Participatory Action Research Applied to an Ear, Nose, and Throat Specialty Service Redesign in Remote Australia: A Mixed-Methods Study of Key Stakeholder Perspectives
Abstract
1. Introduction
1.1. Evidence Base
1.2. Current Service Delivery Model of Care for ENT
2. Materials and Methods
2.1. Initial PHC Staff Perspective Survey
2.2. Stakeholder Open Forum and Follow-up Survey
2.3. Data Collection and Analysis
2.4. Ethics
3. Results
3.1. PHC Staff Perspective Survey
3.1.1. Assessing, Diagnosing, and Management of Ear Conditions
3.1.2. Telehealth
3.1.3. Training and Further Education in Ear and Hearing Health
3.2. Stakeholder Forum and Follow-up Survey
3.2.1. Theme 1: Training for Health Workers in ENT Management
3.2.2. Theme 2: Improve Local Service Access
3.2.3. Theme 3: New Referral Pathways to Improve Continuity of Care
3.2.4. Theme 4: Introduction to Telehealth
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Survey Multiple Choice Options (Number of Responses) | N (%) |
|---|---|
| Demographics of Respondents | |
| Q1 Current working role in Cape York (n = 19) | |
| Clinical Nurse | 8 (42%) |
| Medical Officer | 3 (16%) |
| Indigenous Health Worker | 2 (11%) |
| Nursing Manager | 2 (11%) |
| Audiologist | 1 (5%) |
| Visiting Specialist | 1 (5%) |
| Other (please specify) | 2 (11%) |
| Q2 Length in current role (n = 19) | |
| ≤3 months | 1 (5%) |
| 3–6 months | 0 (0%) |
| 7–12 months | 1 (5%) |
| 13 months–5 years | 13 (68%) |
| ≥6 years | 4 (21%) |
| Community Ear and Hearing Health Process Review | |
| Q3 Work for any of the following primary health care providers? (n = 17) | |
| Torres and Cape Hospital Health Service | 9 (53%) |
| Apunipima Cape York Health Council | 7 (41%) |
| Royal Flying Doctor Service | 3 (18%) |
| Deadly Ears Program | 1 (6%) |
| Q4 Equipment used to asses ear and hearing health (n = 18) | |
| Otoscope | 18 (100%) |
| Tympanometer | 13 (72%) |
| Audiometer | 6 (33%) |
| Video otoscope | 3 (17%) |
| Flexicam otoscope | 0 (0%) |
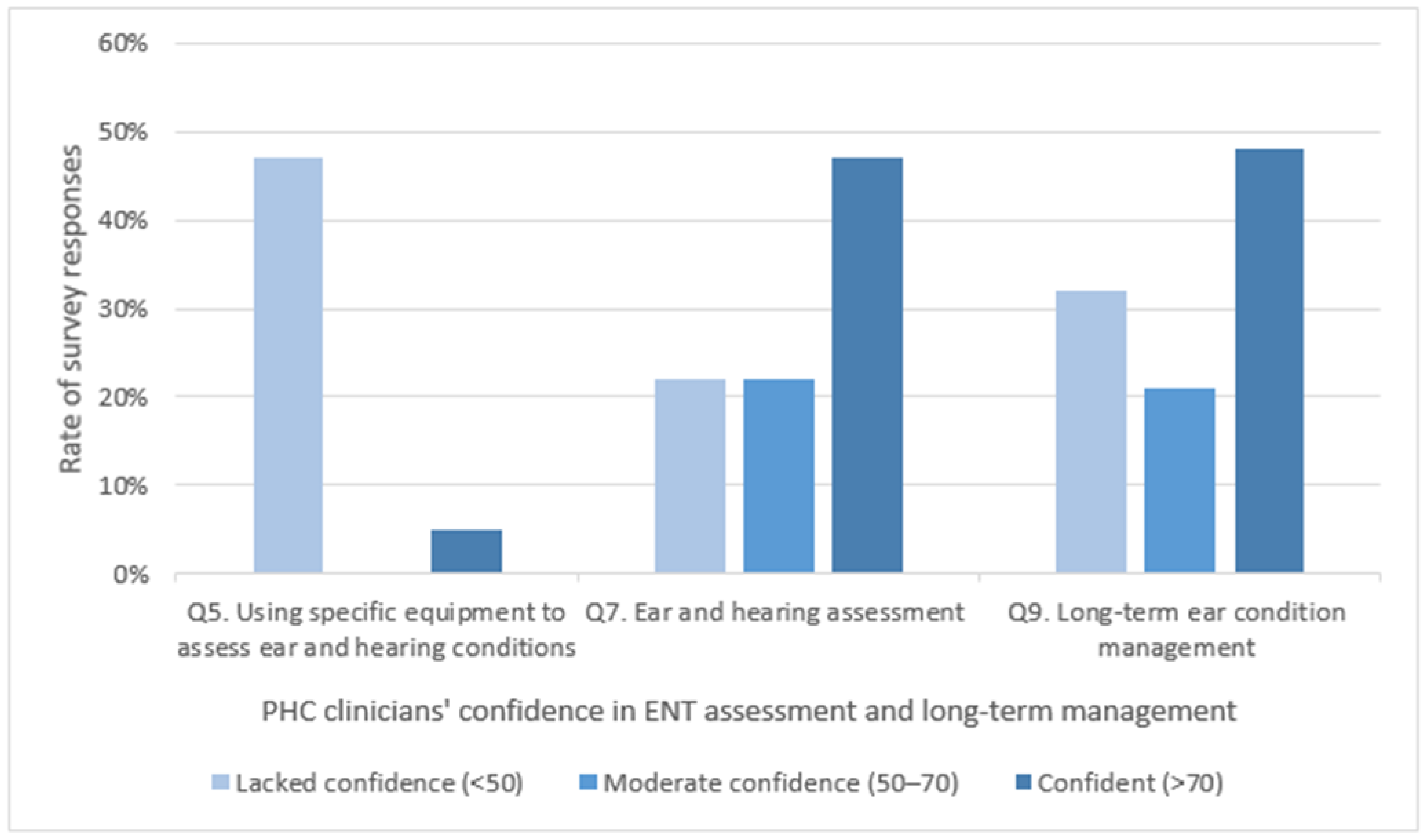
| Q5. Lack of confidence using specific equipment (n = 19) | |
| Audiometer | 9 (47%) |
| Tympanometer | 9 (47%) |
| Otoscope | 8 (42%) |
| Video otoscope | 8 (42%) |
| Flexicam otoscope | 8 (42%) |
| None—I am confident using all equipment | 1 (5%) |
| Q6 Clinical care guidelines used when reviewing ear or hearing presentations (n = 19) | |
| Primary clinical care manual | 17 (90%) |
| Clinical care guidelines for treatment of otitis media in Aboriginal & Torres Strait Islander populations | 8 (42%) |
| Clinical judgement | 7 (37%) |
| Therapeutic guidelines | 4 (21%) |
| Deadly Ears guidelines and protocols | 2 (11%) |
| Central Australian Rural Practitioners Association | 1 (5%) |
| Clinical Prioritisation Criteria | 0 (0%) |
| Q7 Confidence in making ear/hearing assessments (n = 18) | |
| Not confident (<20) | 2 (11%) |
| Not very confident (20–50) | 2 (11%) |
| A little confident (51–70) | 4 (22%) |
| Quite confident (71–90) | 7 (40%) |
| Very confident (>90) | 3 (7%) |
| Q8 Conditions you’re unsure of in your ear assessments (n = 18) | |
| Otitis media effusion | 8 (44%) |
| Acute otitis media | 4 (22%) |
| Acute otitis media without perforation | 4 (22%) |
| Acute otitis media with perforation | 4 (22%) |
| Chronic suppurative otitis media | 4 (22%) |
| Dry perforation | 4 (22%) |
| None—confident in all assessments | 6 (33%) |
| Other (exostosis/osteoma n = 1; early cholesteatoma n = 1) | 2 (11%) |
| Q9 Confidence in long-term ear condition management (n = 19) | |
| Not confident (<20) | 3 (16%) |
| Not very confident (20–50) | 3 (16%) |
| A little confident (51–70) | 4 (21%) |
| Quite confident (71–90) | 6 (32%) |
| Very confident (>90) | 3 (16%) |
| Q10 Lack of confidence in managing conditions (n = 16) | |
| Otitis media with effusion | 4 (25%) |
| Acute otitis media with perforation | 3 (19%) |
| Chronic suppurative otitis media | 3 (19%) |
| Dry perforation | 3 (19%) |
| Acute otitis media | 2 (13%) |
| Acute otitis media without perforation | 2 (13%) |
| None—I’m confident in all of them | 8 (50%) |
| Q11 Reasons for referral to medical or ENT specialist for advice (n = 19) | |
| To refer for surgery | 15 (79%) |
| For a second opinion on a clinical decision | 14 (74%) |
| To take over patient ear condition management | 12 (63%) |
| For ear condition management advice | 12 (63%) |
| Other (if not seen in timely manner) | 1 (5%) |
| Q12 Telehealth for ENT consults (n = 16) | |
| I consider they would be well received | 13 (81%) |
| No—I don’t think they would be well received | 3 (19%) |
| Q13 Would community members (patient/carers) welcome Ear Health information to take home? (n = 17) | |
| I consider this would be well received | 10 (83%) |
| No—I don’t consider they would be well received | 2 (17%) |
| Q14 Face-to-face ear and hearing training for PHC clinicians (n = 19) | |
| Yes | 16 (84%) |
| No | 0 (0%) |
| Other | 3 (16%) |
| Q15 Specifically, what training interests you (n = 15) | |
| Ear suctioning and tympanometry | 15 (100%) |
| Long-term community management of otitis media | 12 (80%) |
| How and when to seek specialist ENT input (referral) | 11 (73%) |
| Use of current guidelines for treatment and management of ear disease | 11 (73%) |
| Identification of different otitis media conditions | 9 (60%) |
| All of the above | 2 (13%) |
References
- Australian Bureau of Statistics. Australian Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, 2012–2013; Australian Bureau of Statistics: Canberra, Australia, 2013.
- Gruen, R.L.; Bailie, R.S.; Wang, Z.; Heard, S.; O’Rourke, I.C. Specialist outreach to isolated and disadvantaged communities: A population-based study. Lancet 2006, 368, 130–138. [Google Scholar] [CrossRef]
- Wakerman, J.; Humphreys, J.S.; Wells, R.; Kuipers, P.; Entwistle, P.; Jones, J. Primary health care delivery models in rural and remote Australia: A systematic review. BMC Health Serv. Res. 2008, 8, 276. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Population by Age and Sex, Regions of Australia. In Regional Population Growth, Australia, 2013–2014; Australian Bureau of Statistics: Canberra, Australia, 2014. [Google Scholar]
- Gunasekera, H.; Morris, P.S.; Daniels, J.; Couzos, S.; Craig, J.C. Otitis media in Aboriginal children: The discordance between burden of illness and access to services in rural/remote and urban Australia. J. Paediatr. Child Health 2009, 45, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Begg, S.; Bright, M.; Harper, C. Burden of Disease and Injury, Life Expectancy and Health-Adjusted Life Expectancy in Queensland Health Service Districts, 2006; Queensland Health: Brisbane, Australia, 2009. [Google Scholar]
- Jacups, S.P.; Newman, D.; Dean, D.; Richards, A.; McConnon, K.M. An innovative approach to improve ear, nose and throat surgical access for remote living Cape York Indigenous children. Int. J. Pediatr. Otorhinolaryngol. 2017, 100, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Children’s Health Queensland Hospital and Health Service. Deadly Ears; 2020. Available online: https://www.childrens.health.qld.gov.au/chq/our-services/community-health-services/deadly-ears/ (accessed on 12 November 2020).
- Children’s Health Queensland Hospital and Health Service. Deadly Ears Program; 2020. Available online: https://www.childrens.health.qld.gov.au/service-deadly-ears-program/ (accessed on 12 November 2020).
- Free Map Tools. Measure a Distance. n.d. Available online: https://www.freemaptools.com/measure-distance.htm (accessed on 12 November 2020).
- Jacups, P.S.; McConnon, K.M. Reducing ear, nose and throat (ENT) waitlists: Implications of a referral audit. Health Policy 2019, 123, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Queensland Government. Waiting Lists. Hospital Care, Surgical Procedures and Waiting Lists. 2015. Available online: https://www.qld.gov.au/health/services/hospital-care/waiting-lists (accessed on 12 November 2020).
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Health 2006, 60, 854–857. [Google Scholar] [CrossRef]
- Andersson, N. Participatory research—A modernizing science for primary health care. J. General Fam. Med. 2018, 19, 154–159. [Google Scholar] [CrossRef]
- Harris, J.; Cook, T.; Gibbs, L.; Oetzel, J.; Salsberg, J.; Shinn, C.; Springett, J.; Wallerstein, N.; Wright, M. Searching for the Impact of Participation in Health and Health Research: Challenges and Methods. Biomed. Res. Int. 2018, 2018. [Google Scholar] [CrossRef]
- Boote, J.; Wong, R.; Booth, A. Talking the talk or walking the walk? A bibliometric review of the literature on public involvement in health research published between 1995 and 2009. Health Expect 2015, 18, 44–57. [Google Scholar] [CrossRef]
- Feldmann, J.; Puhan, M.A.; Mütsch, M. Characteristics of stakeholder involvement in systematic and rapid reviews: A methodological review in the area of health services research. BMJ Open 2019, 9, e024587. [Google Scholar] [CrossRef]
- Kokesh, J.; Ferguson, A.S.; Patricoski, C. Telehealth in Alaska: Delivery of health care services from a specialist’s perspective. Int. J. Circumpolar Health 2004, 63, 387–400. [Google Scholar] [CrossRef]
- Kokesh, J.; Ferguson, A.S.; Patricoski, C. Preoperative planning for ear surgery using store-and-forward telemedicine. Otolaryngol. Head Neck Surg. 2010, 143, 253–257. [Google Scholar] [CrossRef]
- Smith, A.C.; Armfield, N.R.; Wu, W.I.; Brown, C.A.; Perry, C. A mobile telemedicine-enabled ear screening service for Indigenous children in Queensland: Activity and outcomes in the first three years. J. Telemed. Telecare 2012, 18, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Wakerman, J. Innovative rural and remote primary health care models: What do we know and what are the research priorities? Aust. J. Rural Health 2009, 17, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.S.; Clapin, M. Ear health of aboriginal primary school children in the Eastern Goldfields Region. of Western Australia. Aust. J. Public Health 1992, 16, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Reeve, C.; Thomas, A.; Mossenson, A.; Reeve, D.; Davis, S. Evaluation of an ear health pathway in remote communities: Improvements in ear health access. Aust. J. Rural Health 2014, 22, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.; Gasser, L.; Blignault, I.; Collins, R. Taking telehealth to the bush: Lessons from north Queensland. J. Telemed. Telecare 2001, 7, 20–23. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Ethical Considerations in Quality Assurance and Evaluation Activities; Australian Government: Canberra, Australia, 2014.
- Hofstetter, P.J.; Kokesh, J.; Ferguson, A.S.; Hood, L.J. The Impact of Telehealth on Wait Time for ENT Specialty Care. Telemed. E-Health 2010, 16, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Elliott, G.; Smith, A.C.; Bensink, M.E.; Brown, C.; Stewart, C.; Perry, C.; Scuffham, P. The feasibility of a community-based mobile telehealth screening service for Aboriginal and Torres Strait Islander children in Australia. Telemed. J. E-Health 2010, 16, 950–956. [Google Scholar] [CrossRef]
- Caffery, L.J.; Farjian, M.; Smith, A.C. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: A scoping review. J. Telemed. Telecare 2016, 22, 504–512. [Google Scholar] [CrossRef]
- Jacups, S.P.; Kinchin, I.; McConnon, K.M. Ear, nose, and throat surgical access for remote living Indigenous children: What is the least costly model? J. Eval. Clin. Pract. 2018, 24, 1330–1338. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, J.; Tan, P.L.; Hoverman, S.; Baldwin, C. The value and limitations of Participatory Action Research methodology. J. Hydrol. 2012, 474, 11–21. [Google Scholar] [CrossRef]

| Survey Question | Additional Comments |
|---|---|
| Q12 Telehealth | “Rather than travelling for a consult this prepares families to make better decision & choices for themselves about ENT services” |
| Q14 and Q15 Training and Further Education | “Need for continual training and support for staff—also new staff training” “Those attending [a training session] should have ear health included in their clinical practice post-training and have strategic plans for using the training” |
| Free text | “[There is a] lack of ENT service… delays in ENT services… lack of coordination of ENT services… [and] lack of evidence of ENT interventions” “Need to improve communication from leaders to clinicians, also, intra-agency communication between service providers regarding ENT services in the Cape. Improvements in communication will assist clinicians on the ground know what is happening and to avoid duplication of services” |
| Identified Gaps/Barriers in Ear and Hearing Service Delivery | Rate of Agreeance by Follow-up Survey Respondents (%) |
|---|---|
| Administration systems poorly functioning, i.e., referrals, appointment processes | 88% |
| Ear pathology difficult in PHC setting, making diagnosis by PHC clinicians poor | 71% |
| Ear condition management not always adhered to by PHC clinicians | 71% |
| Telehealth not well supported by PHC clinicians | 53% |
| Specialist recommendations not adhered to by PHC clinicians | 41% |
| Other | 41% |
| Identified Gaps/Barriers in Ear and Hearing Service Delivery | Potential Solutions |
|---|---|
| Theme 1: Training for health workers in ENT management | |
| “Poor diagnostics skills in community for ear conditions- therefore inappropriate management” | “More health workers and nurses properly trained at ground level” “Appropriate management and hearing health promotion funded more extensively and given more recognition of need” |
| Theme 2: Improve local service access | |
| “As a PHC GP I found that the service provision has been so infrequent that we basically have no ENT service in Cape York. Therefore all my clients are referred to Cairns which is sometimes very difficult for my patients to attend and they miss appointments” | “Regular visits by outreach specialists with the possibility to discuss in person regular review or follow up of the patients seen clear advice how to continue management or treatment” “More regular visits to build rapport with communities so that recs are more likely to be followed” |
| Theme 3: New referral pathways to improve continuity of care | |
| “Present referrals, appointments, telehealth, and clinical data storage, all fallible” “PHC care plans not being followed—Staff not recording information, such as commencement of procedures (dry mopping)… Filing of documentation, evidence of referrals, care paths, consultations etc. in patient’s medical notes” “Challenging getting feedback when multiple services work in one community including some duplications in service. Only one audiologist employed by Apunipima means she’s extremely stretched and there’s a delay getting results of screening tests. Difficult to get feedback on clients seen by Australian hearing re: plan for follow up etc.” | “A regular service that is well coordinated with systems aligning with current processes, communication of case management needs to be completed from referral, review, management, follow-up and discharge.” “Soon to roll out checklist which is aimed at addressing [lack of patient information]” “Local review & theatre—increases compliance of patients attending appointments/operations. Maintains skills of local clinicians” |
| Theme 4: Introduction to telehealth | |
| “[ENT] services should be supported via telehealth but with lack of appropriate clinical support, turnover of staff, need for specialist equipment etc. implementation is proving difficult at this time.” | “More telehealth with images sent from appropriate machines giving good images. Possibly an email link to consultants for guidance regarding management and a regular outreach audiometry service” “Telehealth training: take otoscopic images and send them for review…ENT/specialist who reviews them can be anywhere… Train staffed to use digital otoscope and take pictures—less reliance on diagnostic skills” |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jacups, S.P.; Kinchin, I.; Edwards, L. Participatory Action Research Applied to an Ear, Nose, and Throat Specialty Service Redesign in Remote Australia: A Mixed-Methods Study of Key Stakeholder Perspectives. Int. J. Environ. Res. Public Health 2021, 18, 167. https://doi.org/10.3390/ijerph18010167
Jacups SP, Kinchin I, Edwards L. Participatory Action Research Applied to an Ear, Nose, and Throat Specialty Service Redesign in Remote Australia: A Mixed-Methods Study of Key Stakeholder Perspectives. International Journal of Environmental Research and Public Health. 2021; 18(1):167. https://doi.org/10.3390/ijerph18010167
Chicago/Turabian StyleJacups, Susan P., Irina Kinchin, and Layla Edwards. 2021. "Participatory Action Research Applied to an Ear, Nose, and Throat Specialty Service Redesign in Remote Australia: A Mixed-Methods Study of Key Stakeholder Perspectives" International Journal of Environmental Research and Public Health 18, no. 1: 167. https://doi.org/10.3390/ijerph18010167
APA StyleJacups, S. P., Kinchin, I., & Edwards, L. (2021). Participatory Action Research Applied to an Ear, Nose, and Throat Specialty Service Redesign in Remote Australia: A Mixed-Methods Study of Key Stakeholder Perspectives. International Journal of Environmental Research and Public Health, 18(1), 167. https://doi.org/10.3390/ijerph18010167






