The Urban-Rural Disparity in the Status and Risk Factors of Health Literacy: A Cross-Sectional Survey in Central China
Abstract
1. Introduction
2. Materials and Methods
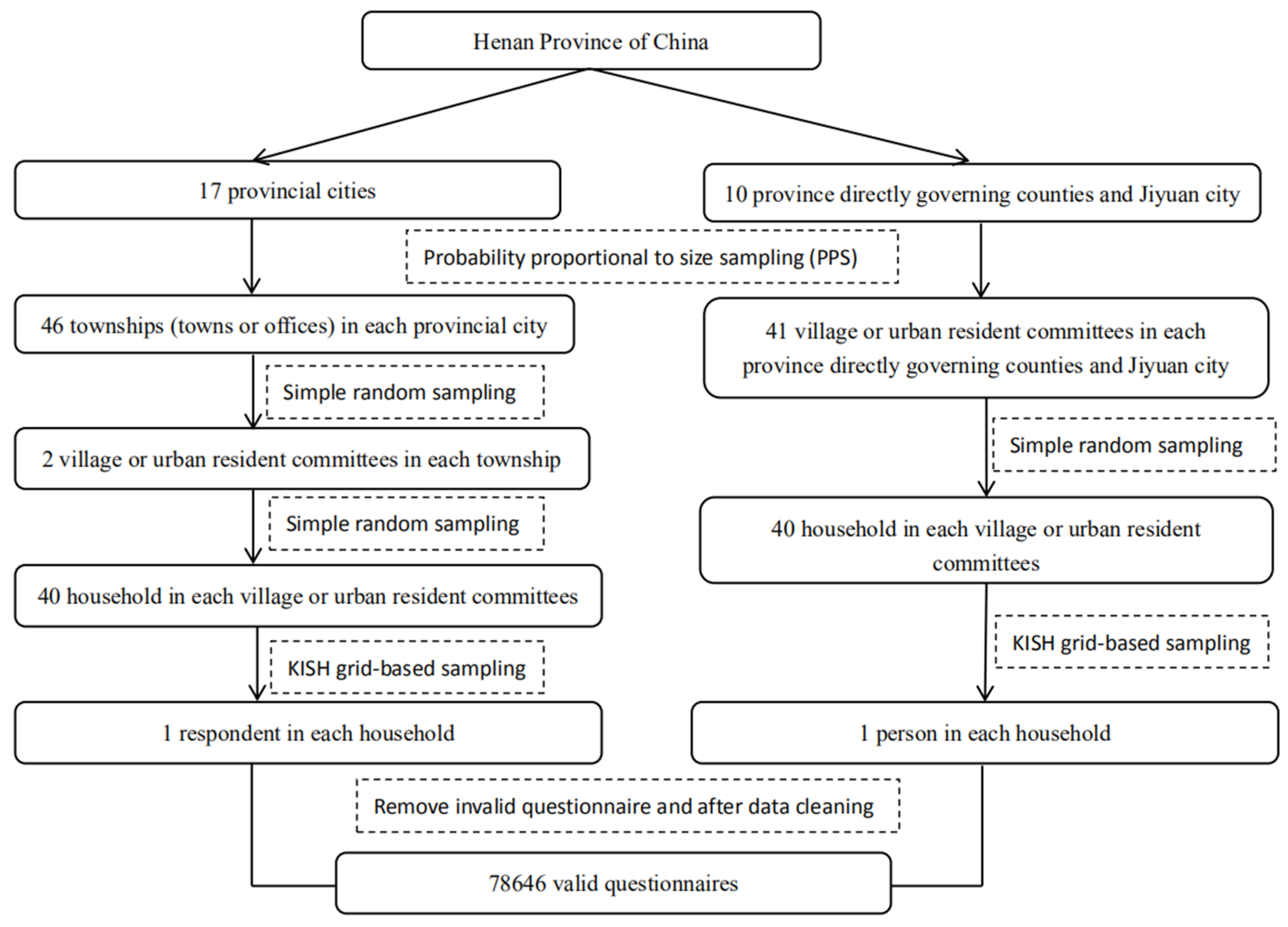
2.1. Study Population and Sampling Design
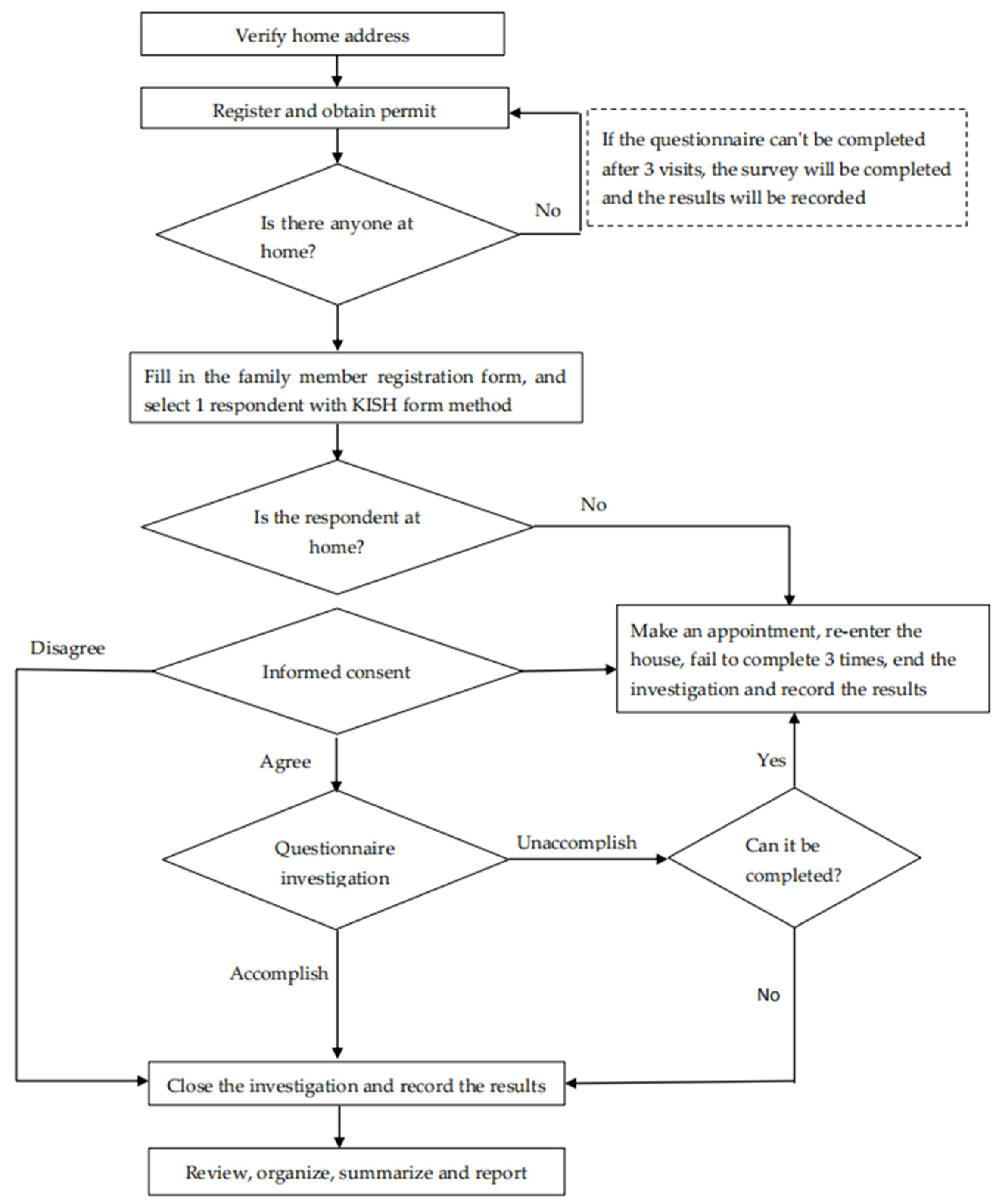
2.2. Measures and Data Collection
2.3. Statistical Analysis
3. Results
3.1. Population Characteristics and Health Literacy Status
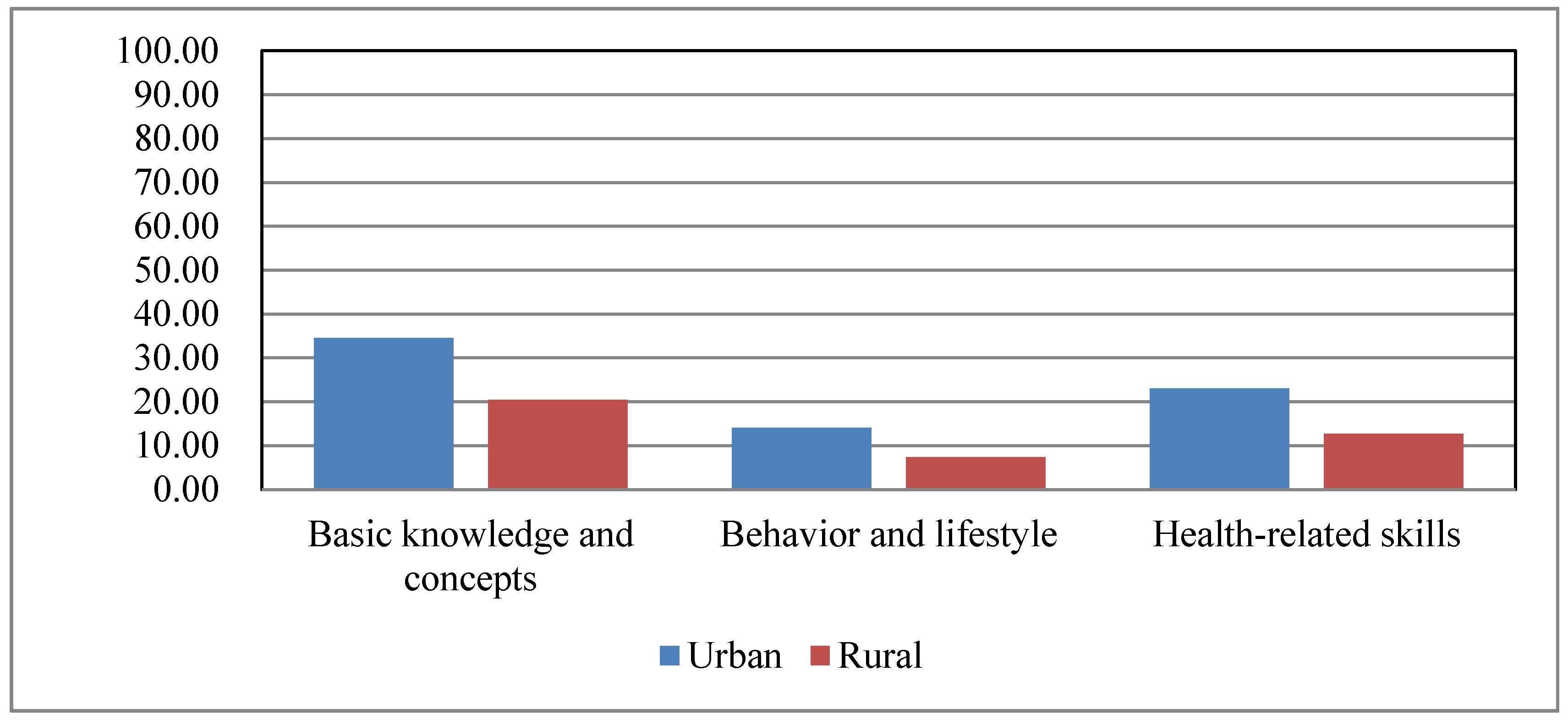
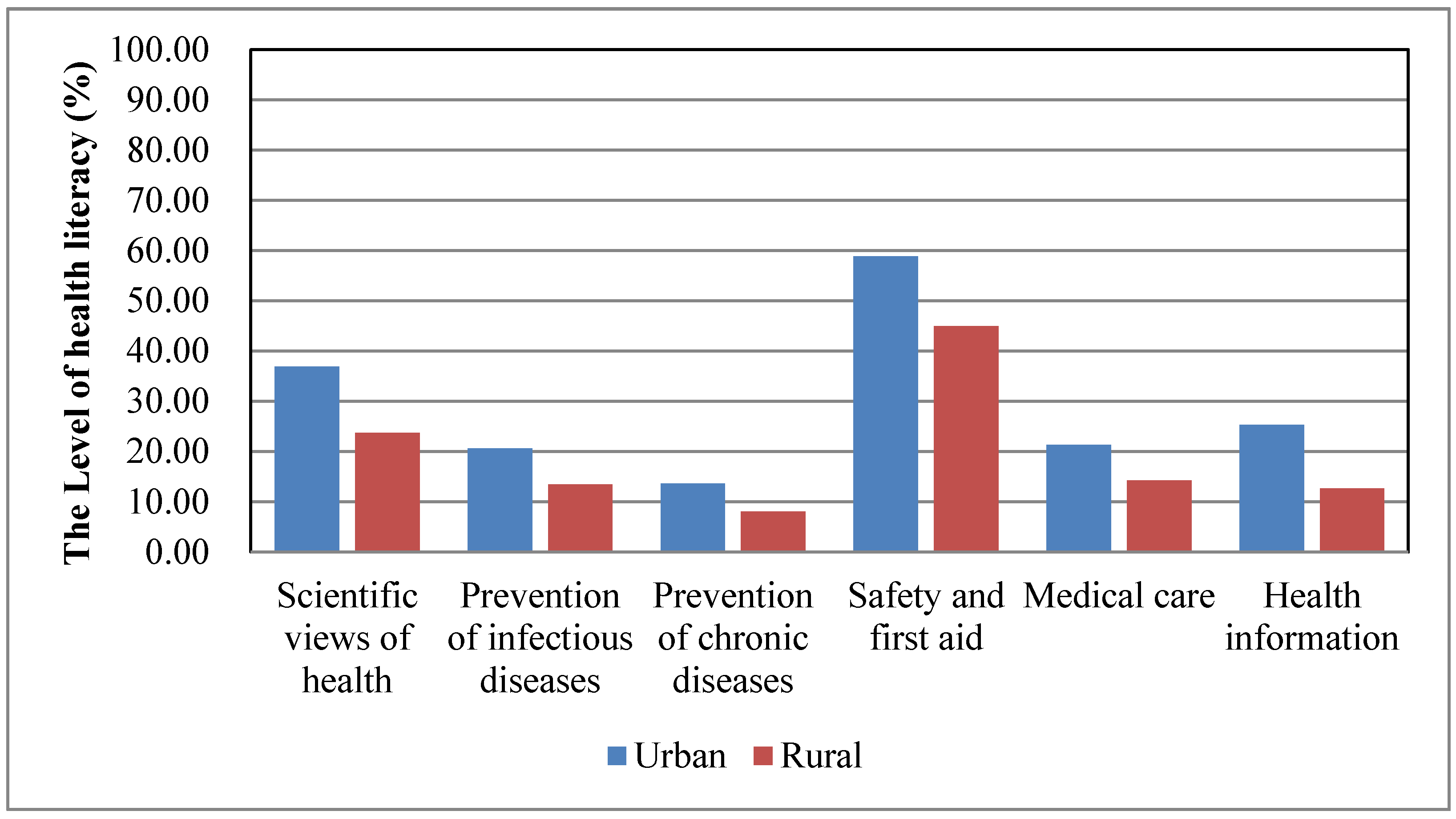
3.2. The Urban–Rural Disparity in Different Aspects and Health Issues of Health Literacy
3.3. The Urban–Rural Disparity of Risk Factors Associated with Health Literacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sorensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Katz, A. Health Literacy: What Do You Know? Oncol. Nurs. Forum. 2017, 44, 521–522. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.; Royne, M.B. The Impact of Consumers’ Health Literacy on Public Health. J. Consum. Aff. 2009, 43, 367–372. [Google Scholar] [CrossRef]
- Aaby, A.; Friis, K.; Christensen, B.; Rowlands, G.; Maindal, H.T. Health literacy is associated with health behaviour and self-reported health: A large population-based study in individuals with cardiovascular disease. Eur. J. Prev. Cardiol. 2017, 24, 1880–1888. [Google Scholar] [CrossRef] [PubMed]
- Rudolf, K.; Biallas, B.; Dejonghe, L.A.L.; Grieben, C.; Rückel, L.-M.; Schaller, A.; Stassen, G.; Pfaff, H.; Froböse, I. Influence of Health Literacy on the Physical Activity of Working Adults: A Cross-Sectional Analysis of the TRISEARCH Trial. Int. J. Environ. Res. Public Health 2019, 16, 4948. [Google Scholar] [CrossRef] [PubMed]
- Bostock, S.; Steptoe, A. Association between low functional health literacy and mortality in older adults: Longitudinal cohort study. BMJ 2012, 344, e1602. [Google Scholar] [CrossRef]
- Nelson, J.C.; Schwartzberg, J.G.; Vergara, K.C. The public’s and the patient’s right to know: AMA commentary on “Public health literacy in America: An ethical imperative”. Am. J. Prev. Med. 2005, 28, 325–326. [Google Scholar] [CrossRef]
- Xie, Y.; Ma, M.; Zhang, Y.N.; Tan, X.D. Factors associated with health literacy in rural areas of Central China: Structural equation model. BMC Health Serv. Res. 2019, 19, 300. [Google Scholar] [CrossRef]
- Berens, E.M.; Vogt, D.; Messer, M.; Hurrelmann, K.; Schaeffer, D. Health literacy among different age groups in Germany: Results of a cross-sectional survey. BMC Public Health 2016, 16, 1151. [Google Scholar] [CrossRef]
- National Bureau of Statistics. Communique of the National Bureau of Statistics of People’s Republic of China on Major Figures of the 2010 Population Census (No. 1). Available online: http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm (accessed on 1 March 2020).
- Wu, Y.; Wang, L.; Cai, Z.; Bao, L.; Ai, P.; Ai, Z. Prevalence and Risk Factors of Low Health Literacy: A Community-Based Study in Shanghai, China. Int. J. Environ. Res. Public Health 2017, 14, 628. [Google Scholar] [CrossRef]
- Ministry of Health of the People’s Republic of China. Report on the First Chinese Residents Health Literacy Monitoring Program. Available online: http://www.nhc.gov.cn/tigs/s9665/201208/a4149c8844854124b8c038521b1b5fe0.shtml (accessed on 1 March 2020).
- LI, Y.H.; NIE, X.Q. Contrast analysis of 2008 and 2012 Chinese health literacy survey scheme. Chin. J. Health Educ. 2014, 2, 176–177. [Google Scholar]
- World Health Organization. Shanghai Declaration on Promoting Health in the 2030 Agenda for Sustainable Development 2016. Available online: https://www.who.int/healthpromotion/conferences/9gchp/shanghaideclaration/en/ (accessed on 3 March 2020).
- Song, H.; Feng, D.; Wang, R.; Yang, J.; Li, Y.; Gao, J.; Wang, Z.; Yan, Z.; Long, C.; Zhou, J.; et al. The urban-rural disparity in the prevalence and risk factors of hypertension among the elderly in China-a cross-sectional study. Peer J. 2019, 7, e8015. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Guo, H.; Wang, L.; Li, X.; Huang, M.; Liu, Z.; Liu, X.; K, W.; Alamian, A.; Anderson, J.L. Investigation of residents’ health literacy status and its risk factors in Jiangsu Province of China. Asia Pac. J. Public Health 2015, 27, 2764–2772. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.R.; Yu, F.; He, L. A Study on the Current Status and Influential Factors of Urban and Rural Residents in Hebei Province in 2016. Chin. J. Health Educ. 2019, 35, 977–982. [Google Scholar]
- Voss, P.; Kornadt, A.E.; Hess, T.M.; Fung, H.H.; Rothermund, K. A world of difference? Domain-specific views on aging in China, the US, and Germany. Psychol. Aging 2018, 33, 595–606. [Google Scholar] [CrossRef]
- Li, F.; Otani, J. Financing elderly people’s long-term care needs: Evidence from China. Int. J. Health Plan. Manag. 2018, 33, 479–488. [Google Scholar] [CrossRef]
- Henan Province Bureau of Statistics. 2017 Statistical Bulletin of National Economic and Social Development of Henan Province. Available online: http://www.ha.stats.gov.cn/sitesources/hntj/page_pc/tjfw/tjgb/qstjgb/articlead6e17ff1d804bd4ad2859d99f02d284.html (accessed on 3 March 2020).
- Zhang, Y.L.; Wang, W.W.; Yan, G.; Zhou, G. Analysis on status of health literacy among residents in Henan Province. Chin. J. Health Educ. 2014, 33, 675–680. [Google Scholar]
- Shen, M.; Hu, M.; Liu, S.; Chang, Y.; Sun, Z.Q. Assessment of the Chinese Resident Health Literacy Scale in a population-based sample in South China. BMC Public Health 2015, 15, 637. [Google Scholar] [CrossRef]
- The Central People’s Government of the People’s Republic of China. China Promotes the Level of Residents’ Health Literacy to 30% by 2030. Available online: http://www.gov.cn/zhengce/2019-07/16/content_5410313.htm (accessed on 3 March 2020).
- Tang, C.; Wu, X.; Chen, X.; Pan, B.; Yang, X. Examining income-related inequality in health literacy and health-information seeking among urban population in China. BMC Public Health 2019, 19, 221. [Google Scholar] [CrossRef]
- Ehmann, A.T.; Groene, O.; Rieger, M.A.; Siegel, A. The Relationship between Health Literacy, Quality of Life, and Subjective Health: Results of a Cross-Sectional Study in a Rural Region in Germany. Int. J. Environ. Res. Public Health 2020, 17, 1683. [Google Scholar] [CrossRef]
- Jeong, S.H.; Kim, H.K. Health literacy and barriers to health information seeking: A nationwide survey in South Korea. Patient Educ. Couns. 2016, 99, 1880–1887. [Google Scholar] [CrossRef] [PubMed]
- Paasche-Orlow, M.K.; Parker, R.M.; Gazmararian, J.A.; Nielsen-Bohlman, L.T.; Rudd, R.R. The Prevalence of Limited Health Literacy. J. Gen. Intern. Med. 2005, 20, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Golboni, F.; Nadrian, H.; Najafi, S.; Shirzadi, S.; Mahmoodi, H. Urban-rural differences in health literacy and its determinants in Iran: A community-based study. Aust. J. Rural. Health 2018, 26, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Orom, H.; Hay, J.L.; Waters, E.A.; Schofield, E.; Li, Y.; Kiviniemi, M.T. Differences in Rural and Urban Health Information Access and Use. J. Rural. Health 2019, 35, 405–417. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Mao, Q.; Shi, Q. The level of health literacy of Chinese residents in 2012: Surveillance results. Chin. Health Educ. 2015, 31, 99–103. [Google Scholar]
- World Health Organization, Regional Office for the Eastern Mediterranean. Health Education: Theoretical Concepts, Effective Strategies and Core Competencies: A Foundation Document to Guide Capacity Development of Health Educators. Available online: https://apps.who.int/iris/handle/10665/119953 (accessed on 23 May 2020).
- World Health Organization. Global Status Report on Non-communicable Diseases 2014. Available online: http://www.who.int/nmh/publica-tions/ncd-status-report-2014/en/.2014 (accessed on 3 March 2020).
- Liu, X.; Mao, Z.; Li, Y.; Wu, W.; Zhang, X.; Huo, W.; Yu, S.; Shen, L.; Li, L.; Tu, R.; et al. Cohort Profile: The Henan Rural Cohort: A prospective study of chronic non-communicable diseases. Int. J. Epidemiol. 2019, 48, 1756–1756j. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Ren, R.; Wang, Y.; Guo, Y.; Fang, J.; Wu, Z.D.; Liu, P.L.; Han, T.R. Fighting against the common enemy of COVID-19: A practice of building a community with a shared future for mankind. Infect. Dis. Poverty 2020, 9, 34. [Google Scholar] [CrossRef]
- Lake, M.A. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. (Lond.) 2020, 20, 124–127. [Google Scholar] [CrossRef]
- Huang, C.-H.; Talley, P.C.; Lin, C.-W.; Huang, R.-Y.; Liu, I.-T.; Chiang, I.-H.; Lu, I.-C.; Lai, Y.-C.; Kuo, K.-M. Factors associated with low health literacy among community-dwelling women in Taiwan. Women Health 2020, 60, 487–501. [Google Scholar] [CrossRef]
- Banihashemi, S.T.; Amir Khani, A.; Haghdoust, A. Health literacy and the influencing factors: A study in five provinces of Iran. Stud. Dev. Med. Educ. 2007, 4, 1–9. [Google Scholar]
| Variable | Category | n | % | Level of Health Literacy | χ2 | p | |
|---|---|---|---|---|---|---|---|
| Sample Rate | Weighted Rate | ||||||
| Region | Urban | 17,813 | 22.65 | 15.65 | 16.92 | ||
| Rural | 60,833 | 77.35 | 5.77 | 8.09 | |||
| 1826.324 | <0.001 | ||||||
| Sex | Male | 36,625 | 46.57 | 8.32 | 10.10 | ||
| Female | 42,021 | 53.43 | 7.94 | 10.31 | |||
| 3.800 | >0.05 | ||||||
| Age groups | 15–24 | 3594 | 4.57 | 11.30 | 11.39 | ||
| 25–34 | 10,303 | 13.10 | 14.11 | 14.88 | |||
| 35–44 | 13,527 | 17.20 | 11.67 | 12.01 | |||
| 45–54 | 24,396 | 31.02 | 6.51 | 6.81 | |||
| 55–64 | 18,254 | 23.21 | 5.17 | 5.34 | |||
| 65–69 | 8572 | 10.90 | 3.82 | 4.10 | |||
| 1298.920 | <0.001 | ||||||
| Education | Uneducated | 12,088 | 15.37 | 1.91 | 2.13 | ||
| Primary school | 18,254 | 23.21 | 3.60 | 4.16 | |||
| Junior middle school | 31,104 | 39.55 | 6.38 | 7.08 | |||
| High school or vocational school | 11,718 | 14.90 | 14.41 | 14.65 | |||
| Diploma or undergraduate | 5262 | 6.69 | 31.35 | 29.44 | |||
| Postgraduate and above | 220 | 0.28 | 36.41 | 38.40 | |||
| 5996.713 | <0.001 | ||||||
| Occupation | Civil servant | 645 | 0.82 | 22.14 | 20.71 | ||
| Teacher | 1510 | 1.92 | 24.20 | 23.46 | |||
| Medical staff | 1258 | 1.6 | 35.04 | 37.78 | |||
| Personnel of other government-sponsored institution | 2084 | 2.65 | 19.65 | 18.68 | |||
| Student | 1486 | 1.89 | 12.81 | 13.63 | |||
| Farmer | 57,191 | 72.72 | 4.65 | 5.83 | |||
| Worker | 6064 | 7.71 | 13.42 | 14.64 | |||
| Personnel of other enterprises | 3201 | 4.07 | 20.42 | 20.86 | |||
| Others | 5207 | 6.62 | 15.24 | 15.68 | |||
| 4434.476 | <0.001 | ||||||
| Total | 78,646 | 8.01 | 10.21 | ||||
| Risk Factor | Urban | Rural | |||
|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | ||
| Education | Uneducated | Reference | |||
| Primary school | 1.071 (0.780, 1.471) | 0.670 | 1.897 (1.625,2.215) | <0.001 | |
| Junior middle school | 1.537 (1.154, 2.048) | 0.003 | 3.164 (2.738, 3.656) | <0.001 | |
| High school or vocational school | 2.742 (2.051, 3.664) | <0.001 | 5.979 (5.136, 6.959) | <0.001 | |
| Diploma or undergraduate | 5.142 (3.816, 6.928) | <0.001 | 10.844 (9.185, 12.803) | <0.001 | |
| Postgraduate and above | 10.552 (6.738, 16.523) | <0.001 | 13.541 (9.749, 18.809) | <0.001 | |
| Occupation | Civil servant | Reference | |||
| Teacher | 1.449 (1.069, 1.964) | 0.017 | 1.233 (0.952, 1.595) | 0.112 | |
| Medical staff | 2.14 (1.553, 2.949) | <0.001 | 2.261 (1.734, 2.949) | <0.001 | |
| Personnel of other institutions | 1.209 (0.910, 1.606) | 0.190 | 1.112 (0.863, 1.433) | 0.412 | |
| Student | 1.116 (0.742, 1.679) | 0.597 | 0.949 (0.699, 1.289) | 0.738 | |
| Farmer | 0.676 (0.508, 0.899) | 0.007 | 0.672 (0.529, 0.853) | 0.001 | |
| Worker | 1.122 (0.851, 1.478) | 0.415 | 1.115 (0.873, 1.424) | 0.383 | |
| Other enterprise personnel | 1.218 (0.927, 1.600) | 0.157 | 1.246 (0.976, 1.591) | 0.077 | |
| Others | 1.076 (0.819, 1.415) | 0.598 | 1.176 (0.922, 1.500) | 0.191 | |
| Age groups | 15–24 | Reference | |||
| 25–34 | 1.422 (1.122, 1.803) | 0.004 | 1.224 (1.055, 1.421) | 0.008 | |
| 35–44 | 1.688 (1.335, 2.134) | <0.001 | 1.17 (1.010, 1.356) | 0.037 | |
| 45–54 | 1.332 (1.053, 1.686) | 0.017 | 0.846 (0.730, 0.981) | 0.027 | |
| 55–64 | 1.156 (0.903, 1.479) | 0.251 | 0.716 (0.614, 0.836) | <0.001 | |
| 65–69 | 1.293 (0.980, 1.707) | 0.070 | 0.679 (0.567, 0.812) | <0.001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, W.; Zhang, Y.; Lin, B.; Mei, Y.; Ping, Z.; Zhang, Z. The Urban-Rural Disparity in the Status and Risk Factors of Health Literacy: A Cross-Sectional Survey in Central China. Int. J. Environ. Res. Public Health 2020, 17, 3848. https://doi.org/10.3390/ijerph17113848
Wang W, Zhang Y, Lin B, Mei Y, Ping Z, Zhang Z. The Urban-Rural Disparity in the Status and Risk Factors of Health Literacy: A Cross-Sectional Survey in Central China. International Journal of Environmental Research and Public Health. 2020; 17(11):3848. https://doi.org/10.3390/ijerph17113848
Chicago/Turabian StyleWang, Wenna, Yulin Zhang, Beilei Lin, Yongxia Mei, Zhiguang Ping, and Zhenxiang Zhang. 2020. "The Urban-Rural Disparity in the Status and Risk Factors of Health Literacy: A Cross-Sectional Survey in Central China" International Journal of Environmental Research and Public Health 17, no. 11: 3848. https://doi.org/10.3390/ijerph17113848
APA StyleWang, W., Zhang, Y., Lin, B., Mei, Y., Ping, Z., & Zhang, Z. (2020). The Urban-Rural Disparity in the Status and Risk Factors of Health Literacy: A Cross-Sectional Survey in Central China. International Journal of Environmental Research and Public Health, 17(11), 3848. https://doi.org/10.3390/ijerph17113848




