Mental Health and Psychosocial Functioning in Recently Separated U.S. Women Veterans: Trajectories and Bi-Directional Relationships
Abstract
:1. Introduction
1.1. Mental Health and Psychosocial Functioning in Men
1.2. Mental Health and Psychosocial Functioning in Women
- How does women veterans’ mental health and psychosocial functioning change over time?
- How do deployment stressors and changes in mental health symptom severity affect changes in women veterans’ psychosocial functioning over time?
- Is there a bi-directional relationship between women veterans’ mental health symptom severity and psychosocial functioning?
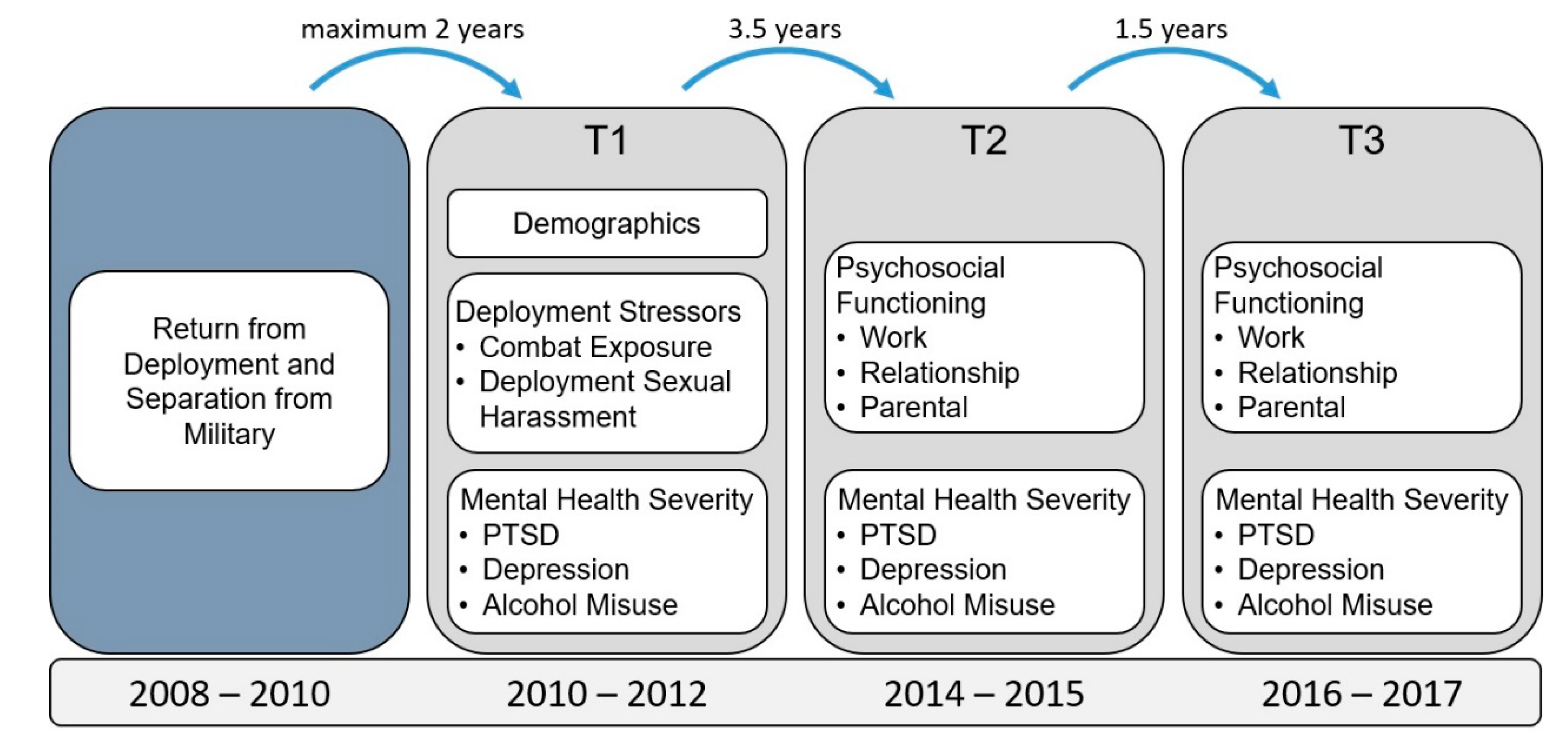
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Mental Health Conditions
2.2.2. Psychosocial Functioning
2.2.3. Deployment Stressors
2.3. Analyses
3. Results
3.1. Trajectories of Mental Health and Psychosocial Functioning
3.2. Effects of Mental Health and Deployment Stressors on Psychosocial Functioning
3.3. Effects of Psychosocial Functioning on Mental Health Symptom Severity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sayer, N.A.; Noorbaloochi, S.; Frazier, P.; Carlson, K.; Gravely, A.; Murdoch, M. Reintegration Problems and Treatment Interests Among Iraq and Afghanistan Combat Veterans Receiving VA Medical Care. Psychiatr. Serv. 2010, 61, 589–597. [Google Scholar] [CrossRef] [PubMed]
- Sayer, N.A.; Carlson, K.F.; Frazier, P.A. Reintegration Challenges in US Service Members and Veterans Following Combat Deployment. Soc. Issues Policy Rev. 2014, 8, 33–73. [Google Scholar] [CrossRef]
- Kleykamp, M. Unemployment, earnings and enrollment among post 9/11 veterans. Soc. Sci. Res. 2013, 42, 836–851. [Google Scholar] [CrossRef] [PubMed]
- Vogt, D.; Smith, B.N.; Fox, A.B.; Amoroso, T.; Taverna, E.; Schnurr, P.P. Consequences of PTSD for the work and family quality of life of female and male U.S. Afghanistan and Iraq War veterans. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Labor, U.S.D.O. Employment Situation of Veterans 2019; 2020. Available online: https://www.bls.gov/news.release/vet.nr0.htm (accessed on 18 January 2021).
- Washington, D.L.; Yano, E.M.; McGuire, J.; Hines, V.; Lee, M.; Gelberg, L. Risk factors for homelessness among women veterans. J. Health Care Poor Underserved 2010, 21, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Gamache, G.; Rosenheck, R.; Tessler, R. Overrepresentation of women veterans among homeless women. Am. J. Public Health 2003, 93, 1132–1136. [Google Scholar] [CrossRef] [PubMed]
- Adler-Baeder, F.; Pittman, J.; Taylor, L. The prevalence of marital transitions in military families. J. Divorce Remarriage 2005, 44, 91–106. [Google Scholar] [CrossRef]
- Department of Veterans Affairs, U.S. VetPop2014. 2014. Available online: https://www.va.gov/vetdata/veteran_population.asp (accessed on 18 January 2021).
- Department of Veterans Affairs, U.S. Women Veterans Report: The Past, Present, and Future of Women Veterans. Available online: https://www.va.gov/vetdata/veteran_population.asp (accessed on 3 June 2020).
- Adler, D.A.; Possemato, K.; Mavandadi, S.; Lerner, D.; Chang, H.; Klaus, J.; Tew, J.D.; Barrett, D.; Ingram, E.; Oslin, D.W. Psychiatric status and work performance of veterans of Operations Enduring Freedom and Iraqi Freedom. Psychiatr. Serv. 2011, 62, 39–46.12. [Google Scholar] [CrossRef]
- Erbes, C.R.; Kaler, M.E.; Schult, T.; Polusny, M.A.; Arbisi, P.A. Mental health diagnosis and occupational functioning in National Guard/Reserve veterans returning from Iraq. J. Rehabil. Res. Dev. 2011, 48, 1159–1170. [Google Scholar] [CrossRef]
- Allen, E.S.; Rhoades, G.K.; Stanley, S.M.; Markman, H.J. Hitting home: Relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. J. Fam. Psychol. 2010, 24, 280–288. [Google Scholar] [CrossRef] [Green Version]
- Gewirtz, A.H.; Polusny, M.A.; DeGarmo, D.S.; Khaylis, A.; Erbes, C.R. Posttraumatic stress symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. J. Consult. Clin. Psychol. 2010, 78, 599–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goff, B.S.; Crow, J.R.; Reisbig, A.M.; Hamilton, S. The impact of individual trauma symptoms of deployed soldiers on relationship satisfaction. J. Fam. Psychol. 2007, 21, 344–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pietrzak, R.H.; Goldstein, M.B.; Malley, J.C.; Rivers, A.J.; Southwick, S.M. Structure of posttraumatic stress disorder symptoms and psychosocial functioning in Veterans of Operations Enduring Freedom and Iraqi Freedom. Psychiatry Res. 2010, 178, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Shea, M.T.; Vujanovic, A.A.; Mansfield, A.K.; Sevin, E.; Liu, F. Posttraumatic stress disorder symptoms and functional impairment among OEF and OIF National Guard and Reserve veterans. J. Trauma. Stress 2010, 23, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.; Harpaz-Rotem, I.; Pietrzak, R.H.; Southwick, S.M. The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry 2012, 75, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Zivin, K.; Campbell, D.; Lanto, A.; Chaney, E.; Bolkan, C.; Bonner, L.; Miller, E.; Valenstein, M.; Waltz, T.; Rubenstein, L. Relationships between mood and employment over time among depressed VA primary care patients. Gen. Hosp. Psychiatry 2012, 34, 468–477. [Google Scholar] [CrossRef] [PubMed]
- Raab, P.A.; Mackintosh, M.A.; Gros, D.F.; Morland, L.A. Impact of comorbid depression on quality of life in male combat Veterans with posttraumatic stress disorder. J. Rehabil. Res. Dev. 2015, 52, 563–576. [Google Scholar] [CrossRef]
- Blow, A.J.; Gorman, L.; Ganoczy, D.; Kees, M.; Kashy, D.A.; Valenstein, M.; Marcus, S.M.; Fitzgerald, H.E.; Chermack, S. Hazardous drinking and family functioning in National Guard veterans and spouses postdeployment. J. Fam. Psychol. 2013, 27, 303–313. [Google Scholar] [CrossRef]
- Possemato, K.; Pratt, A.; Barrie, K.; Ouimette, P. Family Functioning in Recent Combat Veterans With Posttraumatic Stress Disorder and Alcohol Misuse. Traumatology 2015, 21, 267–272. [Google Scholar] [CrossRef]
- Smith, B.N.; Taverna, E.C.; Fox, A.B.; Schnurr, P.P.; Matteo, R.A.; Vogt, D. The Role of PTSD, Depression, and Alcohol Misuse Symptom Severity in Linking Deployment Stressor Exposure and Post-Military Work and Family Outcomes in Male and Female Veterans. Clin. Psychol. Sci. 2017, 5, 664–682. [Google Scholar] [CrossRef]
- Street, A.E.; Gradus, J.L.; Giasson, H.L.; Vogt, D.; Resick, P.A. Gender differences among veterans deployed in support of the wars in Afghanistan and Iraq. J. Gen. Intern. Med. 2013, 28 (Suppl. 2), S556–S562. [Google Scholar] [CrossRef] [Green Version]
- Street, A.E.; Vogt, D.; Dutra, L. A new generation of women veterans: Stressors faced by women deployed to Iraq and Afghanistan. Clin. Psychol. Rev. 2009, 29, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Ziobrowski, H.; Sartor, C.E.; Tsai, J.; Pietrzak, R.H. Gender differences in mental and physical health conditions in U.S. veterans: Results from the National Health and Resilience in Veterans Study. J. Psychosom. Res. 2017, 101, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Maguen, S.; Luxton, D.D.; Skopp, N.A.; Madden, E. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. J. Psychiatr. Res. 2012, 46, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Vogt, D.; Vaughn, R.; Glickman, M.E.; Schultz, M.; Drainoni, M.L.; Elwy, R.; Eisen, S. Gender differences in combat-related stressors and their association with postdeployment mental health in a nationally representative sample of U.S. OEF/OIF veterans. J. Abnorm. Psychol. 2011, 120, 797–806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schnurr, P.P.; Lunney, C.A. Work-related quality of life and posttraumatic stress disorder symptoms among female veterans. Women’s Health Issues Off. Publ. Jacobs Inst. Women’s Health 2011, 21 (Suppl. 4), S169–S175. [Google Scholar] [CrossRef] [PubMed]
- Creech, S.K.; Swift, R.; Zlotnick, C.; Taft, C.; Street, A.E. Combat exposure, mental health, and relationship functioning among women veterans of the Afghanistan and Iraq wars. J. Fam. Psychol. 2016, 30, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Conybeare, D.; Behar, E.; Solomon, A.; Newman, M.G.; Borkovec, T.D. The PTSD Checklist-Civilian Version: Reliability, validity, and factor structure in a nonclinical sample. J. Clin. Psychol. 2012, 68, 699–713. [Google Scholar] [CrossRef]
- Keen, S.M.; Kutter, C.J.; Niles, B.L.; Krinsley, K.E. Psychometric properties of PTSD Checklist in sample of male veterans. J. Rehabil. Res. Dev. 2008, 45, 465–474. [Google Scholar] [CrossRef]
- Weathers, F.; Litz, B.; Herman, D.; Huska, J.; Keane, T. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility; Annual Convention of the International Society for Traumatic Stress Studies: San Antonio, TX, USA, 1993. [Google Scholar]
- Wilkins, K.C.; Lang, A.J.; Norman, S.B. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress Anxiety 2011, 28, 596–606. [Google Scholar] [CrossRef] [Green Version]
- Yeager, D.E.; Magruder, K.M.; Knapp, R.G.; Nicholas, J.S.; Frueh, B.C. Performance characteristics of the posttraumatic stress disorder checklist and SPAN in Veterans Affairs primary care settings. Gen. Hosp. Psychiatry 2007, 29, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Cavalieri, T.A.; Leonard, D.M.; Beck, A.T. Use of the Beck Depression Inventory for Primary Care to screen for major depression disorders. Gen. Hosp. Psychiatry 1999, 21, 106–111. [Google Scholar] [CrossRef]
- Beck, A.; Guth, D.; Steer, R.; Ball, R. Screening for major depression disorders in medical inpatients with the Beck Depression Inventory for Primary Care. Behav. Res. Ther. 1997, 35, 785–791. [Google Scholar] [CrossRef]
- Beck, A.; Steer, R.; Ball, R.; Ciervo, C.; Kabat, M. Use of the Beck Anxiety and Depression Inventories for Primary Care with Medical Outpatients. Assessment 1997, 4, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Hays, R.; Merz, J.; Nicholas, R. Response burden, reliability, and validity of the CAGE, short MAST and AUDIT alcohol screening measures. Behav. Res. Methods Instrum. Comput. 1995, 27, 277–280. [Google Scholar] [CrossRef]
- Reinert, D.F.; Allen, J.P. The alcohol use disorders identification test: An update of research findings. Alcohol. Clin. Exp. Res. 2007, 31, 185–199. [Google Scholar] [CrossRef]
- Bohn, M.; Babor, T.; Kranzler, H. The Alcohol Use Disorders Identification Test (AUDIT): Validation of a screening instrument for use in medical settings. J. Stud. Alcohol. 1995, 56, 423–432. [Google Scholar] [CrossRef]
- Kriston, L.; Holzel, L.; Weiser, A.K.; Berner, M.M.; Harter, M. Meta-analysis: Are 3 questions enough to detect unhealthy alcohol use? Ann. Intern. Med. 2008, 149, 879–888. [Google Scholar] [CrossRef]
- Crawford, E.F.; Fulton, J.J.; Swinkels, C.M.; Beckham, J.C.; Calhoun, P.S.; VA Mid-Atlantic MIRECC OEF/OIF Registry Workgroup. Diagnostic efficiency of the AUDIT-C in U.S. veterans with military service since September 11, 2001. Drug Alcohol Depend. 2013, 132, 101–106. [Google Scholar] [CrossRef]
- Bradley, K.A.; Bush, K.R.; Epler, A.J.; Dobie, D.J.; Davis, T.M.; Sporleder, J.L.; Maynard, C.; Burman, M.L.; Kivlahan, D.R. Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Arch. Intern. Med. 2003, 163, 821–829. [Google Scholar] [CrossRef] [Green Version]
- Ewing, J. Detecting alcoholism: The CAGE Questionnaire. J. Am. Med Assoc. 1984, 252, 1905–1907. [Google Scholar] [CrossRef]
- Mayfield, D.; McLeod, O.; Hall, P. The CAGE questionnaire: Validation of a new alcoholism screening instrument. Am. J. Psychiatry 1974, 131, 1121–1123. [Google Scholar] [PubMed]
- Dhalla, S.; Kopec, J.A. The CAGE questionnaire for alcohol misuse: A review of reliability and validity studies. Clin. Investig. Med. 2007, 30, 33–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smart, R.G.; Adlaf, E.M.; Knoke, D. Use of the CAGE scale in a population survey of drinking. J. Stud. Alcohol 1991, 52, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Skogen, J.C.; Overland, S.; Knudsen, A.K.; Mykletun, A. Concurrent validity of the CAGE questionnaire. The Nord-Trondelag Health Study. Addict. Behav. 2011, 36, 302–307. [Google Scholar] [CrossRef]
- Schwab, K.A.; Ivins, B.; Cramer, G.; Johnson, W.; Sluss-Tiller, M.; Kiley, K.; Lux, W.; Warden, D. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: Initial investigation of the usefulness of a short screening tool for traumatic brain injury. J. Head Trauma Rehabil. 2007, 22, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Bovin, M.J.; Black, S.K.; Rodriguez, P.; Lunney, C.A.; Kleiman, S.E.; Weathers, F.W.; Schnurr, P.P.; Spira, J.; Keane, T.M.; Marx, B.P. Development and validation of a measure of PTSD-related psychosocial functional impairment: The Inventory of Psychosocial Functioning. Psychol. Serv. 2018, 15, 216–229. [Google Scholar] [CrossRef] [PubMed]
- Holowka, D.; Marx, B. Assessing PTSD-related functional impairment and quality of life. In The Oxford Handbook of Traumatic Stress Disorders; Beck, J., Sloan, D., Eds.; Oxford University Press: Oxford, UK, 2012; pp. 315–330. [Google Scholar]
- McQuaid, J.R.; Marx, B.P.; Rosen, M.I.; Bufka, L.F.; Tenhula, W.; Cook, H.; Keane, T.M. Mental health assessment in rehabilitation research. J. Rehabil. Res. Dev. 2012, 49, 121–138. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, P.; Holowka, D.W.; Marx, B.P. Assessment of posttraumatic stress disorder-related functional impairment: A review. J. Rehabil. Res. Dev. 2012, 49, 649–665. [Google Scholar] [CrossRef] [PubMed]
- Maoz, H.; Goldwin, Y.; Lewis, Y.D.; Bloch, Y. Exploring Reliability and Validity of the Deployment Risk and Resilience Inventory-2 Among a Nonclinical Sample of Discharged Soldiers Following Mandatory Military Service. J. Trauma. Stress 2016, 29, 556–562. [Google Scholar] [CrossRef] [Green Version]
- Vogt, D.; Smith, B.N.; King, L.A.; King, D.W.; Knight, J.; Vasterling, J.J. Deployment risk and resilience inventory-2 (DRRI-2): An updated tool for assessing psychosocial risk and resilience factors among service members and veterans. J. Trauma. Stress 2013, 26, 710–717. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows, Version 26.0; IBM Corp: Armonk, NY, USA, 2019. [Google Scholar]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- Resnick, E.M.; Mallampalli, M.; Carter, C.L. Current challenges in female veterans’ health. J. Womens Health 2012, 21, 895–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerber, M.R.; King, M.W.; Iverson, K.M.; Pineles, S.L.; Haskell, S.G. Association Between Mental Health Burden and Coronary Artery Disease in US Women Veterans Over 45: A National Cross-Sectional Study. J. Women’s Health 2018, 27, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Zivin, K.; Yosef, M.; Miller, E.M.; Valenstein, M.; Duffy, S.; Kales, H.C.; Vijan, S.; Kim, H.M. Associations between depression and all-cause and cause-specific risk of death: A retrospective cohort study in the Veterans Health Administration. J. Psychosom. Res. 2015, 78, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Adler, D.A.; McLaughlin, T.J.; Rogers, W.H.; Chang, H.; Lapitsky, L.; Lerner, D. Job performance deficits due to depression. Am. J. Psychiatry 2006, 163, 1569–1576. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, M.H.; Morris, D.W.; Wisniewski, S.R.; Lesser, I.; Nierenberg, A.A.; Daly, E.; Kurian, B.T.; Gaynes, B.N.; Balasubramani, G.K.; Rush, A.J. Increase in work productivity of depressed individuals with improvement in depressive symptom severity. Am. J. Psychiatry 2013, 170, 633–641. [Google Scholar] [CrossRef]
- Beck, A.; Crain, L.A.; Solberg, L.I.; Unutzer, J.; Maciosek, M.V.; Whitebird, R.R.; Rossom, R.C. The effect of depression treatment on work productivity. Am. J. Manag. Care 2014, 20, e294–e301. [Google Scholar]
- Sienkiewicz, M.E.; Amalathas, A.; Iverson, K.M.; Smith, B.N.; Mitchell, K.S. Examining the association between trauma exposure and work-related outcomes in women veterans. Int. J. Environ. Res. Public Health 2020, 17, 4585. [Google Scholar] [CrossRef]
- Bell, M.E.; Reardon, A. Experiences of sexual harassment and sexual assault in the military among OEF/OIF veterans: Implications for health care providers. Soc. Work Health Care 2011, 50, 34–50. [Google Scholar] [CrossRef]
- Bell, M.E.; Dardis, C.M.; Vento, S.A.; Street, A.E. Victims of sexual harassment and sexual assault in the military: Understanding risks and promoting recovery. Mil. Psychol. 2018, 30, 219–228. [Google Scholar] [CrossRef]
- Davis, L.L.; Kyriakides, T.C.; Suris, A.M.; Ottomanelli, L.A.; Mueller, L.; Parker, P.E.; Resnick, S.G.; Toscano, R.; Scrymgeour, A.A.; Drake, R.E.; et al. Support Toward Advancing Recovery, I., Effect of Evidence-Based Supported Employment vs Transitional Work on Achieving Steady Work Among Veterans With Posttraumatic Stress Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2018, 75, 316–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mueller, L.; Wolfe, W.R.; Neylan, T.C.; McCaslin, S.E.; Yehuda, R.; Flory, J.D.; Kyriakides, T.C.; Toscano, R.; Davis, L.L. Positive impact of IPS supported employment on PTSD-related occupational-psychosocial functional outcomes: Results from a VA randomized-controlled trial. Psychiatr. Rehabil. J. 2019, 42, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Plaisier, I.; de Graaf, R.; de Bruijn, J.; Smit, J.; van Dyck, R.; Beekman, A.; Penninx, B. Depressive and anxiety disorders on-the-job: The importance of job characteristics for good work functioning in persons with depressive and anxiety disorders. Psychiatry Res. 2012, 200, 382–388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heinz, A.J.; Meffert, B.N.; Halvorson, M.A.; Blonigen, D.; Timko, C.; Cronkite, R. Employment characteristics, work environment, and the course of depression over 23 years: Does employment help foster resilience? Depress Anxiety 2018, 35, 861–867. [Google Scholar] [CrossRef] [PubMed]
| Mental Health Variable | Work | Relationship | Parental | |||
| B (95% CI) | p | B (95% CI) | p | B (95% CI) | p | |
| Unadjusted | ||||||
| PTSD | 0.244 (0.067, 0.420) | 0.007 * | 0.128 (−0.027, 0.283) | 0.105 | 0.178 (0.032, 0.323) | 0.017 * |
| Depression | 0.384 (0.126, 0.641) | 0.004 * | 0.433 (0.188, 0.679) | 0.001 * | 0.230 (−0.012, 0.473) | 0.063 |
| Alcohol Misuse | 0.229 (−0.572, 1.029) | 0.574 | 0.135 (−0.597, 0.865) | 0.717 | 0.169 (−0.535, 0.872) | 0.636 |
| Combat Exposure | −0.351 (−0.645, −0.058) | 0.019 * | −0.377 (−0.596, −0.158) | 0.000 * | −0.258 (−0.450, −0.065) | 0.009 * |
| Sexual Harassment | −0.882 (−1.340, −0.424) | <0.001 * | −0.639 (−1.042, −0.235) | 0.002 * | −0.459 (−0.787, −0.131) | 0.006 * |
| Adjusted for Covariates | ||||||
| PTSD | 0.338 (0.154, 0.520) | <0.001 * | 0.235 (0.068, 0.402) | 0.006 * | 0.286 (0.135, 0.438) | <0.001 * |
| Depression | 0.397 (0.141, 0.652) | 0.003 * | 0.471 (0.227, 0.716) | <0.001 * | 0.215 (−0.020, 0.451) | 0.073 |
| Alcohol Misuse | 0.572 (−0.282, 1.425) | 0.188 | 0.449 (−0.316, 1.212) | 0.249 | 0.664 (−0.081, 1.407) | 0.080 |
| Mental Health Variable | Work | Relationship | Parental | |||
| B | 95% CI | B | 95% CI | B | 95% CI | |
| Unadjusted | ||||||
| PTSD | 0.145 | −0.048, 0.337 | 0.024 | −0.152, 0.199 | 0.156 | −0.006, 0.319 |
| Depression | 0.320 | 0.037, 0.603 * | 0.386 | 0.108, 0.666 * | 0.157 | −0.112, 0.427 |
| Alcohol Misuse | 0.171 | −0.629, 0.973 | −0.100 | −0.846, 0.643 | −0.031 | −0.786, 0.719 |
| Adjusted for Covariates | ||||||
| PTSD | 0.218 | 0.016, 0.420 * | 0.143 | −0.047, 0.334 | 0.280 | 0.111, 0.450 * |
| Depression | 0.296 | 0.023, 0.568 * | 0.336 | 0.062, 0.610 * | 0.055 | −0.200, 0.311 |
| Alcohol Misuse | 0.470 | −0.387, 1.326 | 0.190 | −0.587, 0.965 | 0.429 | −0.373, 1.229 |
| Combat Exposure | −0.299 | −0.591, −0.009 * | −0.343 | −0.587, −0.099 * | −0.205 | −0.410, −0.001 |
| Sexual Harassment | −0.850 | −1.433, −0.267 * | −0.768 | −1.317, −0.217 * | −0.762 | −1.199, −0.324 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawrence, K.A.; Vogt, D.; Dugan, A.J.; Nigam, S.; Slade, E.; Smith, B.N. Mental Health and Psychosocial Functioning in Recently Separated U.S. Women Veterans: Trajectories and Bi-Directional Relationships. Int. J. Environ. Res. Public Health 2021, 18, 935. https://doi.org/10.3390/ijerph18030935
Lawrence KA, Vogt D, Dugan AJ, Nigam S, Slade E, Smith BN. Mental Health and Psychosocial Functioning in Recently Separated U.S. Women Veterans: Trajectories and Bi-Directional Relationships. International Journal of Environmental Research and Public Health. 2021; 18(3):935. https://doi.org/10.3390/ijerph18030935
Chicago/Turabian StyleLawrence, Karen A., Dawne Vogt, Adam J. Dugan, Shawn Nigam, Emily Slade, and Brian N. Smith. 2021. "Mental Health and Psychosocial Functioning in Recently Separated U.S. Women Veterans: Trajectories and Bi-Directional Relationships" International Journal of Environmental Research and Public Health 18, no. 3: 935. https://doi.org/10.3390/ijerph18030935






