Quality of Life After Coronary Artery Bypass Surgery: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Selection Process and Result Codification
2.4. Critical Reading and Level of Evidence
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Studies Included
3.2. Quality of Life Before and After a CABG
3.3. Differences in Quality of Life Scores Before and After a CABG
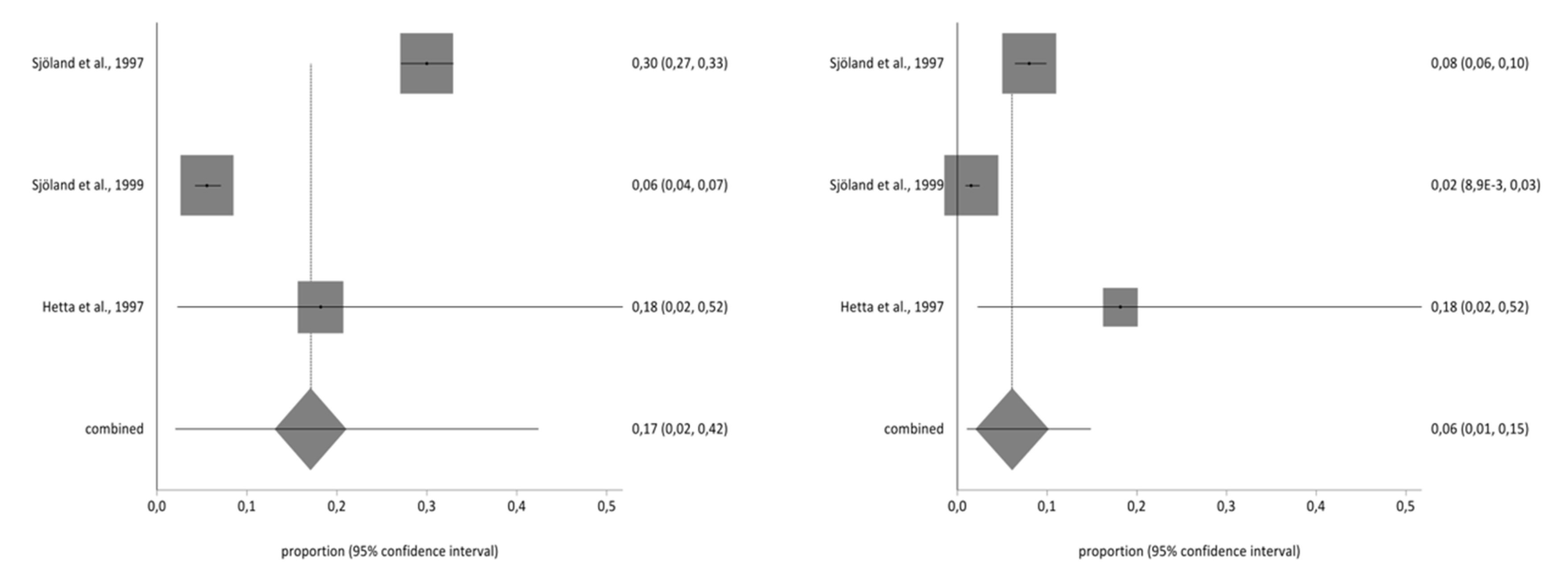
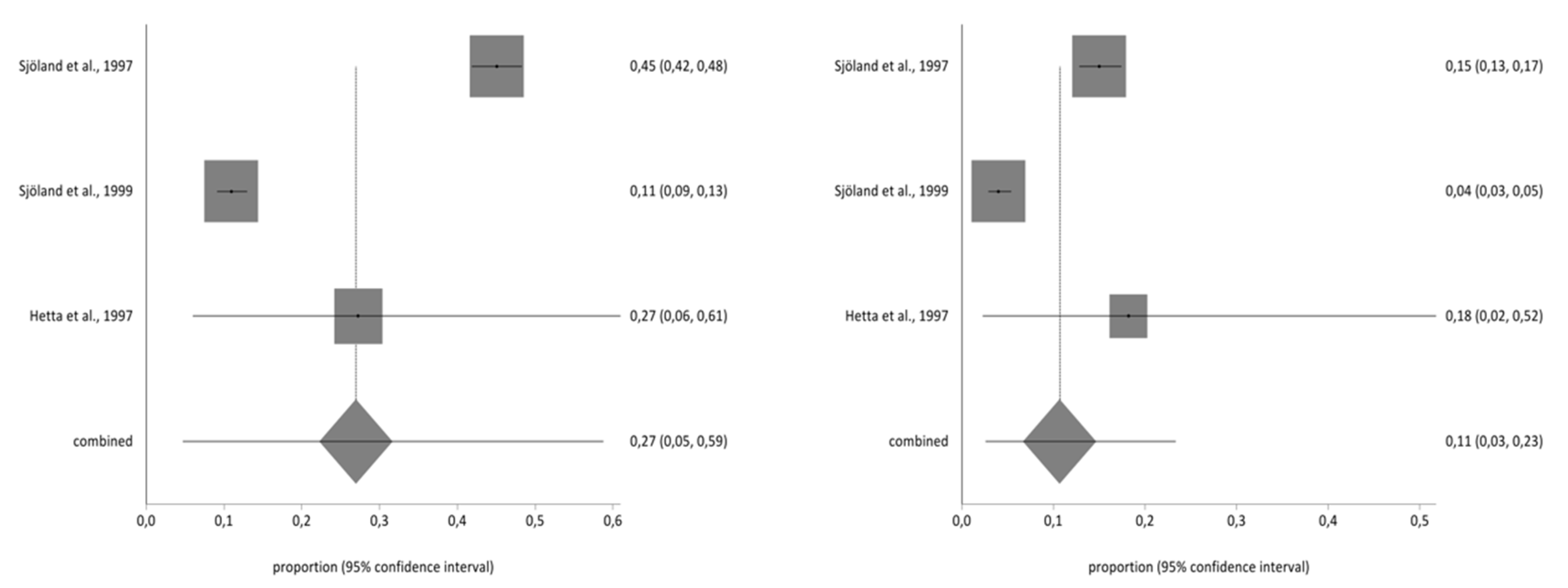
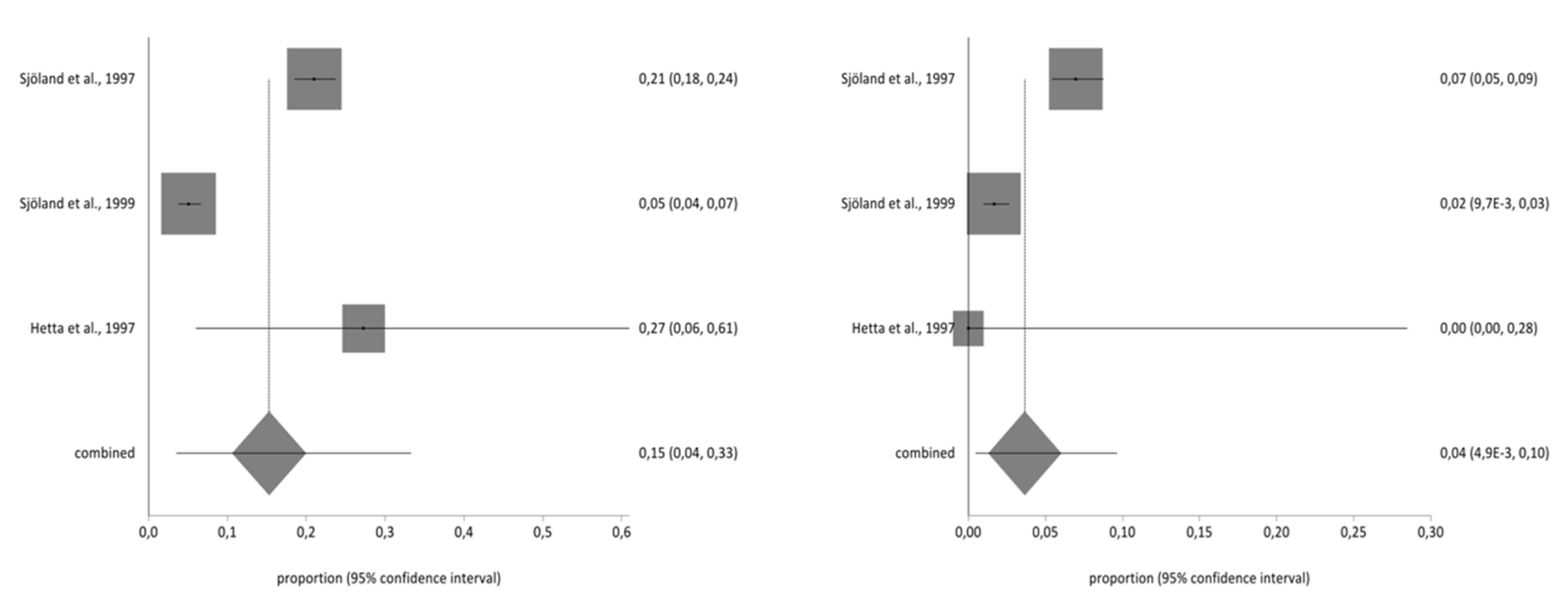
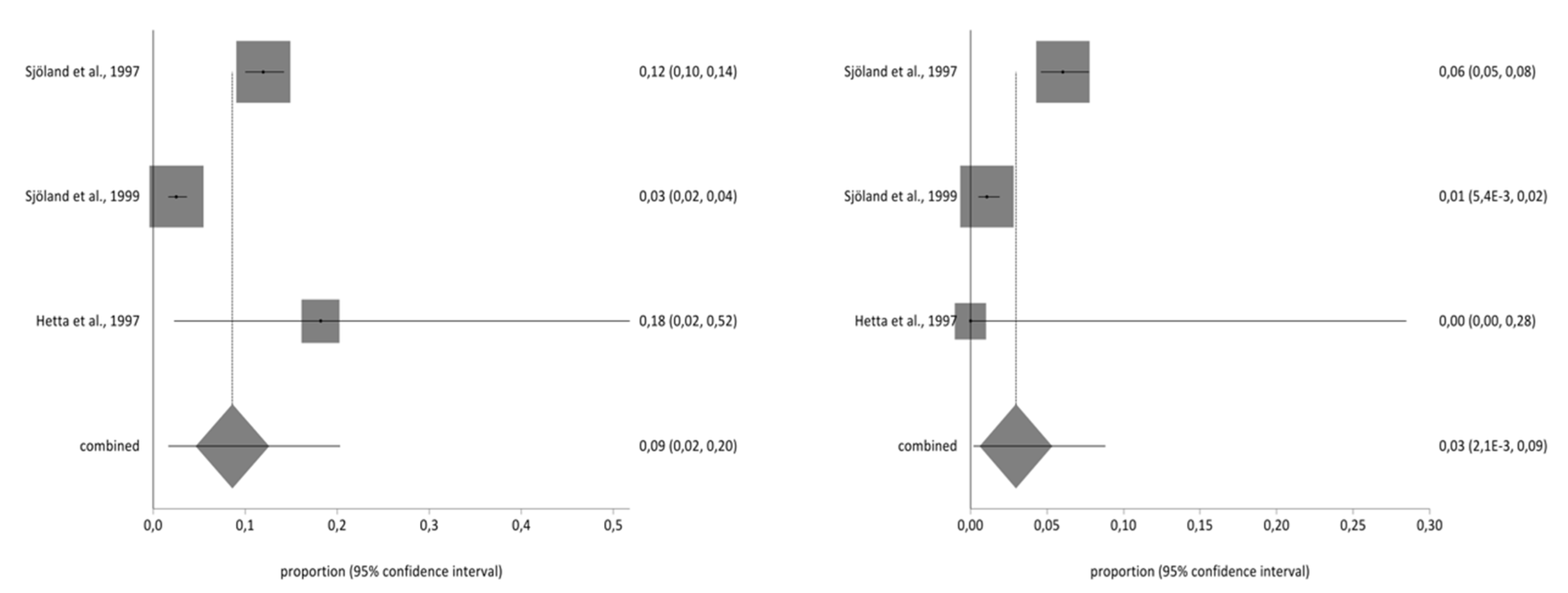
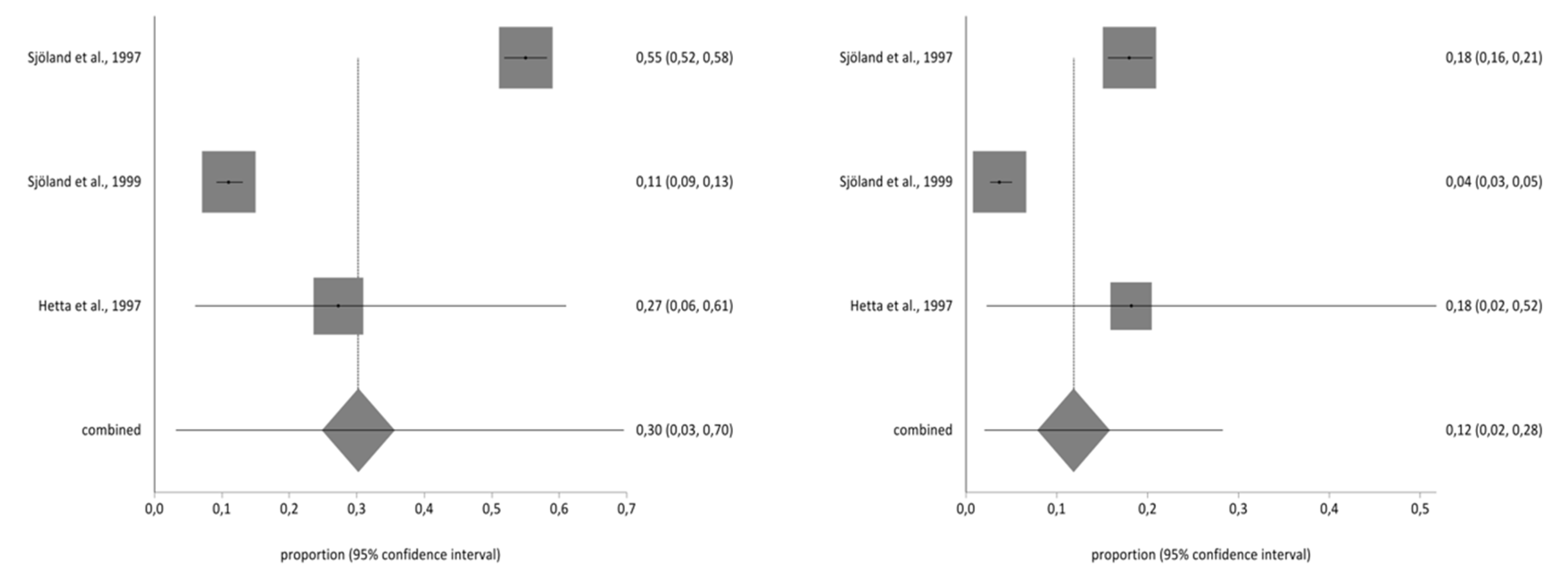
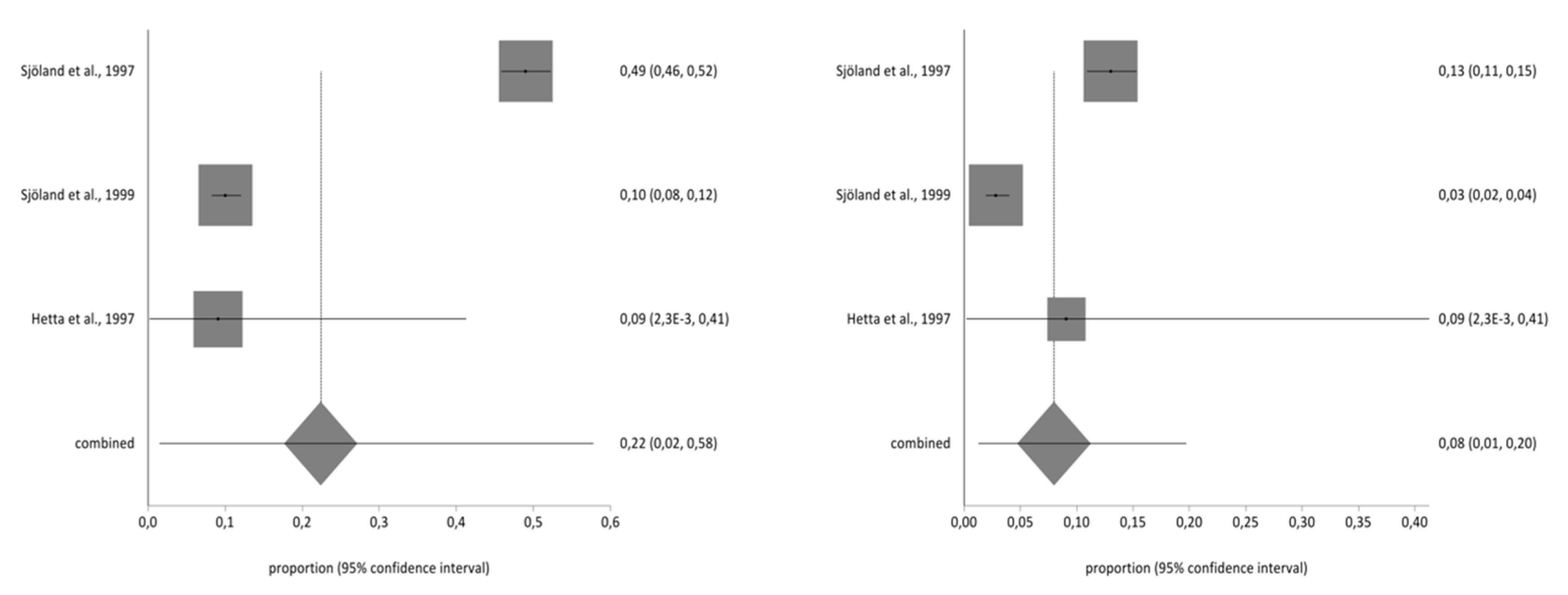
3.4. Meta-Analysis for Estimating the Prevalence of Pre- and Post-CABG Impact on Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sawatzky, J.V.; Naimark, B.J. The coronary artery bypass graft surgery trajectory: Gender differences revisited. J. Cardiothorac. Surg. 2009, 8, 302–308. [Google Scholar] [CrossRef]
- Baptista, V.C.; Palhares, L.C.; de Oliveira, P.P.M.; Silveira Filho, L.M.; Vilarinho, K.A.; Severino, E.S.B.; Lavagnoli, C.F.R.; Petrucci, O. Six-minute walk test as a tool for assessing the quality of life in patients undergoing coronary artery bypass grafting surgery. Rev. Bras. Cir. Cardiovasc. 2012, 27, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Fatima, K.; Yousuf-Ul-Islam, M.; Ansari, M.; Bawany, F.I.; Khan, M.S.; Khetpal, A.; Khetpal, N.; Lashari, M.N.; Arshad, M.H.; Bin Amir, R.; et al. Comparison of the Postprocedural Quality of Life between Coronary Artery Bypass Graft Surgery and Percutaneous Coronary Intervention: A Systematic Review. Cardiol. Res. Pract. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Ludovic, M.; Gianluca, T.; Timothy, L.; Jean-Luc, J.; John, D.P. Fifty years of coronary artery bypass grafting. J. Thorac. Dis. 2018, 10, 1960–1967. [Google Scholar]
- Kivimäki, M.; Head, J.; Ferrie, J.E.; Hemingway, H.; Shipley, M.J.; Vahtera, J.; Marmot, M.G. Working while ill as a risk factor for serious coronary events: The Whitehall II study. Am. J. Public Health 2005, 95, 98–102. [Google Scholar] [CrossRef]
- Barrantes, M. Factores asociados a la calidad de vida relacionada a la salud en pacientes con cardiopatía coronaria y diabetes mellitus. Rev. Med. Herediana 2010, 21, 118–127. [Google Scholar] [CrossRef]
- Soto, M.; Failde, I. La calidad de vida relacionada a la salud como medida de resultados en pacientes con cardiopatía isquémica. Rev. Soc. Esp Dolor 2004, 11, 505–514. [Google Scholar]
- Meyer, T.; Belnap, B.H.; Herrmann-Lingen, C.; He, F.; Mazumdar, S.; Rollman, B.L. Benefits of collaborative care for post-CABG depression are not related to adjustments in antidepressant pharmacotherapy. J. Psychosom. Res. 2014, 76, 28–33. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Kosinski, M.; Gandek, B. SF-36 Health Survey: Manual & Interpretation Guide, 2nd ed.; New England Medical Center: Boston, MA, USA, 2000. [Google Scholar]
- Hunt, S.M.; McKenna, S.P.; McEwen, J.; Williams, J.; Papp, E. The Nottingham Health Profile: Subjective health status and medical consultations. Soc. Sci. Med. 1981, 15, 221–229. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P). Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Sanderson, S.; Tatt, I.D.; Higgins, J.P.T. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: A systematic review and annotated bibliography. Int. J. Epidemiol. 2007, 36, 666–676. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalg, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H. The Oxford 2011 Levels of Evidence; CEBM: Oxford, UK, 2011. [Google Scholar]
- Sandau, K.E.; Lindquist, R.A.; Treat-Jacobson, D.; Savik, K. Health-related quality of life and subjective neurocognitive function three months after coronary artery bypass graft surgery. Heart Lung 2008, 37, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Grady, K.L.; Lee, R.; Subacius, H.; Malaisrie, S.C.; McGee, E.C.J.; Kruse, J.; Goldberger, J.J.; McCarthy, P.M. Improvements in health-related quality of life before and after isolated cardiac operations. Ann. Thorac. Surg. 2011, 91, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Rumsfeld, J.S.; Ho, P.M.; Magid, D.J.; McCarthy, M.; Shroyer, A.L.W.; Mawhinney, S.; Grover, F.L.; Hammermeister, K.E. Predictors of health-related quality of life after coronary artery bypass surgery. Ann. Thorac. Surg. 2004, 77, 1508–1513. [Google Scholar] [CrossRef]
- Sjoland, H.; Caidahl, K.; Wiklund, I.; BW, K.; Karlsson, T.; Winberg, L.; Herlitz, J. Effects of age on quality of life before and after coronary artery bypass grafting. Cardiol. Elder 1996, 4, 195–200. [Google Scholar]
- Sjoland, H.; Wiklund, I.; Caidahl, K.; Haglid, M.; Westberg, S.; Herlitz, J. Improvement in quality of life and exercise capacity after coronary bypass surgery. Arch. Intern. Med. 1999, 156, 265–271. [Google Scholar] [CrossRef]
- Herlitz, J.; Brandrup-Wognsen, G.; Caidahl, K.; Haglid, M.; Karlson, B.W.; Hartford, M.; Karlsson, T.; Sjöland, H. Improvement and factors associated with improvement in quality of life during 10 years after coronary artery bypass grafting. Coron. Artery Dis. 2003, 14, 509–517. [Google Scholar] [CrossRef]
- Herlitz, J.; Brandrup-Wognsen, G.; Caidahl, K.; Hartford, M.; Haglid, M.; Karlson, B.W.; Karlsson, T.; Sjöland, H. Determinants for an impaired quality of life 10 years after coronary artery bypass surgery. Int. J. Cardiol. 1998, 98, 447–452. [Google Scholar] [CrossRef]
- Edell-Gustafsson, U.M.; Hetta, J.E.; Aren, G.B.; Hamrin, E.K.F. Measurement of sleep and quality of life before and after coronary artery bypass grafting: A pilot study. Int. J. Nurs. Pract. 1997, 3, 239–246. [Google Scholar]
- Lie, I.; Arnesen, H.; Sandvik, L.; Hamilton, G.; EH, B. Predictors for physical and mental health 6months after coronary artery bypass grafting: A cohort study. Eur. J. Cardiovasc. Nurs. 2010, 9, 238–243. [Google Scholar] [CrossRef]
- Ballan, A.; Lee, G. A comparative study of patient perceived quality of life pre and post coronary artery bypass graft surgery. Aust. J. Adv. Nurs. 2007, 24, 24–28. [Google Scholar] [PubMed]
- Oreel, T.H.; Nieuwkerk, P.T.; Hartog, I.D.; Netjes, J.E.; Vonk, A.B.A.; Lemkes, J.; Van Laarhoven, H.W.M.; Scherer-Rath, M.; Sprangers, M.A.G.; Henriques, J.P.S. Gender differences in quality of life in coronary artery disease patients with comorbidities undergoing coronary revascularization. PLoS ONE 2020, 15, e0234543. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo Neto, J.A.; Reis, L.M.C.B.; Veras, M.R.; Queiroz, L.L.C.; de Paiva Lima Nogueira Nunes, K.; de Oliveira Miranda, P.; dos Santos, A.F.; Nunes, J.K.V.R. Impact of cardiovascular interventions on the quality of life in the elderly. Braz. J. Cardiovasc. Sur. 2015, 30, 626–630. [Google Scholar] [CrossRef][Green Version]
- Mathisen, L.; Andersen, M.H.; Veenstra, M.; Wahl, A.K.; Hanestad, B.R.; Fosse, E. Quality of life can both influence and be an outcome of general health perceptions after heart surgery. Health Qual Life Outcomes 2007, 5, 27. [Google Scholar] [CrossRef] [PubMed]
- Peric, V.; Borzanovic, M.; Jovanovic, A.; Stolic, R.; Sovtic, S.; Trajkovic, G. The relationship between EuroSCORE preoperative risk prediction and quality of life changes after coronary artery by-pass surgery. Interact. Cardiovasc. Thorac. Surg. 2005, 4, 622–626. [Google Scholar] [CrossRef]
- Peric, V.M.; Borzanovic, M.D.; Stolic, R.V.; Jovanovic, A.N.; Sovtic, S.R. Severity of angina as a predictor of quality of life changes six months after coronary artery bypass surgery. Ann. Thorac. Surg. 2006, 81, 2115–2120. [Google Scholar] [CrossRef]
- Peric, V.; Borzanovic, M.; Stolic, R.; Jovanovic, A.; Sovtic, S.; Djikic, D.; Marcetic, Z.; Dimkovic, S. Quality of life in patients related to gender differences before and after coronary artery bypass surgery. Interact. Cardiovasc. Thorac. Surg. 2010, 10, 232–238. [Google Scholar] [CrossRef]
- Correa-Rodríguez, M.; Abu Ejheisheh, M.; Suleiman-Martos, N.; Membrive-Jiménez, M.J.; Velando-Soriano, A.; Schmidt-RioValle, J.; Gómez-Urquiza, J.L. Prevalence of Depression in Coronary Artery Bypass Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 26, 9909. [Google Scholar] [CrossRef]
- Harris, R.; Croce, B.; Tian, D.H. Coronary artery bypass grafting. Ann. Cardiothorac. Surg. 2013, 2, 579. [Google Scholar]
- Murashita, T. The role of coronary artery bypass grafting in patients with ischemic cardiomyopathy in the current era. J. Thorac. Dis. 2016, 8, E1032–E1033. [Google Scholar] [CrossRef]
- Koene, R.J.; Kealhofer, J.V.; Adabag, S.; Vakil, K.; Florea, V.G. Effect of coronary artery bypass graft surgery on left ventricular systolic function. J. Thorac. Dis. 2017, 9, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Rupprecht, L.; Schmid, C.; Debl, K.; Lunz, D.; Flörchinger, B.; Keyser, A. Impact of coronary angiography early after CABG for suspected postoperative myocardial ischemia. J. Cardiothorac. Surg. 2019, 14, 54. [Google Scholar] [CrossRef] [PubMed]
- Ascenzo, F.; De Filippo, O.; Elia, E.; Doronzo, M.P.; Omedè, P.; Montefusco, A.; Pennone, M.; Salizzoni, S.; Conrotto, F.; Gallone, G.; et al. Percutaneous vs. surgical revascularization for patients with unprotected left main stenosis: A meta-analysis of 5 years follow-up RCTs. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 11, qcaa041. [Google Scholar] [CrossRef] [PubMed]


| Study | Design | Sample | TYPE OF CABG | Quality of Life Measurement Questionnaire | Follow-Up | Average (DE) Pre | Average (DE) Post | Main Results | EL/RG |
|---|---|---|---|---|---|---|---|---|---|
| Lie et al [22], 2010 Norway | Prospective Cohorts | 185 90% men | Elective | SF36 | Beforehand, after 6 months | MSC 47.7 (11.2) PCS 39.0 (SD 10.2) | MSC 51.3 (10.7) PCS 47.2 (SD 9.8) | Studying cardiac, non-cardiac, preoperative and early postoperative factors helps us predict the quality of life of patients after surgery. | 2b/B |
| Sjöland et al. [18], 1997 Sweden | Prospective Cohorts | Pre: 1160 Post-3 months: 1059, 1 year: 1045, 2 years: 1027 83% men | Emergency and Elective | NHP | Beforehand (at angiography appointment), after 3 months, 1 year, 2 years | 20.5 | 3 months: 11.4 1 year: 11.9 2 years: 10.4 | The greatest improvement in quality of life was at 3 months, for physical capacity and patient pain. Sexual problems persisted for 2 years after the surgery. | 2b/B |
| Sandau et al. [14], 2007 USA | Prospective Cohorts | 64 78.1% men | Elective | SF12 (short form of SF36) | 72 h beforehand, after 3 months | MCS 49.6 (9.6) PCS 40.0 (10.6) | MCS 53.2 (9.5) PCS 42.2 (10.3) | Participants gained an average of 2.2 points (PCS) and 3.6 points (MCS). Although these changes appear small, the clinical significance of changes in an individual’s score depends largely on the functional capacity associated with the score. | 2b/B |
| Ballan and Lee [23], 2007 Australia | Quasi-experimental | 62 87.1% men | Elective | SF36 | Beforehand, after 6 weeks | MSC 53.4 (12.7) PSC 26.1 (8.0) | MSC 53.7 (10.1) PSC 33.5 (10.2) | The PCS scores improved and were statistically significant 6 weeks after surgery. No significant differences were found in MCS scores. | 1B/A |
| Herlitz et al. [19], 2003 Sweden | Prospective Cohorts | 1225 (beforehand), 1358 (5 years), 976 (10 years) 98.5% men | Emergency and elective | NHP | Beforehand (during angiography), after 5 years, and 10 years | 20.8 | 12.1 (5 years) 14.5 (10 years) | Patient quality of life improved, generally, at 10 years, despite increasing age. The scores for the second and third measurements deteriorated. | 2b/B |
| Oreel et al. [24], 2020 The Netherlands | Prospective Cohorts | 48 87.5% men | Elective | SF36 | Beforehand, after 6 months | MCS 46.2(-) PCS 36(-) | MCS 51.9(-) PCS 43(-) | Quality of life was lower in women, and their physical health improved more slowly than that of male patients. | 2b/B |
| Herlitz et al. [20], 2005 Sweden | Prospective Cohorts | 637 75% men | (1) normal waiting list, (2) admitted patients, (3) patients with unstable angina, (4) emergency patients with unstable angiography, (5) emergency patients with acute myocardial infaction, (6) emergency patients with ventricular fibrillation | NHP | Beforehand, after 10 years | - | - | Being female, age, hypertension, obesity, renal failure, and cerebrovascular disease all play a role in the post-surgery recovery of quality of life. | 2b/B |
| Neto et al. [25], 2010 Poland | Prospective Cohorts | 44 59% men | Elective | SF36 | Beforehand, after 3 and 6 months | - | - | The older population presents both cardiovascular and quality of life improvement after surgery. There are no statistically significant changes in the physical abilities of patients. | 2b/B |
| Edell-Gustafsson et al [21], 1997 Sweden | Prospective cohorts (Pilot study) | 6 beforehand 5 after 100% men | Elective | NHP | Two days beforehand, 1 month after | 8.3 | 5.8 | After a month, quality of life improved, although wound pain persisted influencing sleep quality. | 2b/B |
| Grady et al. [15], 2011 USA | Prospective cohorts | 136 70% men | Elective | SF36 | Beforehand, after 3, 6, 12 months. Annually | MSC 51.88 (2.24) PSC 43.33 (2.73) | MSC 54.94 (1.61) PSC 51.65 (1.93) | There was an improvement in the quality of life between 3 and 6 months. After 3 years, it remained stable. | 2b/B |
| Sjöland et al. [18], 1999 Sweden | Prospective cohorts | 1160 83% men | - | NHP | Beforehand, 3 months, after 1 year, and 2 years | Men 19 Women 28 | Men 10.4-8.7 Women 13.9-13.6 | The women presented increased concomitant illnesses and a lower quality of life. The men encountered greater sexual problems prior to and 2 years after the surgery. | 2b/B |
| Rumsfeld et al. [16], 2004 USA | Prospective cohorts | 1973 99% men | - | SF36 | Beforehand and after 6 months | MCS 44.3 PCS 33.0 | MSC 46.1 PCS 38.2 | Being a smoker and presenting a psychiatric pathology influences post-surgery quality of life. | 2b/B |
| Mathisen et al. [26], 2007 Norway | Prospective cohorts | 108 81% men | - | SF36 (General-care subscale) | Beforehand, after 3 months, 6 months, and 1 year | 57.7 (21.1) | 67.2 (19.7) | Quality of life can both influence and be used as a health status outcome after surgery. Most of the improvements in quality of life occurred in the first 3 months. | 2b/B |
| Peric et al. [28], 2006 Serbia | Prospective cohorts | 243 80% men | - | NHP | Beforehand and after 6 months | - | - | Patients with a higher degree of angina had worse quality of life both before and after the operation | 2b/B |
| Peric et al. [27], 2005 Serbia | Prospective cohorts | 243 80% men | Elective | NHP | Beforehand and after 6 months | - | - | Patients with a high mortality risk according to EUROSCORE have a worse quality of life before surgery and improved perceived energy after surgery. | 2b/B |
| Peric et al. [29], 2010 Serbia | Prospective cohorts | 243 80% men | Elective | NHP | Beforehand and after 6 months | - | - | Although the quality of life of both sexes improves after CABG, women have a worse quality of life both before and after surgery. | 2b/B |
| Dimension | Prevalence Pre (CI-95%) | Prevalence Post (CI-95%) |
|---|---|---|
| Impact on working life | 17% (2–42%) | 6% (1–15%) |
| Impact on work/housework | 27% (5–59%) | 11% (3–23%) |
| Impact on social life | 15% (4–33%) | 4% (1–10%) |
| Impact on family relationships | 9% (2–20%) | 3% (1–9%) |
| Impact on sex life | 23% (2–58%) | 14% (1–40%) |
| Impact on hobbies | 30% (3–70%) | 12% (2–28%) |
| Impact on holidays | 22% (2–58%) | 8% (1–20%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmidt-RioValle, J.; Abu Ejheisheh, M.; Membrive-Jiménez, M.J.; Suleiman-Martos, N.; Albendín-García, L.; Correa-Rodríguez, M.; Gómez-Urquiza, J.L. Quality of Life After Coronary Artery Bypass Surgery: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8439. https://doi.org/10.3390/ijerph17228439
Schmidt-RioValle J, Abu Ejheisheh M, Membrive-Jiménez MJ, Suleiman-Martos N, Albendín-García L, Correa-Rodríguez M, Gómez-Urquiza JL. Quality of Life After Coronary Artery Bypass Surgery: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(22):8439. https://doi.org/10.3390/ijerph17228439
Chicago/Turabian StyleSchmidt-RioValle, Jacqueline, Moath Abu Ejheisheh, María José Membrive-Jiménez, Nora Suleiman-Martos, Luis Albendín-García, María Correa-Rodríguez, and José Luis Gómez-Urquiza. 2020. "Quality of Life After Coronary Artery Bypass Surgery: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 22: 8439. https://doi.org/10.3390/ijerph17228439
APA StyleSchmidt-RioValle, J., Abu Ejheisheh, M., Membrive-Jiménez, M. J., Suleiman-Martos, N., Albendín-García, L., Correa-Rodríguez, M., & Gómez-Urquiza, J. L. (2020). Quality of Life After Coronary Artery Bypass Surgery: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(22), 8439. https://doi.org/10.3390/ijerph17228439








