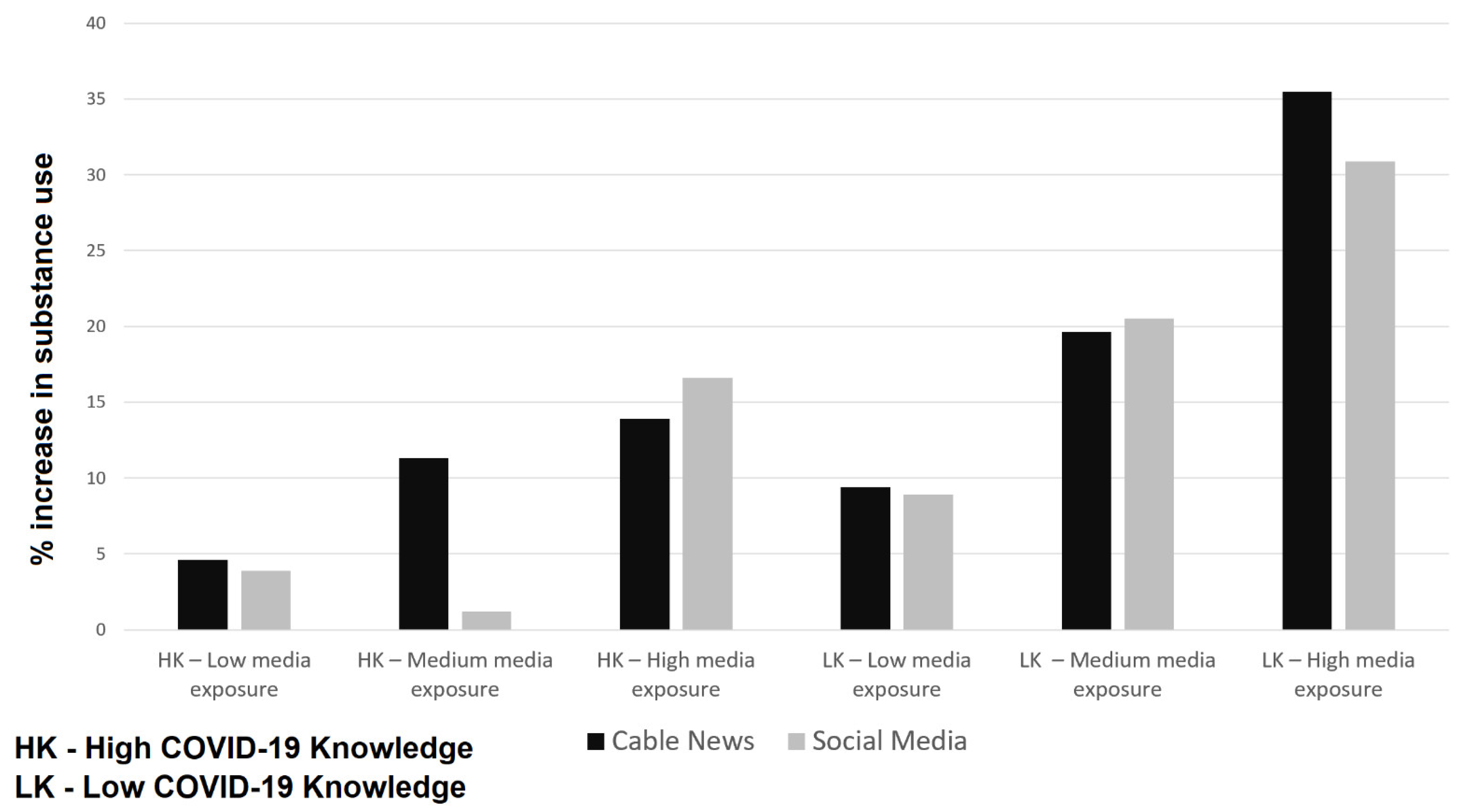
| COVID-19 Knowledge—Cable News Consumption | ||||
| LK–LCC | 106 (8.7) | 96 (90.6) | 10 (9.4) | <0.001 |
| LK–MCC | 168 (13.8) | 135 (80.4) | 33 (19.6) | |
| LK–HCC | 197 (16.2) | 127 (64.5) | 70 (35.5) | |
| HK–LCC | 152 (12.5) | 145 (95.4) | 7 (4.6) | |
| HK–MCC | 265 (21.8) | 235 (88.7) | 30 (11.3) | |
| HK–HCC | 323 (26.2) | 278 (86.1) | 45 (13.9) | |
| NA | 2 (0.1) | 0 (0.0) | 2 (1.0) | |
| COVID-19 Knowledge—Social Media Consumption | ||||
| LK–LSMC | 90 (7.4) | 82 (91.1) | 8 (8.9) | <0.001 |
| LK–MSMC | 112 (9.2) | 89 (79.5) | 23 (20.5) | |
| LK–HSMC | 269 (22.2) | 186 (69.1) | 83 (30.9) | |
| HK–LSMC | 257 (21.2) | 247 (96.1) | 10 (3.9) | |
| HK–MSMC | 170 (14.0) | 149 (98.8) | 21 (1.2) | |
| HK–HSMC | 314 (25.9) | 262 (83.4) | 52 (16.6) | |
| NA | 1 (0.0) | 1 (0.0) | 0 (0.0) | |
| Variable | Unadjusted | Adjusted | |
|---|---|---|---|
| OR | Cable News | Social Media | |
| (95% CI) | OR (95% CI) | OR (95% CI) | |
| COVID-19 Knowledge—Cable News Consumption | |||
| HK–LCC (Ref) | - | - | - |
| HK–MCC | 2.64 (1.19–6.69) ** | 3.42 (1.16–7.44) * | - |
| HK–HCC | 3.35 (1.56–8.30) ** | 4.56 (1.66–10.15) ** | - |
| LK–LCC | 2.15 (0.80–6.12) | 2.94 (0.93–8.29) | - |
| LK–MCC | 5.06 (2.29–12.82) *** | 5.77 (2.06–13.49) ** | - |
| LK–HCC | 11.41 (5.40–28.11) *** | 11.64 (4.01–24.45) *** | - |
| COVID-19 Knowledge—Social Media Consumption | |||
| HK–LSMC (Ref) | - | - | - |
| HK–MSMC | 3.48 (1.63–7.90) ** | - | 2.93 (1.25–7.48) * |
| HK–HSMC | 4.90 (2.54–10.43) *** | - | 4.85 (2.31–11.4) ** |
| LK–LSMC | 2.40 (0.89–6.31) * | - | 2.65 (0.82–7.31) |
| LK–MSMC | 6.38 (2.99–14.53) *** | - | 5.56 (2.21–13.81) *** |
| LK–HSMC | 11.02 (5.82–23.16) *** | - | 9.91 (4.71–23.61) *** |
| Political Orientation | |||
| Liberal (Ref) | - | - | - |
| Moderate | 0.76 (0.45–1.26) | 0.75 (0.44–1.25) | 0.69 (0.40–1.14) |
| Conservative | 1.32 (0.90–1. 94) | 1.18 (0.80–1.74) | 1.21 (0.82–1.78) |
| Age Group | |||
| 18–39 (Ref) | - | - | |
| 40–59 | 1.33 (0.91–1.31) | 1.49 (1.02–2.1) ** | 1.68 (1.15–2.47) * |
| 60 and over | 0.33 (0.18–0.57) *** | 0.51 (0.27–0.93) ** | 0.78 (0.40–1.42) |
| Gender | - | ||
| Female (Ref) | - | - | - |
| Male | 1.39 (1.02–1.90) * | 1.46 (0.99–2.15) | 1.49 (1.02–2.19) * |
| Race | - | ||
| Non-White (Ref) | - | - | |
| White | 0.82 (0.60–1.13) | 0.85 (0.58–1.27) | 0.90 (0.60–1.34) |
| Rurality | |||
| Isolated (Ref) | - | - | |
| Large rural | 0.89 (0.26–3.57) | 1.02 (0.23–5.51) | 1.24 (0.30–6.45) |
| Small rural | 0.51 (0.17–1.91) | 0.47 (0.12–2.37) | 0.57 (0.15–2.76) |
| Urban | 1.02 (0.37–3.56) | 0.99 (0.28–4.67) | 1.17 (0.35–3.56) |
| Income | |||
| <$49,999 (Ref) | - | - | |
| $49,999–$74,999 | 0.66 (0.43–1.02) * | 0.79 (0.49–1.30) | 0.75 (0.46–1.23) |
| >$75,000 | 1.63 (1.11–2.41) ** | 1.31 (0.81–2.14) | 1.27 (0.79–2.08) |
| Education Level | |||
| Higher Education (Ref) | - | - | |
| High School Diploma or less | 0.70 (0.47–1.02) * | 0.90 (0.56–1.42) | 0.85 (0.53–1.32) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amram, O.; Borah, P.; Kubsad, D.; McPherson, S.M. Media Exposure and Substance Use Increase during COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 6318. https://doi.org/10.3390/ijerph18126318
Amram O, Borah P, Kubsad D, McPherson SM. Media Exposure and Substance Use Increase during COVID-19. International Journal of Environmental Research and Public Health. 2021; 18(12):6318. https://doi.org/10.3390/ijerph18126318
Chicago/Turabian StyleAmram, Ofer, Porismita Borah, Deepika Kubsad, and Sterling M. McPherson. 2021. "Media Exposure and Substance Use Increase during COVID-19" International Journal of Environmental Research and Public Health 18, no. 12: 6318. https://doi.org/10.3390/ijerph18126318
APA StyleAmram, O., Borah, P., Kubsad, D., & McPherson, S. M. (2021). Media Exposure and Substance Use Increase during COVID-19. International Journal of Environmental Research and Public Health, 18(12), 6318. https://doi.org/10.3390/ijerph18126318







