Weight Shame, Social Connection, and Depressive Symptoms in Late Adolescence
Abstract
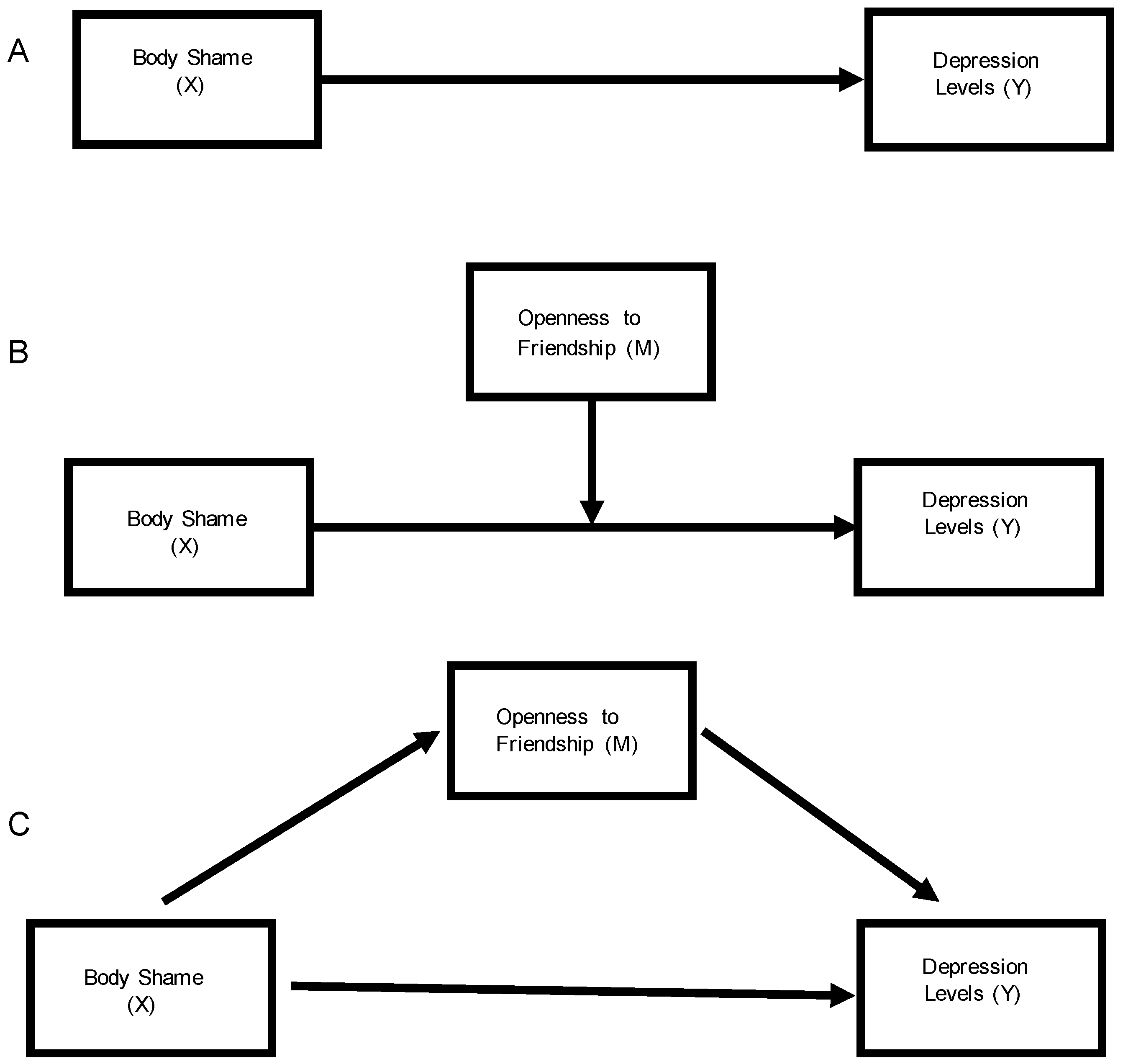
:1. Introduction
1.1. Study Rationale
1.2. Background
1.3. Study Aim
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Collection, Variables, and Measurement
2.2.1. Measurement of Depressive Symptom Levels
2.2.2. Measurement of Body Shame
2.2.3. Measurement of Openness to Friendship
2.2.4. Measurement of Overweight Status and Weight Concern
2.2.5. Key Covariates
2.3. Statistical Analysis
2.4. Ethics Statement
3. Results
3.1. Descriptive Statistics
3.2. Linear Regression Analysis
3.3. Mediation Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Llewellyn, A.; Simmonds, M.; Owen, C.G.; Woolacott, N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Mannan, M.; Mamun, A.; Doi, S.; Clavarino, A. Prospective associations between depression and obesity for adolescent males and females—A systematic review and meta-analysis of longitudinal studies. PLoS ONE 2016, 11, e0157240. [Google Scholar] [CrossRef] [PubMed]
- Major, B.; Tomiyama, A.J.; Hunger, J. The negative and bi-directional effects of weight stigma on health. In The Oxford Handbook of Stigma, Discrimination, and Health; Major, B., Dovidio, J., Link, B., Eds.; Oxford University Press: New York, NY, USA, 2017. [Google Scholar]
- Tomiyama, A.J. Weight stigma is stressful. A review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite 2014, 82, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Brewis, A.A. Stigma and the perpetuation of obesity. Soc. Sci. Med. 2014, 118, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.M.; Heuer, C.A. The stigma of obesity: A review and update. Obesity 2009, 17, 941–964. [Google Scholar] [CrossRef] [PubMed]
- Brewis, A.A.; Han, S.Y.; SturtzSreetharan, C.L. Weight, gender, and depressive symptoms in South Korea. Am. J. Hum. Biol. 2017, 29. [Google Scholar] [CrossRef] [PubMed]
- Su, W.; Di Santo, A. Preschool children’s perceptions of overweight peers. J. Early Child. Res. 2012, 10, 19–31. [Google Scholar] [CrossRef]
- Lumeng, J.C.; Forrest, P.; Appugliese, D.P.; Kaciroti, N.; Corwyn, R.F.; Bradley, R.H. Weight status as a predictor of being bullied in third through sixth grades. Pediatrics 2010, 125, e1301–e1307. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.M.; Latner, J.D.; O’brien, K.; Luedicke, J.; Forhan, M.; Danielsdottir, S. Cross-national perspectives about weight-based bullying in youth: Nature, extent and remedies. Pediatric Obes. 2016, 11, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Pont, S.J.; Puhl, R.; Cook, S.R.; Slusser, W. Stigma experienced by children and adolescents with obesity. Pediatrics 2017, 140, e20173034. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.M.; Brownell, K.D. Confronting and coping with weight stigma: An investigation of overweight and obese adults. Obesity 2006, 14, 1802–1815. [Google Scholar] [CrossRef] [PubMed]
- Brewis, A. Obesity: Cultural and Biocultural Perspectives; Rutgers University Press: New Brunswick, NJ, USA, 2011. [Google Scholar]
- Brewis, A.; Trainer, S.; Han, S.; Wutich, A. Publically misfitting: Extreme weight and the everyday production and reinforcement of felt stigma. Med. Anthropol. Q. 2017, 31, 257–276. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P. The relationship of shame, social anxiety and depression: The role of the evaluation of social rank. Clin. Psychol. Psychother. 2000, 7, 174–189. [Google Scholar] [CrossRef]
- Sjöberg, R.L.; Nilsson, K.W.; Leppert, J. Obesity, shame, and depression in school-aged children: A population-based study. Pediatrics 2005, 116, e389–e392. [Google Scholar] [CrossRef] [PubMed]
- Orth, U.; Berking, M.; Burkhardt, S. Self-conscious emotions and depression: Rumination explains why shame but not guilt is maladaptive. Personal. Soc. Psychol. Bull. 2006, 32, 1608–1619. [Google Scholar] [CrossRef] [PubMed]
- Sikorski, C.; Luppa, M.; Luck, T.; Riedel-Heller, S.G. Weight stigma “gets under the skin”—Evidence for an adapted psychological mediation framework—A systematic review. Obesity 2015, 23, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Cai, L.; Wu, Y.; Wilson, R.F.; Weston, C.; Fawole, O.; Bleich, S.N.; Cheskin, L.J.; Showell, N.N.; Lau, B.D.; et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes. Rev. 2015, 16, 547–565. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, J.E.; Lytle, L.A.; Laska, M.N. Stress, health risk behaviors, and weight status among community college students. Health Educ. Behav. 2016, 43, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Merchant, G.; Weibel, N.; Patrick, K.; Fowler, J.H.; Norman, G.J.; Gupta, A.; Servetas, C.; Calfas, K.; Raste, K.; Donohue, M.; et al. Click “like” to change your behavior: A mixed methods study of college students’ exposure to and engagement with Facebook content designed for weight loss. J. Med. Internet Res. 2014, 16. [Google Scholar] [CrossRef] [PubMed]
- Gow, R.W.; Trace, S.E.; Mazzeo, S.E. Preventing weight gain in first year college students: An online intervention to prevent the “freshman fifteen”. Eat. Behav. 2010, 11, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Trainer, S.; Brewis, A.; Williams, D.; Chavez, J.R. Obese, fat, or “just big”? Young adult deployment of and reactions to weight terms. Hum. Organ. 2015, 74, 266–275. [Google Scholar] [CrossRef]
- Brewis, A.; Brennhofer, S.; van Woerden, I.; Bruening, M. Weight stigma and eating behaviors on a college campus: Are students immune to stigma’s effects? Prev. Med. Rep. 2016, 4, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.C.; Story, M.; Larson, N.I.; Neumark-Sztainer, D.; Lytle, L.A. Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity 2008, 16, 2205–2211. [Google Scholar] [CrossRef] [PubMed]
- Levitsky, D.A.; Halbmaier, C.A.; Mrdjenovic, G. The freshman weight gain: A model for the study of the epidemic of obesity. Int. J. Obes. 2004, 28, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Bodenlos, J.S.; Gengarelly, K.; Smith, R. Gender differences in freshmen weight gain. Eat. Behave. 2015, 19, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Vadeboncoeur, C.; Townsend, N.; Foster, C. A meta-analysis of weight gain in first year university students: Is freshman 15 a myth? BMC Obes. 2015, 2, 22. [Google Scholar] [CrossRef] [PubMed]
- Gropper, S.S.; Simmons, K.P.; Connell, L.J.; Ulrich, P.V. Weight and body composition changes during the first three years of college. J. Obes. 2012. [Google Scholar] [CrossRef] [PubMed]
- Hovell, M.F.; Mewborn, C.R.; Randle, Y.; Fowler-Johnson, S. Risk of excess weight gain in university women: A three-year community controlled analysis. Addict. Behav. 1985, 10, 15–28. [Google Scholar] [CrossRef]
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Buote, V.M.; Pancer, S.M.; Pratt, M.W.; Adams, G.; Birnie-Lefcovitch, S.; Polivy, J.; Wintre, M.G. The importance of friends: Friendship and adjustment among 1st-year university students. J. Adolesc. Res. 2007, 22, 665–689. [Google Scholar] [CrossRef]
- Pliner, P.; Saunders, T. Vulnerability to freshman weight gain as a function of dietary restraint and residence. Physiol. Behav. 2008, 93, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Plotnikoff, R.C.; Costigan, S.A.; Williams, R.L.; Hutchesson, M.J.; Kennedy, S.G.; Robards, S.L.; Allen, J.; Collins, C.E.; Callister, R.; Germov, J. Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 45. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.L.; Brier, S. Friendsickness in the transition to college: Precollege predictors and college adjustment correlates. J. Couns. Dev. 2001, 79, 77–89. [Google Scholar] [CrossRef]
- Crombie, A.P.; Ilich, J.Z.; Dutton, G.R.; Panton, L.B.; Abood, D.A. The freshman weight gain phenomenon revisited. Nutr. Rev. 2009, 67, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Vella-Zarb, R.A.; Elgar, F.J. The ‘freshman 5’: A meta-analysis of weight gain in the freshman year of college. J. Am. Coll. Health 2009, 58, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Trainer, S.; Brewis, A.; Wutich, A.; Han, S.Y. Obesity, depression, and weight-related stigma syndemics. In Foundations of Biosocial Health: Stigma and Illness Interactions; Lerman, S., Ostrach, B., Singer, M., Eds.; Lexington Books: New York, NY, USA, 2017; pp. 83–106. [Google Scholar]
- Schaefer, D.R.; Simpkins, S.D. Using social network analysis to clarify the role of obesity in selection of adolescent friends. Am. J. Public Health 2014, 104, 1223–1229. [Google Scholar] [CrossRef] [PubMed]
- Pearce, M.J.; Boergers, J.; Prinstein, M.J. Adolescent obesity, overt and relational peer victimization, and romantic relationships. Obesity 2002, 10, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Aruguete, M.S.; Edman, J.L.; Yates, A. Romantic interest in obese college students. Eat. Behav. 2009, 10, 143–145. [Google Scholar] [CrossRef] [PubMed]
- Ettekal, A.V.; Simpkins, S.D.; Schaefer, D.R. Obesity and social marginalization: When do organized activities promote or hinder peer relationships? Appl. Dev. Sci. 2017, 1–12. [Google Scholar] [CrossRef]
- Christakis, N.A.; Fowler, J.H. The spread of obesity in a large social network over 32 years. N. Engl. J. Med. 2001, 357, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Brewis, A.A.; Hruschka, D.J.; Wutich, A. Vulnerability to fat-stigma in women’s everyday relationships. Soc. Sci. Med. 2011, 73, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hawkley, L.C.; Thisted, R.A. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol. Aging 2010, 25, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Bruening, M.; Ohri-Vachaspati, P.; Brewis, A.; Laska, M.; Todd, M.; Hruschka, D.; Schaefer, D.R.; Whisner, C.M.; Dunton, G. Longitudinal social networks impacts on weight and weight-related behaviors assessed using mobile-based ecological momentary assessments: Study Protocols for the SPARC study. BMC Public Health 2016, 16, 901. [Google Scholar] [CrossRef] [PubMed]
- American College Health Association. National College Health Assessment, 2013. Available online: http://www.acha-ncha.org/docs/ACHA-NCHA-II_UNDERGRAD_ReferenceGroup_DataReport_Spring2013.pdf (accessed on 22 June 2014).
- Vartanian, L.R.; Shaprow, J.G. Effects of weight stigma on exercise motivation and behavior: A preliminary investigation among college-aged females. J. Health Psychol. 2008, 13, 131–138. [Google Scholar] [CrossRef] [PubMed]
- McAndrew, F. The measurement of ‘rootedness’ and the prediction of attachment to home-towns in college students. J. Environ. Psychol. 1998, 18, 409–417. [Google Scholar] [CrossRef]
- Bui, K.V.T. First-generation college students at a four-year university: Background characteristics, reasons for pursuing higher education, and first-year experiences. Coll. Stud. J. 2002, 36, 3–12. [Google Scholar]
- Kessler, R.C. Epidemiology of women and depression. J. Affect. Disord. 2003, 74, 5–13. [Google Scholar] [CrossRef]
- Asher, M.; Asnaani, A.; Aderka, I.M. Gender differences in social anxiety disorder: A review. Clin. Psychol. Rev. 2017, 56, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Latner, J.D.; Stunkard, A.J.; Wilson, G.T. Stigmatized students: Age, sex, and ethnicity effects in the stigmatization of obesity. Obesity 2005, 13, 1226–1231. [Google Scholar] [CrossRef] [PubMed]
- Hebl, M.R.; Heatherton, T.F. The stigma of obesity in women: The difference is black and white. Personal. Soc. Psychol. Bull. 1998, 24, 417–426. [Google Scholar] [CrossRef]
- McClure, S. Symbolic body capital of an “other” kind: African American females as a bracketed subunit in female body valuation. In Fat Planet; Anderson-Fye, E., Brewis, A., Eds.; University of New Mexico Press: Albuquerque, NM, USA, 2017; pp. 97–124. [Google Scholar]
- Han, S.Y.; Brewis, A.A.; Wutich, A. Body image mediates the depressive effects of weight gain in new mothers, particularly for women already obese: Evidence from the Norwegian Mother and Child Cohort Study. BMC Public Health 2016, 16, 664. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.B.; Perez, M.; Kilpela, L.S.; Diedrichs, P.C.; Trujillo, E.; Stice, E. Engaging stakeholder communities as body image intervention partners: The Body Project as a case example. Eat. Behav. 2017, 25, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Farhat, T. Stigma, obesity and adolescent risk behaviors: Current research and future directions. Curr. Opin. Psychol. 2015, 5, 56–66. [Google Scholar] [CrossRef] [PubMed]
| Key Variables of Interest | Phase 1 Start of Fall Semester | Phase 2 End of Fall Semester | Phase 3 Start of Spring Semester | Phase 4 End of the Spring Semester |
|---|---|---|---|---|
| n = 1430 64.9% Female | n = 629 70.5% Female | n = 555 71.2% Female | n = 534 70.5% Female | |
| Means (SD) | ||||
| Depression levels (0–20 scale) | 5.34 (3.8) | 5.85 (3.9) | 5.13 (3.8) | 5.82 (4.0) |
| Friendship scores (1–4 scale) | 3.3 (0.4) | --* | 3.1 (0.4) | --* |
| Body shame (0–4 scale) | 1.61 (0.8) | 1.61 (0.8) | --* | 1.66 (0.8) |
| Body mass index (BMI) | 24.1 (4.9) | 24.6 (5.1) | 24.6 (5.1) | 29.4 (5.3) |
| Weight concern (believes is overweight) | 3.3 (0.9) | 3.5 (0.8) | 3.5 (0.9) | --* |
| Weight change since Phase 1 (based on BMI change) | -- | .69 (6.9) | 0.72 (7.3) | 0.63 (7.2) |
| Outcome | Predictor | B | SE | 95% CI Lower | 95% CI Upper | p |
|---|---|---|---|---|---|---|
| Depression at start of school year (N = 1443) | Body shame | 0.305 | 0.025 | 0.256 | 0.354 | 0.000 |
| Friendship score | −0.363 | 0.044 | −0.449 | −0.276 | 0.000 | |
| Overweight status | −0.133 | 0.058 | −0.246 | −0.020 | 0.021 | |
| Believes is overweight | 0.005 | 0.027 | −0.047 | 0.058 | 0.846 | |
| Male gender | −0.193 | 0.041 | −0.273 | −0.112 | 0.000 | |
| Majority ethnicity | 0.056 | 0.037 | −0.018 | 0.129 | 0.137 | |
| Depression at end of fall semester (n = 629) | Body shame | 0.240 | 0.064 | 0.114 | 0.366 | 0.000 |
| Friendship score | −0.114 | 0.114 | −0.339 | 0.111 | 0.320 | |
| Overweight status | −0.055 | 0.138 | −0.326 | 0.215 | 0.687 | |
| Believes is overweight | 0.170 | 0.066 | 0.040 | 0.300 | 0.011 | |
| Male gender | −0.003 | 0.100 | −0.200 | 0.194 | 0.978 | |
| Majority ethnicity | 0.098 | 0.090 | −0.079 | 0.275 | 0.276 | |
| Weight change to date | 0.001 | 0.009 | −0.016 | 0.018 | 0.922 | |
| Depression at start of spring semester (n = 555) | Body shame | 0.172 | 0.076 | 0.023 | 0.322 | 0.024 |
| Friendship score | −0.219 | 0.143 | −0.501 | 0.062 | 0.126 | |
| Overweight status | −0.022 | 0.173 | −0.364 | 0.320 | 0.900 | |
| Believes is overweight | 0.204 | 0.069 | 0.069 | 0.340 | 0.003 | |
| Male gender | −0.093 | 0.111 | −0.313 | 0.126 | 0.403 | |
| Majority ethnicity | 0.189 | 0.103 | −0.014 | 0.392 | 0.068 | |
| Weight change to date | 0.010 | 0.008 | −0.006 | 0.026 | 0.220 | |
| Depression at end of school year (n = 534) | Body shame | 0.287 | 0.085 | 0.119 | 0.455 | 0.001 |
| Friendship score | −0.109 | 0.160 | −0.426 | 0.208 | 0.497 | |
| Overweight status | −0.049 | 0.183 | −0.411 | 0.312 | 0.788 | |
| Believes is overweight | 0.241 | 0.091 | 0.061 | 0.420 | 0.009 | |
| Male gender | 0.188 | 0.143 | −0.094 | 0.469 | 0.190 | |
| Majority ethnicity | 0.237 | 0.123 | −0.007 | 0.481 | 0.056 | |
| Weight change to date | 0.012 | 0.011 | −0.010 | 0.035 | 0.284 |
| Phase | Predictor | Outcome | Estimate (b) | SE | p |
|---|---|---|---|---|---|
| Start of the school year | Body shame | Friendship | −0.110 | 0.016 | *** |
| Friendship | Depression | −0.509 | 0.055 | *** | |
| Body shame | Depression | 0.291 | 0.028 | *** | |
| End of fall semester | Body shame | Friendship | −0.100 | 0.022 | *** |
| Friendship | Depression | −0.266 | 0.085 | 0.002 | |
| Body shame | Depression | 0.262 | 0.042 | *** | |
| Start of spring semester | Body shame | Friendship | −0.059 | 0.026 | 0.022 |
| Friendship | Depression | −0.444 | 0.090 | *** | |
| Body shame | Depression | 0.324 | 0.045 | *** | |
| End of spring semester | Body shame | Friendship | −0.033 | 0.027 | 0.210 |
| Friendship | Depression | −0.227 | 0.104 | 0.029 | |
| Body shame | Depression | 0.346 | 0.043 | *** |
| Phase | Predictor | Outcome | Estimate (b) | SE | p |
|---|---|---|---|---|---|
| Start of the school year | Body shame | Friendship | −0.066 | 0.027 | 0.013 |
| Friendship | Depression | −0.155 | 0.069 | 0.025 | |
| Body shame | Depression | 0.285 | 0.041 | *** | |
| End of fall semester | Body shame | Friendship | −0.099 | 0.046 | 0.031 |
| Friendship | Depression | −0.133 | 0.042 | 0.002 | |
| Body shame | Depression | 0.269 | 0.095 | 0.005 | |
| Start of spring semester | Body shame | Friendship | −0.133 | 0.042 | 0.002 |
| Friendship | Depression | −0.145 | 0.173 | 0.402 | |
| Body shame | Depression | 0.269 | 0.095 | 0.005 | |
| End of spring semester | Body shame | Friendship | −0.133 | 0.043 | 0.002 |
| Friendship | Depression | −0.234 | 0.202 | 0.245 | |
| Body shame | Depression | 0.250 | 0.092 | 0.007 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brewis, A.A.; Bruening, M. Weight Shame, Social Connection, and Depressive Symptoms in Late Adolescence. Int. J. Environ. Res. Public Health 2018, 15, 891. https://doi.org/10.3390/ijerph15050891
Brewis AA, Bruening M. Weight Shame, Social Connection, and Depressive Symptoms in Late Adolescence. International Journal of Environmental Research and Public Health. 2018; 15(5):891. https://doi.org/10.3390/ijerph15050891
Chicago/Turabian StyleBrewis, Alexandra A., and Meg Bruening. 2018. "Weight Shame, Social Connection, and Depressive Symptoms in Late Adolescence" International Journal of Environmental Research and Public Health 15, no. 5: 891. https://doi.org/10.3390/ijerph15050891
APA StyleBrewis, A. A., & Bruening, M. (2018). Weight Shame, Social Connection, and Depressive Symptoms in Late Adolescence. International Journal of Environmental Research and Public Health, 15(5), 891. https://doi.org/10.3390/ijerph15050891





