Burnout Assessment Tool (BAT)—Development, Validity, and Reliability
Abstract
1. Introduction
- Formulate an alternative conceptualization of burnout, which is comprehensive in nature and includes all relevant elements that are associated with burnout as conceived by practitioners.
- Develop—based on this new conceptualization—a novel questionnaire that is psychometrically sound and practically useful for the assessment of burnout, dubbed Burnout Assessment Tool (BAT).
2. Part 1: Conceptualization and Constructing of the BAT
2.1. Phase 1. Redefining Burnout
2.1.1. Method
2.1.2. Results
2.2. Phase 2. Item Formulation
2.2.1. Method
2.2.2. Results
3. Part 2: Validity and Reliability of the BAT
3.1. Method
3.1.1. Participants
3.1.2. Measures
3.1.3. Data Analysis
3.1.4. Results
Factorial Validity: Exploring the Factor Structure
Factorial Validity: Confirming the Factor Structure
3.1.5. Reliability
3.1.6. Construct Validity
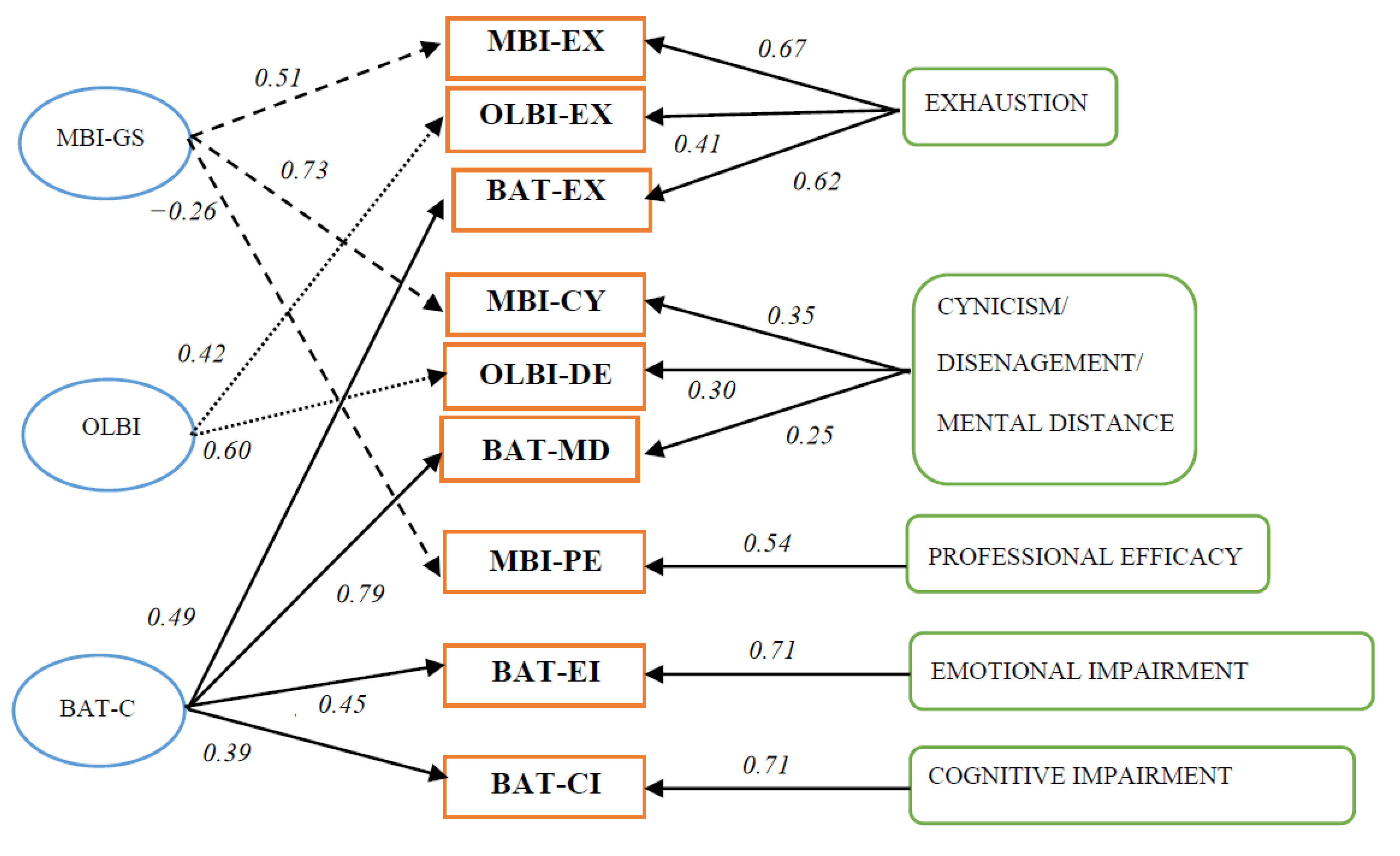
Convergent and Discriminant Validity with Other Burnout Measures
Discriminant Validity with Measures of Work Engagement, Workaholism, and Job Boredom
4. Discussion
4.1. Conceptualization of Burnout
4.2. The Development and Psychometric Evaluation of the BAT
4.3. Limitations and Suggestions for Future Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Questionnaire | Subscale | # Items |
|---|---|---|
| Validated | ||
| Bergen Burnout Inventory (BBI; Salmela-Aro, Rantanen, Hyvönen, Tilleman, & Feldt, 2011) | Exhaustion | 5 |
| Cynicism | 5 | |
| Inadequacy | 5 | |
| Burnout Measure (BM; Pines & Aronson, 1981) | Exhaustion | 21 |
| BurnOut-Neuratshenia Complaints Scale (BONKS; Verbraak, van de Griendt & Hoogduin, 2006) | Mental fatigue | 3 |
| Physical fatigue | 3 | |
| Mental fatigability | 3 | |
| Physical fatigability | 4 | |
| Muscle pain | 5 | |
| Dizziness | 4 | |
| Tension headaches | 6 | |
| Poor sleep | 5 | |
| Inability to relax | 4 | |
| Irritability | 5 | |
| Gastro-intestinal symptoms | 4 | |
| Copenhagen Burnout Inventory (CBI; Kristensen, Borritz, Villadsen, & Christensen, 2005) | Work-related burnout | 5 |
| Spanish Burnout Inventory (SBI; Gil-Monte & Faúndez, 2011) | Work enthusiasm | 5 |
| Psychological exhaustion | 4 | |
| Indolence | 6 | |
| Guilt | 4 | |
| Granada Burnout Questionnaire (GBQ; De la Fuente, et al., 2013) | Emotional exhaustion | 8 |
| Depersonalization | 7 | |
| Personal accomplishment | 11 | |
| Maslach Burnout Inventory-General Survey (MBI-GS; Schaufeli, Leiter, Maslach & Jackson, 1996) | Exhaustion | 5 |
| Cynicism | 5 | |
| Professional efficacy | 6 | |
| Oldenburg Burnout Inventory (OLBI; Demerouti, Bakker, Vardakou & Kantas, 2003) | Exhaustion | 8 |
| Disengagement | 8 | |
| Shirom Melamed Burnout Measure (SMBM; Shirom & Melamed, 2006) | Emotional exhaustion | 4 |
| Chronic fatigue | 4 | |
| Cognitive weariness | 6 | |
| 4-Dimensional Questionnaire (4-DSQ; Terluin, van Marwijk et al., 2006) | Distress | 16 |
| Depression | 6 | |
| Anxiety | 12 | |
| Somatization | 16 | |
| Non-validated | ||
| Boudreau Burnout Questionnaire (BBQ; Boudreau, Cahoon & Wedel, 2006) | Emotional exhaustion | 10 |
| Depersonalization | 10 | |
| Lack of personal accomplishment | 10 | |
| Fatality | 10 | |
| Instrument for the early detection of burnout (FOD, 2017) | Physical symptoms | 4 |
| Cognitive-affective symptoms | 12 | |
| Behavioral symptoms | 5 | |
| Hamburg Burnout Inventory (HBI; Burisch, 2017) | Emotional exhaustion | 5 |
| Distance | 4 | |
| Personal accomplishment | 3 | |
| Depressive reaction | 3 | |
| Helplessness | 4 | |
| Inner void | 4 | |
| Tedium | 5 | |
| Inability to unwind | 3 | |
| Overtaxing oneself | 5 | |
| Aggressive reaction | 3 |
Appendix B
| Never | Rarely | Sometimes | Often | Always | |
|---|---|---|---|---|---|
| Exhaustion | |||||
| 1. At work, I feel mentally exhausted | ☐ | ☐ | ☐ | ☐ | ☐ |
| 2. Everything I do at work requires a great deal of effort | ☐ | ☐ | ☐ | ☐ | ☐ |
| 3. After a day at work, I find it hard to recover my energy | ☐ | ☐ | ☐ | ☐ | ☐ |
| 4. At work, I feel physically exhausted | ☐ | ☐ | ☐ | ☐ | ☐ |
| 5. When I get up in the morning, I lack the energy to start a new day at work | ☐ | ☐ | ☐ | ☐ | ☐ |
| 6. I want to be active at work, but somehow, I am unable to manage | ☐ | ☐ | ☐ | ☐ | ☐ |
| 7. When I exert myself at work, I quickly get tired | ☐ | ☐ | ☐ | ☐ | ☐ |
| 8. At the end of my working day, I feel mentally exhausted and drained | ☐ | ☐ | ☐ | ☐ | ☐ |
| Mental distance | |||||
| 9. I struggle to find any enthusiasm for my work | ☐ | ☐ | ☐ | ☐ | ☐ |
| 10. At work, I do not think much about what I am doing and I function on autopilot | ☐ | ☐ | ☐ | ☐ | ☐ |
| 11. I feel a strong aversion towards my job | ☐ | ☐ | ☐ | ☐ | ☐ |
| 12. I feel indifferent about my job | ☐ | ☐ | ☐ | ☐ | ☐ |
| 13. I’m cynical about what my work means to others | ☐ | ☐ | ☐ | ☐ | ☐ |
| Cognitive impairment | |||||
| 14. At work, I have trouble staying focused | ☐ | ☐ | ☐ | ☐ | ☐ |
| 15. At work I struggle to think clearly | ☐ | ☐ | ☐ | ☐ | ☐ |
| 16. I’m forgetful and distracted at work | ☐ | ☐ | ☐ | ☐ | ☐ |
| 17. When I’m working, I have trouble concentrating | ☐ | ☐ | ☐ | ☐ | ☐ |
| 18. I make mistakes in my work because I have my mind on other things | ☐ | ☐ | ☐ | ☐ | ☐ |
| Emotional impairment | |||||
| 19. At work, I feel unable to control my emotions | ☐ | ☐ | ☐ | ☐ | ☐ |
| 20. I do not recognize myself in the way I react emotionally at work | ☐ | ☐ | ☐ | ☐ | ☐ |
| 21. During my work I become irritable when things don’t go my way | ☐ | ☐ | ☐ | ☐ | ☐ |
| 22. I get upset or sad at work without knowing why | ☐ | ☐ | ☐ | ☐ | ☐ |
| 23. At work I may overreact unintentionally | ☐ | ☐ | ☐ | ☐ | ☐ |
| Never | Rarely | Sometimes | Often | Always | |
|---|---|---|---|---|---|
| Psychological complaints | |||||
| 1. I have trouble falling or staying asleep | ☐ | ☐ | ☐ | ☐ | ☐ |
| 2. I tend to worry | ☐ | ☐ | ☐ | ☐ | ☐ |
| 3. I feel tense and stressed | ☐ | ☐ | ☐ | ☐ | ☐ |
| 4. I feel anxious and/or suffer from panic attacks | ☐ | ☐ | ☐ | ☐ | ☐ |
| 5. Noise and crowds disturb me | ☐ | ☐ | ☐ | ☐ | ☐ |
| Psychosomatic complaints | |||||
| 6. I suffer from palpitations or chest pain | ☐ | ☐ | ☐ | ☐ | ☐ |
| 7. I suffer from stomach and/or intestinal complaints | ☐ | ☐ | ☐ | ☐ | ☐ |
| 8. I suffer from headaches | ☐ | ☐ | ☐ | ☐ | ☐ |
| 9. I suffer from muscle pain, for example in the neck, shoulder or back | ☐ | ☐ | ☐ | ☐ | ☐ |
| 10. I often get sick | ☐ | ☐ | ☐ | ☐ | ☐ |
References
- Maslach, C.; Jackson, S.E. The Measurement of Experienced Burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Boudreau, R.A.; Boudreau, W.F.; Mauthe-Kaddoura, A.J. From 57 for 57: A Bibliography of Burnout Citations. In Proceedings of the 17th Conference of the European Association of Work and Organizational Psychology (EAWOP), Oslo, Norway, 20–22 May 2015. [Google Scholar]
- Maslach, C.; Jackson, S.E. Maslach Burnout Inventory. Manual, 2nd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1986. [Google Scholar]
- Maslach, C.; Leiter, M.P.; Jackson, S.E. Maslach Burnout Inventory Manual, 4th ed.; Mind Garden, Inc.: Palo Alto, CA, USA, 2017. [Google Scholar]
- Schaufeli, W.B.; Leiter, M.P.; Maslach, C.; Jackson, S.E. The Maslach Burnout Inventory–General Survey; Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1996; pp. 19–26. [Google Scholar]
- Deligkaris, P.; Panagopoulou, E.; Montgomery, A.J.; Masoura, E. Job Burnout and Cognitive Functioning: A Systematic Review. Work Stress 2014, 28, 107–123. [Google Scholar] [CrossRef]
- van der Heiden, C.; Hoogduin, C.A.L. Burn-out: Diagnostiek En Behandeling. TBV—Tijdschr. voor Bedrijfs-en Verzek. 2010, 10, 48–53. [Google Scholar] [CrossRef]
- Bianchi, R.; Schonfeld, I.S.; Laurent, E. Is Burnout a Depressive Disorder? A Reexamination with Special Focus on Atypical Depression. Int. J. Stress Manag. 2014, 21, 307–324. [Google Scholar] [CrossRef]
- Koutsimani, P.; Montgomery, A.; Georganta, K. The Relationship Between Burnout, Depression, and Anxiety: A Systematic Review and Meta-Analysis. Front. Psychol. 2019, 10, 284. [Google Scholar] [CrossRef] [PubMed]
- Kakiashvili, T.; Leszek, J.; Rutkowski, K. The Medical Perspective on Burnout. Int. J. Occup. Med. Environ. Health 2013, 26, 401–412. [Google Scholar] [CrossRef]
- Ahola, K.; Hakanen, J.; Perhoniemi, R.; Mutanen, P. Relationship between Burnout and Depressive Symptoms: A Study Using the Person-Centred Approach. Burn. Res. 2014, 1, 29–37. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Taris, T.W. The Conceptualization and Measurement of Burnout: Common Ground and Worlds Apart. Work Stress 2005, 19, 256–262. [Google Scholar] [CrossRef]
- Wheeler, D.L.; Vassar, M.; Worley, J.A.; Barnes, L.L.B. A Reliability Generalization Meta-Analysis of Coefficient Alpha for the Maslach Burnout Inventory. Educ. Psychol. Meas. 2011, 71, 231–244. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Salanova, M. Efficacy or Inefficacy, That’s the Question: Burnout and Work Engagement, and Their Relationships with Efficacy Beliefs. Anxiety Stress Coping 2007, 20, 177–196. [Google Scholar] [CrossRef]
- de Beer, L.T.; Bianchi, R. Confirmatory Factor Analysis of the Maslach Burnout Inventory. Eur. J. Psychol. Assess. 2019, 35, 217–224. [Google Scholar] [CrossRef]
- WHO. International Classification of Diseases (ICD-11); WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Lastovkova, A.; Carder, M.; Rasmussen, H.M.; Sjobergg, L.; de Groene, G.J.; Sauni, R.; Vevoda, J.; Vevodova, S.; Lasfargues, G.; Svartegren, M.; et al. Burnout Syndrome as an Occupational Disease in the European Union: An Exploratory Study. Ind. Health 2018, 56, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Malakh-Pines, A.; Aronson, E.; Kafry, D. Burnout: From Tedium to Personal Growth; Free Press: Washington, DC, USA, 1981. [Google Scholar]
- Shirom, A.; Melamed, S. A Comparison of the Construct Validity of Two Burnout Measures in Two Groups of Professionals. Int. J. Stress Manag. 2006, 13, 176–200. [Google Scholar] [CrossRef]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A New Tool for the Assessment of Burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Salmela-Aro, K.; Rantanen, J.; Hyvönen, K.; Tilleman, K.; Feldt, T. Bergen Burnout Inventory: Reliability and Validity among Finnish and Estonian Managers. Int. Arch. Occup. Environ. Health 2011, 84, 635–645. [Google Scholar] [CrossRef]
- De la Fuente, E.I.; Lozano, L.M.; García-Cueto, E.; Luis, C.S.; Vargas, C.; Cañadas, G.R.; Cañadas-De la Fuente, G.A.; Hambleton, R.K. Development and Validation of the Granada Burnout Questionnaire in Spanish Police. Int. J. Clin. Health Psychol. 2013, 13, 216–225. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Vardakou, I.; Kantas, A. The Convergent Validity of Two Burnout Instruments. Eur. J. Psychol. Assess. 2003, 18, 296–307. [Google Scholar] [CrossRef]
- González-Romá, V.; Schaufeli, W.B.; Bakker, A.B.; Lloret, S. Burnout and Work Engagement: Independent Factors or Opposite Poles? J. Vocat. Behav. 2006, 68, 165–174. [Google Scholar] [CrossRef]
- Thorndike, E.L. Educational Psychology, Volume III: Mental Work and Fatigue, Individual Differences and Their 885 Causes; Teachers College Columbia University: New York, NY, USA, 1914. [Google Scholar]
- Elo, S.; Kyngäs, H. The Qualitative Content Analysis Process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in Qualitative Research: Exploring Its Conceptualization and Operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Burnard, P. A Method of Analysing Interview Transcripts in Qualitative Research. Nurse Educ. Today 1991, 11, 461–466. [Google Scholar] [CrossRef]
- Warr, P. Work, Unemployment, and Mental Health; Oxford University Press: Oxford, UK, 1987. [Google Scholar]
- Mikolajczak, M.; Gross, J.J.; Roskam, I. Parental Burnout: What Is It, and Why Does It Matter? Clin. Psychol. Sci. 2019, 7, 1319–1329. [Google Scholar] [CrossRef]
- Moreno-Jiménez, B.; Barbaranelli, C.; Herrer, M.G.; Hernández, E.G. The Physician Burnout Questionnaire: A New Definition and Measure. TPM—Testing, Psychom. Methodol. Appl. Psychol. 2012, 19, 325–344. [Google Scholar] [CrossRef]
- Terluin, B.; van Marwijk, H.W.; Adèr, H.J.; de Vet, H.C.; Penninx, B.W.; Hermens, M.L.; van Boeijen, C.A.; van Balkom, A.J.; van der Klink, J.J.; Stalman, W.A. The Four-Dimensional Symptom Questionnaire (4DSQ): A Validation Study of a Multidimensional Self-Report Questionnaire to Assess Distress, Depression, Anxiety and Somatization. BMC Psychiatry 2006, 6, 34. [Google Scholar] [CrossRef]
- Van der Klink, J.J.; van Dijk, F.J. Dutch Practice Guidelines for Managing Adjustment Disorders in Occupational and Primary Health Care. Scand. J. Work. Environ. Health 2003, 29, 478–487. [Google Scholar] [CrossRef]
- Terluin, B.; Van Rhenen, W.; Schaufeli, W.B.; De Haan, M. The Four-Dimensional Symptom Questionnaire (4DSQ): Measuring Distress and Other Mental Health Problems in a Working Population. Work Stress 2004, 18, 187–207. [Google Scholar] [CrossRef]
- Verbraak, M.; Kleyweg, J.; van den Griendt, J.; Hoogduin, K. Nadere Verkenning van de Psychometrische Kwaliteiten van de BurnOut-Neurasthenie Klachten Schaal (BO-NKS): Wat Valt Er Te Meten? Dir. Ther. 2008, 28, 187–221. [Google Scholar] [CrossRef]
- Campbell, D.T.; Fiske, D.W. Convergent and Discriminant Validation by the Multitrait-Multimethod Matrix. Psychol. Bull. 1959, 56, 81–105. [Google Scholar] [CrossRef]
- Salanova, M.; Del Líbano, M.; Llorens, S.; Schaufeli, W.B. Engaged, Workaholic, Burned-out or Just 9-to-5? Toward a Typology of Employee Well-Being. Stress Health 2014, 30, 71–81. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Salanova, M.; González-romá, V.; Bakker, A.B. The Measurement of Engagement and Burnout: A Two Sample Confirmatory Factor analytic approach. J. Happiness Stud. 2002, 3, 71–92. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. The Truth about Burnout.; Jossey-Bass: San Fransisco, CA, USA, 1997. [Google Scholar]
- Schaufeli, W.; De Witte, H. Outlook Work Engagement in Contrast to Burnout: Real and Redundant! Burn. Res. 2017, 5, 58–60. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Shimazu, A.; Taris, T.W. Being Driven to Work Excessively Hard. Cross-Cult. Res. 2009, 43, 320–348. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Peeters, M.C.W.; Schaufeli, W.B. Different Types of Employee Well-Being Across Time and Their Relationships With Job Crafting. J. Occup. Health Psychol. 2018, 23, 289–301. [Google Scholar] [CrossRef] [PubMed]
- Burke, R.J. Workaholism in Organizations: Concepts, Results and Future Research Directions. Int. J. Manag. Rev. 2000, 2, 1–16. [Google Scholar] [CrossRef]
- Mikulas, W.L.; Vodanovich, S.J. The Essence of Boredom. Psychol. Rec. 1993, 43, 3–13. [Google Scholar] [CrossRef][Green Version]
- Schaufeli, W.B.; Salanova, M. Burnout, Boredom and Engagement in the Workplace. In People at Work: An Introduction to Contemporary Work Psychology; Peeters, M., de Jonge, J., Taris, T., Eds.; Wiley-Blackwell: Chichester, UK, 2014; pp. 293–320. [Google Scholar]
- Schaufeli, W.B.; van Dierendonck, D. Utrechtse Burnout Schaal. Test Handleiding [Utrecht Burnout Scale. Test Manual].; Swets Test Publishers: Lisse, The Netherlands, 2000. [Google Scholar]
- Schaufeli, W.B.; Shimazu, A.; Hakanen, J.; Salanova, M.; De Witte, H. An Ultra-Short Measure for Work Engagement. Eur. J. Psychol. Assess. 2019, 35, 577–591. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B.; Van Der Heijden, F.M.M.A.; Prins, J.T. Workaholism Among Medical Residents: It Is the Combination of Working Excessively and Compulsively That Counts. Int. J. Stress Manag. 2009, 16, 249–272. [Google Scholar] [CrossRef]
- Reijseger, G.; Schaufeli, W.B.; Peeters, M.C.W.; Taris, T.W.; van Beek, I.; Ouweneel, E. Watching the Paint Dry at Work: Psychometric Examination of the Dutch Boredom Scale. Anxiety Stress Coping 2013, 26, 508–525. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; Sage: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Chen, F.F.; West, S.G.; Sousa, K.H. A Comparison of Bifactor and Second-Order Models of Quality of Life. Multivar. Behav. Res. 2010. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Byrne, B.M. Structural Equation Modeling with AMOS; Lawrence Earlbaum: Mahwah, NJ, USA, 2001. [Google Scholar]
- Hu, L.; Bentler, P. Evaluating Model Fit. In Structural Equation Modeling. Concepts, Issues, and Applications; Hoyle, R.H., Ed.; Sage: London, UK, 1995; pp. 76–99. [Google Scholar]
- Widaman, K.F. Hierarchically Nested Covariance Structure Models for Multi- Trait-Multimethod Data. Appl. Psychol. Meas. 1985, 9, 1–26. [Google Scholar] [CrossRef]
- Raedeke, T.D.; Arce, C.; De Francisco, C.; Seoane, G.; Ferraces, M.J. The Construct Validity of the Spanish Version of the ABQ Using a Multi-Trait/Multi-Method Approach. An. Psicol. 2013, 29, 693–700. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39. [Google Scholar] [CrossRef]
- Hutcheson, G.; Sofroniou, N. The Multivariate Social Scientist: Introductory Statistics Using Generalized Linear Models; Sage Publications: Thousand Oaks, CA, USA, 1999. [Google Scholar]
- Heinemann, L.V.; Heinemann, T. Burnout Research: Emergence and Scientific Investigation of a Contested Diagnosis. SAGE Open 2017. [Google Scholar] [CrossRef]
- Bianchi, R.; Schonfeld, I.S.; Laurent, E. Burnout: Moving beyond the Status Quo. Int. J. Stress Manag. 2019, 26, 36–45. [Google Scholar] [CrossRef]
- Maslach, C.; Schaufeli, W.B. Historical and Conceptual Development of Burnout. In Professional Burnout: Recent Developments in Theory and Research; Schaufeli, W., Maslach, C., Marek, T., Eds.; Taylor & Francis: Washington, DC, USA, 1993; pp. 1–16. [Google Scholar]
- Oosterholt, B.G.; Maes, J.H.R.; Van der Linden, D.; Verbraak, M.J.P.M.; Kompier, M.A.J. Getting Better, but Not Well: A 1.5 Year Follow-up of Cognitive Performance and Cortisol Levels in Clinical and Non-Clinical Burnout. Biol. Psychol. 2016, 117, 89–99. [Google Scholar] [CrossRef] [PubMed]
- van Dam, A.; Keijsers, G.P.J.; Eling, P.A.T.M.; Becker, E.S. Impaired Cognitive Performance and Responsiveness to Reward in Burnout Patients: Two Years Later. Work Stress 2012, 26, 333–346. [Google Scholar] [CrossRef]
- Shirom, A. Burnout in Work Organizations. In International Review of Industrial and Organizational Psychology 1989; John Wiley & Sons: Oxford, UK, 1989; pp. 25–48. [Google Scholar]
- Zapf, D.; Seifert, C.; Schmutte, B.; Mertini, H.; Holz, M. Emotion Work and Job Stressors and Their Effects on Burnout. Psychol. Health 2007. [Google Scholar] [CrossRef]
- Taris, T.W.; Le Blanc, P.M.; Schaufeli, W.B.; Schreurs, P.J.G. Are There Causal Relationships between the Dimensions of the Maslach Burnout Inventory? A Review and Two Longitudinal Tests. Work Stress 2005, 19, 238–255. [Google Scholar] [CrossRef]
- Arrindell, W.; Ettema, H.; Groenman, N.; Brook, F.; Janssen, I.; Slaets, J.; Hekster, G.; Derksen, J.; van der Ende, J.; Land, H.; et al. Further Dutch Experiences with the Symptom Checklist-90 Revised; Swets Test Publishers: Lisse, The Netherlands, 2003. [Google Scholar]
- Sakakibara, K.; Shimazu, A.; Toyama, H.; Schaufeli, W.B. Validation of the Japanese Version of the Burnout Assessment Tool. Front. Psychol. 2020, 11, 1819. [Google Scholar] [CrossRef]
- de Beer, L.T.; Schaufeli, W.B.; De Witte, H.; Hakanen, J.J.; Shimazu, A.; Glaser, J.; Seubert, C.; Bosak, J.; Sinval, J.; Rudnev, M. Measurement Invariance of the Burnout Assessment Tool (BAT) Across Seven Cross-National Representative Samples. Int. J. Environ. Res. Public Health 2020, 17, 5604. [Google Scholar] [CrossRef]
- Hadzibajramovic, E.; Schaufeli, W.B.; De Witte, H. A Rasch Analysis of the Burnout Assessment Tool. PLoS ONE 2020, 15, e0242241. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.; Bernstein, I. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY USA, 1994; Volume 3, p. 701. [Google Scholar]
- Halbesleben, J.R.B.; Demerouti, E. The Construct Validity of an Alternative Measure of Burnout: Investigating the English Translation of the Oldenburg Burnout Inventory. Work Stress 2005, 19, 208–220. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Taris, T.W.; Van Rhenen, W. Workaholism, Burnout, and Work Engagement: Three of a Kind or Three Different Kinds of Employee Well-Being? Appl. Psychol. 2008, 57, 173–203. [Google Scholar] [CrossRef]
- Goldberg, D.P. Manual of the General Health Questionnaire; NFER: Windsor, ON, Canada, 1978. [Google Scholar]
- Streiner, D.L.; Cairney, J. What’s under the ROC? An Introduction to Receiver Operating Characteristics Curves. Can. J. Psychiatry 2007, 52, 121–128. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B.; Hoogduin, K.; Schaap, C.; Kladler, A. On the Clinical Validity of the Maslach Burnout Inventory and the Burnout Measure. Psychol. Health 2001, 16, 565–582. [Google Scholar] [CrossRef]
- Roelen, C.A.M.; van Hoffen, M.F.A.; Groothoff, J.W.; de Bruin, J.; Schaufeli, W.B.; van Rhenen, W. Can the Maslach Burnout Inventory and Utrecht Work Engagement Scale Be Used to Screen for Risk of Long-Term Sickness Absence? Int. Arch. Occup. Environ. Health 2015, 88, 467–475. [Google Scholar] [CrossRef]
| Model | χ2 | S-Bχ2 | df | CFI | TLI | RMSEA [90% CI] | Δχ2 | p | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Core symptoms | ||||||||||
| 1 | Unidimensional model | 2960.13 | 1.29 | 230 | 0.73 | 0.70 | 0.13 [0.12–0.13] | |||
| 2 | Correlated 4-factor model | 773.54 | 1.28 | 224 | 0.95 | 0.94 | 0.06 [0.05–0.06] | 2 vs. 1 | 1700.46 | <0.0001 |
| 3 | Second-order model (4 first order, 1 second order) | 776.79 | 1.28 | 226 | 0.95 | 0.94 | 0.06 [0.05–0.06] | 3 vs. 1 3 vs. 2 | 1522.52 3.25 | <0.0001 0.20 |
| Secondary symptoms | ||||||||||
| 4 | Unidimensional model | 1963.62 | 1.29 | 104 | 0.70 | 0.65 | 0.15 [0.15–0.16] | |||
| 5 | Correlated 2-factor model | 852.11 | 1.30 | 103 | 0.88 | 0.86 | 0.10 [0.09–0.10] | 5 vs. 4 | 5482.03 | <0.0001 |
| 5a | Adjusted correlated 2-factor model | 500.48 | 1.29 | 102 | 0.94 | 0.92 | 0.07 [0.07–0.08] | 5a vs. 4 5a vs. 5 | 2413.39351.63 | <0.0001 |
| Core & secondary symptoms | ||||||||||
| 6 | Correlated 6-factor model | 2244.29 | 1.25 | 687 | 0.91 | 0.90 | 0.06 [0.05–0.06] | |||
| 7 | Second-order model (6 first order, 1 second-order) | 2309.48 | 1.25 | 696 | 0.91 | 0.90 | 0.06 [0.05–0.06] | 7 vs. 6 | 65.19 | <0.0001 |
| 8 | Second-order model (6 first order, 2 second-order) | 2293.77 | 1.25 | 695 | 0.91 | 0.90 | 0.06 [0.05–0.06] | 8 vs. 6 8 vs. 7 | 49.4815.71 | <0.0001 <0.0001 |
| Model | χ2 | df | S-Bχ2 | CFI | TLI | RMSEA [90% CI] | Δχ2 | Δdf | p | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | CT-CM model | 5803.79 | 1310 | 1.1963 | 0.91 | 0.90 | 0.05 [0.04–0.05] | ||||
| 2 | NT-CM model | 10020.64 | 1367 | 1.1974 | 0.83 | 0.82 | 0.07 [0.06–0.07] | 2 vs. 1 | 4134.88 | 57 | <0.0001 |
| 3 | PCT-CM model | 7022.20 | 1313 | 1.1973 | 0.89 | 0.88 | 0.05 [0.04–0.05] | 3 vs. 1 | 896.35 | 3 | <0.0001 |
| 4 | CT-PCM model | 11203.54 | 1320 | 1.1973 | 0.80 | 0.79 | 0.07 [0.06–0.07] | 4 vs. 1 | 4871.58 | 10 | <0.0001 |
| AVE | R2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| 1 | Engagement (UWES) | 0.76 | - | ||||||
| 2 | Workaholism: Excessive working (DUWAS) | 0.51 | 0.07 | - | |||||
| 3 | Workaholism: Compulsive working (DUWAS) | 0.53 | 0.00 | 0.59 | - | ||||
| 4 | Job boredom (DUBS) | 0.58 | 0.41 | 0.12 | 0.05 | - | |||
| 5 | Core symptoms of burnout (BAT-C) | 0.51 | 0.42 | 0.03 | 0.15 | 0.21 | - | ||
| 6 | Secondary burnout symptoms: Psychological distress (BAT-S) | 0.51 | 0.17 | 0.07 | 0.23 | 0.03 | 0.62 | - | |
| 7 | Secondary burnout symptoms: Depressed mood (4DSQ) | 0.52 | 0.15 | 0.02 | 0.12 | 0.10 | 0.38 | 0.39 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schaufeli, W.B.; Desart, S.; De Witte, H. Burnout Assessment Tool (BAT)—Development, Validity, and Reliability. Int. J. Environ. Res. Public Health 2020, 17, 9495. https://doi.org/10.3390/ijerph17249495
Schaufeli WB, Desart S, De Witte H. Burnout Assessment Tool (BAT)—Development, Validity, and Reliability. International Journal of Environmental Research and Public Health. 2020; 17(24):9495. https://doi.org/10.3390/ijerph17249495
Chicago/Turabian StyleSchaufeli, Wilmar B., Steffie Desart, and Hans De Witte. 2020. "Burnout Assessment Tool (BAT)—Development, Validity, and Reliability" International Journal of Environmental Research and Public Health 17, no. 24: 9495. https://doi.org/10.3390/ijerph17249495
APA StyleSchaufeli, W. B., Desart, S., & De Witte, H. (2020). Burnout Assessment Tool (BAT)—Development, Validity, and Reliability. International Journal of Environmental Research and Public Health, 17(24), 9495. https://doi.org/10.3390/ijerph17249495





