Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review
Abstract
1. Introduction
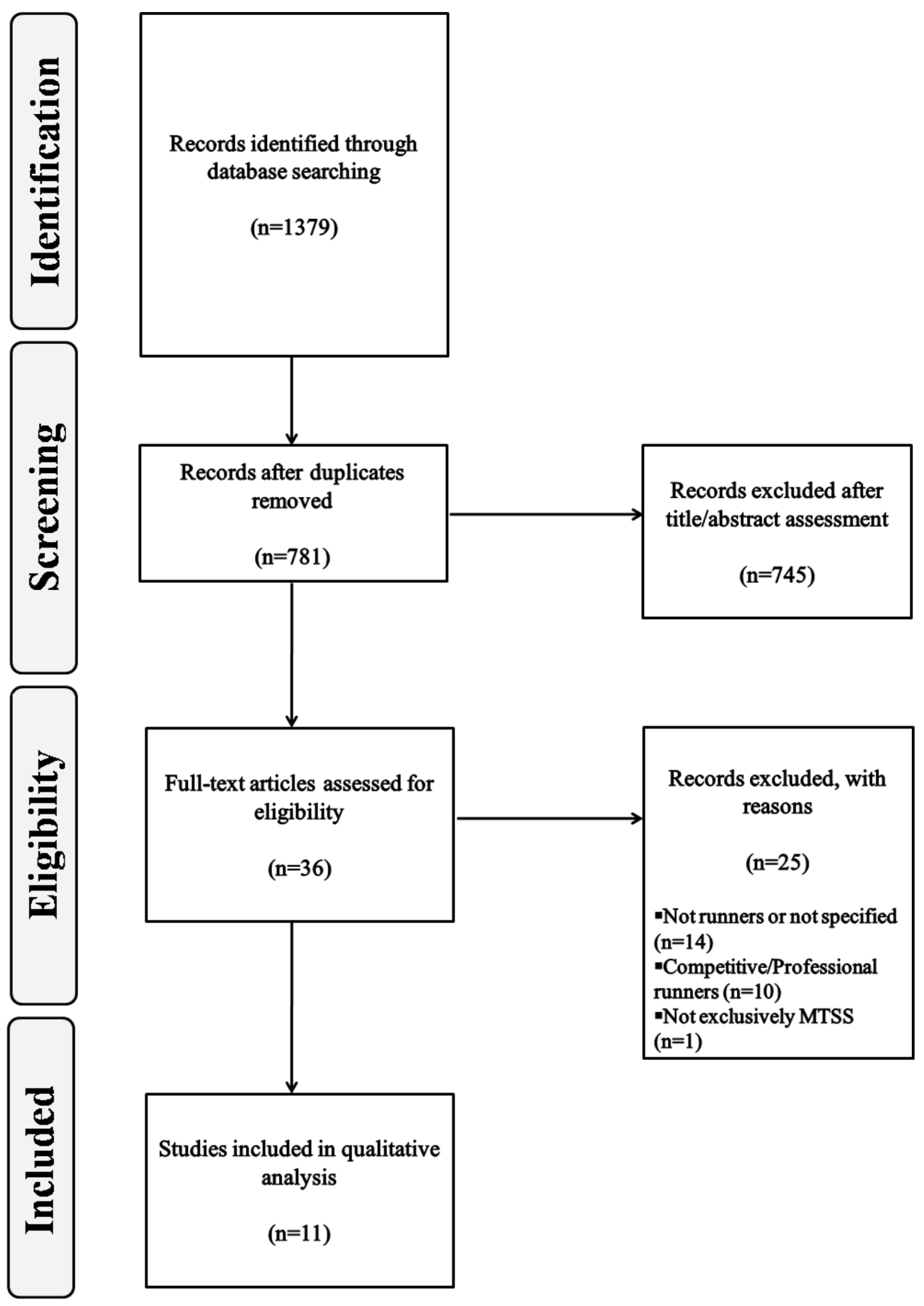
2. Materials and Methods
2.1. Search Strategy and Study Selection
2.2. Data Extraction and Analysis
2.3. Quality Assessment
3. Results
3.1. Etiological Factors
3.2. Diagnostic Procedures
3.3. Treatment Methods and Time to Recovery
4. Discussion
4.1. Clinical Relevance
- To undergo a biomechanical analysis of running movements to identify risk factors for injury.
- To perform a specific running technique to improve running kinematics. This training protocol should be accompanied by strength and neuromuscular control exercises.
- To establish a gradual running program with proper recovery times, in order to manage pain and prevent injury recurrence.
4.2. Quality of the Studies and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| #1 | “running”[Mesh] |
| #2 | “running”[tiab] |
| #3 | #1 OR #2 |
| #4 | “athletes”[Mesh] |
| #5 | “athlete*”[tiab] |
| #6 | #4 OR #5 |
| #7 | “novice”[tiab] |
| #8 | “recreational”[tiab] |
| #9 | #7 OR #8 |
| #10 | “medial tibial stress syndrome”[Mesh] |
| #11 | “medial tibial stress syndrome”[tiab] |
| #12 | #10 OR #11 |
| #13 | #3 AND #6 AND #9 AND #12 |
References
- Van Middelkoop, M.; Kolkman, J.; Van Ochten, J.; Bierma-Zeinstra, S.M.; Koes, B.W. Risk factors for lower extremity injuries among male marathon runners. Scand. J. Med. Sci. Sport 2008, 18, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Nikolaidis, P.; Rosemann, T.; Knechtle, B. A Brief Review of Personality in Marathon Runners: The Role of Sex, Age and Performance Level. Sports 2018, 6, 99. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.D.; Ong, J.C.; Wang, G. Historical analysis of participation in 161km ultramarathons in North America. Int. J. Hist. Sport 2010, 27, 1877–1891. [Google Scholar] [CrossRef] [PubMed]
- Hespanhol Junior, L.C.; Pillay, J.D.; van Mechelen, W.; Verhagen, E. Meta-Analyses of the Effects of Habitual Running on Indices of Health in Physically Inactive Adults. Sport Med. 2015, 45, 1455–1468. [Google Scholar] [CrossRef]
- Videbæk, S.; Bueno, A.M.; Nielsen, R.O.; Rasmussen, S. Incidence of Running-Related Injuries Per 1000 h of running in Different Types of Runners: A Systematic Review and Meta-Analysis. Sport Med. 2015, 45, 1017–1026. [Google Scholar] [CrossRef]
- Hreljac, A. Etiology, prevention, and early intervention of overuse injuries in runners: A biomechanical perspective. Phys. Med. Rehabil. Clin. N. Am. 2005, 16, 651–667. [Google Scholar] [CrossRef]
- Hespanhol Junior, L.C.; de Carvalho, A.C.; Costa, L.O.; Lopes, A.D. Lower limb alignment characteristics are not associated with running injuries in runners: Prospective cohort study. Eur. J. Sport Sci. 2016, 16, 1137–1144. [Google Scholar] [CrossRef]
- Malisoux, L.; Nielsen, R.O.; Urhausen, A.; Theisen, D. A step towards understanding the mechanisms of running-related injuries. J. Sci. Med. Sport 2015, 18, 523–528. [Google Scholar] [CrossRef]
- van Gent, R.N.; Siem, D.; van Middelkoop, M.; van Os, A.G.; Bierma-Zeinstra, S.M.A.; Koes, B.W. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br. J. Sports Med. 2007, 41, 469–480. [Google Scholar] [CrossRef]
- Lopes, A.D.; Hespanhol Junior, L.C.; Yeung, S.S.; Costa, L.O.P.; Hespanhol Junior, L.C.; Yeung, S.S.; Costa, L.O.P. What are the main running-related musculoskeletal injuries? A Systematic Review. Sports Med. 2012, 42, 891–905. [Google Scholar] [CrossRef]
- Yates, B.; White, S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am. J. Sports Med. 2004, 32, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Beck, B.R. Tibial stress injuries. An aetiological review for the purposes of guiding management. Sport Med. 1998, 26, 265–279. [Google Scholar] [CrossRef]
- Mubarak, S.J.; Gould, R.N.; Lee, Y.F.; Schmidt, D.A.; Hargens, A.R. The medial tibial stress syndrome. A cause of shin splints. Am J Sports Med. 1982, 10, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Reshef, N.; Guelich, D.R. Medial tibial stress syndrome. Clin. Sports Med. 2012, 31, 273–290. [Google Scholar] [CrossRef]
- Becker, J.; Nakajima, M.; Wu, W.F.W. Factors Contributing to Medial Tibial Stress Syndrome in Runners: A Prospective Study. Med. Sci. Sports Exerc. 2018, 50, 2092–2100. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.; James, S.; Wayner, R.; Osternig, L.; Chou, L.-S.S. Biomechanical Factors Associated with Achilles Tendinopathy and Medial Tibial Stress Syndrome in Runners. Am. J. Sports Med. 2017, 45, 2614–2621. [Google Scholar] [CrossRef] [PubMed]
- Buist, I.; Bredeweg, S.W.; Lemmink, K.A.; Van Mechelen, W.; Diercks, R.L. Predictors of running-related injuries in novice runners enrolled in a systematic training program: A prospective cohort study. Am. J. Sports Med. 2010, 38, 273–280. [Google Scholar] [CrossRef]
- Linton, L.; Valentin, S. Running with injury: A study of UK novice and recreational runners and factors associated with running related injury. J. Sci. Med. Sport 2018, 21, 1221–1225. [Google Scholar] [CrossRef]
- Kemler, E.; Blokland, D.; Backx, F.; Huisstede, B. Differences in injury risk and characteristics of injuries between novice and experienced runners over a 4-year period. Phys. Sportsmed. 2018, 46, 485–491. [Google Scholar] [CrossRef]
- Panic, N.; Leoncini, E.; de Belvis, G.; Ricciardi, W.; Boccia, S. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS ONE 2013, 8, e83138. [Google Scholar] [CrossRef]
- Sherrington, C.; Herbert, R.D.; Maher, C.G.; Moseley, A.M. PEDro. A database of randomized trials and systematic reviews in physiotherapy. Man. Ther. 2000, 5, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’Connell, J.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality if Nonrandomized Studies in Meta-Analyses. 2009. Available online: https://www.researchgate.net/publication/261773681_The_Newcastle-Ottawa_Scale_NOS_for_Assessing_the_Quality_of_Non-Randomized_Studies_in_Meta-Analysis (accessed on 9 August 2020).
- Newman, P.; Waddington, G.; Adams, R. Shockwave treatment for medial tibial stress syndrome: A randomized double blind sham-controlled pilot trial. J. Sci. Med. Sport 2017, 20, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Aweid, O.; Gallie, R.; Morrissey, D.; Crisp, T.; Maffulli, N.; Malliaras, P.; Padhiar, N. Medial tibial pain pressure threshold algometry in runners. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Loudon, J.K.; Reiman, M.P. Lower extremity kinematics in running athletes with and without a history of medial shin pain. Int. J. Sports Phys. Ther. 2012, 7, 356–364. [Google Scholar]
- Naderi, A.; Degens, H.; Sakinepoor, A. Arch-support foot-orthoses normalize dynamic in-shoe foot pressure distribution in medial tibial stress syndrome. Eur. J. Sport Sci. 2019, 19, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Tweed, J.L.; Campbell, J.A.; Avil, S.J. Biomechanical risk factors in the development of medial tibial stress syndrome in distance runners. J. Am. Podiatr. Med. Assoc. 2008, 98, 436–444. [Google Scholar] [CrossRef]
- Loudon, J.K.; Dolphino, M.R. Use of foot orthoses and calf stretching for individuals with medial tibial stress syndrome. Foot Ankle Spec. 2010, 3, 15–20. [Google Scholar] [CrossRef]
- Mulvad, B.; Nielsen, R.O.; Lind, M.; Ramskov, D. Diagnoses and time to recovery among injured recreational runners in the RUN CLEVER trial. PLoS ONE 2018, 13, e0204742. [Google Scholar] [CrossRef]
- Nielsen, R.O.; Parner, E.T.; Nohr, E.A.; Sorensen, H.; Lind, M.; Rasmussen, S. Excessive progression in weekly running distance and risk of running-related injuries: An association which varies according to type of injury. J. Orthop. Sports Phys. Ther. 2014, 44, 739–747. [Google Scholar] [CrossRef]
- Nielsen, R.O.; Ronnow, L.; Rasmussen, S.; Lind, M. A prospective study on time to recovery in 254 injured novice runners. PLoS ONE 2014, 9, e99877. [Google Scholar] [CrossRef]
- Raissi, G.R.D.; Cherati, A.D.; Mansoori, K.D.; Razi, M.D. The relationship between lower extremity alignment and Medial Tibial Stress Syndrome among non-professional athletes. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2009, 1, 11. [Google Scholar] [CrossRef] [PubMed]
- Gaeta, M.; Minutoli, F.; Vinci, S.; Salamone, I.; D’Andrea, L.; Bitto, L.; Magaudda, L.; Blandino, A. High-resolution CT grading of tibial stress reactions in distance runners. Am. J. Roentgenol. 2006, 187, 789–793. [Google Scholar] [CrossRef]
- Winters, M.; Bakker, E.W.P.; Moen, M.H.; Barten, C.C.; Teeuwen, R.; Weir, A. Medial tibial stress syndrome can be diagnosed reliably using history and physical examination. Br. J. Sports Med. 2018, 52, 1267–1272. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.J.; Host, J.V.; Norton, B.J. Navicular drop as a composite measure of excessive pronation. J. Am. Podiatr. Med. Assoc. 1993, 83, 198–202. [Google Scholar] [CrossRef]
- Bennett, J.E.; Reinking, M.F.; Pluemer, B.; Pentel, A.; Seaton, M.; Killian, C. Factors Contributing to the Development of Medial Tibial Stress Syndrome in High School Runners. J. Orthop. Sports Phys. Ther. 2001, 31, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Ross, M.H.; Smith, M.D.; Mellor, R.; Vicenzino, B. Exercise for posterior tibial tendon dysfunction: A systematic review of randomised clinical trials and clinical guidelines. BMJ Open Sport Exerc. Med. 2018, 4. [Google Scholar] [CrossRef]
- Ferber, R.; Noehren, B.; Hamill, J.; Davis, I.S. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J. Orthop. Sports Phys. Ther. 2010, 40, 52–58. [Google Scholar] [CrossRef]
- Powers, C.M. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J. Orthop. Sports Phys. Ther. 2010, 40, 42–51. [Google Scholar] [CrossRef]
- Tiberio, D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: A theoretical model. J. Orthop. Sports Phys. Ther. 1987, 9, 160–165. [Google Scholar] [CrossRef]
- Khamis, S.; Yizhar, Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 2007, 25, 127–134. [Google Scholar] [CrossRef]
- Saeki, J.; Nakamura, M.; Nakao, S.; Fujita, K.; Yanase, K.; Morishita, K.; Ichihashi, N. Ankle and toe muscle strength characteristics in runners with a history of medial tibial stress syndrome. J. Foot Ankle Res. 2017, 10, 16. [Google Scholar] [CrossRef] [PubMed]
- Dorn, T.W.; Schache, A.G.; Pandy, M.G. Muscular strategy shift in human running: Dependence of running speed on hip and ankle muscle performance. J. Exp. Biol. 2012, 215, 1944–1956. [Google Scholar] [CrossRef] [PubMed]
- Schache, A.G.; Blanch, P.D.; Dorn, T.W.; Brown, N.A.T.; Rosemond, D.; Pandy, M.G. Effect of running speed on lower limb joint kinetics. Med. Sci. Sports Exerc. 2011, 43, 1260–1271. [Google Scholar] [CrossRef] [PubMed]
- Newman, P.; Witchalls, J.; Waddington, G.; Adams, R. Risk factors associated with medial tibial stress syndrome in runners: A systematic review and meta-analysis. Open Access J. Sport Med. 2013, 4, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Reinking, M.F.; Austin, T.M.; Richter, R.R.; Krieger, M.M. Medial Tibial Stress Syndrome in Active Individuals: A Systematic Review and Meta-analysis of Risk Factors. Sports Health 2017, 9, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Davis, I.S.; Bowser, B.J.; Mullineaux, D.R. Greater vertical impact loading in female runners with medically diagnosed injuries: A prospective investigation. Br. J. Sports Med. 2016, 50, 887–892. [Google Scholar] [CrossRef] [PubMed]
- Shen, P.; Mao, D.; Zhang, C.; Sun, W.; Song, Q. Effects of running biomechanics on the occurrence of iliotibial band syndrome in male runners during an eight-week running programme—A prospective study. Sports Biomech. 2019, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.; Greeves, J.P.; Byers, M.; Bennett, A.N.; Spears, I.R. Musculoskeletal injuries in British Army recruits: A prospective study of diagnosis-specific incidence and rehabilitation times Epidemiology of musculoskeletal disorders. BMC Musculoskelet. Disord. 2015, 16, 106. [Google Scholar] [CrossRef]
- Kinser, A.M.; Sands, W.A.; Stone, M.H. Reliability and validity of a pressure algometer. J. Strength Cond. Res. 2009, 23, 312–314. [Google Scholar] [CrossRef]
- Walton, D.; Macdermid, J.; Nielson, W.; Teasell, R.; Chiasson, M.; Brown, L. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J. Orthop. Sports Phys. Ther. 2011, 41, 644–650. [Google Scholar] [CrossRef]
- Magnusson, H.I.; Westlin, N.E.; Nyqvist, F.; Gärdsell, P.; Seeman, E.; Karlsson, M.K. Abnormally decreased regional bone density in athletes with medial tibial stress syndrome. Am. J. Sports Med. 2001, 29, 712–715. [Google Scholar] [CrossRef] [PubMed]
- Ozgürbüz, C.; Yüksel, O.; Ergün, M.; Işlegen, C.; Taskiran, E.; Denerel, N.; Karamizrak, O. Tibial bone density in athletes with medial tibial stress syndrome: A controlled study. J. Sports Sci. Med. 2011, 10, 743–747. [Google Scholar] [PubMed]
- Alfayez, S.M.; Ahmed, M.L.; Alomar, A.Z. A review article of medial tibial stress syndrome. J. Musculoskelet. Surg. Res. 2017, 1, 2. [Google Scholar]
- Winters, M.; Eskes, M.; Weir, A.; Moen, M.H.; Backx, F.J.; Bakker, E.W. Treatment of medial tibial stress syndrome: A systematic review. Sports Med. 2013, 43, 1315–1333. [Google Scholar] [CrossRef]
- Hume, P.; Hopkins, W.; Rome, K.; Maulder, P.; Coyle, G.; Nigg, B. Effectiveness of foot orthoses for treatment and prevention of lower limb injuries: A review. Sport Med. 2008, 38, 759–779. [Google Scholar] [CrossRef]
- Viitasalo, J.T.; Kvist, M. Some biomechanical aspects of the foot and ankle in athletes with and without shin splints. Am. J. Sports Med. 1983, 11, 125–130. [Google Scholar] [CrossRef]
- Vicenzino, B.; Griffiths, S.R.; Griffiths, L.A.; Hadley, A. Effect of antipronation tape and temporary orthotic on vertical navicular height before and after exercise. J. Orthop. Sports Phys. Ther. 2000, 30, 333–339. [Google Scholar] [CrossRef]
- MacLean, C.L.; Davis, I.S.; Hamill, J. Short- and long-term influences of a custom foot orthotic intervention on lower extremity dynamics. Clin. J. Sport Med. 2008, 18, 338–343. [Google Scholar]
- Arnold, J.B.; May, T.; Bishop, C. Predictors of the Biomechanical Effects of Customized Foot Orthoses in Adults With Flat-Arched Feet. Clin. J. Sport Med. 2018, 28, 398–400. [Google Scholar] [CrossRef]
- Moen, M.H.; Rayer, S.; Schipper, M.; Schmikli, S.; Weir, A.; Tol, J.L.; Backx, F.J.G. Shockwave treatment for medial tibial stress syndrome in athletes; a prospective controlled study. Br. J. Sports Med. 2012, 46, 253–257. [Google Scholar] [CrossRef]
- Rompe, J.D.; Cacchio, A.; Furia, J.P.; Maffulli, N. Low-energy extracorporeal shock wave therapy as a treatment for medial tibial stress syndrome. Am. J. Sports Med. 2010, 38, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Gomez Garcia, S.; Ramon Rona, S.; Gomez Tinoco, M.C.; Benet Rodriguez, M.; Chaustre Ruiz, D.M.; Cardenas Letrado, F.P.; Lopez-Illescas Ruiz, A.; Alarcon Garcia, J.M. Shockwave treatment for medial tibial stress syndrome in military cadets: A single-blind randomized controlled trial. Int. J. Surg. 2017, 46, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Moen, M.H.; Holtslag, L.; Bakker, E.; Barten, C.; Weir, A.; Tol, J.L.; Backx, F. The treatment of medial tibial stress syndrome in athletes; a randomized clinical trial. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2012, 4, 12. [Google Scholar] [CrossRef] [PubMed]
| Study | PEDro Score Distribution | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total PEDro Score | |
| Newman et al., 2017 [23] | 1 | 1 | 1 | 1 | 1 | ─ | 1 | 1 | 1 | 1 | 1 | 9 |
| Study Design | Study | Newcastle–Ottawa Scale | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Exposure /Outcome | Total Score | |||||||
| 1 | 2 | 3 | 4 | 1 | 1 | 2 | 3 | |||
| 1 | Aweid et al., 2014 [24] | ★ | ★ | ★★ | ★ | ★ | ★★★★★(6) | |||
| Loudon and Reiman, 2012 [25] | ★ | ★ | ★★ | ★ | ★ | ★ | ★★★★★★★(7) | |||
| Naderi et al., 2019 [26] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | ★★★★★★★★★(9) | |
| Tweed et al., 2008 [27] | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★★★★★★★★(8) | ||
| 2 | Loudon and Dolphino, 2010 [28] | ★ | ★ | ★ | ★★ | ★ | ★ | ★★★★★★★(7) | ||
| Mulvad et al., 2018 [29] | ★ | ★ | ★ | ★★★(3) | ||||||
| Nielsen et al., 2014 [30] | ★ | ★ | ★ | ★★ | ★ | ★ | ★★★★★★★(7) | |||
| Nielsen et al., 2014 [31] | ★ | ★ | ★ | ★ | ★ | ★ | ★★★★★★(6) | |||
| Raissi et al., 2009 [32] | ★ | ★ | ★ | ★★★ (3) | ||||||
| 3 | Gaeta et al., 2006 [33] | ★ | ★★ | ★ | ★★ | ★ | N/A | ★★★★★★★(7) | ||
| Study | Design Level of Evidence (NHMRC) | Participants | Methodology | Results (p <0.05) |
|---|---|---|---|---|
| Loudon and Reiman, 2012 [25] | Case–control III-3 | 28 runners ▪ 14 runners with a history of unilateral MTSS (8♂/6♀)
| ▪ Kinematic analysis of the pelvis, hip and knee during treadmill running | ▪ ↑ PD and peak hip IR, and ↓knee flexion ▪ ↑ PD in the injured limbin♀ vs. ♂ in the MTSS group |
| Nielsen et al., 2014 [30] | Cohort, prospective II | 873 runners ▪ 202 injured (106♂/96♀)
| ▪ Runners were divided into 3 groups according to progression in weekly running distance (wrd) | ▪ >30% wrd ↑ prevalence in MTSS |
| Raissi et al., 2009 [32] | Cohort, prospective II | 66 runners (21♂/45♀)
| Goniometric measurement: intercondylar and intermalleolar interval, Q angles, tibiofemoral angle, rear foot alignment (Achilles or calcaneal angle), tibial alignmentandND test. ▪ Tape measure measurement: leg length. 17-week running program | ▪ 16 runners developed MTSS bilaterally ▪ ↑ ND in MTSS runners |
| Tweed et al., 2008 [27] | Case–control III-3 | 40 runners
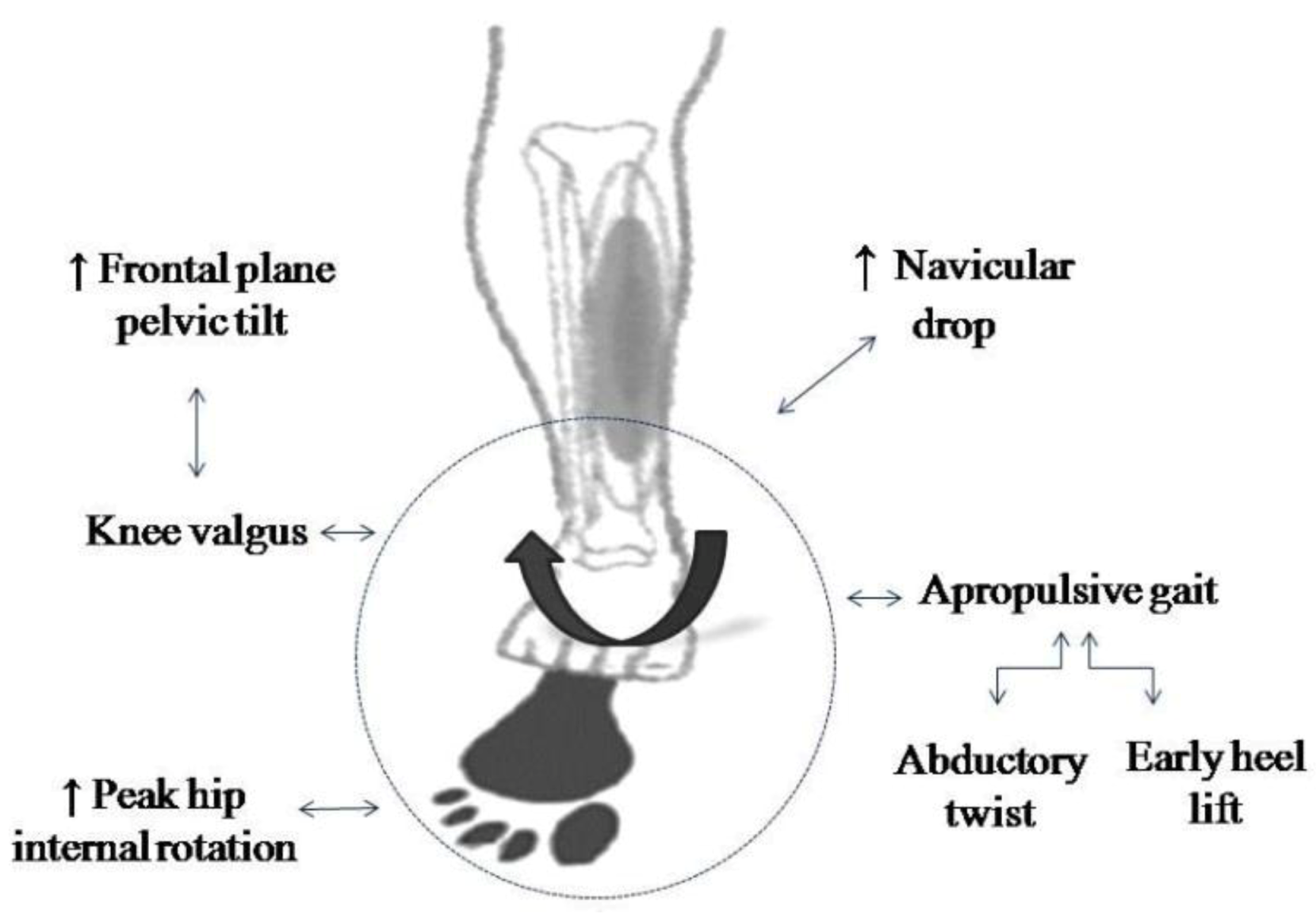
▪ 12 control runners (7♂, 5♀) | ▪ Foot type (Foot Posture Index) Talocrural joint dorsiflexion and the range of motion of the 1st MTPJ (tractography) ▪ Static and dynamic gait kinematic (treadmill running) | ▪ Predictors of MTSS: Difference between neutral and relaxed calcaneal; ROM of the talocrural joint;early heel lift;abductorytwistandapropulsive gait |
| Factors | Type | Study | |
|---|---|---|---|
| Intrinsic | Extrinsic | ||
| ↑ Pelvic drop | ✓ | Loudon and Reiman, 2012 [25] | |
| ↑ Peak hip internal rotation | ✓ | ||
| ↓ Knee flexion | ✓ | ||
| Female sex | ✓ | ||
| ↑ Walking distance | ✓ | Nielsen et al., 2014 [30] | |
| ↑ Navicular drop | ✓ | Raissi et al., 2009 [32] | |
| Early heel lift during the stance phase of gait | ✓ | Tweed et al., 2008 [27] | |
| Abductory twist during gait | ✓ | ||
| Apropulsive gait | ✓ | ||
| Pronation in a static position | ✓ | ||
| Study | Design Level of Evidence (NHMRC) | Participants | Methodology | Results (p < 0.05) |
|---|---|---|---|---|
| Aweid et al., 2014 [24] | Case–control III-3 | 29 runners ▪ 9 runners with MTSS (6♂/3♀)
| ▪ Pressure algometry
| Runners with MTSS: ▪ Males had >PPT than females at the 6/9 area of the tibia Comparison between groups: ▪ ↑ PPT for MTSS runners at the 3/9 site |
| Gaeta et al., 2006 [33] | Cross-sectional IV | 41 participants ▪ 20 asymptomatic runners (14♂/6♀)
| ▪ CT Tibias were classified according to the tibial cortex: - Type 0: no abnormality - Type 1: reduced cortical attenuation - Type 2: cortical osteopenia (MTSS) | ▪ Asymptomatic runners - Type 0: 22 - Type 1: 13 - Type 2: 5 ▪ Runners with MTSS -Type 0: 2 - Type 1: 3 - Type 2: 3 (painless) and 14 (pain) ▪ Symptomatic tibias with CT abnormalities: 100% ▪ Asymptomatic tibias with CT abnormalities: 16.6% |
| Study | Design Level of Evidence (NHMRC) | Participants | Methodology | Results (p <0.05) |
|---|---|---|---|---|
| Loudon and Dolphino, 2010 [28] | Case series IV | 23 runners with MTSS (12♂/11♀)
| Initial measurements: ▪ Alignment: ND test and talocrural dorsiflexion ROM ▪ Pain (NPRS) Treatment (3 weeks): ▪ Off-the-shelf BFO ▪ Home stretching program Follow-up: ▪ GRC questionnaire by email (Post 7 and 21 days) | ▪ ↓ Duration of the symptoms: 44% ♀and 83% ♂ ▪ ↓ Pain level in the successful group ▪ Improvement in GRC in the successful group (post 21 days) |
| Mulvad et al., 2018 [29] | Cohort III-2 | 112 injured runners (30♂/82♀)
| ▪ Clinical examinations | ▪ MTSS had the longest time to recovery (70 days) |
| Naderi et al., 2019 [26] | Case–control III-2 | 100 runners (100♂) ▪ 50 runners with MTSS
| ▪ Arch-support full-length footorthoses in the shoes ▪ Pain measurement (algometry, VAS) ▪ Foot postures (FPI-6) ▪ Dynamic pressure distribution during running (stance phase) | After using arch-support foot- orthosesin MTSS runners: ▪ ↓ Total contact time ▪ ↓ Absolute impulse in the midfoot region and ↑peak pressure and absolute impulse underneath the M5 region ▪ Pressure distribution was laterally at FFF and HO ▪ Pressure displacement was shifted from lateral to medial during FFCP and from medial to lateral during FFPOP ▪ The X-component of the COP was more medially at FFF and was displaced to lateral side during FFPOP ▪ The X-component of the COP was laterally at FFF and the lateral COP displacement ↓during FFPOP |
| Newman et al., 2017 [23] | Randomized controlled trial II | 24 runners with MTSS ▪ Experimental group: 12 (5♂/7♀)
| Treatment: ▪ Experimental group: standard dose shockwave therapy (total = 1450 mJ/mm2) ▪ Control group: sham dose shockwave therapy (total = 70 mJ/mm2)Measurements: ▪ Pain: pressure algometry and during running (NRS) ▪ Self GROC questionnaire Follow-up: 10 weeks | ▪ No significant differences between groups |
| Nielsen et al., 2014 [31] | Cohort III-2 | 254 injured runners ▪ 38 runners with MTSS (15%), (18♂/20♀) | ▪ Clinical examinations ▪ Prospective follow-up to determine time to recovery | ▪ Mean time to recovery of 72 days |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menéndez, C.; Batalla, L.; Prieto, A.; Rodríguez, M.Á.; Crespo, I.; Olmedillas, H. Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 7457. https://doi.org/10.3390/ijerph17207457
Menéndez C, Batalla L, Prieto A, Rodríguez MÁ, Crespo I, Olmedillas H. Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(20):7457. https://doi.org/10.3390/ijerph17207457
Chicago/Turabian StyleMenéndez, Claudia, Lucía Batalla, Alba Prieto, Miguel Ángel Rodríguez, Irene Crespo, and Hugo Olmedillas. 2020. "Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 20: 7457. https://doi.org/10.3390/ijerph17207457
APA StyleMenéndez, C., Batalla, L., Prieto, A., Rodríguez, M. Á., Crespo, I., & Olmedillas, H. (2020). Medial Tibial Stress Syndrome in Novice and Recreational Runners: A Systematic Review. International Journal of Environmental Research and Public Health, 17(20), 7457. https://doi.org/10.3390/ijerph17207457






