Patient–Physician Interaction and Trust in Online Health Community: The Role of Perceived Usefulness of Health Information and Services
Abstract
1. Introduction
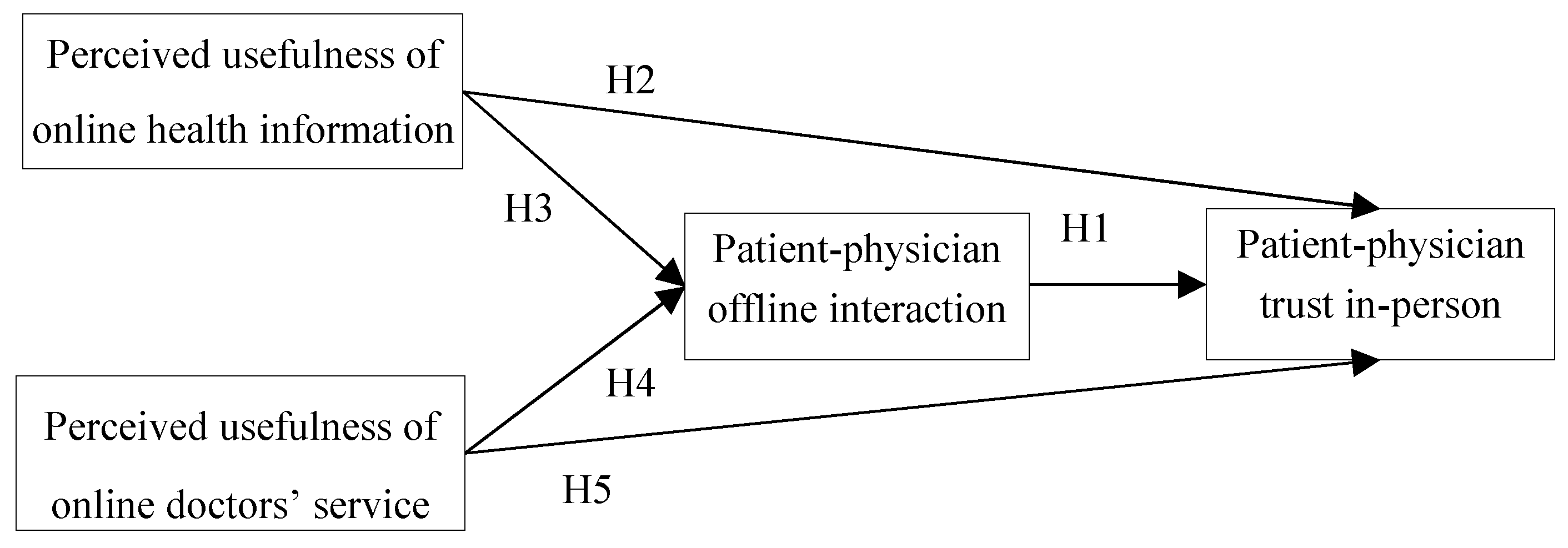
2. Hypothesis Development
2.1. Patient–Physician Interaction and Trust
2.2. Perceived Usefulness of Online Health Information
2.3. Perceived Usefulness of Online Doctors’ Service
3. Data Set and Variables
3.1. Participants and Data Collection
3.2. Measurement Instrument
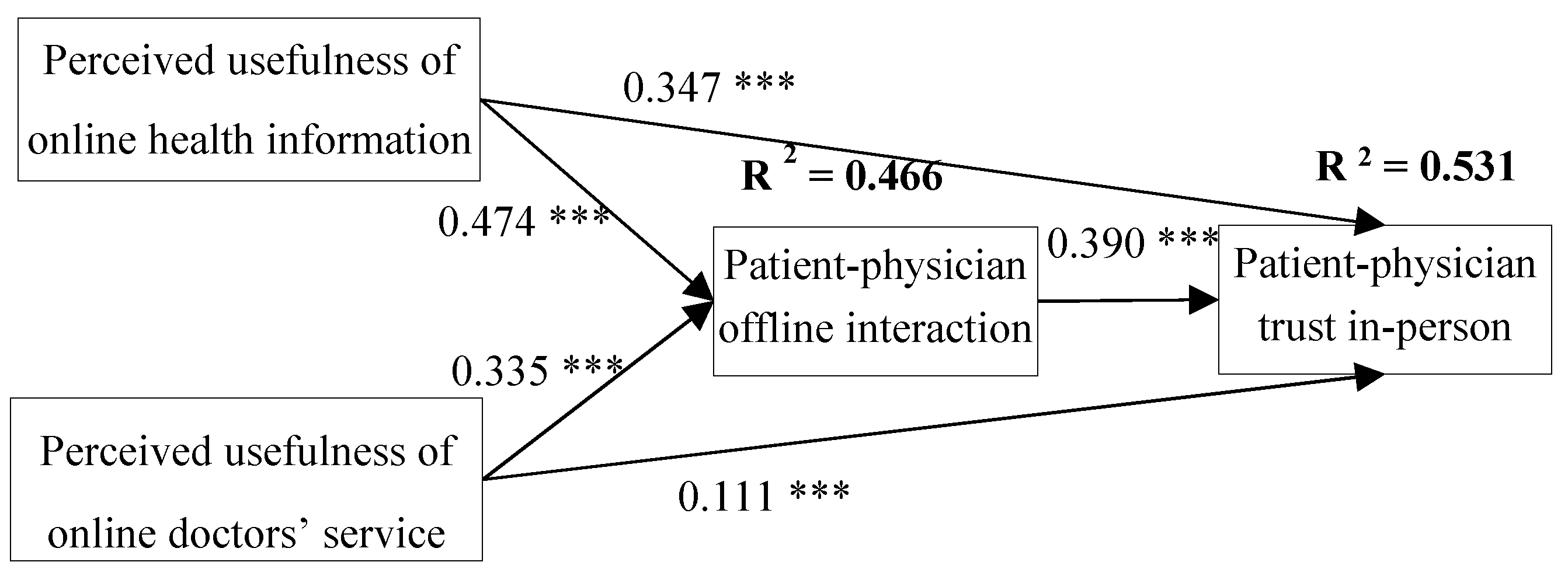
4. Results
5. Discussions
5.1. Implications
5.2. Limitation and Future Research
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- The 43nd “Statistical Report on the Development of Internet in China”. China Internet Network Information Center. 2018. Available online: http://www.cnnic.net.cn/hlwfzyj/hlwxzbg/hlwtjbg/201902/t20190228_70645.htm (accessed on 28 February 2019).
- The Fourth White Paper on the Health Status of Chinese Internet Users. China. 2007. Available online: http://www.docin.com/p-3620017.html (accessed on 5 January 2012).
- Rider, T.; Malik, M.; Chevassut, T. Haematology patients and the Internet—the use of on-line health information and the impact on the patient-doctor relationship. Patient Educ. Couns. 2014, 97, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Tanis, M.; Harrtmann, T.; Poel, F.T. Online health anxiety and consultation satisfaction: A quantitative exploratory study on their relations. Patient Educ. Couns. 2016, 99, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Iverson, S.A.; Howard, K.B.; Penney, B.K. Impact of internet use on health-related behaviors and the patient-physician relationship: A survey-based study and review. J. Am. Osteopath. Assoc. 2008, 108, 699–711. [Google Scholar] [PubMed]
- Tan, S.S.; Goonawardene, N. Internet Health Information Seeking and the Patient-Physician Relationship: A Systematic Review. J. Med Internet Res. 2017, 19, e9. [Google Scholar] [CrossRef] [PubMed]
- Hall, B.J.; Xiong, P.; Chang, K.; Yin, M.; Sui, X.-R. Prevalence of medical workplace violence and the shortage of secondary and tertiary interventions among healthcare workers in China. J. Epidemiol. Community Health 2018, 72, 516–518. [Google Scholar] [CrossRef]
- Morgan, M. Sociology as Applied to Medicine, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2008. [Google Scholar]
- Xu, Y.P.; He, W. More Information = Less Aggression? Impact of Information Asymmetry on Chinese Patients’ Aggression. Front. Public Health 2019, 7, 118. [Google Scholar] [CrossRef]
- Piette, J.D.; Heisler, M.; Krein, S.; Kerr, E.A. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch. Intern. Med. 2005, 165, 1749–1755. [Google Scholar] [CrossRef]
- Osei-Frimpong, K.; Nana, O.F. Value Co-Creation in Health Care: A Phenomenological Examination of the Doctor-Patient Encounter. J. Nonprofit Public Sect. Mark. 2017, 29, 365–384. [Google Scholar] [CrossRef]
- Osei-Frimpong, K.; Wilson, A.; Lemke, F. Patient co-creation activities in healthcare service delivery at the micro level: The influence of online access to healthcare information. Technol. Forecast. Soc. Chang. 2016, 126, 14–27. [Google Scholar] [CrossRef]
- Willard, S.; Cremers, G.; Man, Y.P.; Van Rossum, E.; Spreeuwenberg, M.; De Witte, L. Development and testing of an online community care platform for frail older adults in the Netherlands: A user-centred design. BMC Geriatr. 2018, 18, 1–87. [Google Scholar] [CrossRef]
- Oh, H.J.; Lee, B. The effect of computer-mediated social support in online communities on patient empowerment and doctor-patient communication. Health Commun. 2012, 27, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Broom, A. Virtually healthy: The impact of internet use on disease experience and the doctor-patient relationship. Qual. Health Res. 2005, 15, 325–345. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, K.M.; Moussa, N.A. Internet use by the public to search for health-related information. Int. J. Med. Inform. 2012, 81, 363–373. [Google Scholar] [CrossRef]
- Bianco, A.; Zucco, R.; Nobile, C.G.A.; Pileggi, C.; Pavia, M. Parents Seeking Health-Related Information on the Internet: Cross-Sectional Study. J. Med. Internet Res. 2013, 15, e204. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; Elhadad, M.; Birk, O. Analysis of free online physician advice services. PLoS ONE 2013, 8, e59963. [Google Scholar] [CrossRef]
- Gilmour J, A. Engaging With Patient Online Health Information Use: A Survey of Primary Health Care Nurses. Sage Open 2014, 4, 1–10. [Google Scholar] [CrossRef]
- Chan, S.-C.C. Mistrust of physicians in China: Society, institution, and interaction as root causes. Dev. World Bioeth. 2018, 18, 16–25. [Google Scholar] [CrossRef]
- Marsh, S.; Dibben, M.R. Trust, Untrust, Distrust and Mistrust—An Exploration of the Dark(er) Side. In International Conference on Trust Management; Springer: Berlin/Heidelberg, Germany, 2005; pp. 17–33. [Google Scholar]
- Nie, J.-B.; Tucker, J.D.; Zhu, W.; Cheng, Y.; Wong, B.; Kleinman, A. Rebuilding patient-physician trust in China, developing a trust-oriented bioethics. Dev. Trust. Oriented Bioeth. 2017, 18, 1, 4–6. [Google Scholar] [CrossRef]
- Akbolat, M.; Karakaya, F.; Ugan, C.; Durmug, A. the effect of trust communication in patient-physician relationship on satisfaction and compliance to treatment. Int. J. Health Med. Curr. Res. 2017, 2, 610–619. [Google Scholar]
- Ben-Sira, Z. The function of the professional’s affective behavior in client satisfaction: A revised approach to social interaction theory. J. Health Soc. Behav. 1976, 17, 3–11. [Google Scholar] [CrossRef]
- Onguti, S.; Mathew, S.; Todd, C. Communication and Ethics in the Clinical Examination. Med. Clin. North Am. 2018, 102, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Ponnapureddy, S.; Priskin, J.; Ohnmacht, T.; Vinzenz, F.; Wirth, W. The influence of trust perceptions on German tourists’ intention to book a sustainable hotel: A new approach to analysing marketing information. J. Sustain. Tour. 2017, 25, 1–19. [Google Scholar] [CrossRef]
- Ting, H.; Thaichon, P.; Chuah, F.; Tan, S.R. Consumer behaviour and disposition decisions: The why and how of smartphone disposition. J. Retail. Consum. Serv. 2019, 51, 212–220. [Google Scholar] [CrossRef]
- Shen, X.L.; Cheung, C.M.; Lee, M.K. What leads students to adopt information from Wikipedia? An empirical investigation into the role of trust and information usefulness. Br. J. Educ. Technol. 2013, 44, 3, 502–517. [Google Scholar] [CrossRef]
- Chakraborty, D. Adoption of M-Banking Service Apps for Rural Consumers: An Empirical Analysis. NMIMS Manag. Rev. 2019, 37, 34–52. [Google Scholar]
- Sussman, S.W.; Siegal, W.S. Informational Influence in Organizations: An Integrated Approach to Knowledge Adoption. Inf. Syst. Res. 2003, 14, 47–65. [Google Scholar] [CrossRef]
- Sullivan, Y.W.; Koh, C.E. Social media enablers and inhibitors: Understanding their relationships in a social networking site context. Int. J. Inf. Manag. 2019, 49, 170–189. [Google Scholar] [CrossRef]
- Gong, Z.; Han, Z.; Li, X.; Yu, C.; Jan, D.R. Factors Influencing the Adoption of Online Health Consultation Services: The Role of Subjective Norm, Trust, Perceived Benefit, and Offline Habit. Front. Public Health 2019, 7, 286. [Google Scholar] [CrossRef]
- Lu, T.; Chen, H.; Xu, Y.; Zhang, C. Internet Usage, Physician Performances and Patient’s Trust in Physician During Diagnoses: Investigating Both Pre-Use and Not-Use Internet Groups. In Proceedings of the 49th Hawaii International Conference on System Sciences, Koloa, HI, USA, 5–8 January 2016; pp. 3189–3198. [Google Scholar]
- Beirão, G.; Patrício, L.; Fisk, R.P. Value cocreation in service ecosystems. J. Serv. Manag. 2017, 28, 227–249. [Google Scholar] [CrossRef]
- Haluza, D.; Naszay, M.; Stockinger, A.; Jungwirth, D. Digital Natives versus Digital Immigrants: Influence of Online Health Information Seeking on the Doctor-Patient Relationship. Health Commun. 2017, 32, 11, 1342–1349. [Google Scholar] [CrossRef]
- Presti, L.L.; Testa, M.; Marino, V.; Singer, P. Engagement in Healthcare Systems: Adopting Digital Tools for a Sustainable Approach. Sustainability 2019, 11, 220. [Google Scholar] [CrossRef]
- Mou, J.; Cohen, J. Trust, Risk and Perceived Usefulness in Consumer Acceptance of Online Health Services. Arch. Pédiatrie 2014, 5, 851–860. [Google Scholar]
- Bhattacherjee, A.; Lin, C.P. A unified model of IT continuance: Three complementary perspectives and crossover effects. Eur. J. Inf. Syst. 2015, 24, 364–373. [Google Scholar] [CrossRef]
- Chang, Y.W.; Hsu, P.Y. Integration of online and offline health services: The role of doctor-patient online interaction. Patient Educ. Couns. 2019, 102, 1905–1910. [Google Scholar] [CrossRef]
- Deng, Z.; Liu, S. Understanding consumer health information-seeking behavior from the perspective of the risk perception attitude framework and social support in mobile social media websites. Int. J. Med. Inform. 2017, 105, 98–109. [Google Scholar] [CrossRef]
- Ford, S.; Fallowfield, L.; Lewis, S. Doctor-patient interactions in oncology. Soc. Sci. Med. 1996, 42, 1511–1519. [Google Scholar] [CrossRef]
- Wu, T.; Deng, Z.; Zhang, N.; Buchanan, P.R.; Zha, N.; Wang, R. Seeking and Using Intention of Health Information from Doctors in Social Media: The Effect of Doctor-Consumer Interaction. Int. J. Med. Inform. 2018, 115, 106–113. [Google Scholar] [CrossRef]
- Anderson, L.A.; Dedrick, R.F. Development of the Trust in Physician Scale: A measure to assess interpersonal trust in patient-physician relationships. Psychol. Rep. 1990, 67, 1091–1100. [Google Scholar] [CrossRef]
- Bendassolli, P.F. Theory Building in Qualitative Research: Reconsidering the Problem of Induction. Forum Qual. Soz. Forum Qual. Soc. Res. 2013, 14. [Google Scholar] [CrossRef]
- Damali, U.; Miller, J.L.; Fredendall, L.D.; Moore, D.; Dye, C.J. Co-creating value using customer training and education in a healthcare service design. J. Oper. Manag. 2016, 47, 80–97. [Google Scholar] [CrossRef]
- Gallan, A.S.; Jarvis, C.B.; Brown, S.W.; Bitner, M.J. Customer positivity and participation in services: An empirical test in a health care context. J. Acad. Mark. Sci. 2013, 41, 338–356. [Google Scholar] [CrossRef]
- McColl-Kennedy, J.R.; Vargo, S.L.; Dagger, T.S.; Sweeney, J.C.; Van Kasteren, Y. Health Care Customer Value Cocreation Practice Styles. J. Serv. Res. 2012, 15, 370–389. [Google Scholar] [CrossRef]
- McColl-Kennedy, J.R.; Hogan, S.J.; Witell, L.; Snyder, H. Cocreative customer practices: Effects of health care customer value cocreation practices on well-being. J. Bus. Res. 2016, 70, 55–66. [Google Scholar] [CrossRef]
- Hau, L.N.; Thuy, P.N. Customer participation to co-create value in human transformative services: A study of higher education and health care services. Serv. Bus. 2015, 10, 1–26. [Google Scholar]
- Osei-Frimpong, K. Patient participatory behaviours in healthcare service delivery. J. Serv. Theory Pract. 2017, 27, 453–474. [Google Scholar] [CrossRef]
- Hau, L.N.; Anh PN, T.; Thuy, P.N. The effects of interaction behaviors of service frontliners on customer participation in the value co-creation: A study of health care service. Serv. Bus. 2016, 11, 253–277. [Google Scholar] [CrossRef]
- Ramírez, A.S.; Freres, D.; Martinez, L.S.; Lewis, N.; Bourgoin, A.; Kelly, B.J.; Lee, C.-J.; Nagler, R.; Schwartz, J.S.; Hornik, R.C. Information Seeking From Mediaand Family/Friends Increases The Likelihood of Engaging in Healthy Lifestyle Behaviors. J. Health Commun. 2013, 18, 527–542. [Google Scholar] [CrossRef] [PubMed]
- Audratin-Pontevia, A.F.; Menvielle, L. Do Online Health Communities Enhance Patient–Physician Relationship? An Assessment of the Impact of Social Support and Patient Empowerment. Health Serv. Manag. Res. 2018, 31, 154–162. [Google Scholar] [CrossRef]
| Characteristics | Number | Percentage | |
|---|---|---|---|
| Gender | |||
| male | 222 | 49.5% | |
| female | 224 | 50.2% | |
| Age | |||
| ≤20 | 18 | 4.0% | |
| 20–30 | 288 | 64.6% | |
| ≥30 | 140 | 31.3% | |
| Self-reported health condition | |||
| poor | 304 | 68.2% | |
| good | 142 | 31.8% | |
| intensify health consciousness | |||
| very helpful | 110 | 24.7% | |
| helpful | 308 | 69.1% | |
| no help | 28 | 6.3% | |
| online health information seeking | |||
| before visit | 114 | 25.6% | |
| after visit | 67 | 15.0% | |
| both | 225 | 50.2% | |
| others | 40 | 9.0% | |
| source of health information | |||
| medical professional | 173 | 38.8% | |
| online information | 224 | 50.2% | |
| journal | 11 | 2.5% | |
| friends | 31 | 7.0% | |
| others | 7 | 1.6% | |
| Issues that should be improved | |||
| patient–physician communication | 174 | 39.0% | |
| patient–physician trust | 166 | 37.2% | |
| service attitude of medical professional | 98 | 22.0% | |
| others | 8 | 1.8% | |
| Potential Variables | Items | Questions | Source |
|---|---|---|---|
| Perceived usefulness of online health information | 1 | Online health information helps me validate doctors’ diagnosis | Tan S S et al. [6] |
| 2 | Online health information helps me realize my own health status | ||
| Perceived usefulness of online doctors’ service | 1 | I receive caring and helping from doctors on the online health community. | Iverson S A et al. [5]; Oh, HJ et al. [14] |
| 2 | Online doctors will offer me necessary information when I face disease-related problems. | ||
| Patient–physician interaction | 1 | Interacting with doctors makes me feel smooth. | Oh, HJ et al. [14]; Ford S et al. [41]; Wu T et al. [42] |
| 2 | I will try to get practical information from doctors for my disease management. | ||
| 3 | During my interaction with doctors, the doctors demonstrate sufficient devotion to the management of my problems. | ||
| 4 | When I find some information regarding my disease, I will bring them to my doctor. | ||
| Patient–physician trust | 1 | I trust the doctors so much I always try to follow his/her advice. | Anderson L A et al. [43] |
| 2 | My doctor is a real expert in taking care of medical problems like mine. | ||
| 3 | If my doctor tells me something is so, then it must be true. | ||
| 4 | I trust my doctor to put my medical needs above all other considerations when treating my medical problems. |
| Construct | Items | Factor Loadings | Composite Reliability | Average Variance Extracted | Cronbach’s Alphas |
|---|---|---|---|---|---|
| Patient–Physician Interaction | INT1 | 0.715 | 0.846 | 0.579 | 0.853 |
| INT2 | 0.735 | ||||
| INT3 | 0.772 | ||||
| INT4 | 0.818 | ||||
| Patient–Physician Trust | TRU1 | 0.772 | 0.8088 | 0.5153 | 0.844 |
| TRU2 | 0.758 | ||||
| TRU3 | 0.686 | ||||
| TRU4 | 0.648 | ||||
| perceived usefulness of online health information | UI1 | 0.773 | 0.6985 | 0.5357 | 0.688 |
| UI2 | 0.691 | ||||
| perceived usefulness of online doctors’ services | PH1 | 0.848 | 0.8326 | 0.7132 | 0.779 |
| PH2 | 0.841 |
| . | PUI | PUS | INT | TRU |
|---|---|---|---|---|
| PUI | 0.732 | |||
| PUS | 0.403 | 0.845 | ||
| INT | 0.610 | 0.526 | 0.761 | |
| TRU | 0.633 | 0.455 | 0.662 | 0.718 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, Y.; Yin, P.; Deng, Z.; Wang, R. Patient–Physician Interaction and Trust in Online Health Community: The Role of Perceived Usefulness of Health Information and Services. Int. J. Environ. Res. Public Health 2020, 17, 139. https://doi.org/10.3390/ijerph17010139
Peng Y, Yin P, Deng Z, Wang R. Patient–Physician Interaction and Trust in Online Health Community: The Role of Perceived Usefulness of Health Information and Services. International Journal of Environmental Research and Public Health. 2020; 17(1):139. https://doi.org/10.3390/ijerph17010139
Chicago/Turabian StylePeng, Yuxin, Pingping Yin, Zhaohua Deng, and Ruoxi Wang. 2020. "Patient–Physician Interaction and Trust in Online Health Community: The Role of Perceived Usefulness of Health Information and Services" International Journal of Environmental Research and Public Health 17, no. 1: 139. https://doi.org/10.3390/ijerph17010139
APA StylePeng, Y., Yin, P., Deng, Z., & Wang, R. (2020). Patient–Physician Interaction and Trust in Online Health Community: The Role of Perceived Usefulness of Health Information and Services. International Journal of Environmental Research and Public Health, 17(1), 139. https://doi.org/10.3390/ijerph17010139





