Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults
Abstract
1. Introduction
2. Methods
2.1. Study Design and Samples
2.2. Measures
2.2.1. Outcomes Variables
Depression
Post-Traumatic Stress Symptoms (PTSS)
Insomnia
Mental Health Problems
2.2.2. Independent Variables
Location Wuhan
Media Exposure
Direct Exposure to COVID-19
Impact on Livelihood
Coping Style
Practical Coping Behaviors
2.3. Covariates
2.4. Statistical Analyses
3. Results
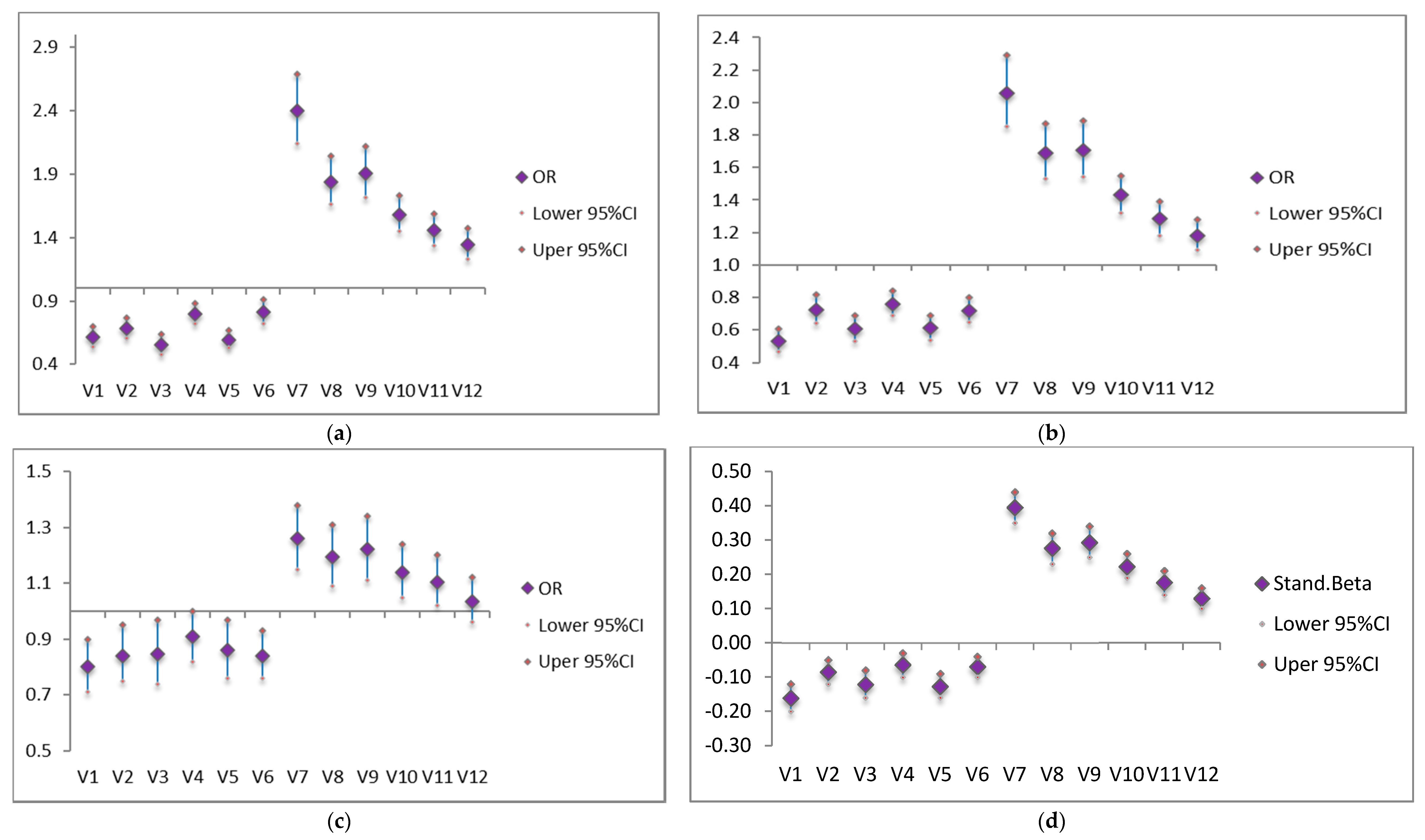
3.1. Predicting Mental Health Problems
3.2. Predicting PTSS, Depression and Insomnia
3.3. Coping Behaviors and Mental Health Problems
4. Discussion
Implications and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pfefferbaum, B.; North, C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Hugh, P.; Irene, T.; Simon, W.; Louise, A.; Clive, B.; Helen, C.; Roxane, C.S.; Ian, E.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet. Psychiat 2020. [Google Scholar] [CrossRef]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R. Coping as a Mediator of Emotion. J. Pers. Soc. Psychol. 1988, 54, 466–475. [Google Scholar] [CrossRef]
- Marshall, H.; Ryan, P.; Roberton, D.; Street, J.; Watson, M. Pandemic Influenza and Community Preparedness. Am. J. Public Health. 2009, 99, S365–S371. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.; Ho, R. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020, 17, 1729. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020, 52, 102066. [Google Scholar] [CrossRef]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020, 10, S30309. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med. Sci. Monit. 2020, 26, e923921. [Google Scholar] [CrossRef]
- Radloff, L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psych. Meas. 1997, 1, 385–401. [Google Scholar] [CrossRef]
- Cheng, S.T.; Chan, A.C.M. The Center for Epidemiologic Studies Depression Scale in older Chinese: Thresholds for long and short forms. Int. J. Geriatr. Psych. 2005, 20, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Chi, X.; Zhang, P.; Wu, H.; Jian, W. Screening for Postpartum Depression and Associated Factors Among Women in China: A Cross-Sectional Study. Front. Psychol. 2016, 7, 1688. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wu, Z.; Fang, G.; Li, J.; Han, B.; Chen, Z. Development of the Chinese age norms of CES-D in urban area. Chin. Ment. Health J. 2010, 24, 139–143. [Google Scholar]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM–5 (PCL-5). National Center for PTSD, 2013. Available online: www.ptsd.va.gov (accessed on 20 January 2020).
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.; Kupfer, D. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiat. Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Lu, T.Y.; Li, Y.; Xia, P. Analysis on reliability and validity of the pittsburgh sleep quality index. Chongqing Med. 2014, 3, 260–263. [Google Scholar]
- Jie, Y. Reliablility and validity of the Chinese version of coping style scale. Chin. J. Clin. Psychol. 1998, 2, 114–115. [Google Scholar]
- Lau, A.L.D.; Chi, I.; Cummins, R.A.; Lee, T.; Chou, K.; Chung, L. The SARS (Severe Acute Respiratory Syndrome) pandemic in Hong Kong: Effects on the subjective wellbeing of elderly and younger people. Aging Ment. Health 2008, 12, 746–760. [Google Scholar] [CrossRef]
- Mak, I.W.C.; Chu, C.M.; Pan, P.C.; Yiu, M.; Ho, S.; Chan, V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen. Hosp. Psychiat. 2010, 32, 590–598. [Google Scholar] [CrossRef]
- Blanc, J.; Rahill, G.; Spruill, T.M.; Jean-Louis, G.; Mouchenik, Y. Association between prenatal exposure to the Haiti 2010 earthquake, consequent maternal PTSD and autistic symptoms in offspring. Eur. J. Trauma Dissociation 2020, 4, 100098. [Google Scholar] [CrossRef]
- Gargano, L.M.; Welch, A.E.; Stellman, S.D. Substance use in adolescents 10 years after the World Trade Center attacks in New York City. J. Child Adolesc. Subst. Abus. 2017, 26, 66–74. [Google Scholar] [CrossRef]
- Polimanti, R.; Carvalho, C.M.; Wendt, F.; Belangero, S.; Nievergelt, C.; Koenen, K.; Gelernter, J. Causal inference using different phenotypic traits related to trauma exposure, trauma response, and posttraumatic stress disorder. Eur. Neuropaycho Pharmacol. 2019, 29, S42–S43. [Google Scholar]
- Topor, A.; Ljungqvist, I. Money, Social Relationships and the Sense of Self: The Consequences of an Improved Financial Situation for Persons Suffering from Serious Mental Illness. Community Ment. Health J. 2017, 53, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Snyder, C.M.; Fauth, E.; Wanzek, J.; Piecy, K.; Norton, M.; Corcoran, C.; Rabins, P.; Lyketsos, C.; Tschanz, J. Dementia caregivers’ coping strategies and their relationship to health and well-being: The Cache County Study. Aging Ment. Health. 2015, 19, 390–399. [Google Scholar] [PubMed]
- Lazarus, R.S. Hope: An emotion and a vital coping resource against despair. Soc. Res. 1999, 66, 653–678. [Google Scholar]
- Qian, M.; Ye, D.; Zhong, J.; Xu, K.; Zhang, L.; Huang, Z.; Dong, W.; Liu, X.; Zhang, X.; Zhang, Z. Behavioural, cognitive and emotional responses to SARS: Differences between college students in Beijing and Suzhou. Stress Health 2005, 21, 87–98. [Google Scholar] [CrossRef]
- Tan, W.; Hao, F.; McIntyre, R.S.; Jiang, L.; Jiang, X.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; Luo, X.; et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Tyler, C. How the Covid-19 Recession Is Like World War II? Bloomberg Opinion. 2020. Available online: https://www.bloomberg.com/opinion/articles/2020-03-24/coronavirus-recession-it-will-be-a-lot-like-world-war-ii (accessed on 20 January 2020).
- Troyer, E.A.; Kohn, J.N.; Hong, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Liu, J.J.W.; Ein, N.; Gervasio, J.; Vickers, K. The efficacy of stress reappraisal interventions on stress responsivity: A metaanalysis and systematic review of existing evidence. PLoS ONE 2019, 14, e0212854. [Google Scholar]
- Hofmann, S.G.; Asnaani, A.; Vonk, I.J.J.; Sawyer, A.T.; Fang, A. The Efficacy of Cognitive Behavioral Therapy: A Review of Metaanalyses. Cogn. Ther. Res. 2012, 36, 427–440. [Google Scholar] [CrossRef]
- Dickerson, S.S.; Kemeny, M.E. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol. Bull. 2004, 130, 355–391. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020. [Google Scholar] [CrossRef]
| Characteristics | Within Wuhan | Sub-Wuhan | Outside Wuhan | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Gender | Male | 87 | 41.4 | 88 | 46.8 | 987 | 48.3 | 1162 | 47.6 |
| Female | 123 | 58.6 | 100 | 53.2 | 1056 | 51.7 | 1279 | 52.4 | |
| Age | 18–25 | 10 | 4.8 | 16 | 8.5 | 278 | 13.6 | 304 | 12.5 |
| 26–30 | 51 | 24.3 | 23 | 12.2 | 539 | 26.4 | 613 | 25.1 | |
| 31–40 | 69 | 32.9 | 73 | 38.8 | 747 | 36.6 | 889 | 36.4 | |
| 41–50 | 46 | 21.9 | 45 | 23.9 | 307 | 15.0 | 398 | 16.3 | |
| ≥51 | 33 | 15.7 | 31 | 16.5 | 166 | 8.1 | 230 | 9.4 | |
| Missing | 1 | 0.48 | 0 | 0 | 6 | 0.3 | 7 | 0.3 | |
| Education | Middle school and below | 40 | 19.1 | 62 | 32.9 | 168 | 8.2 | 270 | 11.1 |
| High school | 25 | 11.9 | 47 | 25.0 | 294 | 14.4 | 366 | 14.9 | |
| Secondary | 21 | 10.0 | 28 | 14.9 | 404 | 19.8 | 453 | 18.6 | |
| Undergraduate | 82 | 39.1 | 42 | 22.3 | 922 | 45.1 | 1046 | 42.9 | |
| Graduate and above | 42 | 20.0 | 9 | 4.8 | 255 | 12.5 | 306 | 12.5 | |
| Married | No | 52 | 24.8 | 39 | 20.7 | 634 | 31.1 | 725 | 29.7 |
| Yes | 158 | 75.2 | 149 | 79.3 | 1409 | 68.9 | 1716 | 70.3 | |
| Income | Poor | 21 | 10.0 | 23 | 12.2 | 218 | 10.7 | 262 | 10.7 |
| Middle and High | 189 | 90.0 | 165 | 87.8 | 1825 | 89.3 | 2179 | 89.3 | |
| Job | Formal sector | 93 | 44.3 | 38 | 20.2 | 812 | 39.8 | 943 | 38.6 |
| Informal sector | 117 | 55.7 | 150 | 79.8 | 1231 | 60.3 | 1498 | 61.4 | |
| Priormental health problems | No | 177 | 84.3 | 172 | 91.5 | 1752 | 85.8 | 2101 | 86.1 |
| Yes | 33 | 15.7 | 16 | 8.5 | 291 | 14.2 | 340 | 13.9 | |
| Two-week disease | Yes | 20 | 9.5 | 10 | 5.3 | 126 | 6.2 | 156 | 6.4 |
| No | 190 | 90.5 | 178 | 94.7 | 1917 | 93.8 | 2285 | 93.6 | |
| Prior exposure | Yes | 19 | 9.1 | 7 | 3.7 | 165 | 8.1 | 191 | 7.8 |
| No | 191 | 90.9 | 181 | 96.3 | 1878 | 91.9 | 2250 | 92.2 | |
| Direct exposure | Yes | 86 | 40.9 | 108 | 57.5 | 384 | 18.8 | 588 | 24.1 |
| No | 124 | 59.1 | 80 | 42.5 | 1659 | 81.2 | 1853 | 75.9 | |
| Media exposure | Very frequent | 120 | 57.1 | 87 | 46.3 | 1196 | 58.5 | 1403 | 57.5 |
| Often | 59 | 28.1 | 56 | 29.8 | 512 | 25.1 | 627 | 25.7 | |
| Some | 14 | 6.7 | 26 | 13.8 | 165 | 8.1 | 205 | 8.4 | |
| Almost none | 17 | 8.1 | 19 | 10.1 | 170 | 8.3 | 206 | 8.4 | |
| Perceived impact on livelihood | None | 56 | 26.7 | 48 | 25.5 | 600 | 29.4 | 704 | 28.8 |
| Some | 63 | 30.0 | 69 | 36.7 | 698 | 34.2 | 830 | 34.0 | |
| Relatively large | 43 | 20.5 | 33 | 17.6 | 437 | 21.4 | 513 | 21.0 | |
| Very large | 48 | 22.9 | 38 | 20.2 | 308 | 15.1 | 394 | 16.1 | |
| PTSS | Yes | 173 | 82.4 | 170 | 90.4 | 1601 | 78.4 | 1944 | 79.6 |
| No | 37 | 17.6 | 18 | 9.6 | 442 | 21.6 | 497 | 20.4 | |
| Depression | Yes | 150 | 71.4 | 158 | 84.0 | 1465 | 71.7 | 1773 | 72.6 |
| No | 60 | 28.6 | 30 | 16.0 | 578 | 28.3 | 668 | 27.4 | |
| Insomnia | Yes | 53 | 25.2 | 34 | 18.1 | 415 | 20.3 | 502 | 20.6 |
| No | 157 | 74.8 | 154 | 81.9 | 1628 | 79.7 | 1939 | 79.4 | |
| Coping style | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Emotion-focused coping | 9.9 | 4.7 | 8.3 | 4.8 | 9.3 | 5.4 | 9.3 | 5.3 | |
| Problem-focused coping | 20.8 | 7.2 | 19.7 | 8.1 | 20 | 8.7 | 20.0 | 8.5 | |
| Independent Variables | Stand.beta | 95% CI | Stand.beta | 95% CI | Stand.beta | 95% CI | Stand.beta | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Model 0 | Model 1 | Model 2 | Model 3 | |||||
| Location | ||||||||
| Wuhan (reference) | ||||||||
| Sub-Wuhan | −0.08 | −0.13–−0.04 *** | −0.07 | −0.12–−0.03 *** | −0.06 | −0.11–−0.02 ** | −0.04 | −0.08–0.00 |
| Outside Wuhan | −0.03 | −0.08–0.02 | 0.00 | −0.05–0.05 | 0.02 | −0.04–0.07 | 0.01 | −0.03–0.06 |
| Media exposure | ||||||||
| Very frequent (reference) | ||||||||
| Often | −0.09 | −0.13–−0.05 *** | −0.09 | −0.12–−0.05 *** | −0.07 | −0.11–−0.03 *** | −0.05 | −0.09–−0.02 ** |
| Some | −0.03 | −0.07–0.01 | −0.03 | −0.07–0.01 | −0.03 | −0.06–0.01 | −0.02 | −0.05–0.01 |
| Almost none | −0.07 | −0.11–−0.04 *** | −0.07 | −0.11–−0.04 *** | −0.07 | −0.10–−0.03 *** | −0.07 | −0.10–−0.03 *** |
| Direct exposure | ||||||||
| No (reference) | ||||||||
| Yes | 0.07 | 0.04–0.11 *** | 0.09 | 0.05–0.13 *** | 0.08 | 0.04–0.12 *** | 0.05 | 0.02–0.09 ** |
| Perceived impact on livelihood | ||||||||
| None (reference) | ||||||||
| Some | 0.07 | 0.03–0.11 *** | 0.08 | 0.04–0.11 *** | 0.05 | 0.02–0.09 ** | ||
| Relatively large | 0.18 | 0.14–0.23 *** | 0.18 | 0.14–0.22 *** | 0.14 | 0.11–0.18 *** | ||
| Very large | 0.21 | 0.16–0.26 *** | 0.21 | 0.16–0.25 *** | 0.15 | 0.10–0.19 *** | ||
| Coping | ||||||||
| Problem-focused | −0.31 | −0.34–−0.27 *** | −0.30 | −0.34–−0.27 *** | ||||
| Emotion-focused | 0.50 | 0.46–0.55 *** | 0.47 | 0.42–0.51 *** | ||||
| Independent Variables | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Model 0 | Model 1 | Model 2 | Model 3 | |||||
| Location | ||||||||
| Within Wuhan (reference) | ||||||||
| Sub-Wuhan | 0.42 | 0.23–0.77 ** | 0.44 | 0.24–0.81 ** | 0.47 | 0.26–0.86 | 0.54 | 0.28–1.05 |
| Outside Wuhan | 1.12 | 0.76–1.65 | 1.27 | 0.85–1.89 | 1.38 | 0.92–2.06 | 1.43 | 0.91–2.23 |
| Media exposure | ||||||||
| Very frequent (reference) | ||||||||
| Often | 0.71 | 0.55–0.91 ** | 0.71 | 0.55–0.92 ** | 0.75 | 0.58–0.97 | 0.78 | 0.59–1.02 |
| Some | 0.83 | 0.56–1.23 | 0.85 | 0.58–1.26 | 0.82 | 0.55–1.23 | 0.86 | 0.57–1.31 |
| Almost none | 0.69 | 0.46–1.04 | 0.69 | 0.45–1.04 | 0.70 | 0.46–1.07 | 0.68 | 0.44–1.06 |
| Direct exposure | ||||||||
| No (reference) | ||||||||
| Yes | 1.20 | 0.95–1.52 | 1.36 | 1.06–1.75 * | 1.37 | 1.05–1.77 * | 1.21 | 0.92–1.60 |
| Perceived impact on livelihood | ||||||||
| None (reference) | ||||||||
| Some | 1.50 | 1.10–2.04 ** | 1.53 | 1.12–2.08 *** | 1.49 | 1.07–2.07 | ||
| Relatively large | 3.09 | 2.25–4.23 *** | 3.09 | 2.25–4.24 *** | 2.95 | 2.11–4.13 *** | ||
| Very large | 2.68 | 1.91–3.76 *** | 2.67 | 1.89–3.76 *** | 2.00 | 1.37–2.93 *** | ||
| Coping | ||||||||
| Problem-focused | 0.91 | 0.89–0.93 *** | 0.91 | 0.89–0.93 *** | ||||
| Emotion-focused | 1.24 | 1.20–1.28 *** | 1.23 | 1.19–1.28 *** | ||||
| Independent Variables | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Model 0 | Model 1 | Model 2 | Model 3 | |||||
| Location | ||||||||
| Within Wuhan (reference) | ||||||||
| Sub-Wuhan | 0.42 | 0.25–0.69 *** | 0.43 | 0.26–0.71 ** | 0.46 | 0.27–0.75 ** | 0.50 | 0.28–0.87 * |
| Outside Wuhan | 0.87 | 0.62–1.21 | 1.03 | 0.73–1.45 | 1.10 | 0.78–1.55 | 1.04 | 0.70–1.53 |
| Media exposure | ||||||||
| Very frequent (reference) | ||||||||
| Often | 0.81 | 0.65–1.02 | 0.82 | 0.65–1.03 | 0.86 | 0.68–1.08 | 0.90 | 0.70–1.16 |
| Some | 1.16 | 0.83–1.63 | 1.19 | 0.85–1.68 | 1.18 | 0.83–1.66 | 1.27 | 0.86–1.87 |
| Almost none | 0.80 | 0.56–1.16 | 0.80 | 0.55–1.15 | 0.83 | 0.57–1.20 | 0.79 | 0.53–1.18 |
| Direct exposure | ||||||||
| No (reference) | ||||||||
| Yes | 1.42 | 1.14–1.76 ** | 1.54 | 1.23–1.93 *** | 1.54 | 1.22–1.94 *** | 1.39 | 1.08–1.80 * |
| Perceived impact on livelihood | ||||||||
| None (reference) | ||||||||
| Some | 1.30 | 1.00–1.69 * | 1.32 | 1.01–1.72 * | 1.25 | 0.94–1.67 | ||
| Relatively large | 2.50 | 1.88–3.31 *** | 2.46 | 1.86–3.27 *** | 2.39 | 1.75–3.26 *** | ||
| Very large | 2.22 | 1.65–3.00 *** | 2.21 | 1.63–2.99 *** | 1.69 | 1.20–2.37 ** | ||
| Coping | ||||||||
| Positive | 0.87 | 0.85–0.89 *** | 0.87 | 0.85–0.89 *** | ||||
| Negative | 1.30 | 1.25–1.34 *** | 1.29 | 1.25–1.34 *** | ||||
| Independent Variables | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Model 0 | Model 1 | Model 2 | Model 3 | |||||
| Location | ||||||||
| Within Wuhan (reference) | ||||||||
| Sub-Wuhan | 0.62 | 0.38–1.02 | 0.67 | 0.40–1.11 | 0.69 | 0.42–1.15 | 0.78 | 0.46–1.33 |
| Outside Wuhan | 0.73 | 0.52–1.02 | 0.95 | 0.66–1.36 | 0.99 | 0.68–1.42 | 0.98 | 0.67–1.44 |
| Media exposure | ||||||||
| Very frequent (reference) | ||||||||
| Often | 0.78 | 0.61–1.00 | 0.78 | 0.61–1.01 | 0.81 | 0.63–1.04 | 0.84 | 0.65–1.09 |
| Some | 0.84 | 0.57–1.23 | 0.84 | 0.57–1.23 | 0.84 | 0.57–1.24 | 0.87 | 0.58–1.30 |
| Almost none | 0.77 | 0.51–1.15 | 0.76 | 0.50–1.13 | 0.77 | 0.51–1.15 | 0.78 | 0.51–1.17 |
| Direct exposure | ||||||||
| No (reference) | ||||||||
| Yes | 1.79 | 1.42–2.25 *** | 1.84 | 1.44–2.35 *** | 1.84 | 1.44–2.35 *** | 1.70 | 1.33–2.19 *** |
| Perceived impact on livelihood | ||||||||
| None (reference) | ||||||||
| Some | 1.05 | 0.80–1.38 | 1.06 | 0.81–1.40 | 1.01 | 0.77–1.34 | ||
| Relatively large | 1.45 | 1.08–1.96 * | 1.44 | 1.07–1.95 * | 1.32 | 0.98–1.79 | ||
| Very large | 1.60 | 1.16–2.20 ** | 1.55 | 1.12–2.14 ** | 1.25 | 0.89–1.75 | ||
| Coping | ||||||||
| Problem-focused | 0.95 | 0.94–0.96 *** | 0.95 | 0.94–0.97 *** | ||||
| Emotion-focused | 1.13 | 1.10–1.16 *** | 1.12 | 1.10–1.15 *** | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, J.; Feng, X.L.; Wang, X.H.; van IJzendoorn, M.H. Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 3857. https://doi.org/10.3390/ijerph17113857
Guo J, Feng XL, Wang XH, van IJzendoorn MH. Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults. International Journal of Environmental Research and Public Health. 2020; 17(11):3857. https://doi.org/10.3390/ijerph17113857
Chicago/Turabian StyleGuo, Jing, Xing Lin Feng, Xiao Hua Wang, and Marinus H. van IJzendoorn. 2020. "Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults" International Journal of Environmental Research and Public Health 17, no. 11: 3857. https://doi.org/10.3390/ijerph17113857
APA StyleGuo, J., Feng, X. L., Wang, X. H., & van IJzendoorn, M. H. (2020). Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults. International Journal of Environmental Research and Public Health, 17(11), 3857. https://doi.org/10.3390/ijerph17113857





