Routine Health Information Systems in the European Context: A Systematic Review of Systematic Reviews
Abstract
1. Introduction
2. Materials and Methods
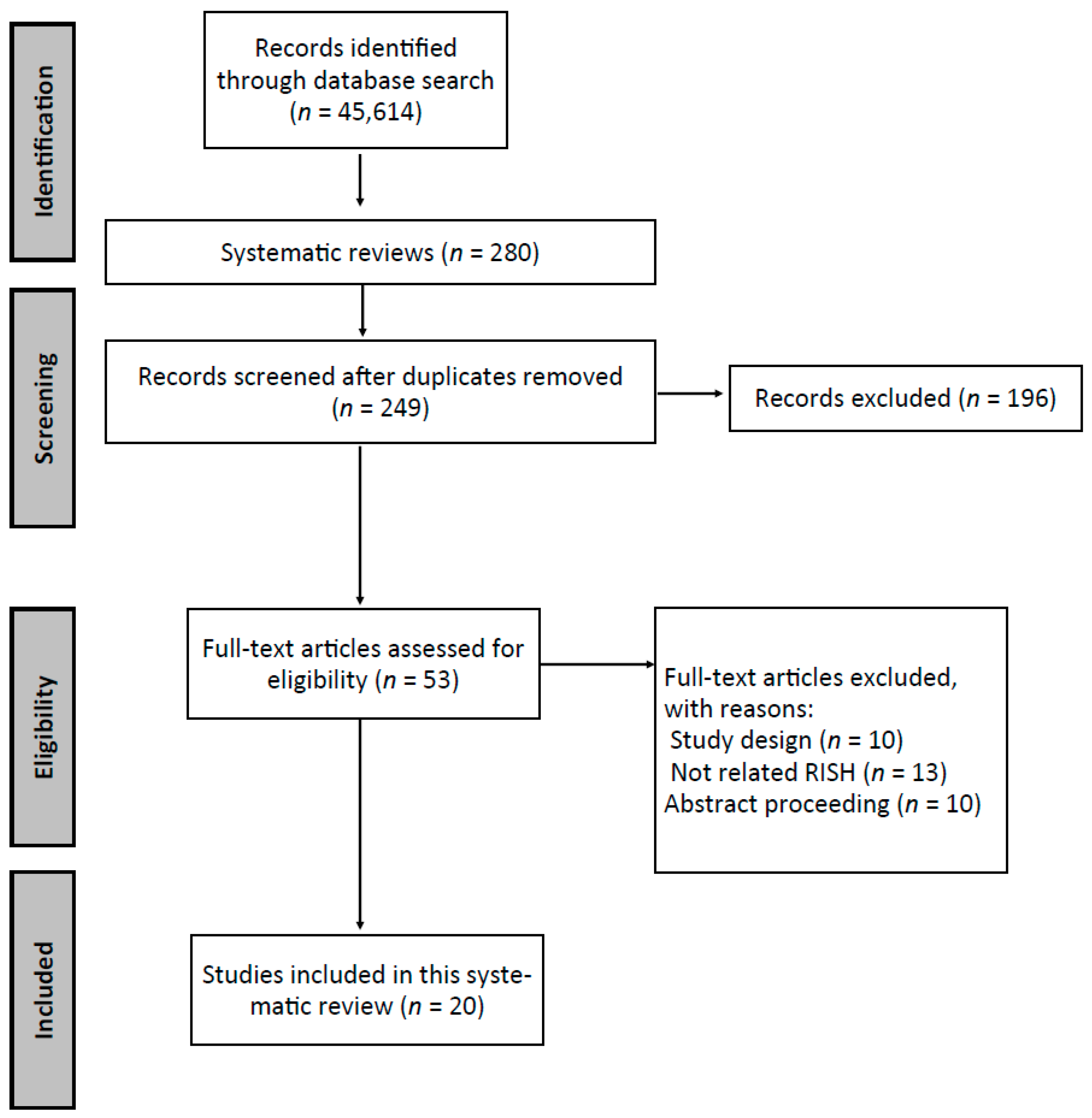
2.1. Search Strategy and Inclusion Criteria
2.2. Study Selection
2.3. Data Extraction and Quality Assessment
3. Results
3.1. Descriptive Analysis of the Systematic Reviews
3.1.1. General Characteristics of Reviewed Papers
3.1.2. Aims
3.1.3. Intervention
3.2. Outcomes
3.3. Areas for Improvement for RHISs According to the PRISM Framework
4. Discussion
- Based on an intervention in the HIS, a set of technological, organizational, and behavioral drivers and barriers arise;
- The interaction between the intervention and the drivers and barriers generates RHIS inputs, i.e., the data that will be used. To achieve this, the data’s needs, production, availability, and use requirements must be precisely defined;
- Once the data have been generated, they are transformed into RHIS outputs, to the extent that they can generate high-quality health information, and then that health information is used effectively for decision making;
- Once health information has been generated and used effectively, the RHIS is ready to generate outcomes, i.e., the results of its implementation. In general, these results refer to the effectiveness of either the information system itself or the health system in general. The ultimate intention is to improve citizens’ health statuses.
4.1. Inputs
4.2. Outputs
4.3. Outcomes
4.4. Efficiency of RHISs in the Prevention/Treatment of COVID-19 Transmission
4.5. Policy Implications
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| AIDS | Acquired Immunodeficiency Syndrome |
| AMSTAR | A Measurement Tool to Assess Systematic Reviews |
| CAAS | Computerized Antimicrobial Approval Systems |
| CDSS | Clinical Decision Support System |
| CIS | Clinical Information System |
| CPOE | Computerized Provider Order Entry |
| DOI | Theory of Diffusion of Innovations |
| D-RHIS | Disease-specific RHIS |
| DSO | Data Scientists Office |
| EHII | European Health Information Initiative |
| EHR | Electronic Health Records |
| EMR | Electronic Medical Records |
| GP | General Practitioner |
| HCH | Home-based Consumer Health |
| HCI | Human–computer Interaction |
| HIE | Health Information Exchange |
| HIS | Health Information System |
| HIT | Health Information Technology |
| HIV | Human Immunodeficiency Virus |
| HSH | Health Smart Homes |
| ICT | Information and Communications Technology |
| INR | International Normalized Ratio (prothrombin time) |
| I-RHIS | Integrated RHIS |
| IT | Information Technology |
| LTC | Long-Term Care |
| PHR | Personal Health records |
| PRISM | Performance of Routine Information System Management |
| RHIO | Regional Health Information Organizations |
| RHIS | Routine Health Information System, Regional Health Information System |
| SS | Surveillance Systems |
| TOE | Theory of Organization and Environment |
| TPB | Theory of Planned Behaviour |
| UTAUT | Unified Theory of Acceptance and Use of Technology |
| WHO | World Health Organization |
References
- WHO. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Health Metrics Network & World Health Organization. Framework and Standards for Country Health Information Systems, 2nd ed. 2008. Available online: https://apps.who.int/iris/handle/10665/43872 (accessed on 9 April 2021).
- Dixon-Woods, M.; Redwood, S.; Leslie, M.; Minion, J.; Martin, G.P.; Coleman, J.J. Improving Quality and Safety of Care Using “Technovigilance”: An Ethnographic Case Study of Secondary Use of Data from an Electronic Prescribing and Decision Support System. Milbank Q. 2013, 91, 424–454. [Google Scholar] [CrossRef]
- Riley, P.L.; Zuber, A.; Vindigni, S.M.; Gupta, N.; Verani, A.R.; Sunderland, N.L.; Friedman, M.; Zurn, P.; Okoro, C.; Patrick, H.; et al. Information systems on human resources for health: A global review. Hum. Resour. Health 2012, 10, 7. [Google Scholar] [CrossRef]
- Willis, C.D.; Riley, B.L.; Herbert, C.P.; Best, A. Networks to Strengthen Health Systems for Chronic Disease Prevention. Am. J. Public Health 2013, 103, e39–e48. [Google Scholar] [CrossRef]
- Chaudhry, B.; Wang, J.; Wu, S.; Maglione, M.; Mojica, W.; Roth, E.; Morton, S.C.; Shekelle, P.G. Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care. Ann. Intern. Med. 2006, 144, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Lippeveld, T.; Sauerborn, R.; Bodart, C.; World Health Organization (Eds.) Design and Implementation of Health Information Systems; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- European Health Report 2018: More than Numbers—Evidence for All. Highlights 2018. Available online: https://www.euro.who.int/__data/assets/pdf_file/0003/380478/HEALTH_REPORT_HIGHLIGHTS_2018_EN.PDF (accessed on 13 April 2021).
- Hotchkiss, D.R.; Diana, M.L.; Foreit, K.G.F. How Can Routine Health Information Systems Improve Health Systems Functioning in Lowand Middle-Income Countries? Assessing the Evidence Base; Emerald Group Publishing Ltd.: Bingley, UK, 2012. [Google Scholar] [CrossRef]
- Arah, O.A.; Klazinga, N.S.; Delnoij, D.M.J.; Asbroek, A.H.A.T.; Custers, T. Conceptual frameworks for health systems performance: A quest for effectiveness, quality, and improvement. Int. J. Qual. Health Care 2003, 15, 377–398. [Google Scholar] [CrossRef]
- Lippeveld, T.; Sauerborn, R.; Sapirie, S. Health information systems—Making them work. World Health Forum. 1997, 18, 176–184. [Google Scholar]
- Aqil, A.; Lippeveld, T.; Hozumi, D. PRISM framework: A paradigm shift for designing, strengthening and evaluating routine health information systems. Health Policy Plan. 2009, 24, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Hotchkiss, D.R.; Aqil, A.; Lippeveld, T.; Mukooyo, E. Evaluation of the Performance of Routine Information System Management (PRISM) framework: Evidence from Uganda. BMC Health Serv. Res. 2010, 10, 188. [Google Scholar] [CrossRef]
- Sligo, J.; Gauld, R.; Roberts, V.; Villa, L. A literature review for large-scale health information system project planning, implementation and evaluation. Int. J. Med. Inform. 2017, 97, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Tursunbayeva, A.; Bunduchi, R.; Franco, M.; Pagliari, C. Human resource information systems in health care: A systematic evidence review. J. Am. Med. Inform. Assoc. 2017, 24, 633–654. [Google Scholar] [CrossRef] [PubMed]
- Aung, E.; Whittaker, M. Preparing routine health information systems for immediate health responses to disasters. Health Policy Plan. 2012, 28, 495–507. [Google Scholar] [CrossRef] [PubMed]
- Cawthon, C.; Mion, L.C.; Willens, D.E.; Roumie, C.L.; Kripalani, S. Implementing routine health literacy assessment in hospital and primary care patients. Jt. Comm. J. Qual. Patient Saf. 2014, 40, 68–76. [Google Scholar] [CrossRef]
- Cheng, C.K.; Ip, D.K.; Cowling, B.J.; Ho, L.M.; Leung, G.M.; Lau, E.H.; Uglow, D.; Timpka, T. Digital Dashboard Design Using Multiple Data Streams for Disease Surveillance With Influenza Surveillance as an Example. J. Med. Internet Res. 2011, 13, e85. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G.; Powell, J.; Englesakis, M.; Rizo, C.; Stern, A. Health related virtual communities and electronic support groups: Systematic review of the effects of online peer to peer interactions. BMJ 2004, 328, 1166. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare inter-ventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Anker, A.E.; Reinhart, A.M.; Feeley, T.H. Health information seeking: A review of measures and methods. Patient Educ. Couns. 2011, 82, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Marschollek, M.; Mix, S.; Wolf, K.-H.; Effertz, B.; Haux, R.; Steinhagen-Thiessen, E. ICT-based health information services for elderly people: Past experiences, current trends, and future strategies. Med. Inform. Internet Med. 2007, 32, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Bayoumi, I.; Al Balas, M.; Handler, S.M.; Dolovich, L.; Hutchison, B.; Holbrook, A. The effectiveness of computerized drug-lab alerts: A systematic review and meta-analysis. Int. J. Med. Inform. 2014, 83, 406–415. [Google Scholar] [CrossRef]
- Baysari, M.T.; Lehnbom, E.C.; Li, L.; Hargreaves, A.; Day, R.O.; Westbrook, J.I. The effectiveness of information technology to improve antimicrobial prescribing in hospitals: A systematic review and meta-analysis. Int. J. Med. Inform. 2016, 92, 15–34. [Google Scholar] [CrossRef]
- Eden, K.B.; Totten, A.M.; Kassakian, S.Z.; Gorman, P.N.; McDonagh, M.S.; Devine, B.; Pappas, M.; Daeges, M.; Woods, S.; Hersh, W.R. Barriers and facilitators to exchanging health information: A systematic review. Int. J. Med. Inform. 2016, 88, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Medic, G.; Kließ, M.K.; Atallah, L.; Weichert, J.; Panda, S.; Postma, M.; El-Kerdi, A. Evidence-based Clinical Decision Support Systems for the prediction and detection of three disease states in critical care: A systematic literature review. F1000Research 2019, 8, 1728. [Google Scholar] [CrossRef]
- Wisner, K.; Lyndon, A.; Chesla, C.A. The electronic health record’s impact on nurses’ cognitive work: An integrative review. Int. J. Nurs. Stud. 2019, 94, 74–84. [Google Scholar] [CrossRef]
- Gentil, M.-L.; Cuggia, M.; Fiquet, L.; Hagenbourger, C.; Le Berre, T.; Banâtre, A.; Renault, E.; Bouzille, G.; Chapron, A. Factors influencing the development of primary care data collection projects from electronic health records: A systematic review of the literature. BMC Med. Inform. Decis. Mak. 2017, 17, 139. [Google Scholar] [CrossRef]
- Arditi, C.; Rège-Walther, M.; Durieux, P.; Burnand, B. Computer-generated reminders delivered on paper to healthcare professionals: Effects on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2017, 2017, CD001175. [Google Scholar] [CrossRef]
- Mahmoudi, E.; Kamdar, N.; Kim, N.; Gonzales, G.; Singh, K.; Waljee, A.K. Use of electronic medical records in development and validation of risk prediction models of hospital readmission: Systematic review. BMJ 2020, 369, m958. [Google Scholar] [CrossRef]
- Ingebrigtsen, T.; Georgiou, A.; Clay-Williams, R.; Magrabi, F.; Hordern, A.; Prgomet, M.; Li, J.; Westbrook, J.; Braithwaite, J. The impact of clinical leadership on health information technology adoption: Systematic review. Int. J. Med. Inform. 2014, 83, 393–405. [Google Scholar] [CrossRef] [PubMed]
- Reeder, B.; Meyer, E.; Lazar, A.; Chaudhuri, S.; Thompson, H.J.; Demiris, G. Framing the evidence for health smart homes and home-based consumer health technologies as a public health intervention for independent aging: A systematic review. Int. J. Med. Inform. 2013, 82, 565–579. [Google Scholar] [CrossRef]
- Oluoch, T.; Santas, X.; Kwaro, D.; Were, M.C.; Biondich, P.G.; Bailey, C.; Abu-Hanna, A.; De Keizer, N. The effect of electronic medical record-based clinical decision support on HIV care in resource-constrained settings: A systematic review. Int. J. Med. Inform. 2012, 81, e83–e92. [Google Scholar] [CrossRef] [PubMed]
- Cresswell, K.; Sheikh, A. Organizational issues in the implementation and adoption of health information technology innovations: An interpretative review. Int. J. Med. Inform. 2013, 82, e73–e86. [Google Scholar] [CrossRef] [PubMed]
- Alexander, G.L.; Georgiou, A.; Doughty, K.; Hornblow, A.; Livingstone, A.; Dougherty, M.; Jacobs, S.; Fisk, M.J. Advancing health information technology roadmaps in long term care. Int. J. Med. Inform. 2020, 136, 104088. [Google Scholar] [CrossRef] [PubMed]
- Mäenpää, T.; Suominen, T.; Asikainen, P.; Maass, M.; Rostila, I. The outcomes of regional healthcare information systems in health care: A review of the research literature. Int. J. Med. Inform. 2009, 78, 757–771. [Google Scholar] [CrossRef]
- Åkesson, K.M.; Saveman, B.I.B.-I.; Nilsson, G. Health care consumers’ experiences of information communication technolo-gy-A summary of literatura. Int. J. Med. Inform. 2007, 76, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.R.; Staggers, N.; Laukert, T. Reviewing the impact of computerized provider order entry on clinical outcomes: The quality of systematic reviews. Int. J. Med. Inform. 2012, 81, 219–231. [Google Scholar] [CrossRef] [PubMed]
- Andargoli, A.E.; Scheepers, H.; Rajendran, D.; Sohal, A. Health information systems evaluation frameworks: A systematic review. Int. J. Med. Inform. 2017, 97, 195–209. [Google Scholar] [CrossRef] [PubMed]
- Meidiawati, Y.; Siregar, K.N.; Srimayarti, B.N. Potential Use of Personal Health Records in Managing Hypertension: A Systematic Review. Indian J. Public Health Res. Dev. 2020, 11. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G. Davis User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Ajzen, I. Attitudes, Personality, and Behavior, Berksh; Open Press: England, UK; New York, NY, USA, 2005. [Google Scholar]
- Rogers, E.M. Diffusion of Innovations, Free Press. 2003. Available online: https://books.google.es/books/about/Diffusion_of_Innovations_5th_Edition.html?id=9U1K5LjUOwEC&redir_esc=y (accessed on 8 September 2017).
- Kuan, K.K.; Chau, P.Y. A perception-based model for EDI adoption in small businesses using a technology–organization–environment framework. Inf. Manag. 2001, 38, 507–521. [Google Scholar] [CrossRef]
- Alaiad, A.; Zhou, L. The determinants of home healthcare robots adoption: An empirical investigation. Int. J. Med. Inform. 2014, 83, 825–840. [Google Scholar] [CrossRef]
- Alaiad, A.; AlSharo, M.; Alnsour, Y. The Determinants of M-Health Adoption in Developing Countries: An Empirical Investigation. Appl. Clin. Inform. 2019, 10, 820–840. [Google Scholar] [CrossRef]
- Cook, E.J.; Randhawa, G.; Sharp, C.; Ali, N.; Guppy, A.; Barton, G.; Bateman, A.; Crawford-White, J. Exploring the factors that influence the decision to adopt and engage with an integrated assistive telehealth and telecare service in Cambridgeshire, UK: A nested qualitative study of patient ‘users’ and ‘non-users’. BMC Health Serv. Res. 2016, 16, 137. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.-C.; Jen, W.-Y. The Adoption of Mobile Health Management Services: An Empirical Study. J. Med. Syst. 2010, 36, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Paré, G.; Raymond, L.; de Guinea, A.O.; Poba-Nzaou, P.; Trudel, M.-C.; Marsan, J.; Micheneau, T. Barriers to organizational adoption of EMR systems in family physician practices: A mixed-methods study in Canada. Int. J. Med. Inform. 2014, 83, 548–558. [Google Scholar] [CrossRef]
- Hoque, R. An empirical study of mHealth adoption in a developing country: The moderating effect of gender concern. BMC Med. Inform. Decis. Mak. 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Zhang, X.; Pérez-Stable, E.J.; Bourne, P.E.; Peprah, E.; Duru, O.K.; Breen, N.; Berrigan, D.; Wood, F.; Jackson, J.S.; Wong, D.W.; et al. Big Data Science: Opportunities and Challenges to Address Minority Health and Health Disparities in the 21st Century. Ethn. Dis. 2017, 27, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Vaportzis, E.; Clausen, M.G.; Gow, A.J. Older Adults Perceptions of Technology and Barriers to Interacting with Tablet Computers: A Focus Group Study. Front. Psychol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Data for Impact. Estimating the Effect of COVID-19 on Total Utilization of Health Services in Bangladesh—DataForIm-pactProject. 2021. Available online: https://www.data4impactproject.org/publications/estimating-the-effect-of-covid-19-on-total-utilization-of-health-services-in-bangladesh/ (accessed on 9 April 2021).
- Xiao, H.; Dai, X.; Wagenaar, B.H.; Liu, F.; Augusto, O.; Guo, Y.; Unger, J.M. The impact of the COVID-19 pandemic on health services utilization in China: Time-series analyses for 2016–2020. Lancet Reg. Health West. Pac. 2021, 9. [Google Scholar] [CrossRef]
- The Health System Response Monitor (HSRM). COVID-19 Health System Response Monitor. Policy Responses for Bulgaria: Monitoring and Surveillance. Available online: https://www.covid19healthsystem.org/mainpage.aspx (accessed on 9 April 2021).
- World Health Organization. Health Service Data—WHO. World Health Data Platform/Data Collection Tools/Health Service Data. 2021. Available online: https://www.who.int/data/data-collection-tools/health-service-data (accessed on 9 April 2021).
- World Health Organization. Analysing and Using Routine Data to Monitor the Effects of COVID-19 on Essential Health Ser-vices: Practical Guide for National and Subnational Decision-Makers. COVID-19: Essential Health Services. 2021. Available online: https://www.who.int/publications/i/item/who-2019-nCoV-essential-health-services-monitoring-2021-1 (accessed on 9 April 2021).
- Michelsen, K.; Helmut, P.; Achterberg, J. Wilkinson, Promoting Better Integration of Health Information Systems: Best Practices and Challenges Health Evidence Network Synthesis Report; WHO Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- Bogaert, P.; For BRIDGE Health; Van Oyen, H. An integrated and sustainable EU health information system: National public health institutes’ needs and possible benefits. Arch. Public Health 2017, 75, 1–5. [Google Scholar] [CrossRef]
- Lau, F.; Kuziemsky, C.; Price, M.; Gardner, J. A review on systematic reviews of health information system studies. J. Am. Med. Inform. Assoc. 2010, 17, 637–645. [Google Scholar] [CrossRef]
- Busza, J.; Lemma, S.; Janson, A.; Adem, S.O.; Berhanu, D.; Defar, A.; Persson, L.-Å.; Källestål, C. Strengthening routine health data analysis in Ethiopia: The Operational Research and Coaching for Analysts (ORCA) experience. Glob. Health Action 2021, 14, 1901390. [Google Scholar] [CrossRef]
- Leon, N.; Balakrishna, Y.; Hohlfeld, A.; Odendaal, W.A.; Schmidt, B.-M.; Zweigenthal, V.; Watkins, J.A.; Daniels, K. Routine Health Information System (RHIS) improvements for strengthened health system management. Cochrane Database Syst. Rev. 2020, 2020. [Google Scholar] [CrossRef]
- Nguefack-Tsague, G.; Tamfon, B.B.; Ngnie-Teta, I.; Ngoufack, M.N.; Keugoung, B.; Bataliack, S.M.; Ndongo, C.B. Factors associated with the performance of routine health information system in Yaoundé-Cameroon: A cross-sectional survey. BMC Med. Inform. Decis. Mak. 2020, 20, 1–8. [Google Scholar] [CrossRef]
- Hoxha, K.; Hung, Y.W.; Irwin, B.R.; Grépin, K.A. Understanding the challenges associated with the use of data from routine health information systems in low- and middle-income countries: A systematic review. Health Inf. Manag. J. 2020, 2020. [Google Scholar] [CrossRef]
- Dossa, N.I.; Philibert, A.; Dumont, A. Using routine health data and intermittent community surveys to assess the impact of maternal and neonatal health interventions in low-income countries: A systematic review. Int. J. Gynecol. Obstet. 2016, 135, S64–S71. [Google Scholar] [CrossRef] [PubMed]
- Blaya, J.A.; Shin, S.S.; Yagui, M.; Contreras, C.; Cegielski, P.; Yale, G.; Suárez, C.; Asencios, L.; Bayona, J.; Kim, J.; et al. Reducing Communication Delays and Improving Quality of Care with a Tuberculosis Laboratory Information System in Resource Poor Environments: A Cluster Randomized Controlled Trial. PLoS ONE 2014, 9, e90110. [Google Scholar] [CrossRef]
- Wagenaar, B.H.; Sherr, K.; Fernandes, Q.; Wagenaar, A.C. Using routine health information systems for well-designed health evaluations in low- and middle-income countries. Health Policy Plan. 2016, 31, 129–135. [Google Scholar] [CrossRef] [PubMed]
| Ref. | Technical | Organizational | Data Needs, Data Production, Data Availability, Data Use | OUTPUT Good Quality of Information |
|---|---|---|---|---|
| Eden et al., 2016 [25] | (-) The changing nature of HIE across users, information systems, and organization contexts. (-) Lack of standard classification and description of HIE architectures. (-) Lack of a theoretical framework underpinning HIE implementation and evaluation. | (+) Strong privacy and safety policies and patient training; registered or online informed consent; approaches to identify patients. | ||
| Medic et al., 2019 [26] | (+) Easy-to-use, (Human–computer interaction) HCI-centric interfaces during deployment | (+) Show justification for decisions and underlying data to clinical users | (+) Access and compilation of information at the patient level through retrospective studies via EHR | |
| Gentil et al., 2017 [28] | (-) The influence of the technological infrastructure (HCE software for data extraction) on the scope of data collection projects. (-) The challenges of provider choice and initial purchase negotiations for EHR software. | (-) The nature of the data analyzed (coded or free text data) or privacy management is a major deterrent for GPs. | (-) Most of AP’s data collection projects were not limited to a specific geographic location within a country. | |
| (+) The set of facilities, services, and products offered by networks that extract data sets from the data warehouse in the areas of medical research and public healthcare | ||||
| Reeder et al., 2013 [32] | (-) Future HSH and HCH research should explore how to capture and implement standardized measures reported by participants in PHR. (-) Family members should be included as participants. | (+) The incorporation of data on the activity of the elderly in clinical information systems for (1) preventive health self-management and self-monitoring, (2) IT strategies to connect multiple stakeholders. | (-) Lack of evidence that technology provides feedback to older adults for decision making in their daily activities or maintaining their own health | |
| Anker et al., 2011 [21] | (+) Frequency of use, information, channels, and contents of the search; credibility of the information source, satisfaction with the information obtained | |||
| Marschollek et al., 2007 [22] | (-) Accessibility remains largely hypothetical for groups of older people, the most disadvantaged | (-) The quality and semantic accessibility of website content is a major issue. | ||
| Meidiawati et al., 2020 [40] | (-) Mobile applications should be associated with information that comes from the medical record, having a storage option so the data is more concise and can be viewed quickly. | |||
| Alexander et al., 2020 [35] | (-) Administrative data are inherently limited due to the lack of clinical specificity for laboratory conditions and results. (-) New clinical data needs to be included in the EMRs. | (+) The roadmap has five areas and content areas that LTC leaders should use to make strategic and comprehensive approach decisions. | ||
| Mahmoudi et al., 2020 [30] | (-) Granular data elements should be implemented through text mining, merging them with smaller geographic units of analysis, or by encouraging health systems to collect these outstanding attributes. | (+) EMR encompasses a large repository of multidimensional data. | ||
| Mäenpää et al., 2009 [36] | (-) Lack of common rules and policies for sharing clinical data. Lack of a consistent strategic plan. This results in consequences at the level of the organization’s culture and resistance to change. | |||
| Wisner et al., 2019 [27] | (+) Focus on best practices for physician input on IT design to ensure that the content of the preconfigured templates makes it clinically meaningful and organized in a way that supports clinical work | (+) Effectively integrate narrative notes into EHR as an organizational aspect of clinical practice | (+) Improves the knowledge of professionals through greater access and visibility to information, having it available to multiple users, with data integrity and readability, or automatic data entry. | (+) Collect and synthesize information through data sources to contextualize and synthesize the information for the general description of the patient and to support clinical work. |
| Ref. | Technical | Behavioral | Organizational | OUTPUT Effective Use of Information for Decision-Making |
|---|---|---|---|---|
| Eden et al., 2016 [25] | (-) Contrasting evidence is lacking on barriers to the use of HIEs by function type or by architecture type. (-) Technology and user needs. (-) The optimal functionality of HIE is challenged by the lack of consistent classification and terminology of HIEs and by the changing nature of the sociotechnical systems involved. | (-) Information is lacking in the HIE to justify its use (perception of privacy and patient safety; incompatibility or population scope; competition with health systems; liability and negligence issues). | (+) The vision of information technology in health as sociotechnical systems characterized by dynamic interdependence and the co-evolution of technologies and the social contexts in which they are used. (+) Thoughtful implementation and workflow. | (+) Include end users in identifying key HIE functions. |
| (-) Following organizational and workflow aspects. | ||||
| Gentil et al., 2017 [28] | (+) Offer to GPs simplified data extraction tools to minimize additional workload. | (+) Promote to GPs with financial benefits, training sessions (in data coding), feedback reports, and participation in research studies. | (-) The limited applicability and usefulness of EHR data for large-scale research purposes. | (-) By using a single software application, it limits interoperability issues and facilitates technical data analysis. |
| Reeder et al., 2013 [32] | (-) Market forces dictate access to technology and services. (-) Existing commercial lifestyle monitoring technologies may not be ready for large-scale deployment. (-) Information related to technology costs and sustainable reimbursement models is lacking. | (+) Involve and inform family members of older adults and stakeholders in the development of HSH or HCH technology. | (-) The communication gap between health sciences and technology researchers. This makes transferability difficult when trying to redesign business processes and change the organizational culture of organizations. | |
| Åkesson et al., 2007 [37] | (+) Cooperation between nursing professionals and software engineering is important in creating consumer applications. | (-) More research is needed to measure consumer digital experiences in health and the factors that influence them. | ||
| Anker et al., 2011 [21] | (+) Keep in mind the following attitudinal aspects: locus of control, self-efficacy, desire, and intentions to have medical information, satisfaction with the doctor–patient relationship. | |||
| Eslami Andargoli et al., 2017 [39] | (+) Overcome partial approaches and use more holistic approaches that consider content, process, and context. | |||
| Marschollek et al., 2007 [22] | (-) Not much work is being performed on the design of the interface for the elderly or people with functional disabilities. | (-) Positive attitudes toward web-based communication on the part of older people have been contrasted. (-) Technological limitations. | ||
| Meidiawati et al., 2020 [40] | (+) PHRs can encourage users to engage in healthy living behaviors | |||
| Weir et al., 2012 [38] | (-) The recommendations emphasize clarifying the phenomenon of CPOE, avoiding reporting conclusions through subgroup analysis, developing theoretical models, including more quantitative evaluations of results. | |||
| Oluoch et al., 2012 [33] | (-) Technical infrastructure problems (electrical power, erratic Internet connectivity, and access to mobile phones) impede the implementation and effective use of EMR–CDSS. | (-) Limited computer skills of clinicians prevent effective use of EMR–CDSS. | (-) Failure to comply with reminders by providers prevents effective use of EMR–CDSS. | |
| Bayoumi et al., 2014 [23] | (-) Due to their wide range, they may be more subject to alert fatigue. | (-) More research is required to find out about the quality, relevance, and usability of decision support, and to study clinical outcomes and costs. | ||
| Alexander et al., 2020 [35] | (-) Lack of trust in HIT providers; lack of interoperability between systems; and lack of adaptation of IT to existing work patterns. | (-) Limited financial resources for LTC technologies; deficits in human capital to execute and maintain HIT; shortage of vital networks that support the adoption, use, and exchange of information through technology. | (-) Research is lacking in LTC activities under healthcare delivery systems. | |
| Mahmoudi et al., 2020 [30] | (-) Machine learning methods vary substantially in their interpretation, creating barriers and impediments to clinical acceptance and their implementation in all health systems. | (+) The use of EMR data and machine learning methods has created a huge opportunity to refine risk prediction tools for readmission of risk groups. | ||
| Mäenpää et al., 2009 [36] | (-) Aspects related to usability, privacy, and confidentiality. | (+) Advances in computer skills, employee engagement, leadership, and organizational rules; formal and sustainable business model | (+) Political initiatives (a strategic framework, construction of an electronic health information infrastructure, and an implementation plan that takes the organizations into consideration). | |
| Ingebrigtsen et al., 2014 [31] | (+) Strong, visible, and proactive leadership of a clinical profile with technical IT skills in health and with previous experience in IT project management. (+) International educational initiatives to improve the scope and dissemination of IT competencies in health | (+) The positive impact of clinical leaders on successful IT adoption (cultivating necessary IT competencies, establishing mutual partnerships with IT professionals, and executing identifiable proactive IT behaviors). | ||
| Baysari et al., 2016 [24] | (-) The usability of the system and the negative impact of these systems on workflow or efficiency | (-) Low acceptance of IT systems by individual, clinical, and organizational factors, including the setting between technology and the different ways physicians work | (+) IT interventions can be effective in improving the appropriate use of antimicrobials in hospitals. | |
| Cresswell and Sheikh, 2013 [34] | (+) Technology has the potential to adapt (or be customized) to support changing needs and individual and organizational contexts of use. | (-) End-user resistance to the use of systems that are deemed inappropriate or that interferes with their values, aspirations, and roles. | (+) Research drawing on experience in disciplines or fields of knowledge that contribute to the study of technical, social, and organizational issues is essential to promote knowledge about organizational adoption and best practices for implementation. | |
| Wisner et al., 2019 [27] | (-) The structure of the EHR does not always match the way of thinking and working of nurses, generating additional work to integrate the use of the EHR into their complex and dynamic workflows. | (+) EHR improves some aspects of cognitive work. | (-) The EHR’s focus on data integrity, aggregation, and storage has produced large volumes of information that clinicians find difficult to navigate and synthesize, making clinically meaningful information less accessible and available. |
| Ref. | Behavioral | Organizational | OUTCOMES RHIS Performance | OUTCOMES Health Systems Performance | IMPACT Health Status |
|---|---|---|---|---|---|
| Eden et al., 2016 [25] | (-) Some hospital systems are hesitant to share health data with competitors because they are worried about losing patients and their market share. | ||||
| Arditi et al., 2017 [29] | (+) Reminders can improve the quality of care in various settings and under various conditions | (-) There is no certainty that reminders improve patient outcomes as the evidence is minimal. | |||
| Medic et al., 2019 [26] | (+) Efficient and training just in time. | (+) Integrate CDS into clinical workflows without adding unnecessary additional work. (+) Evaluate the effectiveness and risks of CDS. (+) Provide ongoing feedback to clinicians. (+) Understand the ethical challenges for CDS. (+) Standardize the implementation. | (+) Machine-learning techniques depending on the selected problem and the types of data used. | ||
| Gentil et al., 2017 [28] | (+) Involvement of government services, academic institutions, and software companies, financing long-term and wide-ranging data collection projects. | (+) The local network effect facilitates the diffusion of initiatives. | (+) AI can provide clinical decision support systems, providing capabilities to analyze free-text information through new natural language processing algorithms. | ||
| (-) Using different software applications hampers data collection and adds interoperability issues. | |||||
| Åkesson et al., 2007 [37] | (+) ICT can improve the nurse-patient relationship and increase the welfare of patients. (+) ICT resources made consumers feel more confident and empowered, increased their knowledge, and improved their health status. | ||||
| Anker et al., 2011 [21] | (-) Future research should analyze how the search for health information influences health management. | ||||
| Eslami Andargoli et al., 2017 [39] | (+) Map existing health information systems and assess their integrity based on their response to what (content), how and when (process), and who and why (context). | (+) Overcome partial approaches and address more holistic approaches that consider the content, process, and context approach. | |||
| Marschollek et al., 2007 [22] | (-) Health information systems continue to be used primarily in health care for monitoring purposes, not as information brokering. | ||||
| Meidiawati et al., 2020 [40] | (+) PHRs can be tools to monitor physical exercise, eating behaviors, and weight control to evaluate whether hypertension has been controlled based on measures and related laboratory results. | ||||
| Weir et al., 2012 [38] | (+) CPOE is associated with improvements in medication errors. | ||||
| Oluoch et al., 2012 [33] | (+) With EMP–CDSS, a reduction in data errors, missed appointments, missed CD4 results, and patient waiting times was observed. | ||||
| (-) With EMP–CDSS, a significant increase was observed in the time dedicated by physicians to direct patient care. | |||||
| Bayoumi et al., 2014 [23] | (-) Multidrug alert systems rarely target only those drugs known to have the greatest potential for clinical benefit or harm, decreasing the likelihood of clinical benefit. | (+) Process results (changes in laboratory control behavior or prescription). | (+) Clinical outcomes (adverse drug events and length of hospitalization). (+) Clinical results substitutes (hypoglycemia and blood sugar average time in therapeutic range for INRs). | ||
| Alexander et al., 2020 [35] | (+) Promoting policy drivers, implementing HIT benchmarking, and decision support in senior healthcare. | (-) Slow adoption of many of the clinical support HIT technologies by LTC facilities, developments around LTC HIT. | (-) Absence of longitudinal care plans for the elderly with care needs; lack of codesign of technology and related systems for the provision of care. | ||
| Mahmoudi et al., 2020 [30] | (+) The use of big data and sophisticated machine learning methods improve the predictability of readmission risk models based on EMR data. | (-) Explainable machine learning methods need to be developed and implemented to establish clinical utility and inspire potential changes in practice patterns. | (-) Health systems are not yet systematically collecting data about social and environmental factors, readmission risk, or other adverse health events. | ||
| Mäenpää et al., 2009 [36] | (-) Evaluate the value of the services arising from the exchange of health information for various stakeholder groups, such as providers, key players, and employers. | (-) There is a lack of experiences and data on factors for the successful formation and sustainability of clinical data exchanges; development and implementation of a framework for a health information network. | (+) RHIS provides patient information in real time; improves communication and coordination within a region, and case management and consultation with colleagues; allows patient-centered care processes to be redesigned; enables empowerment and multidisciplinary teamwork. | (+) RHIS enables improved clinical efficacy through the access and sharing of clinical data, leading to better health outcomes. | |
| Ingebrigtsen et al., 2014 [31] | (-) National “top-down” policies, legislation, and financing. | ||||
| Baysari et al., 2016 [24] | (-) The lack of comparative analyses of different IT interventions to assess their relative performance in improving prescribing. (-) The variety of study designs and outcome measures used to evaluate IT interventions prevented meaningful comparisons between different types of IT systems. | (+) IT interventions may be effective in improving the appropriate use of antimicrobials in hospitals. | (-) Variable evidence of the impact of IT interventions on health outcomes, such as mortality and length of stay. | ||
| Cresswell and Sheikh, 2013 [34] | (+) Early and ongoing user engagement, technology’s relative advantage and early demonstrable benefits, communication, close adjustment to organizational priorities and processes, training and support, effective leadership and change management, and partnership and financial considerations. | (+) The potential of numerous disciplines or bodies of knowledge on the study of technical, social, and organizational issues to facilitate the implementation and adoption of innovations in complex health service systems. (+) The dimensions “implementation and use/design of technology” are interrelated. Factors must adapt to compensate for the change. | (+) Technical, social, and organizational considerations are essential to ensure that technological innovations are useful and usable (care provision) and support organizations or systems (organizational functioning). | ||
| Wisner et al., 2019 [27] | (+) Effectively evaluating the impact of EHRs requires the interactions between physician, technology, the environment, and the social system to be considered. (-) Workflows in the clinical setting and the use of EHR in real life are rarely linear and predictable. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saigí-Rubió, F.; Pereyra-Rodríguez, J.J.; Torrent-Sellens, J.; Eguia, H.; Azzopardi-Muscat, N.; Novillo-Ortiz, D. Routine Health Information Systems in the European Context: A Systematic Review of Systematic Reviews. Int. J. Environ. Res. Public Health 2021, 18, 4622. https://doi.org/10.3390/ijerph18094622
Saigí-Rubió F, Pereyra-Rodríguez JJ, Torrent-Sellens J, Eguia H, Azzopardi-Muscat N, Novillo-Ortiz D. Routine Health Information Systems in the European Context: A Systematic Review of Systematic Reviews. International Journal of Environmental Research and Public Health. 2021; 18(9):4622. https://doi.org/10.3390/ijerph18094622
Chicago/Turabian StyleSaigí-Rubió, Francesc, José Juan Pereyra-Rodríguez, Joan Torrent-Sellens, Hans Eguia, Natasha Azzopardi-Muscat, and David Novillo-Ortiz. 2021. "Routine Health Information Systems in the European Context: A Systematic Review of Systematic Reviews" International Journal of Environmental Research and Public Health 18, no. 9: 4622. https://doi.org/10.3390/ijerph18094622
APA StyleSaigí-Rubió, F., Pereyra-Rodríguez, J. J., Torrent-Sellens, J., Eguia, H., Azzopardi-Muscat, N., & Novillo-Ortiz, D. (2021). Routine Health Information Systems in the European Context: A Systematic Review of Systematic Reviews. International Journal of Environmental Research and Public Health, 18(9), 4622. https://doi.org/10.3390/ijerph18094622










