Effects of the COVID-19 Pandemic on the Budgetary Mechanism Established to Cover Public Health Expenditure. A Case Study of Romania
Abstract
:1. Introduction
2. Retrospective Analysis of Romanian Public Health Care System and Prospective Implication of COVID-19 on the Economy
3. Materials and Methods
- M = average value
- Vt = actual value for for specif
- time/period t
- Wt = weighting factor for specific time/period t
- n = number of periods in the weighting group
- Zij = standardized value for variable j in sample uniti
- xij = data for variable j in sample uniti
- = sample mean for variable j
- sj = sample standard deviation for variable j
- It is not included the intercept ;
- It included intercept ;
- It included intercept and trend .
4. Empirical Results
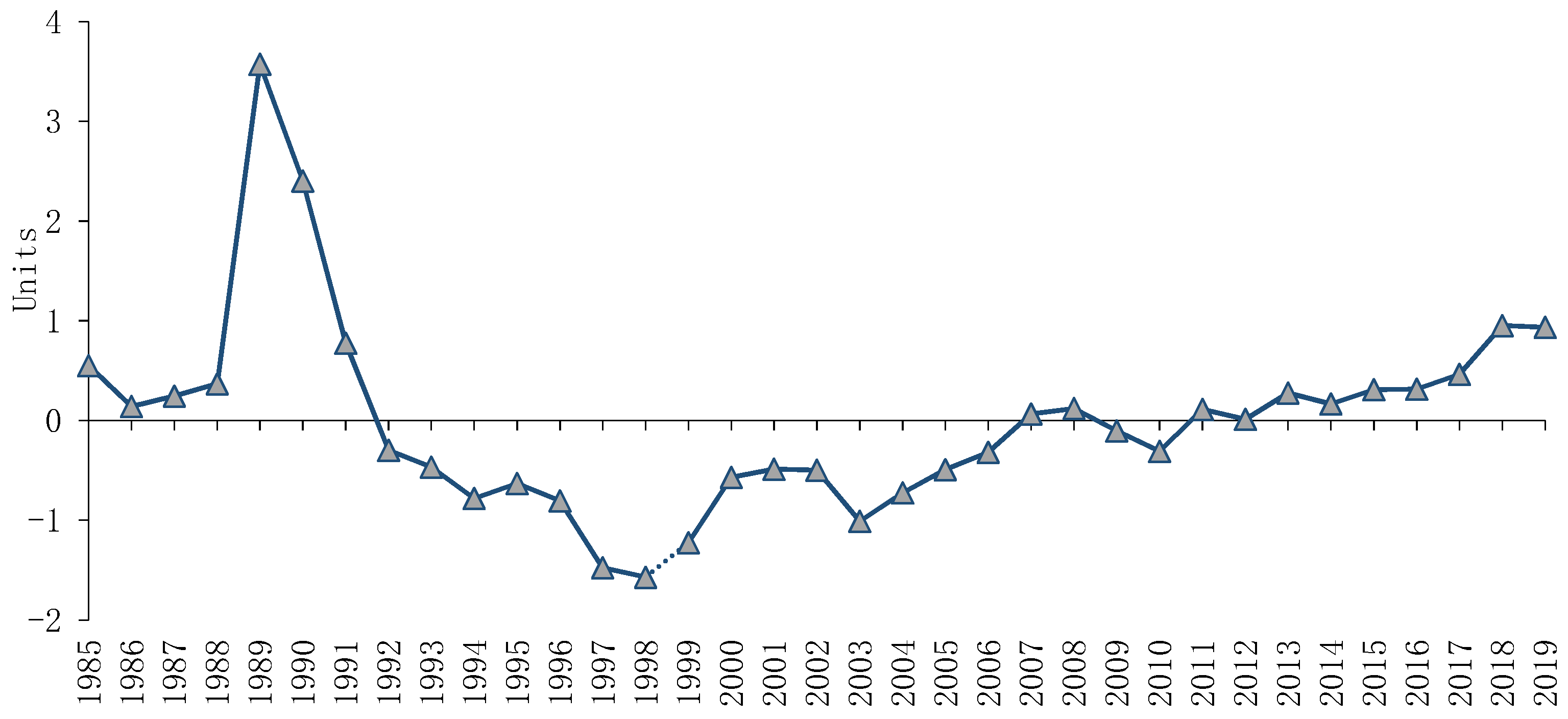
4.1. The Sustainability Index for Public Health
4.2. The Causal Relationship between Health Expenditure and GDP in Romania
5. Discussions
5.1. The Sustainability Index for Public Health
5.2. The Causal Relationship between Health Expenditure and GDP in Romania
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
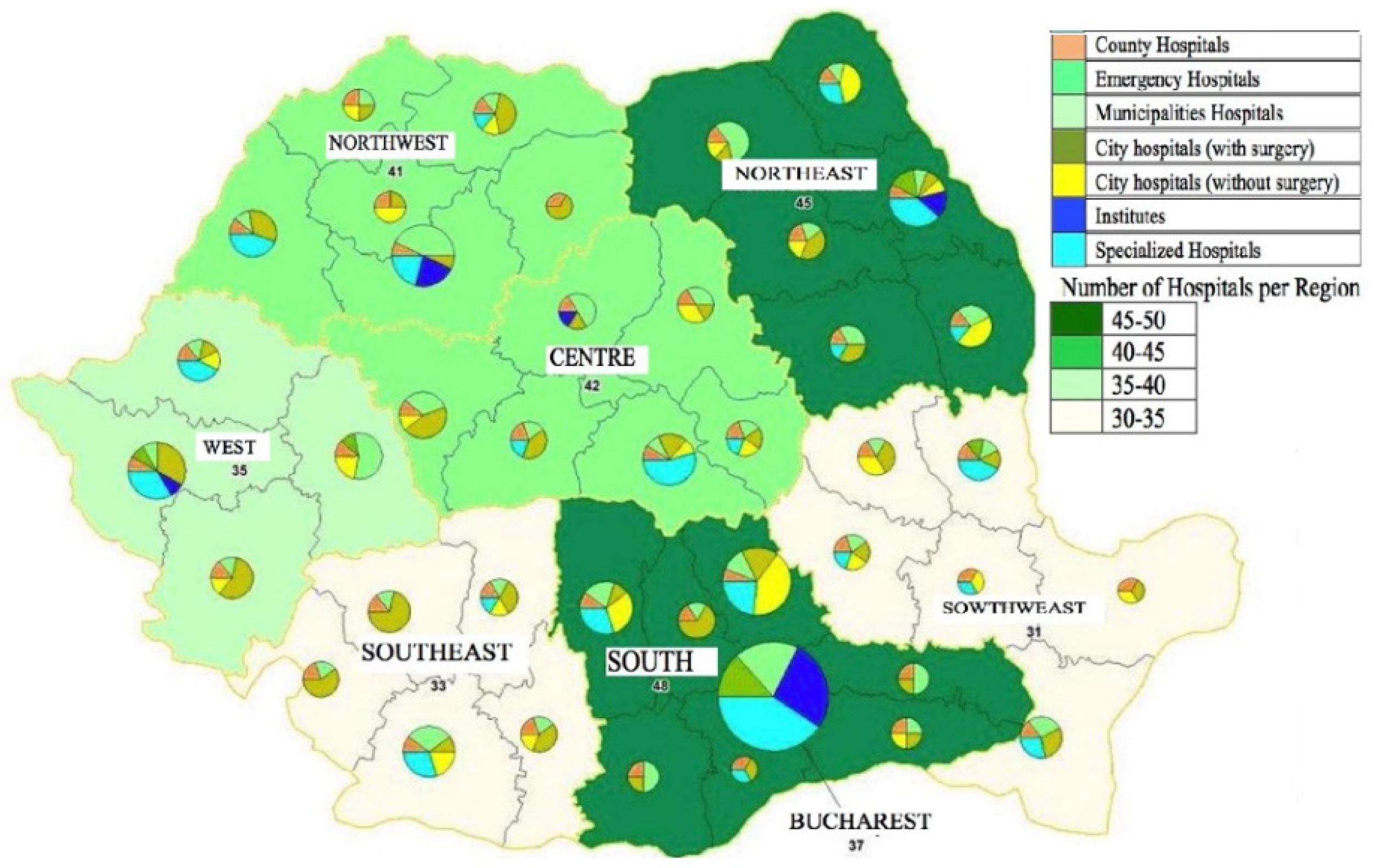
- County Hospitals—the hospitals located in the capital county, which have the human and material resources and the competences to ensure definitive medical care (including emergency medical care) for most cases that come from the county and cannot be treated permanently locally in hospitals municipal or urban centres or in the permanence centres, in accordance with the protocols in force;
- Emergency Hospitals—county hospitals, municipal hospitals, city hospitals (with surgery), and specialized hospitals with human and material resources and the competences to ensure definitive emergency medical care;
- Municipalities Hospitals—the hospitals located in municipal cities, respectively to centre of permanence, with the human and material resources and the competences to ensure definitive medical care (including emergency medical care) necessary to solve a part of the local emergencies; the emergencies that cannot be solved definitively are stabilized and transferred to the county hospital, as the case may be, in accordance with the protocols in force;
- City Hospitals (with surgery)—the hospitals located in cities with infrastructure to treat locally (including emergency medical care); the emergencies that cannot be solved definitively are stabilized and transferred to the municipal or county hospital, in accordance with the protocols in force;
- City Hospitals (without surgery)—the hospitals located in cities with infrastructure to treat locally; the emergencies are stabilized and transferred to the municipal or county hospital, in accordance with the protocols in force;
- Institutes or public health centres are regional or national public institutions, with legal personality, subordinated to the Ministry of Health, and which technically and methodologically coordinate the specialized activity in the field of substantiation, elaboration and implementation of strategies regarding disease prevention, control of diseases, and of public health policies in specific fields, at national and/or regional level; if they have a university clinical department they are clinical hospitals;
- Specialized Hospitals—hospitals that treat patients mainly with a certain dysfunction or from a certain social category. Thus, this category includes burn hospitals (treats people with burns), hospitals for people with mental health problems and children’s hospitals.
References
- Berardi, C.; Antonini, M.; Genie, M.G.; Cotugno, G.; Lanteri, A.; Melia, A.; Paolucci, F. The COVID-19 pandemic in Italy: Policy and technology impact on health and non-health outcomes. Health Policy Technol. 2020, 9, 454–487. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Hangrist, N.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S. Variation in government responses to COVID-19. Work. Pap. Sch. Gov. Blavatnik Oxf. 2020, 31, 2020-11. [Google Scholar]
- Moy, N.; Antonini, M.; Kyhlstedt, M.; Paolucci, F. Categorising Policy & Technology Interventions for a Pandemic: A Comparative and Conceptual Frame-Work. Work. Pap. 2020. Available online: http://ssrn.com/abstract=36229662020 (accessed on 5 November 2020).
- IMF (International Monetary Fund). Policy response to Covid-19 Policy Tracker. 2020. Available online: https://www.imf.org/en/Topics/imf-and-covid19/Policy-Responses-to-COVID-19 (accessed on 12 November 2020).
- OECD. Key Country Policy Tracker. 2020. Available online: https://www.oecd.org/coronavirus/en/#policy-responses (accessed on 4 November 2020).
- European Commission. State of Health in the EU Romania. Country Health Profile. 2017. Available online: https://ec.europa.eu/health/sites/health/files/state/docs/chp_romania_english.pdf (accessed on 25 October 2020).
- Dumitrache, L.; Nae, M.; Simion, G.; Taloș, A.-M. Modelling Potential Geographical access of the Population to Public Hospitals and Quality Health Care in Romania. Int. J. Environ. Res. Public Health 2020, 17, 8487. [Google Scholar] [CrossRef]
- Zamfir, D.; Dumitrache, L.; Stoica, I.V.; Vârdol, D. Spatial inequalities in health care provision in Romania: Milestones for territorial sustainable development. Carpathian J. Earth Environ. Sci. 2015, 10, 177–188. [Google Scholar]
- Vlădescu, C.; Scîntee, S.G.; Olsavszky, V.; Hernaández-Quevedo, C.; Sagan, A. Romania: Health system review. Health Syst. Transit. 2016, 18, 1–170. [Google Scholar]
- Dumitrache, L. Défis, incohérences et échecs de la réforme sanitaire en Roumanie. In Migration en Blanc. Medecins D’est en Ouest; Krasteva, A., Vasilcu, D., Eds.; Edition L’Harmattan, Collection Global et Local: Paris, France, 2014; pp. 21–40. [Google Scholar]
- Dumitrache, L.; Nae, M.; Dumbrăveanu, D.; Simion, G.; Suditu, B. Contrasting Clustering in Health Care Provision in Romania: Spatial and Aspatial Limitations. Procedia Environ. Sci. 2016, 32, 290–299. [Google Scholar] [CrossRef] [Green Version]
- Indaco. Government Decision no. 303/2011 or the approval of the National Strategy for the rationalization of hospitals, based on Antunes, E., Mordelet, P. De Groote, T. Elaborarea unei strategii pentru dezvoltarea infrastructurii spitalicești în România. Bucharest, Romania. Available online: https://lege5.ro/Gratuit/ge2demzzhe/hotararea-nr-303-2011-pentru-aprobarea-strategiei-nationale-de-rationalizare-a-spitalelor (accessed on 18 October 2020).
- Romanian Court of Accounts. Gestionarea resurselor publice în perioada stării de urgență (Management of public resources during the period state of emergency Special report made at the request of the Romanian Parliament). Bucharest. 2020. Available online: http://www.curteadeconturi.ro/Publicatii/Raport_stare_urgenta_11082020.pdf (accessed on 28 November 2020).
- European Commission. European Economic Forecast. Institutional Paper 136. 2020. Available online: https://ec.europa.eu/info/sites/info/files/economy-finance/ip136_en.pdf (accessed on 2 December 2020).
- Romanian Government. 2020; Regulation Process. Available online: https://gov.ro/ro/guvernul/procesul-legislativ (accessed on 4 December 2020).
- Douglas, L.A.; Calhoun, A.; Robichaux, C.B.; Elliott, M.B.; Moreland-Russell, S. Peer reviewed: The program sustainability assessment tool: A new instrument for public health programs. Prev. Chronic Dis. 2014, 11, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Härdle, W.K.; Simar, L. Applied Multivariate Statistical Analysis; Springer: Berlin, Germany, 2015. [Google Scholar]
- Subramanian, L.; Alexiou, C.; Nellis, J.G.; Steele, P.; Tolani, F. Developing a sustainability index for public health supply chains. Sustain. Futures 2020, 2, 100019. [Google Scholar] [CrossRef]
- Mapar, M.; Jafari, M.J.; Mansouri, N.; Arjmandi, R.; Azizinezhad, R.; Ramos, T.B. A composite index for sustainability assessment of health, safety and environmental performance in municipalities of megacities. Sustain. Cities Soc. 2020, 60, 102164. [Google Scholar] [CrossRef]
- World Bank. Open Data 2020. Available online: https://data.worldbank.org/ (accessed on 22 October 2020).
- World Health Organization (WHO). World Health Data Platform. 2020. Available online: https://www.who.int/data/collections (accessed on 24 October 2020).
- European Commission. EUROSTAT Database 2020b. Available online: https://ec.europa.eu/eurostat/data/database (accessed on 25 October 2020).
- Romanian Ministry of Finance. Database 2020. Available online: https://www.mfinante.gov.ro/pjuridice.html?pagina=domenii (accessed on 26 October 2020).
- Kim, T.K.; Lane, S.R. Government health expenditure and public health outcomes: A comparative study among 17 countries and implications for US health care reform. Am. Int. J. Contemp. Res. 2013, 3, 8–13. [Google Scholar]
- Kawabata, K.; Xu, K.; Carrin, G. Preventing impoverishment through protection against catastrophic health expenditure. Bull. World Health Organ. 2002, 80, 612. [Google Scholar] [PubMed]
- van den Heuvel, W.J.A.; Olaroiu, M. How important are health care expenditures for life expectancy? A comparative, European analysis. J. Am. Med Dir. Assoc. 2017, 18, 276.e9–276.e12. [Google Scholar] [CrossRef] [PubMed]
- Linden, M.; Ray, D. Life expectancy effects of public and private health expenditures in OECD countries 1970–2012: Panel time series approach. Econ. Anal. Policy 2017, 56, 101–113. [Google Scholar] [CrossRef] [Green Version]
- Scheffler, R.M.; Liu, J.X.; Kinfu, Y.; Dal Poz, M.R. Forecasting the global shortage of physicians: An economic-and needs-based approach. Bull. World Health Organ. 2008, 86, 516–523B. [Google Scholar] [CrossRef]
- Apergis, N.; Bhattacharya, M.; Hadhri, W. Health care expenditure and environmental pollution: A cross-country comparison across different income groups. Environ. Sci. Pollut. Res. 2020, 27, 8142–8156. [Google Scholar] [CrossRef]
- Chen, F.; Chen, Z. Cost of economic growth: Air pollution and health expenditure. Sci. Total Environ. 2020, 755, 142543. [Google Scholar] [CrossRef]
- Zaidi, S.; Saidi, K. Environmental pollution, health expenditure and economic growth in the Sub-Saharan Africa countries: Panel ARDL approach. Sustain. Cities Soc. 2018, 41, 833–840. [Google Scholar] [CrossRef]
- Khoshnevis Yazdi, S.; Khanalizadeh, B. Air pollution, economic growth and health care expenditure. Econ. Res. Ekon. Istraživanja 2017, 30, 1181–1190. [Google Scholar] [CrossRef] [Green Version]
- Chaabouni, S.; Saidi, K. The dynamic links between carbon dioxide (CO2) emissions, health spending and GDP growth: A case study for 51 countries. Environ. Res. 2017, 158, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Samakovlis, E.; Huhtala, A.; Bellander, T.; Svartengren, M. Valuing health effects of air pollution—focus on concentration-response functions. J. Urban Econ. 2005, 58, 230–249. [Google Scholar] [CrossRef]
- Huttinger, A.; Dreibelbis, R.; Kayigamba, F.; Ngabo, F.; Mfura, L.; Merryweather, B.; Cadon, A.; Moe, C. Water, sanitation and hygiene infrastructure and quality in rural healthcare facilities in Rwanda. BMC Health Serv. Res. 2017, 17, 517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geere, J.-A.L.; Hunter, P.R. The association of water carriage, water supply and sanitation usage with maternal and child health. A combined analysis of 49 Multiple Indicator Cluster Surveys from 41 countries. Int. J. Hyg. Environ. Health 2020, 223, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Freudenberg, N.; Vlahov, D. Cities and population health. Soc. Sci. Med. 2005, 60, 1017–1033. [Google Scholar] [CrossRef] [PubMed]
- Dye, C. Health and urban living. Science 2008, 319, 766–769. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. How to normalize cooccurrence data? An analysis of some well-known similarity measures. J. Am. Soc. Inf. Sci. Technol. 2009, 60, 1635–1651. [Google Scholar] [CrossRef] [Green Version]
- Fuller, W.A. Introduction to Statistical Time Series; John Wiley and Sons: New York, NY, USA, 1976. [Google Scholar]
- Elliott, G.; Rothenberg, T.J.; Stock, J.H. Efficient Tests for an Autoregressive Unit Root. Econometrica 1996, 64, 813–836. [Google Scholar] [CrossRef] [Green Version]
- Phillips, P.C.B.; Perron, P. Testing for a Unit Root in Time Series Regression. Biometrika 1988, 75, 335–346. [Google Scholar] [CrossRef]
- Russell, D.; MacKinnon, J.G. Econometric Theory and Methods; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Antony, G.M.; Visweswara Rao, K. A composite index to explain variations in poverty, health, nutritional status and standard of living: Use of multivariate statistical methods. Public Health 2007, 121, 578–587. [Google Scholar] [CrossRef]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research; SAGE: Memphis, TN, USA, 2003. [Google Scholar]
- Hightower, W.L. Development of an index of health utilizing factor analysis. Med. Care 1978, 16, 245–255. Available online: http://www.jstor.org/stable/3763294 (accessed on 22 November 2020). [CrossRef]
- Vlădescu, C.; Rădulescu, S.; Cace, S. The Romanian healthcare system: Between Bismark and Semashko. Decentralization in healthcare: Analyses and experiences in Central and Eastern Europe in the 1990s. In Local Government and Public Service Reform Initiative; Open Society Institute: Budapest, Hungary, 2005. [Google Scholar]
- Singh, D. Attitudes and praxis of traditional forms of health care in a post-communist Romanian Romani community. Anthropol. East Eur. Rev. 2011, 29, 127–140. [Google Scholar]
- Li, J. The influence of state policy and proximity to medical services on health outcomes. J. Urban Econ. 2014, 80, 97–109. [Google Scholar] [CrossRef]
- Bostan, I.; Burciu, A.; Condrea, P.; Durac, G. Involvement of legal responsibility for severe acts of pollution and noncompliance. Environ. Eng. Manag. J. 2009, 8, 469–473. [Google Scholar]
- Bostan, I. Pro sustainable development: The influence of the law of entropy on economic systems. Environ. Eng. Manag. J. 2016, 15, 2429–2432. [Google Scholar] [CrossRef]
- Kar, M.; Ağır, H. Relationship between human capital and economic growth in Turkey: Cointegration approach to causality test, 1926–1994. Sos. Ve Ekon. Araştırmalar Derg. 2006, 6, 51–68. [Google Scholar]
- Wang, Z.; Rettenmaier, A.J. A note on cointegration of health expenditures and income. Health Econ. 2007, 16, 559–578. [Google Scholar] [CrossRef]
- Taban, S. Causal relationship between health and economic growth in Turkey. Sosyoekonomi 2006, 4, 31–46. [Google Scholar]
- Mehrara, M.; Musai, M. The causality between health expenditure and economic growth in Iran. Int. J. Econ. Resour. 2011, 2, 13–19. [Google Scholar]
- European Commission; OECD. Health at a Glance Europe 2018 State of Health in the EU Cycle. Available online: https://www.oecd.org/health/health-systems/Health-at-a-Glance-Europe-2018-CHARTSET.pdf (accessed on 26 November 2020).
- Nielsen, H.B. Cointegration analysis in the presence of outliers. Econom. J. 2004, 7, 249–271. Available online: https://www.jstor.org/stable/23115009 (accessed on 29 November 2020). [CrossRef]
- Nielsen, H.B. Non-Stationary Time Series, Cointegration and Spurious Regression. 2005. Available online: http://www.econ.ku.dk/metrics/Econometrics2_05_II/Slides/10_cointegration_2pp.pdf (accessed on 29 November 2020).
- Nielsen, H.B.; Rahbek, A. The likelihood ratio test for cointegration ranks in the I (2) model. Econom. Theory 2007, 23, 615–637. [Google Scholar] [CrossRef]
- MacKinnon, J.; Haug, A.; Michelis, L. Numerical Distribution Functions of Likelihood Ratio Tests for Cointegration. J. Appl. Econom. 1999, 14, 563–577. [Google Scholar] [CrossRef]
- Atilgan, E.; Kilic, D.; Ertugrul, H.M. The dynamic relationship between health expenditure and economic growth: Is the health-led growth hypothesis valid for Turkey? Eur. J. Health Econ. 2017, 18, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Antoun, J.; Phillips, F.; Johnson, T. Post-Soviet Transition: Improving Health Services Delivery and Management. Mt. Sinai J. Med. A J. Transl. Pers. Med. 2011, 78, 436–448. [Google Scholar] [CrossRef] [PubMed]
- Miron, O. A radiography of the health system in Romania. Rev. De Știinte Politice 2020, VIII, 1–12. [Google Scholar]
- Bilan, I. Fiscal Consolidation as Alternative Public Debts Reduction Strategy in the EU Member States. In Proceedings of the International Conference on European Financial Regulation–EUFIRE, Iasi, Romania, 18–20 May 2017; pp. 40–53. [Google Scholar]
- Gavriluţă (Vatamanu), A.F.; Onofrei, M.; Cigu, E. Fiscal Decentralization and Inequality: An Analysis on Romanian Regions. Ekon. Cas. 2020, 68, 3–32. [Google Scholar]
| Indicators | Years | ||
|---|---|---|---|
| 2020 | 2021 * | 2022 * | |
| GDP % | −5.2 | 3.3 | 3.8 |
| Unemployment rate % | 5.9 | 6.2 | 5.1 |
| General government balance % GDP | −10.3 | −11.3 | −12.5 |
| Cyclically adjusted budget balance as a % of potential GDP | −8.6 | −9.9 | −11.5 |
| General government gross debt % GDP | 46.7 | 54.6 | 63.6 |
| Normative acts adopted in the context of the COVID pandemic (2020) | |||
| Military Ordinance | 9 | ||
| Emergency Government Ordinance | 10 | ||
| Government Decision | 25 | ||
| Factor Analysis/Correlation, Method: Principal Factors, Rotation: (Unrotated) | ||||
|---|---|---|---|---|
| Factor | Eigenvalue | Difference | Proportion | Cumulative |
| Factor1 | 7.70694 | 5.12482 | 0.6640 | 0.6640 |
| Factor2 | 2.58212 | 1.90516 | 0.2225 | 0.8864 |
| Factor3 | 0.67696 | 0.35902 | 0.0583 | 0.9447 |
| Factor4 | 0.31794 | 0.11200 | 0.0274 | 0.9721 |
| Factor5 | 0.20594 | 0.08267 | 0.0177 | 0.9899 |
| Factor6 | 0.12326 | 0.10286 | 0.0106 | 1.0005 |
| Factor7 | 0.02041 | 0.01044 | 0.0018 | 1.0022 |
| Factor8 | 0.00997 | 0.01200 | 0.0009 | 1.0031 |
| Factor9 | −0.00203 | 0.00474 | −0.0002 | 1.0029 |
| Factor10 | −0.00677 | 0.00431 | −0.0006 | 1.0023 |
| Factor11 | −0.01108 | 0.00506 | −0.0010 | 1.0014 |
| Factor12 | −0.01614 | −0.0014 | 1.0000 | |
| Unrotated Loadings | ||||
|---|---|---|---|---|
| F1 | F2 | Uniqueness | ||
| HE | 0.7813 | 0.1740 | 0.3593 | |
| MRB | −0.9895 | 0.1154 | 0.0076 | |
| PH | 0.8383 | −0.2166 | 0.2504 | |
| HB | −0.9295 | −0.0181 | 0.1357 | |
| CO2 | −0.8586 | −0.2395 | 0.2054 | |
| NOE | −0.9181 | −0.1555 | 0.1330 | |
| GH | −0.0434 | 0.9690 | 0.0592 | |
| NO | 0.1578 | 0.9644 | 0.0450 | |
| ISF | 0.8800 | −0.2825 | 0.1458 | |
| UP | 0.6725 | 0.5815 | 0.2097 | |
| LE | 0.9545 | −0.2361 | 0.0333 | |
| GDP | 0.8979 | −0.2591 | 0.1267 | |
| Factor | Variance | Difference | Proportion | Cumulative |
| F1 | 4.63553 | 1.11718 | 0.3994 | 0.3994 |
| F2 | 3.51836 | 1.11009 | 0.3031 | 0.7025 |
| F3 | 1.40826 | … | 0.1075 | 0.9099 |
| Variables | Deterministics | ADF | PP | ||
|---|---|---|---|---|---|
| t-stat | prob | t-stat | prob | ||
| Log real GDP per capita | None | 2.95 | (0.839) | 2.03 | (0.988) |
| Intercept | 0.54 | (0.592) | 0.73 | (0.467) | |
| Intercept and trend | −1.13 | (0.264) | −2.33 | (0.407) | |
| Log health expenditure per capita (HE) | None | 1.93 | (0.985) | 1.69 | (0.976) |
| Intercept | 0.56 | (0.574) | −0.66 | (0.508) | |
| Intercept and trend | −3.96 | (0.020) | −3.93 | (0.021) | |
| Unrestricted Cointegration Rank Test (Trace) | ||||
|---|---|---|---|---|
| Hypothesized | Trace | 0.05 | ||
| No. of CE(s) | Eigenvalue | Statistic | Critical Value | Prob. ** |
| None * | 0.444946 | 21.62329 | 15.49471 | 0.0053 |
| At most 1 | 0.083357 | 2.785185 | 3.841466 | 0.0951 |
| Unrestricted Cointegration Rank Test (Maximum Eigenvalue) | ||||
| Hypothesized | Max-Eigen | 0.05 | ||
| No. of CE(s) | Eigenvalue | Statistic | Critical Value | Prob. ** |
| None * | 0.444946 | 18.83810 | 14.26460 | 0.0088 |
| At most 1 | 0.083357 | 2.785185 | 3.841466 | 0.0951 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Onofrei, M.; Cigu, E.; Gavriluta, A.-F.; Bostan, I.; Oprea, F. Effects of the COVID-19 Pandemic on the Budgetary Mechanism Established to Cover Public Health Expenditure. A Case Study of Romania. Int. J. Environ. Res. Public Health 2021, 18, 1134. https://doi.org/10.3390/ijerph18031134
Onofrei M, Cigu E, Gavriluta A-F, Bostan I, Oprea F. Effects of the COVID-19 Pandemic on the Budgetary Mechanism Established to Cover Public Health Expenditure. A Case Study of Romania. International Journal of Environmental Research and Public Health. 2021; 18(3):1134. https://doi.org/10.3390/ijerph18031134
Chicago/Turabian StyleOnofrei, Mihaela, Elena Cigu, Anca-Florentina Gavriluta (Vatamanu), Ionel Bostan, and Florin Oprea. 2021. "Effects of the COVID-19 Pandemic on the Budgetary Mechanism Established to Cover Public Health Expenditure. A Case Study of Romania" International Journal of Environmental Research and Public Health 18, no. 3: 1134. https://doi.org/10.3390/ijerph18031134
APA StyleOnofrei, M., Cigu, E., Gavriluta, A.-F., Bostan, I., & Oprea, F. (2021). Effects of the COVID-19 Pandemic on the Budgetary Mechanism Established to Cover Public Health Expenditure. A Case Study of Romania. International Journal of Environmental Research and Public Health, 18(3), 1134. https://doi.org/10.3390/ijerph18031134










