Survival and Estimation of Direct Medical Costs of Hospitalized COVID-19 Patients in the Kingdom of Saudi Arabia
Abstract
:1. Introduction
2. Methods
2.1. Ethical Approval of the Study Protocol
2.2. Data Source
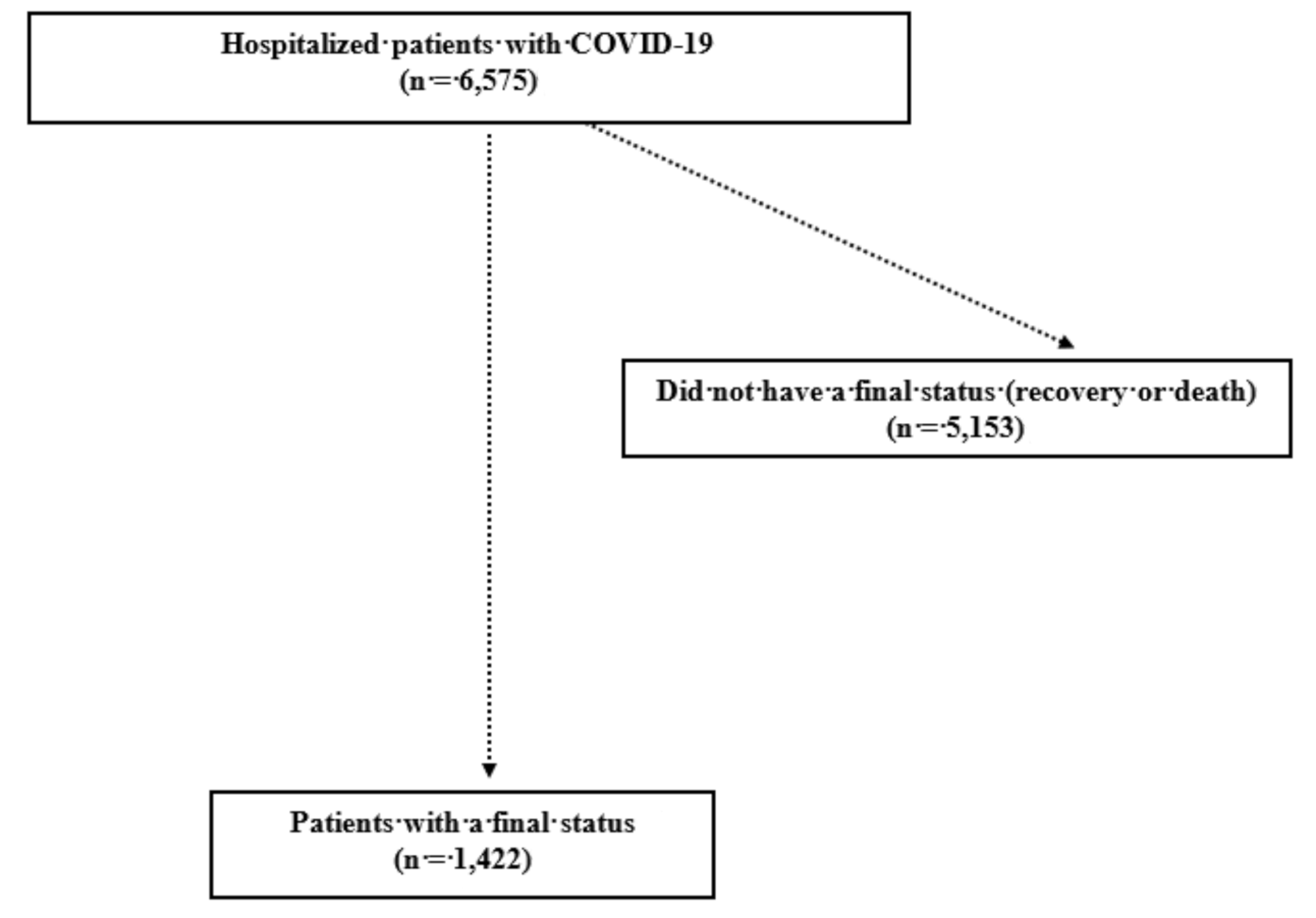
2.3. Inclusion/Exclusion Criteria
2.4. Statistical Analyses
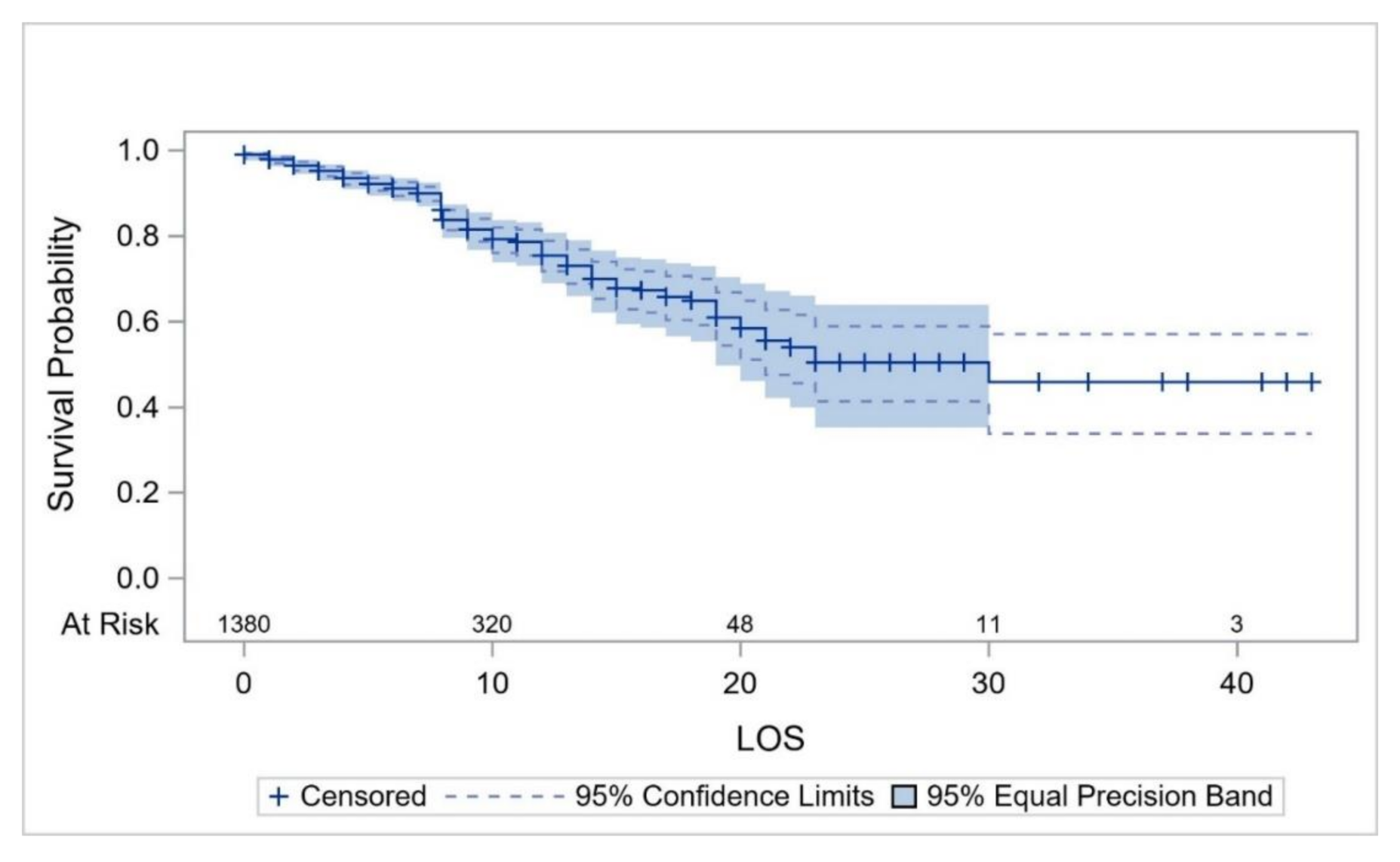
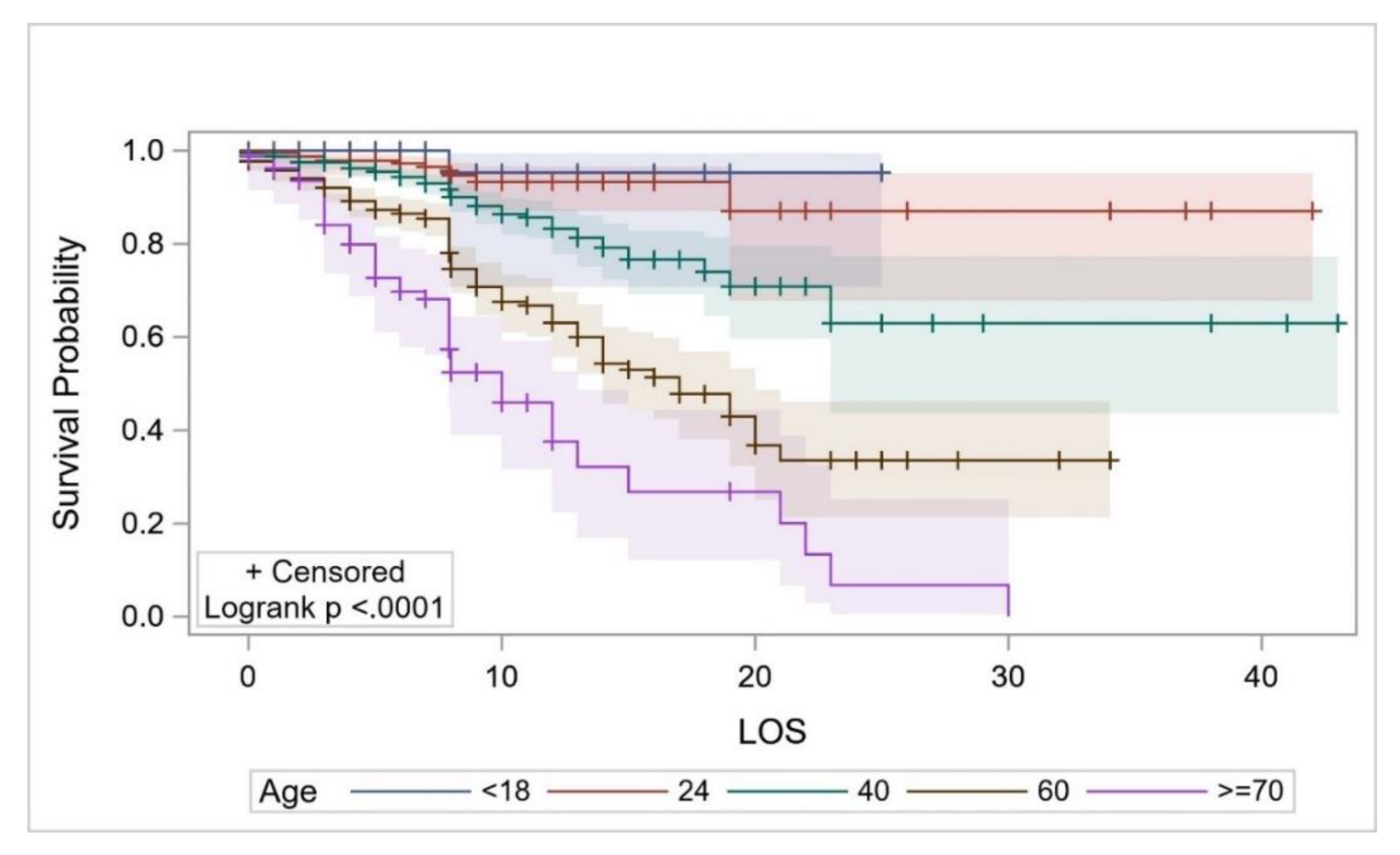
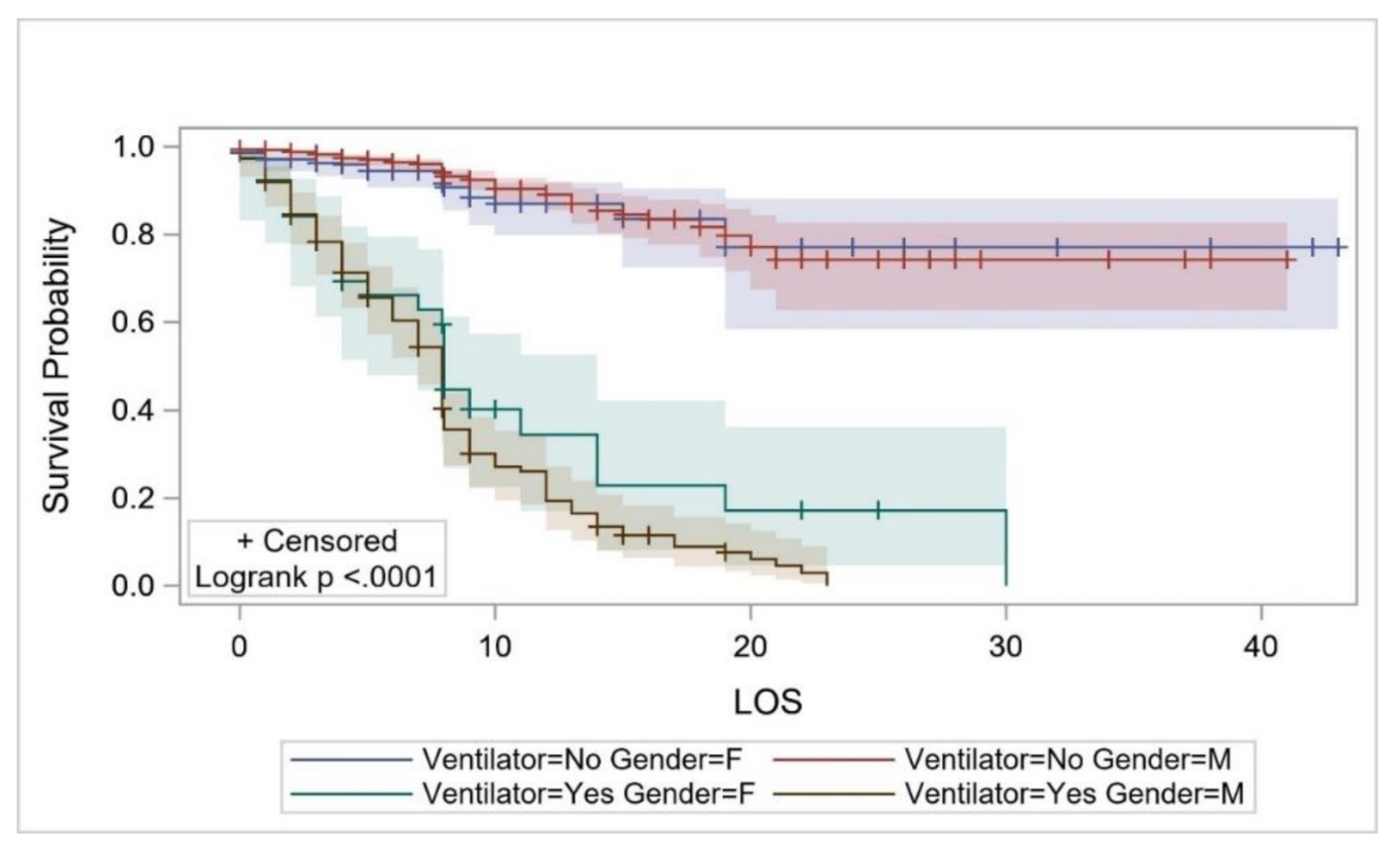
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Ludvigsson, J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020, 109, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Weekly, C.C. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19)—China, 2020. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 2, 113–122. [Google Scholar] [CrossRef]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 2020. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Salje, H.; Kiem, C.T.; Lefrancq, N.; Courtejoie, N.; Bosetti, P.; Paireau, J.; Andronico, A.; Hozé, N.; Richet, J.; Dubost, C.-L.; et al. Estimating the burden of SARS-CoV-2 in France. Science 2020, eabc3517. [Google Scholar] [CrossRef]
- Giangreco, G. Case fatality rate analysis of Italian COVID-19 outbreak. J. Med. Virol. 2020, 92, 919–923. [Google Scholar] [CrossRef] [Green Version]
- Mi, Y.-N.; Huang, T.-T.; Zhang, J.-X.; Qin, Q.; Gong, Y.-X.; Liu, S.-Y.; Xue, H.-M.; Ning, C.-H.; Cao, L.; Cao, Y.-X. Estimating the instant case fatality rate of COVID-19 in China. Int. J. Infect. Dis. 2020, 97, 1–6. [Google Scholar] [CrossRef]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Phua, J.; Weng, L.; Ling, L.; Egi, M.; Lim, C.-M.; Divatia, J.V.; Shrestha, B.R.; Arabi, Y.M.; Ng, J.; Gomersall, C.D.; et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir. Med. 2020, 8, 506–517. [Google Scholar] [CrossRef]
- Alsofayan, Y.M.; Althunayyan, S.M.; Khan, A.A.; Hakawi, A.M.; Assiri, A.M. Clinical characteristics of COVID-19 in Saudi Arabia: A national retrospective study. J. Infect. Public Health 2020, 13, 920–925. [Google Scholar] [CrossRef] [PubMed]
- AlRuthia, Y.; Somily, A.M.; Alkhamali, A.S.; Bahari, O.H.; AlJuhani, R.J.; Alsenaidy, M.; Balkhi, B. Estimation of Direct Medical Costs of Middle East Respiratory Syndrome Coronavirus Infection: A Single-Center Retrospective Chart Review Study. Infect. Drug Resist. 2019, 12, 3463–3473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Saudi Ministry of Health (MOH) COVID-19 Media Center. 2020. Available online: https://covid19.moh.gov.sa (accessed on 22 June 2020).
- Khafaie, M.A.; Rahim, F. Perspectives, R. Cross-country comparison of case fatality rates of COVID-19/SARS-COV-2. Osong Public Health Res. Perspect. 2020, 11, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Docherty, A.B.; Harrison, E.M.; Green, C.A.; Hardwick, H.E.; Pius, R.; Norman, L.; A Holden, K.; Read, J.M.; Dondelinger, F.; Carson, G.; et al. Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol. Clin. Characterisation Protoc. 2020, 2020. [Google Scholar] [CrossRef]
- Giorgi Rossi, P.; Ferroni, E.; Spila Alegiani, S.; Leoni, O.; Pitter, G.; Cereda, D.; Marino, M.; Pellizzari, M.; Sultana, J.; Trifirò, G.; et al. Survival of hospitalized COVID-19 patients in Northern Italy: A population-based cohort study by the ITA-COVID19 Network. medRxiv 2020. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhanm, M.; Crawfordm, J.M.; McGinn, T.; Davidson, K.W. The Northwell COVID-19 Research Consortium. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Wang, Z.; Ji, J.S.; Liu, Y.; Liu, R.; Zha, Y.; Chang, X.; Zhang, L.; Zhang, Y.; Zeng, J.; Dong, T.; et al. Survival analysis of hospital length of stay of novel coronavirus (COVID-19) pneumonia patients in Sichuan, China. medRxiv. 2020, 2020. [Google Scholar] [CrossRef]
- Du, R.-H.; Liang, L.-R.; Yang, C.-Q.; Wang, W.; Cao, T.-Z.; Li, M.; Guo, G.-Y.; Du, J.; Zheng, C.-L.; Zhu, Q.; et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. Eur. Respir. J. 2020, 55, 2000524. [Google Scholar] [CrossRef] [Green Version]
- Tian, W.; Jiang, W.; Yao, J.; Nicholson, C.J.; Li, R.H.; Sigurslid, H.H.; Wooster, L.; Rotter, J.I.; Guo, X.; Malhotra, R. Predictors of mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Abate, S.; Checkol, Y.; Mantedafro, B.; Basu, B. Prevalence and risk factors of mortality among hospitalized patients with COVID-19: A systematic review and Meta-analysis. Bull. World Health Organ. 2020. [CrossRef]
- Jin, J.-M.; Bai, P.; He, W.; Wu, F.; Liu, X.-F.; Han, D.-M.; Liu, S.; Yang, J.-K. Gender Differences in Patients with COVID-19: Focus on Severity and Mortality. Front. Public Heal. 2020, 8, 152. [Google Scholar] [CrossRef] [PubMed]
- Wenham, C.; Smith, J.; Morgan, R. COVID-19: The gendered impacts of the outbreak. Lancet 2020, 395, 846–848. [Google Scholar] [CrossRef] [Green Version]
- Auld, S.C.; Caridi-Scheible, M.; Blum, J.M.; Robichaux, C.; Kraft, C.; Jacob, J.T.; Jabaley, C.S.; Carpenter, D.; Kaplow, R.; Hernandez-Romieu, A.C.; et al. ICU and Ventilator Mortality among Critically Ill Adults with Coronavirus Disease 2019. Crit. Care Med. 2020. [Google Scholar] [CrossRef]
- Pareek, M.; Bangash, M.N.; Pareek, N.; Pan, D.; Sze, S.; Minhas, J.S.; Hanif, W.; Khunti, K. Ethnicity and COVID-19: An urgent public health research priority. Lancet 2020, 395, 1421–1422. [Google Scholar] [CrossRef]
- Rae, M.; Claxton, G.; Kurani, N.; McDermott, D.; Cox, C. Potential Costs of Coronavirus Treatment for People with Employer Coverage. Peterson–KFF Health System Tracker Website. 2020. Available online: org/brief/potential-costs-of-coronavirus-treatment-for-people-with-employer-coverage/ (accessed on 21 June 2020).
- Xijin, H. China Spends $2395 on Average for each COVID-19 Patient. 2020. Available online: https://www.globaltimes.cn/content/1184060.shtml (accessed on 22 June 2020).
- Wang, Q.; Shi, N.; Huang, J.; Cui, T.; Yang, L.; Ai, J.; Ji, H.; Xu, K.; Ahmad, T.; Bao, C.; et al. Effectiveness and cost-effectiveness of public health measures to control COVID-19: A modelling study. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Rao, S.R. Rs 3.5 Lakh Spent on Each Covid-19 Patient in Victoria Hospital: Karnataka Minister. 2020. Available online: https://timesofindia.indiatimes.com/city/bengaluru/rs-3-5-lakh-spent-on-each-covid-19-patient-in-victoria-hospital-karnataka-minister/articleshow/75639482.cms (accessed on 22 June 2020).
- Bartsch, S.M.; Ferguson, M.C.; McKinnell, J.A.; O’Shea, K.J.; Wedlock, P.T.; Siegmund, S.S.; Lee, B.Y. The Potential Health Care Costs and Resource Use Associated with COVID-19 in The United States. Health Aff. (Project Hope) 2020, 39, 927–935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sjödin, H.; Johansson, A.F.; Brännström, Å.; Farooq, Z.; Kriit, H.K.; Wilder-Smith, A.; Ås tröm, C.; Thunberg, J.; Rocklöv, J. Covid-19 health care demand and mortality in Sweden in response to non-pharmaceutical (NPIs) mitigation and suppression scenarios. Int. J. Epidemiol. 2020. [Google Scholar] [CrossRef]

| Characteristic | N (%) |
|---|---|
| Sex | |
| Male | 1105 (77.71) |
| Female | 317 (22.29) |
| Age group (years) | |
| 0–4 | 19 (1.34) |
| 5–14 | 24 (1.69) |
| 15–24 | 77 (5.41) |
| 25–34 | 351 (24.68) |
| 35–44 | 317 (22.29) |
| 45–54 | 294 (20.68) |
| 55–64 | 191 (13.43) |
| 65–74 | 98 (6.89) |
| 75–84 | 36 (2.53) |
| ≥85 | 15 (1.05) |
| Nationality | |
| Saudi | 444 (31.22) |
| Non-Saudi | 978 (68.78) |
| City | |
| Al Ahsa | 82 (5.77) |
| AlBahah | 39 (2.74) |
| Sakaka | 4 (0.28) |
| Khamis Mushait | 11 (0.77) |
| Bisha | 5 (0.35) |
| Hafar Al Batin | 2 (0.14) |
| Hail | 38 (2.67) |
| Jizan | 16 (1.13) |
| Makkah | 205 (14.42) |
| Medina | 824 (57.95) |
| Najran | 37 (2.60) |
| Arar | 2 (0.14) |
| Buraydah | 52 (3.66) |
| Al Qunfudhah | 5 (0.35) |
| Riyadh | 4 (0.28) |
| Tabouk | 39 (2.74) |
| Taif | 57 (4.01) |
| Inpatient environment | |
| GMW | 1200 (84.39) |
| ICU | 222 (15.61) |
| Use of mechanical ventilator | |
| Yes | 188 (13.22) |
| No | 1234 (86.78) |
| Characteristic | Mean Survival ± SE | P |
|---|---|---|
| Overall | 21.44 ± 0.55 | — |
| Sex | ||
| Male | 17.78 ± 0.34 | 0.597 |
| Female | 22.81 ± 1.08 | |
| Age (years) | ||
| 30 to <50 | 18.12 ± 0.29 | <0.0001 * |
| 50 to <70 | 14.63 ± 0.47 | |
| ≥70 | 12.01 ± 1.34 | |
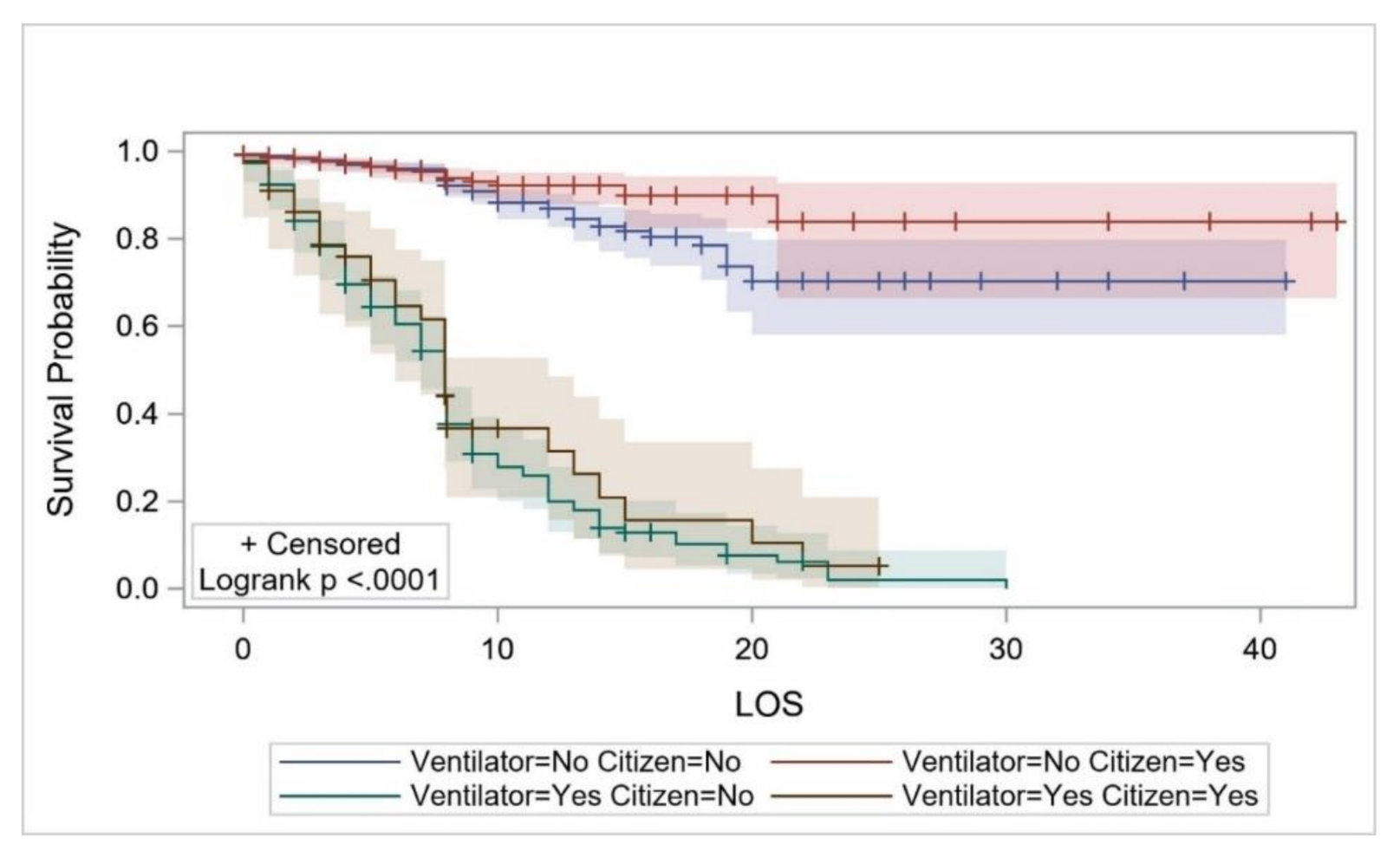
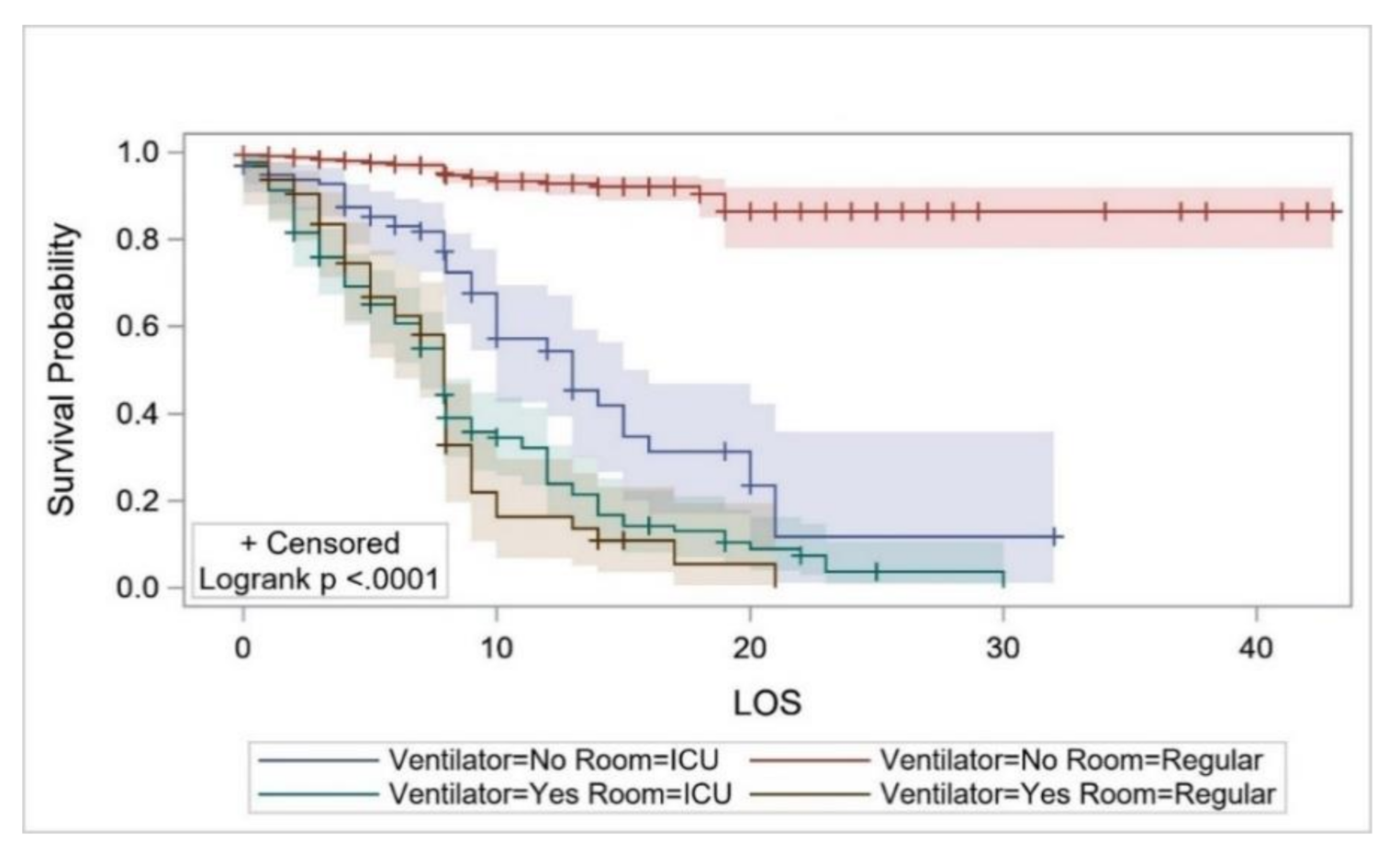
| Use of mechanical ventilator | ||
| Yes | 8.87 ± 0.55 | <0.0001 * |
| No | 18.93 ± 0.21 | |
| Inpatient environment | ||
| ICU | 11.13 ± 0.66 | <0.0001 * |
| GMW | 18.893 ± 0.21 |
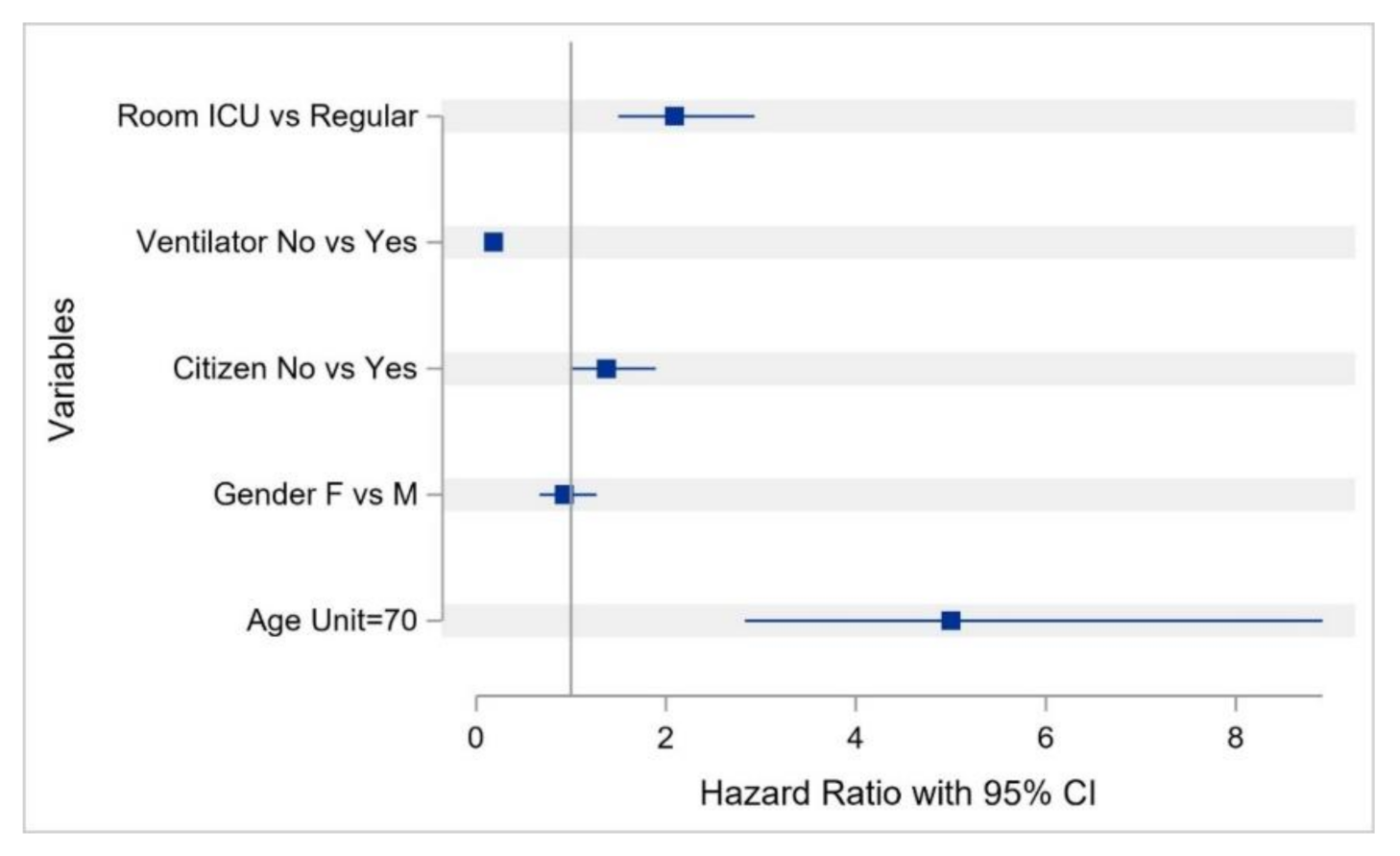
| Variable | HR (95%CI) | P |
|---|---|---|
| Age | 1.023 (1.01–1.03) | <0.0001 * |
| Sex (female vs. male) | 0.944 (0.68–1.30) | 0.725 |
| Use of mechanical ventilator (no vs. yes) | 0.194 (0.137–0.273) | <0.0001 * |
| Nationality (non-Saudi vs. Saudi) | 1.36 (1.001–1.865) | 0.049 * |
| Inpatient environment (ICU vs. GMW) | 2.088 (1.495–2.916) | <0.0001 * |
| Inpatient Setting | Mechanical-Ventilator Use | Number of Patients | Mean ± SD | Median (Q1-Q3) |
|---|---|---|---|---|
| ICU | No | 97 | 73,289.57 ± 47,216.44 | 54,603.92 (54,603.92–81,140.48) |
| Yes | 125 | 84,174.19 ± 61,162.84 | 78,625.02 (44,080.16–88,030.36) | |
| GMW | No | 1137 | 42,712.59 ± 30,048.16 | 38,436.71 (25,306.50–43,231.70) |
| Yes | 63 | 42,558.34 ± 25,360.95 | 38,207.80 (28,445.20–47,970.40) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, A.A.; AlRuthia, Y.; Balkhi, B.; Alghadeer, S.M.; Temsah, M.-H.; Althunayyan, S.M.; Alsofayan, Y.M. Survival and Estimation of Direct Medical Costs of Hospitalized COVID-19 Patients in the Kingdom of Saudi Arabia. Int. J. Environ. Res. Public Health 2020, 17, 7458. https://doi.org/10.3390/ijerph17207458
Khan AA, AlRuthia Y, Balkhi B, Alghadeer SM, Temsah M-H, Althunayyan SM, Alsofayan YM. Survival and Estimation of Direct Medical Costs of Hospitalized COVID-19 Patients in the Kingdom of Saudi Arabia. International Journal of Environmental Research and Public Health. 2020; 17(20):7458. https://doi.org/10.3390/ijerph17207458
Chicago/Turabian StyleKhan, Anas A., Yazed AlRuthia, Bander Balkhi, Sultan M. Alghadeer, Mohamad-Hani Temsah, Saqer M. Althunayyan, and Yousef M. Alsofayan. 2020. "Survival and Estimation of Direct Medical Costs of Hospitalized COVID-19 Patients in the Kingdom of Saudi Arabia" International Journal of Environmental Research and Public Health 17, no. 20: 7458. https://doi.org/10.3390/ijerph17207458







