How a Depressive Medical Doctor Profited in the Long-Term from a New and Short Psychological Group-Treatment against Major Depressive Disorder
Abstract
1. Introduction
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pub.: Washington, DC, USA, 2013; p. 795ff. [Google Scholar]
- Munkholm, K.; Paludan-Müller, A.S.; Boesen, K. Considering the methodological limitations in the evidence base of antidepressants for depression: A reanalysis of a network meta-analysis. BMJ Open 2019, 9, e024886. [Google Scholar] [CrossRef]
- Hengartner, M.P. Scientific debate instead of beef; challenging misleading arguments about the efficacy of antidepressants. Acta Neuropsychiatr. 2019, 31, 235–236. [Google Scholar] [CrossRef] [PubMed]
- Covi, L.; Lipman, R.; Pattison, J.; Derogatis, L.; Uhlenhuth, E. Length of treatment with anxiolytic sedatives and response to their sudden withdrawal. Acta Psychiatr. Scand. 1973, 49, 51–64. [Google Scholar] [CrossRef]
- Fontaine, R.; Chouinard, G.; Annable, L. Rebound anxiety in anxious patients after abrupt withdrawal of benzodiazepine treatment. Am. J. Psychiatry 1984, 141, 848–852. [Google Scholar] [PubMed]
- Chouinard, G.; Chouinard, V.-A. New classification of selective serotonin reuptake inhibitor withdrawal. Psychother. Psychosom. 2015, 84, 63–71. [Google Scholar] [CrossRef]
- World Health Organization. WHO Expert Committee on Drug Dependence: Thirty-Third Report; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Cipriani, A.; Furukawa, T.A.; Salanti, G.; Chaimani, A.; Atkinson, L.Z.; Ogawa, Y.; Leucht, S.; Ruhe, H.G.; Turner, E.H.; Higgins, J.P.T.; et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Focus 2018, 16, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Hengartner, M.P.; Plöderl, M. Newer-generation antidepressants and suicide risk in randomized controlled trials: A re-analysis of the FDA database. Psychother. Psychosom. 2019, 88, 247–248. [Google Scholar] [CrossRef] [PubMed]
- Hengartner, M.P.; Plöderl, M. Statistically significant antidepressant-placebo differences on subjective symptom-rating scales do not prove that the drugs work: Effect size and method bias matter! Front. Psychiatry 2018, 9, 517. [Google Scholar] [CrossRef] [PubMed]
- Gaynes, B.N.; Lloyd, S.W.; Lux, L.; Gartlehner, G.; Hansen, R.A.; Brode, S.; Jonas, D.E.; Evans, T.W.; Viswanathan, M.; Lohr, K.N. Repetitive transcranial magnetic stimulation for treatment-resistant depression: A systematic review and meta-analysis. J. Clin. Psychiatry 2014, 75, 477–489. [Google Scholar] [CrossRef]
- Salehi, I.; Hosseini, S.M.; Haghighi, M.; Jahangard, L.; Bajoghli, H.; Gerber, M.; Pühse, U.; Holsboer-Trachsler, E.; Brand, S. Electroconvulsive therapy (ECT) and aerobic exercise training (AET) increased plasma BDNF and ameliorated depressive symptoms in patients suffering from major depressive disorder. J. Psychiatr. Res. 2016, 76, 1–8. [Google Scholar] [CrossRef]
- Ren, J.; Li, H.; Palaniyappan, L.; Liu, H.; Wang, J.; Li, C.; Rossini, P.M. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: A systematic review and meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2014, 51, 181–189. [Google Scholar] [CrossRef]
- Li, J.-M.; Zhang, Y.; Su, W.-J.; Liu, L.-L.; Gong, H.; Peng, W.; Jiang, C.-L. Cognitive behavioral therapy for treatment-resistant depression: A systematic review and meta-analysis. Psychiatry Res. 2018, 268, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Berking, M.; Andersson, G.; Quigley, L.; Kleiboer, A.; Dobson, K.S. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Can. J. Psychiatry 2013, 58, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.; Reichert, T.; Bagatini, N.C.; Bgeginski, R.; Stubbs, B. Physical activity and sedentary behavior in people with major depressive disorder: A systematic review and meta-analysis. J. Affect. Disord. 2017, 210, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Morres, I.D.; Ekkekakis, P.; Rosenbaum, S.; Stubbs, B. A critical review of exercise as a treatment for clinically depressed adults: Time to get pragmatic. Acta Neuropsychiatr. 2017, 29, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.; Vasconcelos-Moreno, M.; Borowsky, C.; Zimmermann, A.; Rocha, N.; Fleck, M. Exercise and severe major depression: Effect on symptom severity and quality of life at discharge in an inpatient cohort. J. Psychiatr. Res. 2015, 61, 25–32. [Google Scholar] [CrossRef]
- Stubbs, B.; Rosenbaum, S.; Vancampfort, D.; Ward, P.B.; Schuch, F.B. Exercise improves cardiorespiratory fitness in people with depression: A meta-analysis of randomized control trials. J. Affect. Disord. 2016, 190, 249–253. [Google Scholar] [CrossRef]
- Netterstrøm, B.; Conrad, N.; Bech, P.; Fink, P.; Olsen, O.; Rugulies, R.; Stansfeld, S. The relation between work-related psychosocial factors and the development of depression. Epidemiol. Rev. 2008, 30, 118–132. [Google Scholar] [CrossRef]
- Stansfeld, S.; Candy, B. Psychosocial work environment and mental health—A meta-analytic review. Scand. J. Work Environ. Health 2006, 32, 443–462. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, K.; Bruinvels, D.; Frings-Dresen, M. Psychosocial work environment and stress-related disorders, a systematic review. Occup. Med. 2010, 60, 277–286. [Google Scholar] [CrossRef]
- Ndjaboué, R.; Brisson, C.; Vézina, M. Organisational justice and mental health: A systematic review of prospective studies. Occup. Environ. Med. 2012, 69, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, M.; Nyberg, S.T.; Batty, G.D.; Jokela, M.; Heikkilä, K.; Fransson, E.I.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; et al. Perceived job insecurity as a risk factor for incident coronary heart disease: Systematic review and meta-analysis. BMJ 2013, 374, f4746. [Google Scholar] [CrossRef] [PubMed]
- Stuke, H.; Bermpohl, F. Welche Arbeitsbedingungen begünstigen die Entwicklung einer depressiven Störung? Psychiatr. Prax. 2016, 43, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Lépine, J.-P.; Briley, M. The increasing burden of depression. Neuropsychiatr. Dis. Treat. 2011, 7 (Suppl. 1), 3. [Google Scholar]
- Amos, T.B.; Tandon, N.; Lefebvre, P.; Pilon, D.; Kamstra, R.L.; Pivneva, I.; Greenberg, P.E. Direct and Indirect Cost Burden and Change of Employment Status in Treatment-Resistant Depression: A Matched-Cohort Study Using a US Commercial Claims Database. J. Clin. Psychiatry 2018, 79, 17m11725. [Google Scholar] [CrossRef]
- Lerner, D.; Adler, D.A.; Chang, H.; Lapitsky, L.; Hood, M.Y.; Perissinotto, C.; Reed, J.; McLaughlin, T.J.; Berndt, E.R.; Rogers, W.H. Unemployment, job retention, and productivity loss among employees with depression. Psychiatr. Serv. 2004, 55, 1371–1378. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Koeser, L.; Knapp, M.; Longhitano, C.; Zohar, J.; Kuhn, K. Evaluating the economic impact of screening and treatment for depression in the workplace. Eur. Neuropsychopharmacol. 2016, 26, 1004–1013. [Google Scholar] [CrossRef]
- McTernan, W.P.; Dollard, M.F.; LaMontagne, A.D. Depression in the workplace: An economic cost analysis of depression-related productivity loss attributable to job strain and bullying. Work Stress 2013, 27, 321–338. [Google Scholar] [CrossRef]
- McCrone, P.; Rost, F.; Koeser, L.; Koutoufa, I.; Stephanou, S.; Knapp, M.; Goldberg, D.; Taylor, D.; Fonagy, P. The economic cost of treatment-resistant depression in patients referred to a specialist service. J. Ment. Health 2018, 27, 567–573. [Google Scholar] [CrossRef]
- Schramm, E.; Berger, M. Interpersonal psychotherapy for work-related stress depressive disorders. Nervenarzt 2013, 84, 813–822. [Google Scholar] [CrossRef]
- Niedermoser, D.W.; Kalak, N.; Kiyhankhadiv, A.; Brand, S.; Walter, C.; Schweinfurth, N.; Lang, U.E. Workplace-Related Interpersonal Group Psychotherapy to Improve Life at Work in Individuals With Major Depressive Disorders: A Randomized Interventional Pilot Study. Front. Psychiatry 2020, 11, 168. [Google Scholar] [CrossRef]
- Cuijpers, P.; van Straten, A.; Hollon, S.; Andersson, G. The contribution of active medication to combined treatments of psychotherapy and pharmacotherapy for adult depression: A meta-analysis. Acta Psychiatr. Scand. 2010, 121, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Brakemeier, E.-L.; Köhler, S.; Sterzer, P. Schulenübergreifende Psychotherapie der chronischen Depression. PID-Psychother. Dialog 2013, 14, 34–38. [Google Scholar] [CrossRef][Green Version]
- Boesen, K.; Paludan-Müller, A.S.; Munkholm, K. Network meta-analysis of antidepressants. Lancet 2018, 392, 1011–1012. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Knapp, M. Global patterns of workplace productivity for people with depression: Absenteeism and presenteeism costs across eight diverse countries. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1525–1537. [Google Scholar] [CrossRef] [PubMed]
| Module | Goals |
|---|---|
|
|
|
|
|
|
|
|
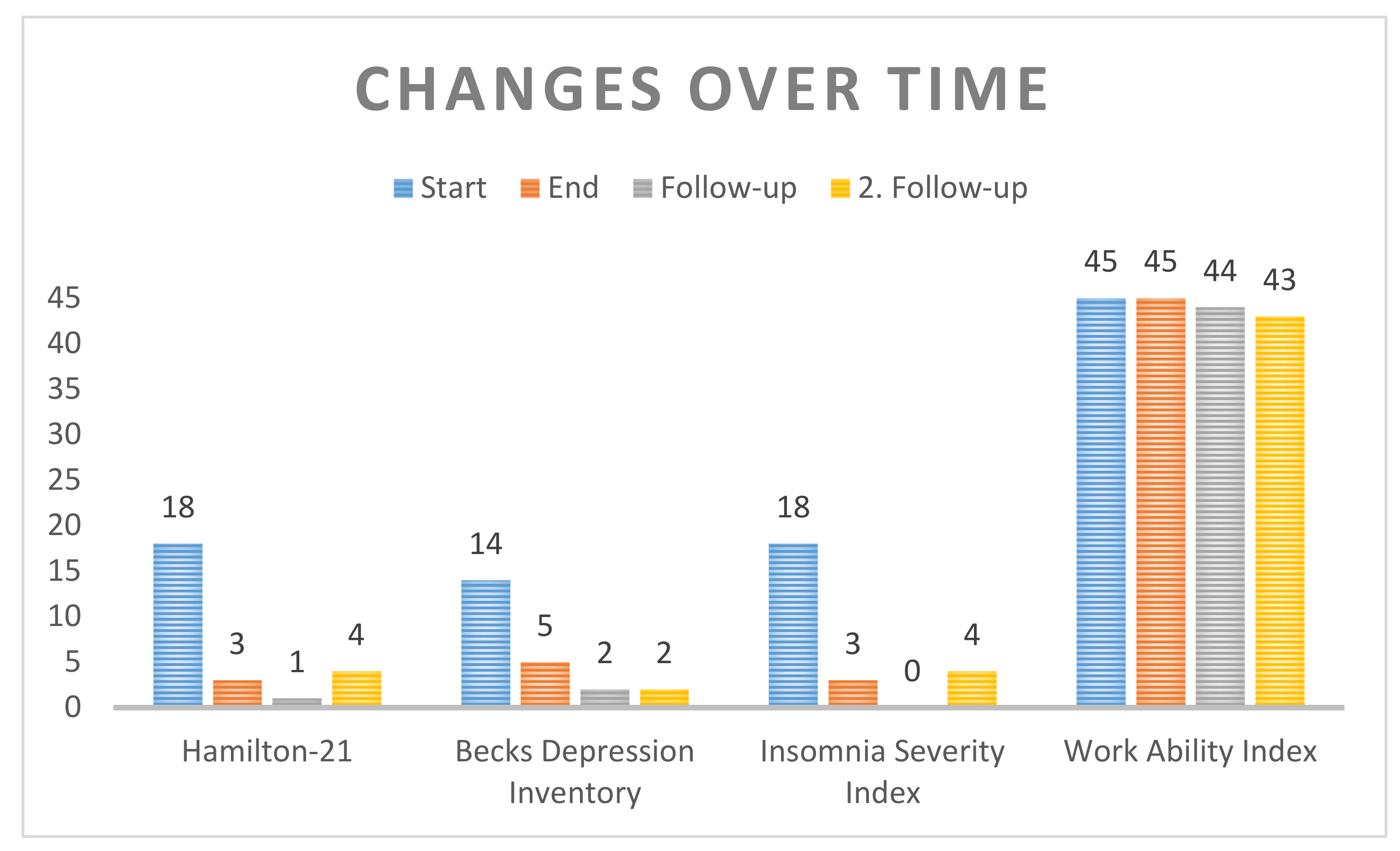
| Start | End | Follow-Up | 2. Follow-Up (15 Months) | |
|---|---|---|---|---|
| Hamilton-21 | 18 | 3 | 1 | 4 |
| Becks Depression Inventory | 14 | 5 | 2 | 2 |
| Insomnia Severity Index | 18 | 3 | 0 | 4 |
| Work Ability Index | 45 | 45 | 44 | 43 |
| Start | End | Follow-Up | 2. Follow-Up (15 Months) | |
|---|---|---|---|---|
| Hamilton-21 | Moderate depression | No depression | No depression | No depression |
| Becks Depression Inventory | Mild depression | No depression | No depression | No depression |
| Insomnia Severity Index | Clinical insomnia, moderate severity | No clinically significant insomnia | No clinically significant insomnia | No clinically significant insomnia |
| Work Ability Index | Very good work ability | Very good work ability | Very good work ability | Good work ability |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niedermoser, D.W.; Kalak, N.; Meyer, M.; Schweinfurth, N.; Walter, M.; E. Lang, U. How a Depressive Medical Doctor Profited in the Long-Term from a New and Short Psychological Group-Treatment against Major Depressive Disorder. Int. J. Environ. Res. Public Health 2021, 18, 1925. https://doi.org/10.3390/ijerph18041925
Niedermoser DW, Kalak N, Meyer M, Schweinfurth N, Walter M, E. Lang U. How a Depressive Medical Doctor Profited in the Long-Term from a New and Short Psychological Group-Treatment against Major Depressive Disorder. International Journal of Environmental Research and Public Health. 2021; 18(4):1925. https://doi.org/10.3390/ijerph18041925
Chicago/Turabian StyleNiedermoser, Daryl Wayne, Nadeem Kalak, Martin Meyer, Nina Schweinfurth, Marc Walter, and Undine E. Lang. 2021. "How a Depressive Medical Doctor Profited in the Long-Term from a New and Short Psychological Group-Treatment against Major Depressive Disorder" International Journal of Environmental Research and Public Health 18, no. 4: 1925. https://doi.org/10.3390/ijerph18041925
APA StyleNiedermoser, D. W., Kalak, N., Meyer, M., Schweinfurth, N., Walter, M., & E. Lang, U. (2021). How a Depressive Medical Doctor Profited in the Long-Term from a New and Short Psychological Group-Treatment against Major Depressive Disorder. International Journal of Environmental Research and Public Health, 18(4), 1925. https://doi.org/10.3390/ijerph18041925






